Optimal Ablation Settings Predicting Durable Scar Detected Using LGE-MRI after Modified Left Atrial Anterior Line Ablation
Abstract
1. Introduction
2. Methods
2.1. Patient Population
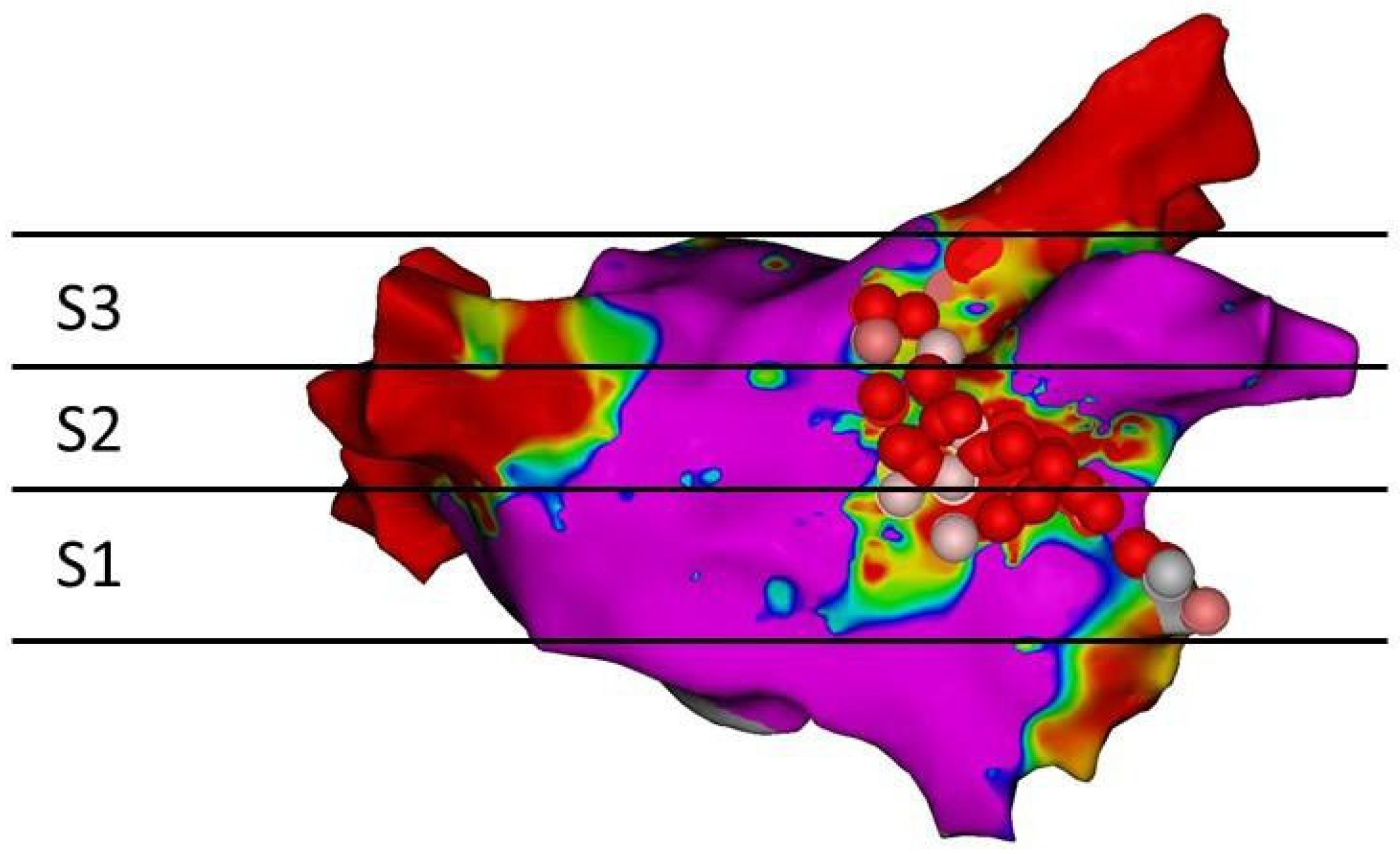
2.2. Ablation Procedure
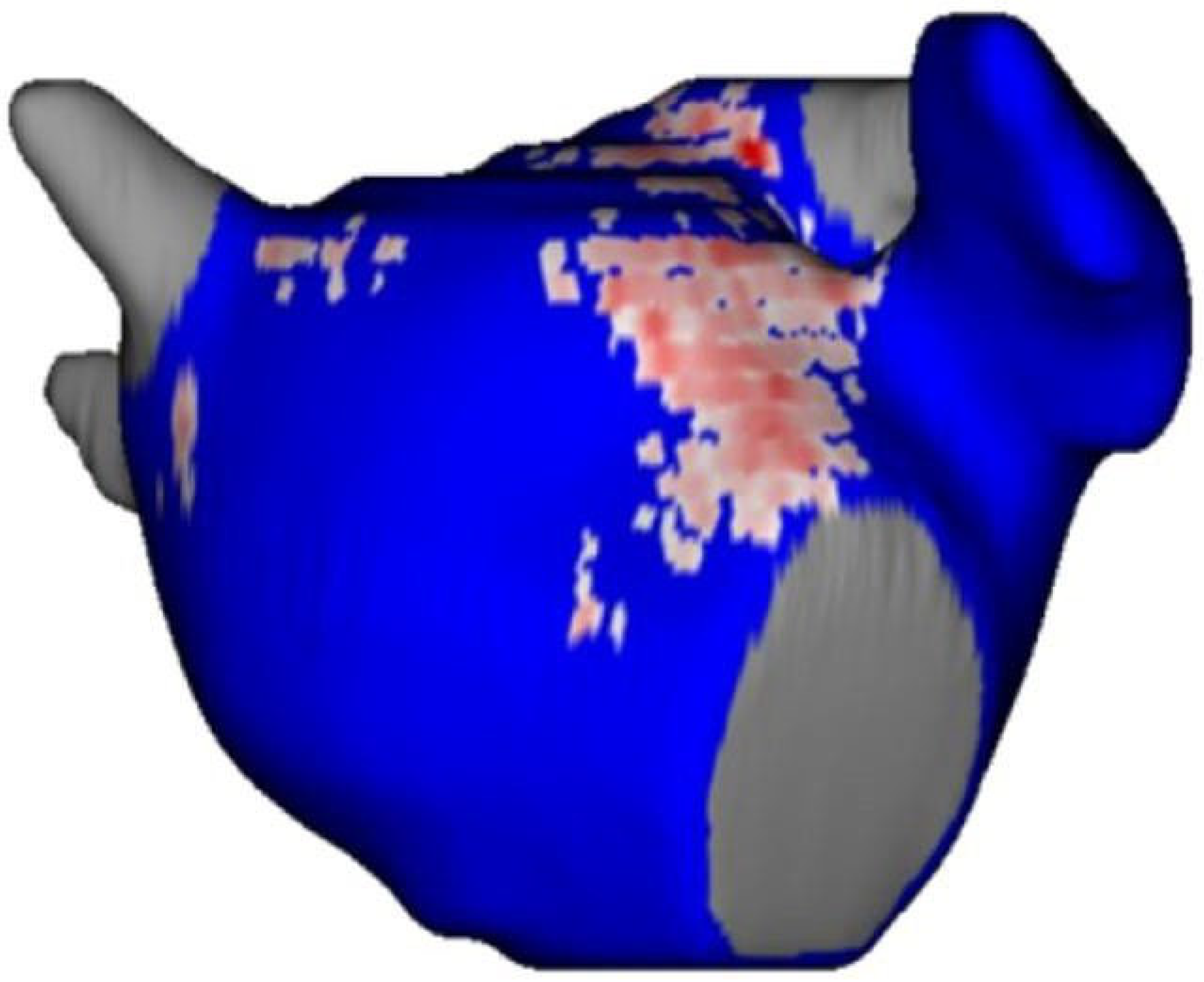
2.3. Late Gadolinium Enhancement Magnetic Resonance Imaging
2.4. Analysis of Scar
2.5. Statistical Analysis
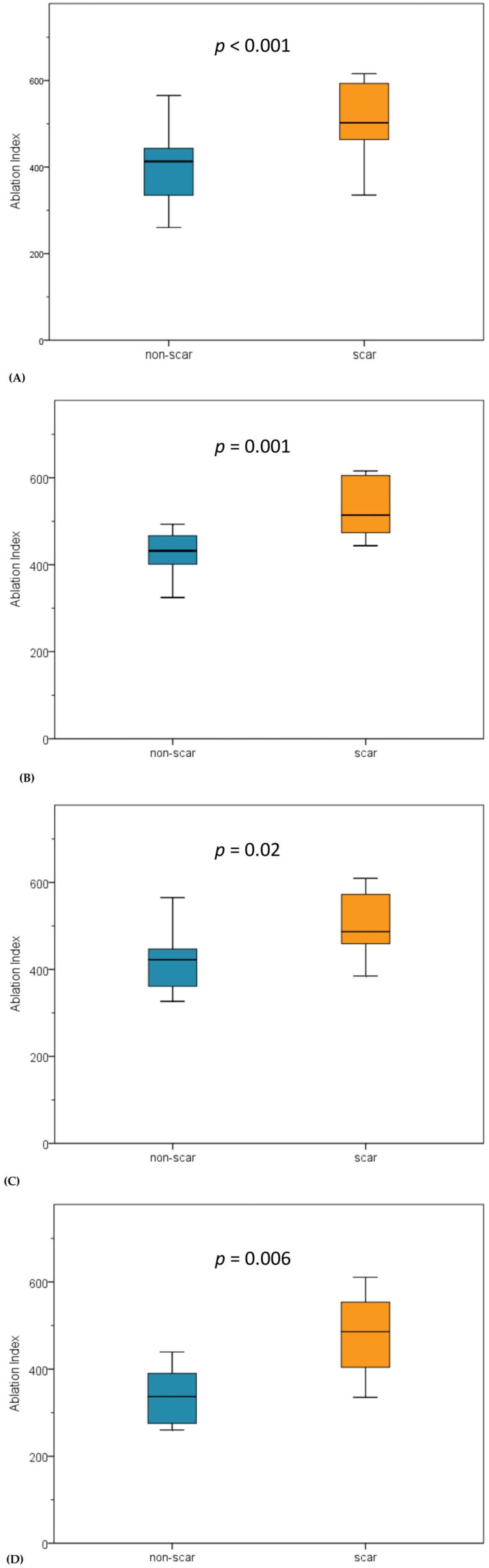
3. Results
3.1. Acute Results
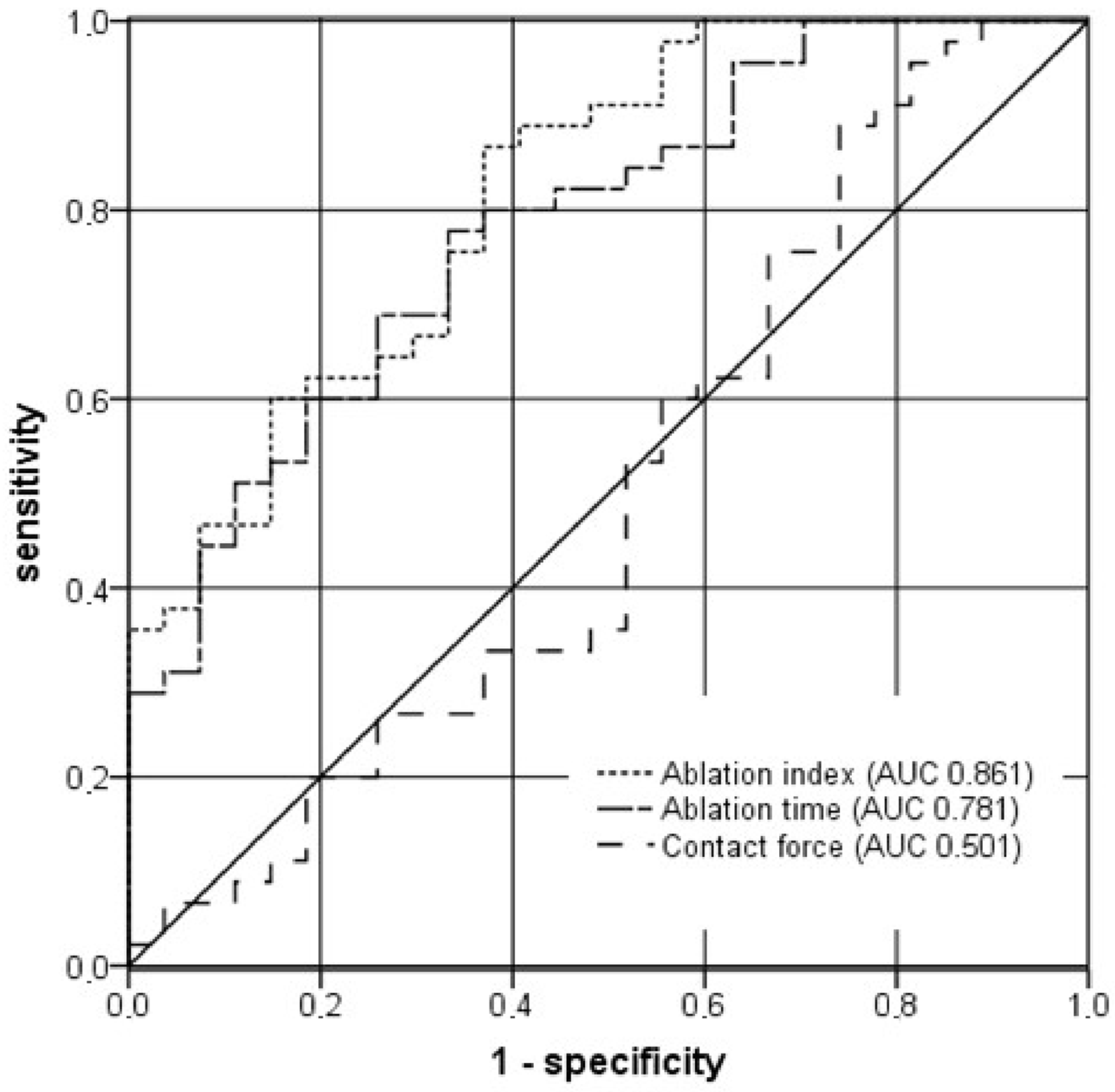
3.2. LGE-MRI Results
4. Discussion
4.1. Main Findings
4.2. Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Matsuo, S.; Wright, M.; Knecht, S.; Nault, I.; Lellouche, N.; Lim, K.T.; Arantes, L.; O’Neill, M.D.; Hocini, M.; Jaïs, P.; et al. Peri-mitral atrial flutter in patients with atrial fibrillation ablation. Heart Rhythm 2010, 7, 2–8. [Google Scholar] [CrossRef]
- Ammar, S.; Luik, A.; Hessling, G.; Bruhm, A.; Reents, T.; Semmler, V.; Buiatti, A.; Kathan, S.; Hofmann, M.; Kolb, C.; et al. Ablation of perimitral flutter: Acute and long-term success of the modified anterior line. Europace 2015, 17, 447–452. [Google Scholar] [CrossRef]
- Kircher, S.; Arya, A.; Altmann, D.; Rolf, S.; Bollmann, A.; Sommer, P.; Dagres, N.; Richter, S.; Breithardt, O.A.; Dinov, B.; et al. Individually tailored vs. standardized substrate modification during radiofrequency catheter ablation for atrial fibrillation: A randomized study. Europace 2018, 20, 1766–1775. [Google Scholar] [CrossRef] [PubMed]
- Tzeis, S.; Luik, A.; Jilek, C.; Schmitt, C.; Estner, H.L.; Wu, J.; Reents, T.; Fichtner, S.; Kolb, C.; Karch, M.R.; et al. The modified anterior line: An alternative linear lesion in perimitral flutter. J. Cardiovasc. Electrophysiol. 2010, 21, 665–670. [Google Scholar] [CrossRef] [PubMed]
