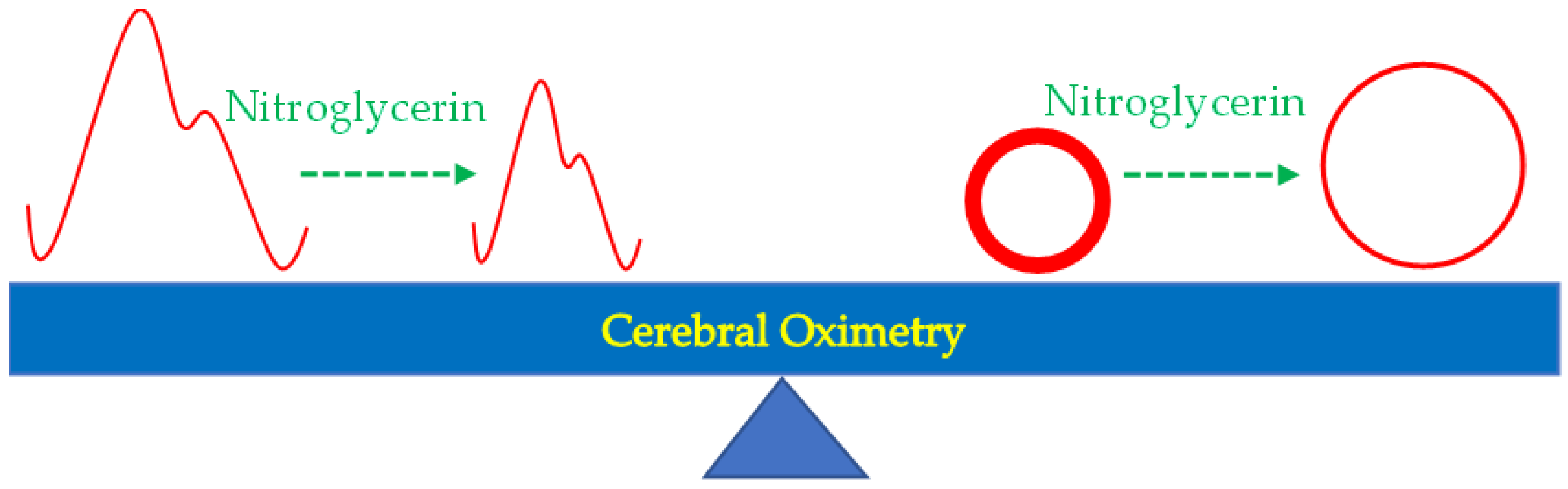
Cerebral Oximetry-Monitored Nitroglycerin Infusion and Tissue Perfusion during Rewarming of Cardiopulmonary Bypass in Cardiac Surgery: A Prospective Randomized Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Anesthetic Procedure and Cardiopulmonary Bypass
2.3. Treatment Protocol
2.4. Data Acquisition
2.5. Data Analysis
3. Results
3.1. Participant Recruitment
3.2. General Characteristics of Participants
3.3. Perioperative Outcomes
3.4. Perioperative Parameters
4. Discussion
4.1. Main Findings
4.2. Personalized Cerebral Oximetry Monitoring during Hypothermic CPB
4.3. Hypoperfusion during Hypothermic CPB and Nitroglycerin Infusion for Rewarming
4.4. Heparin Reversal and Nitroglycerin Infusion
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Laffey, J.G.; Boylan, J.F.; Cheng, D.C. The systemic inflammatory response to cardiac surgery: Implications for the anesthesiologist. Anesthesiology 2002, 97, 215–252. [Google Scholar] [PubMed]
- Piquette, D.; Deschamps, A.; Belisle, S.; Pellerin, M.; Levesque, S.; Tardif, J.C.; Denault, A.Y. Effect of intravenous nitroglycerin on cerebral saturation in high-risk cardiac surgery. Can. J. Anaesth. 2007, 54, 718–727. [Google Scholar] [CrossRef] [PubMed][Green Version]
- O’Connor, E.; Fraser, J.F. The interpretation of perioperative lactate abnormalities in patients undergoing cardiac surgery. Anaesth. Intensive Care 2012, 40, 598–603. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.C.; Hsu, C.H.; Huang, G.S.; Lu, C.C.; Wu, Z.F.; Tsai, Y.T.; Lin, C.Y.; Lin, Y.C.; Tsai, C.S.; Lin, T.C. Extreme hyperlactatemia after heart transplantation: One center’s experience. Transpl. Proc. 2015, 47, 1945–1948. [Google Scholar] [CrossRef]
- Hajjar, L.A.; Almeida, J.P.; Fukushima, J.T.; Rhodes, A.; Vincent, J.L.; Osawa, E.A.; Galas, F.R. High lactate levels are predictors of major complications after cardiac surgery. J. Thorac. Cardiovasc. Surg. 2013, 146, 455–460. [Google Scholar] [CrossRef]
- Lima, A.; van Genderen, M.E.; van Bommel, J.; Klijn, E.; Jansem, T.; Bakker, J. Nitroglycerin reverts clinical manifestations of poor peripheral perfusion in patients with circulatory shock. Crit. Care 2014, 18, R126. [Google Scholar] [CrossRef]
- den Uil, C.A.; Caliskan, K.; Lagrand, W.K.; van der Ent, M.; Jewbali, L.S.; van Kuijk, J.P.; Spronk, P.E.; Simoons, M.L. Dose-dependent benefit of nitroglycerin on microcirculation of patients with severe heart failure. Intensive Care Med. 2009, 35, 1893–1899. [Google Scholar] [CrossRef]
