Longitudinal Speckle Tracking Strain Abnormalities in Chagas Disease: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
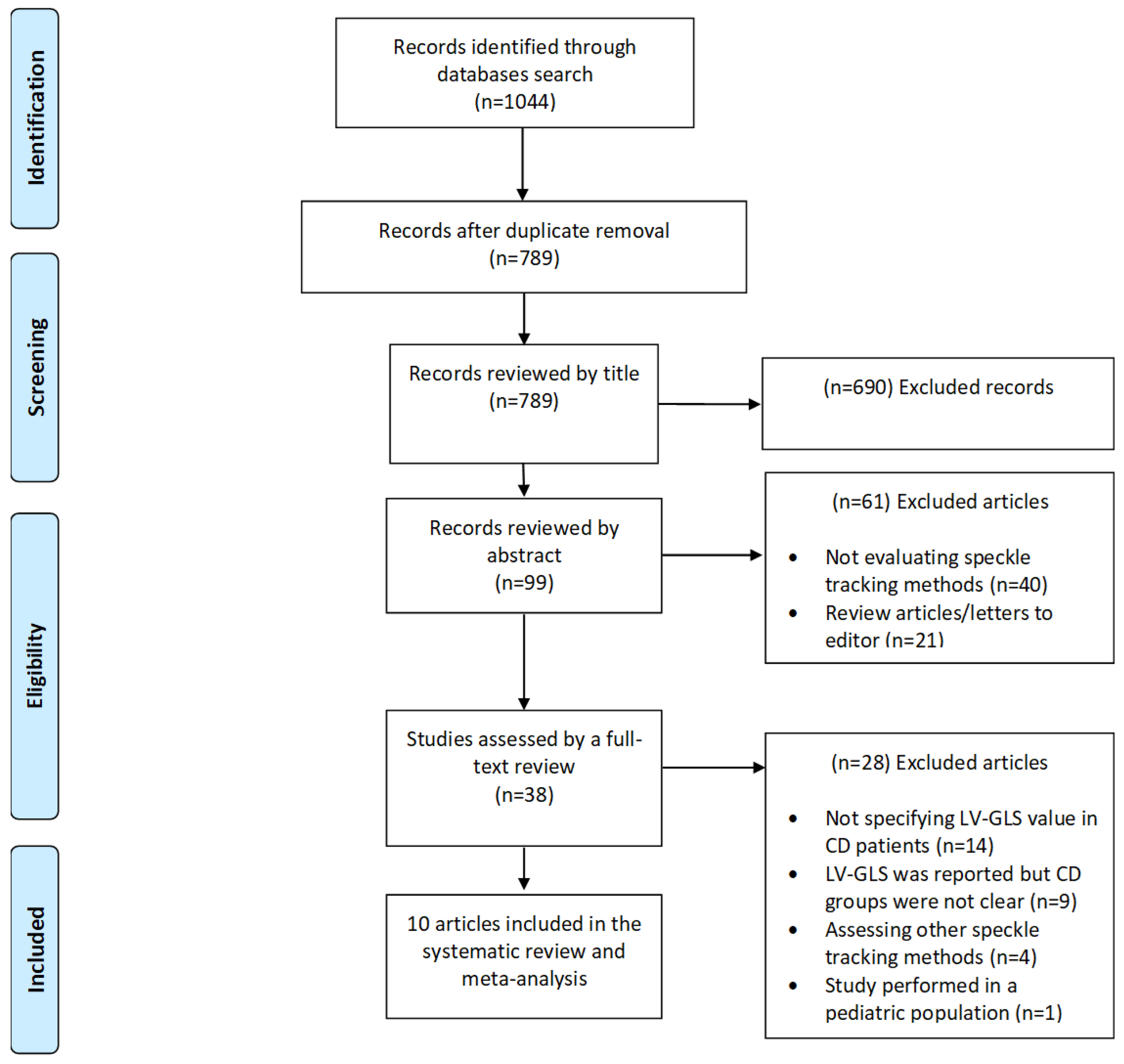
2. Methods
2.1. Data Source and Strategy
2.2. Study Selection and Eligibility Criteria
2.3. Data Extraction
2.4. Risk of Bias Assessment and Quality Assessment
2.5. Statistical Analysis
2.6. Sensitivity Analyses
3. Results
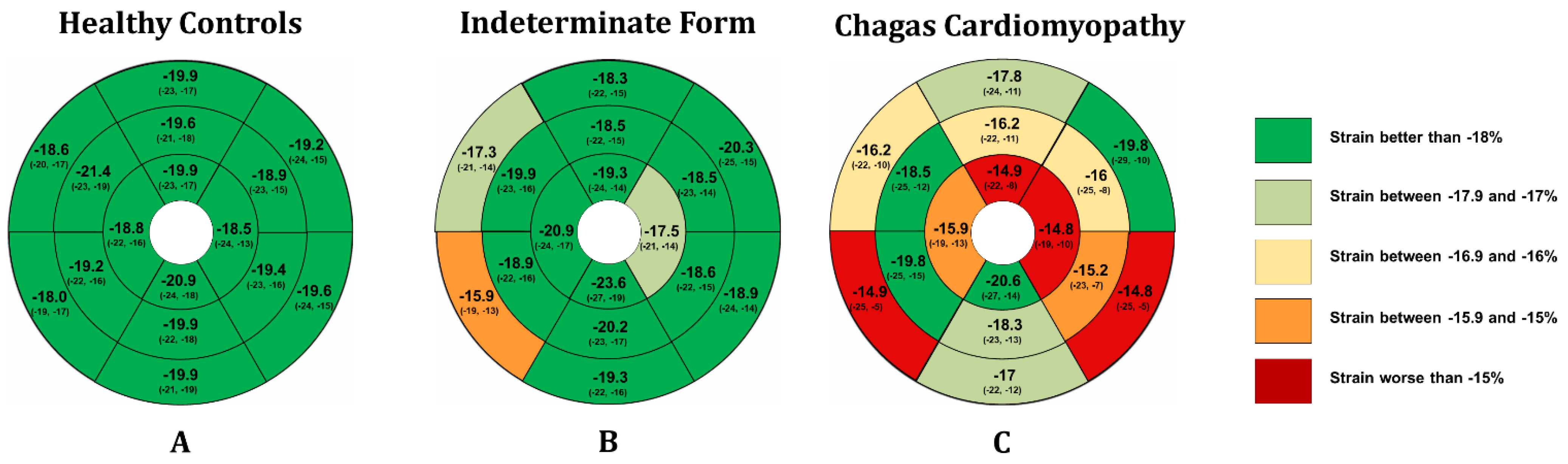
3.1. Longitudinal Speckle Tracking Strain in the Indeterminate form of Chagas Disease
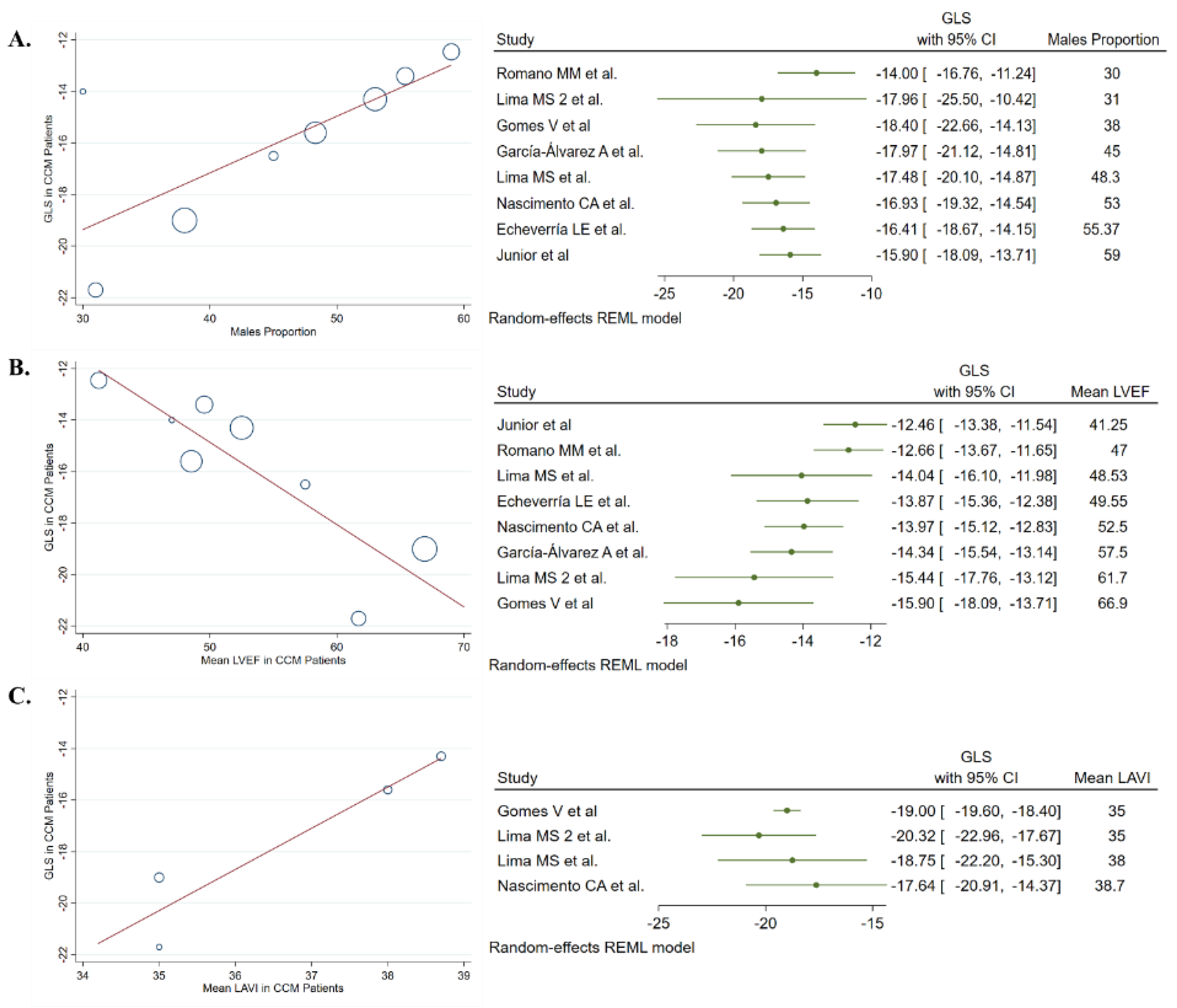
3.2. Longitudinal Speckle Tracking Strain in Chronic Chagas Cardiomyopathy
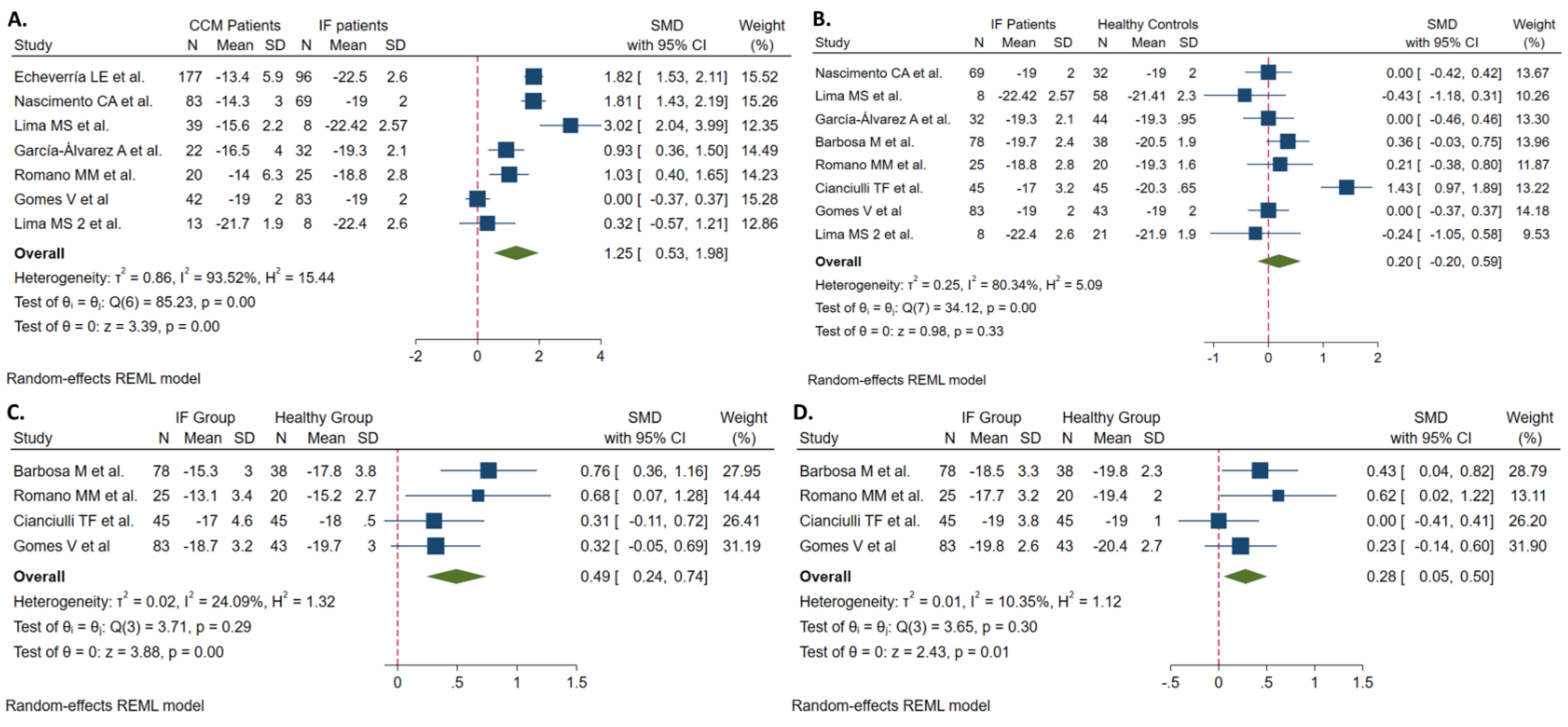
3.3. CCM vs. Indeterminate Patients
3.4. Indeterminate Patients vs. Healthy Controls
3.5. Sensitivity Analysis
3.6. Quality of Studies and Publication Bias
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Echeverria, L.E.; Morillo, C.A. American Trypanosomiasis (Chagas Disease). Infect. Dis. Clin. N. Am. 2019, 33, 119–134. [Google Scholar] [CrossRef] [PubMed]
- Requena-Méndez, A.; Aldasoro, E.; De Lazzari, E.; Sicuri, E.; Brown, M.; Moore, D.A.J.; Gascon, J.; Muñoz, J. Prevalence of Chagas Disease in Latin-American Migrants Living in Europe: A Systematic Review and Meta-analysis. PLoS Negl. Trop. Dis. 2015, 9, e0003540. [Google Scholar] [CrossRef] [PubMed]
- Bern, C.; Messenger, L.A.; Whitman, J.D.; Maguire, J.H. Chagas Disease in the United States: A Public Health Approach. Clin. Microbiol. Rev. 2019, 33, e00023-19. [Google Scholar] [CrossRef] [PubMed]
- Manne-Goehler, J.; Umeh, C.; Montgomery, S.P.; Wirtz, V.J. Estimating the Burden of Chagas Disease in the United States. PLoS Negl. Trop. Dis. 2016, 10, e0005033. [Google Scholar] [CrossRef] [PubMed]
- Strasen, J.; Williams, T.; Ertl, G.; Zoller, T.; Stich, A.; Ritter, O. Epidemiology of Chagas disease in Europe: Many calculations, little knowledge. Clin. Res. Cardiol. 2013, 103, 1–10. [Google Scholar] [CrossRef]
- González, F.B.; Villar, S.R.; Pacini, M.F.; Bottasso, O.A.; Perez, A.R. Immune-neuroendocrine and metabolic disorders in human and experimental T. cruzi infection: New clues for understanding Chagas disease pathology. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2020, 1866, 165642. [Google Scholar] [CrossRef]