- Calkins, H.; Hindricks, G.; Cappato, R.; Kim, Y.H.; Saad, E.B.; Aguinaga, L.; Akar, J.G.; Badhwar, V.; Brugada, J.; Camm, J.; et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace 2018, 20, e1–e160. [Google Scholar] [CrossRef] [PubMed]
- Jais, P.; Haissaguerre, M.; Shah, D.C.; Takahashi, A.; Hocini, M.; Lavergne, T.; Lafitte, S.; Le Mouroux, A.; Fischer, B.; Clementy, J. Successful irrigated-tip catheter ablation of atrial flutter resistant to conventional radiofrequency ablation. Circulation 1998, 98, 835–838. [Google Scholar] [CrossRef] [PubMed]
- Haines, D.E.; Strunk, A.R.; Novichenok, A.; Kirchhof, N.; Stewart, M. The Biophysics of Passive Convective Cooling During Catheter Ablation with Gold versus Platinum Electrodes and Multielectrode Phased Radiofrequency Energy Delivery. J. Cardiovasc. Electrophysiol. 2015, 26, 1257–1261. [Google Scholar] [CrossRef] [PubMed]
- Bisbal, F.; Guiu, E.; Cabanas-Grandio, P.; Berruezo, A.; Prat-Gonzalez, S.; Vidal, B.; Garrido, C.; Andreu, D.; Fernandez-Armenta, J.; Tolosana, J.M.; et al. CMR-guided approach to localize and ablate gaps in repeat AF ablation procedure. JACC Cardiovasc. Imaging 2014, 7, 653–663. [Google Scholar] [CrossRef]
- Chubb, H.; Aziz, S.; Karim, R.; Sohns, C.; Razeghi, O.; Williams, S.E.; Whitaker, J.; Harrison, J.; Chiribiri, A.; Schaeffter, T.; et al. Optimization of late gadolinium enhancement cardiovascular magnetic resonance imaging of post-ablation atrial scar: A cross-over study. J. Cardiovasc. Magn. Reson. Off. J. Soc. Cardiovasc. Magn. Reson. 2018, 20, 30. [Google Scholar] [CrossRef] [PubMed]