- Masoumi, G.; Pour, E.H.; Sadeghpour, A.; Ziayeefard, M.; Alavi, M.; Anbardan, S.J.; Shirani, S. Effect of different dosages of nitroglycerin infusion on arterial blood gas tensions in patients undergoing on- pump coronary artery bypass graft surgery. J. Res. Med. Sci. 2012, 17, 123–127. [Google Scholar]
- Tai, Y.H.; Chang, K.Y.; Liao, S.W.; Chung, K.C.; Shih, C.C.; Ho, S.T.; Lu, C.C.; Tsou, M.Y. Intravenous loading of nitroglycerin during rewarming of cardiopulmonary bypass improves metabolic homeostasis in cardiac surgery: A retrospective analysis. J. Anesth. 2016, 30, 779–788. [Google Scholar] [CrossRef]
- Ono, M.; Brady, K.; Easley, R.B.; Brown, C.; Kraut, M.; Gottesman, R.F.; Hogue, C.W., Jr. Duration and magnitude of blood pressure below cerebral autoregulation threshold during cardiopulmonary bypass is associated with major morbidity and operative mortality. J. Thorac. Cardiovasc. Surg. 2014, 147, 483–489. [Google Scholar] [CrossRef]
- Juliana, N.; Abu Yazit, N.A.; Kadiman, S.; Muhammad Hafidz, K.; Azmani, S.; Mohd Fahmi Teng, N.I.; Das, S. Intraoperative cerebral oximetry in open heart surgeries reduced postoperative complications: A retrospective study. PLoS ONE 2021, 16, e0251157. [Google Scholar] [CrossRef] [PubMed]
- Van Noord, B.A.; Stalker, C.L.; Roffey, P.; Thangathurai, D. The use of regional cerebral oximetry monitoring during controlled hypotension: A case series. J. Clin. Monit. Comput. 2014, 28, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.H.; Hsu, Y.C.; Huang, G.S.; Lu, C.C.; Ho, S.T.; Liaw, W.J.; Tsai, Y.T.; Lin, C.Y.; Tsai, C.S.; Lin, T.C. Isoflurane compared with fentanyl-midazolam-based anesthesia in patients undergoing heart transplantation: A retrospective cohort study. Medicine 2016, 95, e4699. [Google Scholar] [CrossRef]
- Demers, P.; Elkouri, S.; Martineau, R.; Couturier, A.; Cartier, R. Outcome with high blood lactate levels during cardiopulmonary bypass in adult cardiac operation. Ann. Thorac. Surg. 2000, 70, 2082–2086. [Google Scholar] [CrossRef]
- Ono, M.; Joshi, B.; Brady, K.; Easley, R.B.; Zheng, Y.; Brown, C.; Baumgartner, W.; Hogue, C.W. Risks for impaired cerebral autoregulation during cardiopulmonary bypass and postoperative stroke. Br. J. Anaesth. 2012, 109, 391–398. [Google Scholar] [CrossRef]
- Joshi, B.; Ono, M.; Brown, C.; Brady, K.; Easley, R.B.; Yenokyan, G.; Gottesman, R.F.; Hogue, C.W. Predicting the limits of cerebral autoregulation during cardiopulmonary bypass. Anesth. Analg. 2012, 114, 503–510. [Google Scholar] [CrossRef]