- Nunes, M.C.P.; Beaton, A.; Acquatella, H.; Bern, C.; Bolger, A.F.; Echeverría, L.E.; Dutra, W.O.; Gascon, J.; Morillo, C.A.; Oliveira-Filho, J.; et al. Chagas Cardiomyopathy: An Update of Current Clinical Knowledge and Management: A Scientific Statement From the American Heart Association. Circulation 2018, 138, e169–e209. [Google Scholar] [CrossRef]
- Echeverría, L.E.; Marcus, R.; Novick, G.; Sosa-Estani, S.; Ralston, K.; Zaidel, E.J.; Forsyth, C.; Ribeiro, A.L.P.; Mendoza, I.; Falconi, M.L.; et al. WHF IASC Roadmap on Chagas Disease. Glob. Hear. 2020, 15, 26. [Google Scholar] [CrossRef]
- Hasslocher-Moreno, A.M.; Xavier, S.S.; Saraiva, R.M.; de Sousa, A.S. Indeterminate form of Chagas disease: Historical, conceptual, clinical, and prognostic aspects. Rev. Soc. Bras. Med. Trop. 2021, 54, e02542021. [Google Scholar] [CrossRef]
- Issa, V.S. The Indeterminate Form of Chagas Disease. Arq. Bras. Cardiol. 2018, 110, 111–112. [Google Scholar] [CrossRef]
- Bonney, K.M.; Luthringer, D.J.; Kim, S.A.; Garg, N.J.; Engman, D.M. Pathology and Pathogenesis of Chagas Heart Disease. Annu. Rev. Pathol. Mech. Dis. 2019, 14, 421–447. [Google Scholar] [CrossRef] [PubMed]
- Acquatella, H.; Asch, F.M.; Barbosa, M.M.; Barros, M.; Bern, C.; Cavalcante, J.L.; Correa, L.E.E.; Lima, J.; Marcus, R.; Marin-Neto, J.A.; et al. Recommendations for Multimodality Cardiac Imaging in Patients with Chagas Disease: A Report from the American Society of Echocardiography in Collaboration With the InterAmerican Association of Echocardiography (ECOSIAC) and the Cardiovascular Imaging Department of the Brazilian Society of Cardiology (DIC-SBC). J. Am. Soc. Echocardiogr. 2018, 31, 3–25. [Google Scholar]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F.; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef] [PubMed]
- Rassi, D.; Vieira, M.L.; Arruda, A.L.; Hotta, V.T.; Furtado, R.G.; Rassi, D.T.; Rassi, S. Echocardiographic parameters and survival in Chagas heart disease with severe systolic dysfunction. Arq. Bras. Cardiol. 2014, 102, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Echeverría, L.E.; Rojas, L.Z.; Villamizar, M.C.; Luengas, C.; Chaves, A.M.; Rodríguez, J.A.; Campo, R.; Clavijo, C.; Redondo, A.M.; López, L.A.; et al. Echocardiographic parameters, speckle tracking, and brain natriuretic peptide levels as indicators of progression of indeterminate stage to Chagas cardiomyopathy. Echocardiography 2020, 37, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Kalam, K.; Otahal, P.; Marwick, T.H. Prognostic implications of global LV dysfunction: A systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart Br. Card. Soc. 2014, 100, 1673–1680. [Google Scholar] [CrossRef]