- Spragg, D.D.; Khurram, I.; Zimmerman, S.L.; Yarmohammadi, H.; Barcelon, B.; Needleman, M.; Edwards, D.; Marine, J.E.; Calkins, H.; Nazarian, S. Initial experience with magnetic resonance imaging of atrial scar and co-registration with electroanatomic voltage mapping during atrial fibrillation: Success and limitations. Heart Rhythm 2012, 9, 2003–2009. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, K.; Kamali, R.; Kwan, E.; MacLeod, R.S.; Dosdall, D.J.; Ranjan, R. Effective Ablation Settings That Predict Chronic Scar After Left Atrial Ablation. JACC Clin. Electrophysiol. 2020, 6, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Akoum, N.; Wilber, D.; Hindricks, G.; Jais, P.; Cates, J.; Marchlinski, F.; Kholmovski, E.; Burgon, N.; Hu, N.; Mont, L.; et al. MRI Assessment of Ablation-Induced Scarring in Atrial Fibrillation: Analysis from the DECAAF Study. J. Cardiovasc. Electrophysiol. 2015, 26, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Phlips, T.; Taghji, P.; El Haddad, M.; Wolf, M.; Knecht, S.; Vandekerckhove, Y.; Tavernier, R.; Duytschaever, M. Improving procedural and one-year outcome after contact force-guided pulmonary vein isolation: The role of interlesion distance, ablation index, and contact force variability in the ‘CLOSE’-protocol. Europace 2018, 20, f419–f427. [Google Scholar] [CrossRef] [PubMed]
- Hussein, A.; Das, M.; Riva, S.; Morgan, M.; Ronayne, C.; Sahni, A.; Shaw, M.; Todd, D.; Hall, M.; Modi, S.; et al. Use of Ablation Index-Guided Ablation Results in High Rates of Durable Pulmonary Vein Isolation and Freedom From Arrhythmia in Persistent Atrial Fibrillation Patients: The PRAISE Study Results. Circ. Arrhythmia Electrophysiol. 2018, 11, e006576. [Google Scholar] [CrossRef]