- Zhang, T.; Li, J.; Cao, S. Prognostic value of left ventricular global longitudinal strain in chronic kidney disease patients: A systematic review and meta-analysis. Int. Urol. Nephrol. 2020, 52, 1747–1756. [Google Scholar] [CrossRef]
- Janwanishstaporn, S.; Cho, J.Y.; Feng, S.; Brann, A.; Seo, J.-S.; Narezkina, A.; Greenberg, B. Prognostic Value of Global Longitudinal Strain in Patients With Heart Failure With Improved Ejection Fraction. JACC Hear. Fail. 2021, 10, 27–37. [Google Scholar] [CrossRef]
- Olsen, F.J.; Pedersen, S.; Jensen, J.S.; Biering-Sørensen, T. Global longitudinal strain predicts incident atrial fibrillation and stroke occurrence after acute myocardial infarction. Medicine 2016, 95, e5338. [Google Scholar] [CrossRef]
- Nikoo, M.H.; Naeemi, R.; Moaref, A.; Attar, A. Global longitudinal strain for prediction of ventricular arrhythmia in patients with heart failure. ESC Hear. Fail. 2020, 7, 2956–2961. [Google Scholar] [CrossRef]
- Romano MM, D.; Moreira, H.T.; Marin-Neto, J.A.; Baccelli, P.E.; Alenezi, F.; Klem, I.; Maciel, B.C.; Kisslo, J.; Schmidt, A.; Velazquez, E.J. Early impairment of myocardial deformation assessed by regional speckle-tracking echocardiography in the indeterminate form of Chagas disease without fibrosis detected by cardiac magnetic resonance. PLoS Negl. Trop. Dis. 2020, 14, e0008795. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, C.A.S.; Gomes, V.A.M.; Silva, S.K.; Santos, C.R.F.; Chambela, M.C.; Madeira, F.S.; Holanda, M.T.; Brasil, P.E.A.; Sousa, A.S.; Xavier, S.S.; et al. Left Atrial and Left Ventricular Diastolic Function in Chronic Chagas Disease. J. Am. Soc. Echocardiogr. 2013, 26, 1424–1433. [Google Scholar] [CrossRef] [PubMed]
- Muka, T.; Glisic, M.; Milic, J.; Verhoog, S.; Bohlius, J.; Bramer, W.; Chowdhury, R.; Franco, O.H. A 24-step guide on how to design, conduct, and successfully publish a systematic review and meta-analysis in medical research. Eur. J. Epidemiol. 2019, 35, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef]
- García-Álvarez, A.; Sitges, M.; Regueiro, A.; Poyatos, S.; Pinazo, M.J.; Posada, E.; Bijnens, B.; Heras, M.; Gascon, J.; Sanz, G. Myocardial Deformation Analysis in Chagas Heart Disease With the Use of Speckle Tracking Echocardiography. J. Card. Fail. 2011, 17, 1028–1034. [Google Scholar] [CrossRef]
- Barbosa, M.M.; Rocha, M.O.C.; Vidigal, D.F.; de Carvalho Bicalho, C.R.; Araújo, R.D.; Palma, M.C.; De Barros, M.V.L.; Nunes, M.C.P. Early Detection of Left Ventricular Contractility Abnormalities by Two-Dimensional Speckle Tracking Strain in Chagas’ Disease. Echocardiography 2013, 31, 623–630. [Google Scholar] [CrossRef]
- Gomes, V.A.M.; Alves, G.F.; Hadlich, M.; Azevedo, C.F.; Pereira, I.M.; Santos, C.R.F.; Brasil, P.E.; Sangenis, L.H.C.; Cunha, A.B.; Xavier, S.S.; et al. Analysis of Regional Left Ventricular Strain in Patients with Chagas Disease and Normal Left Ventricular Systolic Function. J. Am. Soc. Echocardiogr. 2016, 29, 679–688. [Google Scholar] [CrossRef]
- Lima, M.S.M.; Villarraga, H.R.; Abduch, M.C.D.; Lima, M.F.; Cruz, C.B.B.V.; Bittencourt, M.S.; Voos, M.C.; Sbano, J.C.N.; Mathias, W.; Tsutsui, J.M. Comprehensive left ventricular mechanics analysis by speckle tracking echocardiography in Chagas disease. Cardiovasc. Ultrasound 2015, 14, 20. [Google Scholar] [CrossRef]
- Lima MS, M.; Voos, M.C.; Mathias, W.; Tsutsui, J.M. Indeterminate form of Chagas disease: Is left ventricular torsional mechanics a clue to subclinical myocardial abnormalities? J. Echocardiogr. 2017, 15, 6–12. [Google Scholar] [CrossRef]
- Santos Junior, O.R.; da Costa Rocha, M.O.; Rodrigues de Almeida, F.; Sales da Cunha, P.F.; Souza, S.C.S.; Saad, G.P.; Santos, T.A.D.Q.; Ferreira, A.M.; Tan, T.C.; Nunes, M.C.P. Speckle tracking echocardiographic deformation indices in Chagas and idiopathic dilated cardiomyopathy: Incremental prognostic value of longitudinal strain. PLoS ONE 2019, 14, e0221028. [Google Scholar] [CrossRef] [PubMed]
- Cianciulli, T.F.; Albarracín, G.A.; Llobera, M.N.; Prado, N.G.; Saccheri, M.C.; Vásquez, Y.M.H.; Méndez, R.J.; Beck, M.A.; Baez, K.G.; Balletti, L.R. Speckle tracking echocardiography in the indeterminate form of Chagas disease. Echocardiography 2020, 38, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Jones, E.M.; Colley, D.; Tostes, S.; Lopes, E.R.; Vnencak-Jones, C.L.; McCurley, T.L. Amplification of a Trypanosoma Cruzi DNA Sequence from Inflammatory Lesions in Human Chagasic Cardiomyopathy. Am. J. Trop. Med. Hyg. 1993, 48, 348–357. [Google Scholar] [CrossRef] [PubMed]
- Higuchi Mde, L.; De Brito, T.; Martins Reis, M.; Barbosa, A.; Bellotti, G.; Pereira-Barreto, A.C.; Pileggi, F. Correlation between Trypanosoma cruzi parasitism and myocardial inflammatory infiltrate in human chronic chagasic myocarditis: Light microscopy and immunohistochemical findings. Cardiovasc. Pathol. 1993, 2, 101–106. [Google Scholar] [CrossRef]