- Teres, C.; Soto-Iglesias, D.; Penela, D.; Jauregui, B.; Ordonez, A.; Chauca, A.; Huguet, M.; Ramirez-Paesano, C.; Oller, G.; Jornet, A.; et al. Left atrial wall thickness of the pulmonary vein reconnection sites during atrial fibrillation redo procedures. Pacing Clin. Electrophysiol. PACE 2021, 44, 824–834. [Google Scholar] [CrossRef]
- Beinart, R.; Abbara, S.; Blum, A.; Ferencik, M.; Heist, K.; Ruskin, J.; Mansour, M. Left atrial wall thickness variability measured by CT scans in patients undergoing pulmonary vein isolation. J. Cardiovasc. Electrophysiol. 2011, 22, 1232–1236. [Google Scholar] [CrossRef]
- Ikeda, A.; Nakagawa, H.; Lambert, H.; Shah, D.C.; Fonck, E.; Yulzari, A.; Sharma, T.; Pitha, J.V.; Lazzara, R.; Jackman, W.M. Relationship between catheter contact force and radiofrequency lesion size and incidence of steam pop in the beating canine heart: Electrogram amplitude, impedance, and electrode temperature are poor predictors of electrode-tissue contact force and lesion size. Circ. Arrhythmia Electrophysiol. 2014, 7, 1174–1180. [Google Scholar] [CrossRef]
- Williams, S.E.; Harrison, J.; Chubb, H.; Bloch, L.O.; Andersen, N.P.; Dam, H.; Karim, R.; Whitaker, J.; Gill, J.; Cooklin, M.; et al. The Effect of Contact Force in Atrial Radiofrequency Ablation: Electroanatomical, Cardiovascular Magnetic Resonance, and Histological Assessment in a Chronic Porcine Model. JACC Clin. Electrophysiol. 2015, 1, 421–431. [Google Scholar] [CrossRef]
- Andreu, D.; Gomez-Pulido, F.; Calvo, M.; Carlosena-Remirez, A.; Bisbal, F.; Borras, R.; Benito, E.; Guasch, E.; Prat-Gonzalez, S.; Perea, R.J.; et al. Contact force threshold for permanent lesion formation in atrial fibrillation ablation: A cardiac magnetic resonance-based study to detect ablation gaps. Heart Rhythm 2016, 13, 37–45. [Google Scholar] [CrossRef][Green Version]