- Bellotti, G.; Bocchi, E.A.; de Moraes, A.V.; Higuchi, M.L.; Barbero-Marcial, M.; Sosa, E.; Esteves-Filho, A.; Kalil, R.; Weiss, R.; Jatene, A.; et al. In vivo detection of Trypanosoma cruzi antigens in hearts of patients with chronic Chagas’ heart disease. Am. Heart J. 1996, 131, 301–307. [Google Scholar] [CrossRef]
- Simões, M.V.; Pintya, A.O.; Bromberg-Marin, G.; Sarabanda, V.; Antloga, C.M.; Pazin-Filho, A.; Maciel, B.C.; Marin-Neto, J.A. Relation of regional sympathetic denervation and myocardial perfusion disturbance to wall motion impairment in Chagas’ cardiomyopathy. Am. J. Cardiol. 2000, 86, 975–981. [Google Scholar] [CrossRef]
- Marin-Neto, J.; Marzullo, P.; Marcassa, C.; Gallo, L.; Maciel, B.C.; Bellina, C.; L’Abbate, A. Myocardial perfusion abnormalities in chronic Chagas’ disease as detected by thallium-201 scintigraphy. Am. J. Cardiol. 1992, 69, 780–784. [Google Scholar] [CrossRef]
- Barizon, G.C.; Simões, M.V.; Schmidt, A.; Gadioli, L.P.; Murta Junior, L.O. Relationship between microvascular changes, autonomic denervation, and myocardial fibrosis in Chagas cardiomyopathy: Evaluation by MRI and SPECT imaging. J. Nucl. Cardiol. 2020, 27, 434–444. [Google Scholar] [CrossRef]
- Diaz, A.; Diaztagle, J.J.; Olaya, A.; Mora, G.; López-Lima, I.; Ayala, C.; Infante, G.P.P.; Galizio, N.; Manrique, F.T.; Forero, J.F.; et al. Cardiovascular Magnetic Resonance Imaging Evidence of Edema in Chronic Chagasic Cardiomyopathy. Cardiol. Res. Pr. 2019, 2019, 6420364. [Google Scholar] [CrossRef]
- Duran-Crane, A.; Rojas, C.A.; Cooper, L.T.; Medina, H.M. Cardiac magnetic resonance imaging in Chagas’ disease: A parallel with electrophysiologic studies. Int. J. Cardiovasc. Imaging 2020, 36, 2209–2219. [Google Scholar] [CrossRef]
- Lee-Felker, S.; Thomas, M.; Felker, E.; Traina, M.; Salih, M.; Hernandez, S.; Bradfield, J.; Lee, M.; Meymandi, S. Value of cardiac MRI for evaluation of chronic Chagas disease cardiomyopathy. Clin. Radiol. 2016, 71, 618.e1–618.e7. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, M.D.L.; Fukasawa, S.; De Brito, T.; Parzianello, L.C.; Bellotti, G.; Ramires, J.A.F. Different microcirculatory and interstitial matrix patterns in idiopathic dilated cardiomyopathy and Chagas’ disease: A three dimensional confocal microscopy study. Heart 1999, 82, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Caetano, L.C.; Santello, F.H.; Filipin, M.D.V.; Brazão, V.; Caetano, L.N.; Toldo, M.P.A.; Caldeira, J.C.; Prado, J.C.D. Trypanosoma cruzi: Dehydroepiandrosterone (DHEA) and immune response during the chronic phase of the experimental Chagas’ disease. Vet. Parasitol. 2009, 163, 27–32. [Google Scholar] [CrossRef]