- Thomas, S.; Silvernagel, J.; Angel, N.; Kholmovski, E.; Ghafoori, E.; Hu, N.; Ashton, J.; Dosdall, D.J.; MacLeod, R.; Ranjan, R. Higher contact force during radiofrequency ablation leads to a much larger increase in edema as compared to chronic lesion size. J. Cardiovasc. Electrophysiol. 2018, 29, 1143–1149. [Google Scholar] [CrossRef]
- Yokoyama, K.; Nakagawa, H.; Shah, D.C.; Lambert, H.; Leo, G.; Aeby, N.; Ikeda, A.; Pitha, J.V.; Sharma, T.; Lazzara, R.; et al. Novel contact force sensor incorporated in irrigated radiofrequency ablation catheter predicts lesion size and incidence of steam pop and thrombus. Circ. Arrhythmia Electrophysiol. 2008, 1, 354–362. [Google Scholar] [CrossRef]
- Bourier, F.; Popa, M.; Kottmaier, M.; Maurer, S.; Bahlke, F.; Telishevska, M.; Lengauer, S.; Koch-Buttner, K.; Kornmayer, M.; Risse, E.; et al. RF electrode-tissue coverage significantly influences steam pop incidence and lesion size. J. Cardiovasc. Electrophysiol. 2021, 32, 1594–1599. [Google Scholar] [CrossRef] [PubMed]
- Chinitz, J.S.; Kapur, S.; Barbhaiya, C.; Kumar, S.; John, R.; Epstein, L.M.; Tedrow, U.; Stevenson, W.G.; Michaud, G.F. Sites With Small Impedance Decrease During Catheter Ablation for Atrial Fibrillation Are Associated With Recovery of Pulmonary Vein Conduction. J. Cardiovasc. Electrophysiol. 2016, 27, 1390–1398. [Google Scholar] [CrossRef]
- Leshem, E.; Zilberman, I.; Tschabrunn, C.M.; Barkagan, M.; Contreras-Valdes, F.M.; Govari, A.; Anter, E. High-Power and Short-Duration Ablation for Pulmonary Vein Isolation: Biophysical Characterization. JACC Clin. Electrophysiol. 2018, 4, 467–479. [Google Scholar] [CrossRef]