- Pérez, A.R.; Morrot, A.; Carvalho, V.F.; de Meis, J.; Savino, W. Role of Hormonal Circuitry Upon T Cell Development in Chagas Disease: Possible Implications on T Cell Dysfunctions. Front. Endocrinol. 2018, 9, 334. [Google Scholar] [CrossRef]
- Mirea, O.; Duchenne, J.; Voigt, J.-U. Recent advances in echocardiography: Strain and strain rate imaging. F1000Research 2016, 5, 787. [Google Scholar] [CrossRef][Green Version]
- Inciardi, R.M.; Galderisi, M.; Nistri, S.; Santoro, C.; Cicoira, M.; Rossi, A. Echocardiographic advances in hypertrophic cardiomyopathy: Three-dimensional and strain imaging echocardiography. Echocardiography 2018, 35, 716–726. [Google Scholar] [CrossRef] [PubMed]
- Galderisi, M.; Esposito, R.; Schiano-Lomoriello, V.; Santoro, A.; Ippolito, R.; Schiattarella, P.; Strazzullo, P.; De Simone, G. Correlates of global area strain in native hypertensive patients: A three-dimensional speckle-tracking echocardiography study. Eur. Hear. J. Cardiovasc. Imaging 2012, 13, 730–738. [Google Scholar] [CrossRef] [PubMed]
- Kuznetsova, T.; Cauwenberghs, N.; Knez, J.; Yang, W.-Y.; Herbots, L.; D’Hooge, J.; Haddad, F.; Thijs, L.; Voigt, J.-U.; Staessen, J.A. Additive Prognostic Value of Left Ventricular Systolic Dysfunction in a Population-Based Cohort. Circ. Cardiovasc. Imaging 2016, 9, e004661. [Google Scholar] [CrossRef] [PubMed]
- Pastore, M.C.; De Carli, G.; Mandoli, G.E.; D’Ascenzi, F.; Focardi, M.; Contorni, F.; Mondillo, S.; Cameli, M. The prognostic role of speckle tracking echocardiography in clinical practice: Evidence and reference values from the literature. Hear. Fail. Rev. 2020, 26, 1371–1381. [Google Scholar] [CrossRef]
- Zegkos, T.; Parcharidou, D.; Ntelios, D.; Efthimiadis, G.; Karvounis, H. The Prognostic Implications of Two-Dimensional Speckle Tracking Echocardiography in Hypertrophic Cardiomyopathy: Current and Future Perspectives. Cardiol. Rev. 2018, 26, 130–136. [Google Scholar] [CrossRef]
- Noya-Rabelo, M.M.; Macedo, C.T.; Larocca, T.; Machado, A.; Pacheco, T.; Torreão, J.; Souza, B.S.D.F.; Soares, M.B.P.; Ribeiro-Dos-Santos, R.; Correia, L.C.L. The Presence and Extension of Myocardial Fibrosis in the Undetermined Form of Chagas’ Disease: A Study Using Magnetic Resonance. Arq. Bras. Cardiol. 2018, 110, 124–131. [Google Scholar] [CrossRef]
- Añez, N.; Carrasco, H.; Parada, H.; Crisante, G.; Rojas, A.; Guevara, P.; Borges, R.; Fuenmayor, C.; Ramirez, J.L.; Gonzalez, N.; et al. Myocardial parasite persistence in chronic chagasic patients. Am. J. Trop. Med. Hyg. 1999, 60, 726–732. [Google Scholar] [CrossRef] [PubMed]
- Andrade, Z.A.; Andrade, S.G.; Sadigursky, M.; Wenthold, R.J., Jr.; Hilbert, S.L.; Ferrans, V.J. The indeterminate phase of Chagas’ disease: Ultrastructural characterization of cardiac changes in the canine model. Am. J. Trop. Med. Hyg. 1997, 57, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Marin-Neto, J.A.; Almeida Filho, O.C.; Pazin-Filho, A.; Maciel, B.C. [Indeterminate form of Chagas’ disease. Proposal of new diagnostic criteria and perspectives for early treatment of cardiomyopathy]. Arq. Bras. Cardiol. 2002, 79, 623–627. [Google Scholar] [PubMed]
- Pazin-Filho, A.; Romano, M.; Almeida-Filho, O.; Furuta, M.; Viviani, L.; Schmidt, A.; Marin-Neto, J.; Maciel, B. Minor segmental wall motion abnormalities detected in patients with Chagas’ disease have adverse prognostic implications. Braz. J. Med Biol. Res. 2006, 39, 483–487. [Google Scholar] [CrossRef]
| Studies | Publication Year | Country | Total Patients | CCM Patients | Mean Age of CCM Patients | CCM Men (%) | IF Patients | Mean Age of IF Patients | IF Men (%) | Healthy Controls | Mean Age of Healthy Controls | Controls Men (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| García-Álvarez A et al. | 2011 | Spain | 98 | 22 | 42.7 ± 9.6 | 45 | 32 | 36.8 ± 10.8 | 34 | 44 | 34 ± 8.5 | 41 |
| Nascimento CA et al. | 2013 | Brazil | 184 | 83 | 48 ± 8.7 | 53 | 69 | 45 ± 9 | 48 | 32 | 44 ± 7 | 44 |
| Barbosa M et al. | 2013 | Brazil | 116 | - | - | - | 78 | 44.7 ± 8.6 | 46 | 38 | 44 ± 9.2 | 58 |
| Gomes V et al. | 2016 | Brazil | 168 | 42 | 47 ± 8 | 38 | 83 | 44 ± 9 | 46 | 43 | 44 ± 7 | 49 |
| Lima MS 2 et al. | 2016 | Brazil | 42 | 13 | 53 ± 11.6 | 31 | 8 | 57 ± 7.5 | 13 | 21 | 50 ± 6.4 | 33 |
| Lima MS et al. | 2016 | Brazil | 105 | 39 | 55 ± 11 | 48.3 | 8 | 56 ± 7 | 12 | 58 | 37 ± 12 | 43 |
| Santos Junior et al. | 2019 | Brazil | 81 | 81 | 57 ± 11 | 59 | - | - | - | - | - | - |
| Echeverría LE et al. | 2020 | Colombia | 273 | 177 | 59 ± 11 | 55.37 | 96 | 49 ± 11 | 25.19 | - | - | - |
| Romano MM et al. | 2020 | Brazil | 65 | 20 | 53 ± 12 | 30 | 25 | 55 ± 12 | 60 | 20 | 48 ± 10 | 55 |