- Ali-Ahmed, F.; Goyal, V.; Patel, M.; Orelaru, F.; Haines, D.E.; Wong, W.S. High-power, low-flow, short-ablation duration-the key to avoid collateral injury? J. Interv. Card. Electrophysiol. Int. J. Arrhythm. Pacing 2019, 55, 9–16. [Google Scholar] [CrossRef]
- Winkle, R.A.; Mohanty, S.; Patrawala, R.A.; Mead, R.H.; Kong, M.H.; Engel, G.; Salcedo, J.; Trivedi, C.G.; Gianni, C.; Jais, P.; et al. Low complication rates using high power (45-50 W) for short duration for atrial fibrillation ablations. Heart Rhythm 2019, 16, 165–169. [Google Scholar] [CrossRef]
- Bourier, F.; Duchateau, J.; Vlachos, K.; Lam, A.; Martin, C.A.; Takigawa, M.; Kitamura, T.; Frontera, A.; Cheniti, G.; Pambrun, T.; et al. High-power short-duration versus standard radiofrequency ablation: Insights on lesion metrics. J. Cardiovasc. Electrophysiol. 2018, 29, 1570–1575. [Google Scholar] [CrossRef]
- Zanchi, S.; Chen, S.; Bordignon, S.; Bianchini, L.; Tohoku, S.; Bologna, F.; Tondo, C.; Chun, K.R.J.; Schmidt, B. Ablation Index-guided high-power (50 W) short-duration for left atrial anterior and roofline ablation: Feasibility, procedural data, and lesion analysis (AI High-Power Linear Ablation). J. Cardiovasc. Electrophysiol. 2021, 32, 984–993. [Google Scholar] [CrossRef]
- Badger, T.J.; Daccarett, M.; Akoum, N.W.; Adjei-Poku, Y.A.; Burgon, N.S.; Haslam, T.S.; Kalvaitis, S.; Kuppahally, S.; Vergara, G.; McMullen, L.; et al. Evaluation of left atrial lesions after initial and repeat atrial fibrillation ablation: Lessons learned from delayed-enhancement MRI in repeat ablation procedures. Circ. Arrhythmia Electrophysiol. 2010, 3, 249–259. [Google Scholar] [CrossRef]
- Althoff, T.F.; Garre, P.; Caixal, G.; Perea, R.; Prat, S.; Tolosana, J.M.; Guasch, E.; Roca-Luque, I.; Arbelo, E.; Sitges, M.; et al. Late gadolinium enhancement-MRI determines definite lesion formation most accurately at 3 months post ablation compared to later time points. Pacing Clin. Electrophysiol. PACE 2022, 45, 72–82. [Google Scholar] [CrossRef]
- Kheirkhahan, M.; Baher, A.; Goldooz, M.; Kholmovski, E.G.; Morris, A.K.; Csecs, I.; Chelu, M.G.; Wilson, B.D.; Marrouche, N.F. Left atrial fibrosis progression detected by LGE-MRI after ablation of atrial fibrillation. Pacing Clin. Electrophysiol. PACE 2020, 43, 402–411. [Google Scholar] [CrossRef]

| Patient Characteristics (n = 24) | |
|---|---|
| Age, years | 72 ± 9.3 |
| Male, % | 45.8 |
| CHA2DSVASc Score | 3.1 ± 1.1 |
| Body mass index, kg/m2 | 30.5 ± 5.9 |
| LA-diameter, mm | 51.9 ± 7.2 |
| LVEF, % | 57.1 ± 12.4 |
| Time of LGE-CMR after ablation, days | 97.5 ± 14.6 |
| Non-Scar | Scar | p Value | |
|---|---|---|---|
| Total MAL | |||
| N | 295 | 564 | |
| AI | 413.19 (326.84–446.97) | 502.1 (450.2–583.4) | <0.0001 |
| Impedance drop, ohms | 4.8 (3.4–6.3) | 5.6 (3.8–6.8) | 0.118 |
| Force, g | 17.9 (11.9–19.9) | 17.1 (13.9–19.3) | 0.986 |
| Time, s | 15.5 (12.2–18.8) | 19.5 (16.6–26.3) | <0.0001 |
| S1 | |||
| N | 88 | 172 | |
| AI | 432.1 (395.3–474.8) | 514.2 (471.1–605.6) | 0.001 |
| Impedance drop, ohms | 4.5 (3.1–6.6) | 5.7 (3.7–6.7) | 0.391 |
| Force, g | 18.5 (14.8–26.9) | 17.6 (13.7–21.2) | 0.668 |
| Time, s | 15.8 (13.2–17.5) | 20.4 (17.8–23.9) | 0.012 |
| S2 | |||
| N | 92 | 185 | |
| AI | 422.4 (352.1–481.6) | 486.7 (446.1–603.7) | 0.020 |