| Cianciulli TF et al. | 2020 | Argentina | 90 | - | - | - | 45 | 59 ± 9.9 | 41.2 | 45 | 57 ± 18.4 | 35.6 |
| Variables | CCM | IF | Healthy Controls | CCM vs. IF | IF vs. Controls |
|---|---|---|---|---|---|
| Mean age | 50.8 (43.8, 57.8) | 50.4 (45, 56) | 44.3 (38.5, 50.2) | 0.312 (−0.02, 0.64. I2 = 72%) | 0.391 (0.06, 0.72. I2= 72%) |
| Males proportion (%) | 49 (42, 56) | 39 (31, 48) | 44 (39, 50) | p-value = 0.213 | p-value = 0.098 |
| LVEF (%) | 58.4 (51.5, 65.4) | 63.3 (58.4, 68.2) | 64.8 (60.6, 68.9) | −1.169 (−1.88, −0.46. I2 = 83%) | 0.063 (−0.19, 0.32. I2 = 0%) |
| LAVI (ml/m2) | 33.3 (27.6, 38.8) | - | - | - | - |
| LAD (mm) | 35.8 (32.5, 39.2) | 34.5 (30.6, 38.5) | 34.6 (31.2, 37.9) | 0.608 (0.05, 1.17. I2 = 43%) | 0.115 (−0.29, 0.52. I2 = 9%) |
| LVD (mm) | 53.3 (50.8, 55.9) | 48.2 (43.9, 52.6) | 49.2 (45.9, 52.4) | 1.559 (0.45, 2.67. I2 = 92%) | 0.022 (−0.28, 0.32. I 2= 21%) |
| LVS (mm) | 34.7 (30.4, 38.9) | 30.4 (25.9, 34.8) | 30.3 (27.8, 32.8) | 1.106 (0.37, 1.84. I2 = 84%) | −0.030 (−0.39, 0.33. I2 = 42%) |
| E/e’ ratio | 8.2 (5.6, 10.9) | 7.1 (3.6, 10.5) | 6.6 (4.5, 8.7) | - | - |
| GLS (%) | −15.9 (−18.1, −13.7) | −19.9 (−21.2, −18.7) | −20.1 (−20.8, −19.3) | 1.253 (0.53, 1.98. I2 = 94%) | 0.197 (−0.19, 0.59. I2 = 80%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Ochoa, S.A.; Rojas, L.Z.; Hernández-Vargas, J.A.; Largo, J.; Muka, T.; Echeverría, L.E. Longitudinal Speckle Tracking Strain Abnormalities in Chagas Disease: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 769. https://doi.org/10.3390/jcm11030769
Gómez-Ochoa SA, Rojas LZ, Hernández-Vargas JA, Largo J, Muka T, Echeverría LE. Longitudinal Speckle Tracking Strain Abnormalities in Chagas Disease: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(3):769. https://doi.org/10.3390/jcm11030769
Chicago/Turabian StyleGómez-Ochoa, Sergio Alejandro, Lyda Z. Rojas, Juliana Alexandra Hernández-Vargas, Jorge Largo, Taulant Muka, and Luis E. Echeverría. 2022. "Longitudinal Speckle Tracking Strain Abnormalities in Chagas Disease: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 3: 769. https://doi.org/10.3390/jcm11030769
APA StyleGómez-Ochoa, S. A., Rojas, L. Z., Hernández-Vargas, J. A., Largo, J., Muka, T., & Echeverría, L. E. (2022). Longitudinal Speckle Tracking Strain Abnormalities in Chagas Disease: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 11(3), 769. https://doi.org/10.3390/jcm11030769