| Impedance drop, ohms | 5.2 (4.0–6.9) | 5.6 (4.0–6.5) | 1.000 |
| Force, g | 18.1 (15.1–19.4) | 15.6 (13.8–19.6) | 0.519 |
| Time, s | 15.4 (12.1–19.1) | 22.1 (17.8–28.7) | 0.018 |
| S3 | |||
| N | 115 | 207 | |
| AI | 336.8 (272.2–402.5) | 485.9 (396.1–563.7) | 0.006 |
| Impedance drop, ohms | 3.9 (3.2–5.7) | 6.1 (4.5–8.9) | 0.089 |
| Force, g | 13.8 (9.6–19.4) | 16.8 (14.1–18.1) | 0.482 |
| Time, s | 13.9 (9.1–19.1) | 20.2 (14.6–27.7) | 0.026 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forkmann, M.; Mahnkopf, C.; Mitlacher, M.; Wolff, M.; Tose Costa Paiva, B.; Busch, S. Optimal Ablation Settings Predicting Durable Scar Detected Using LGE-MRI after Modified Left Atrial Anterior Line Ablation. J. Clin. Med. 2022, 11, 830. https://doi.org/10.3390/jcm11030830
Forkmann M, Mahnkopf C, Mitlacher M, Wolff M, Tose Costa Paiva B, Busch S. Optimal Ablation Settings Predicting Durable Scar Detected Using LGE-MRI after Modified Left Atrial Anterior Line Ablation. Journal of Clinical Medicine. 2022; 11(3):830. https://doi.org/10.3390/jcm11030830
Chicago/Turabian StyleForkmann, Mathias, Christian Mahnkopf, Marcel Mitlacher, Marc Wolff, Beatriz Tose Costa Paiva, and Sonia Busch. 2022. "Optimal Ablation Settings Predicting Durable Scar Detected Using LGE-MRI after Modified Left Atrial Anterior Line Ablation" Journal of Clinical Medicine 11, no. 3: 830. https://doi.org/10.3390/jcm11030830
APA StyleForkmann, M., Mahnkopf, C., Mitlacher, M., Wolff, M., Tose Costa Paiva, B., & Busch, S. (2022). Optimal Ablation Settings Predicting Durable Scar Detected Using LGE-MRI after Modified Left Atrial Anterior Line Ablation. Journal of Clinical Medicine, 11(3), 830. https://doi.org/10.3390/jcm11030830