- Brady, K.; Joshi, B.; Zweifel, C.; Smielewski, P.; Czosnyka, M.; Easley, R.B.; Hogue, C.W., Jr. Real-time continuous monitoring of cerebral blood flow autoregulation using near-infrared spectroscopy in patients undergoing cardiopulmonary bypass. Stroke 2010, 41, 1951–1956. [Google Scholar] [CrossRef]
- Deschamps, A.; Lambert, J.; Couture, P.; Rochon, A.; Lebon, J.-S.; Ayoub, C.; Cogan, J.; Denault, A. Reversal of decreases in cerebral saturation in high-risk cardiac surgery. J. Cardiothorac. Vasc. Anesth. 2013, 27, 1260–1266. [Google Scholar] [CrossRef]
- Slater, J.P.; Guarino, T.; Stack, J.; Vinod, K.; Bustami, R.T.; Brown, J.M., III; Rodriguez, A.L.; Magovern, C.J.; Zaubler, T.; Freundlich, K.; et al. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann. Thorac. Surg. 2009, 87, 36–45. [Google Scholar] [CrossRef]
- Jo, Y.Y.; Shim, J.K.; Soh, S.; Suh, S.; Kwak, Y.L. Association between cerebral oxygen saturation with outcome in cardiac surgery: Brain as an index organ. J. Clin. Med. 2020, 9, 840. [Google Scholar] [CrossRef] [PubMed]
- Mullane, D.; Lenihan, M.; Hanley, C.; Wall, T.; Bukowska, I.; Griffin, M.; Flood, G. Efficacy of Glyceryl trinitrate (GTN) to facilitate the rewarming process during cardiopulmonary bypass. J. Cardiothorac. Surg. 2020, 15, 214. [Google Scholar] [CrossRef] [PubMed]
- Finley, A.; Greenberg, C. Review article: Heparin sensitivity and resistance: Management during cardiopulmonary bypass. Anesth. Analg. 2013, 116, 1210–1222. [Google Scholar] [CrossRef] [PubMed]
- Spronk, P.E.; Ince, C.; Gardien, M.J.; Mathura, K.R.; Oudemans-van Straaten, H.M.; Zandstra, D.F. Nitroglycerin in septic shock after intravascular volume resuscitation. Lancet 2002, 360, 1395–1396. [Google Scholar] [CrossRef]
- Boerma, E.C.; Koopmans, M.; Konijn, A.; Kaiferova, K.; Bakker, A.J.; van Roon, E.N.; Buter, H.; Bruins, N.; Egbers, P.H.; Gerritsen, R.T.; et al. Effects of nitroglycerin on sublingual microcirculatory blood flow in patients with severe sepsis/septic shock after a strict resuscitation protocol: A double-blind randomized placebo controlled trial. Crit. Care Med. 2010, 38, 93–100. [Google Scholar] [CrossRef]

| Nitroglycerin 1–5 mcg/kg/min (n = 32) | Nitroglycerin 0–0.1 mcg/kg/min (n = 31) | p-Value | |
|---|---|---|---|
| Male/female, n | 22/10 | 21/10 | 0.999 a |
| Age, year | 62.5 ± 12.2 | 59.3 ± 13.2 | 0.389 b |
| Weight, kg | 63.5 ± 11.9 | 68.4 ± 17.6 | 0.271 b |
| Height, cm | 162.9 ± 7.9 | 164.7 ± 9.7 | 0.413 b |
| Body mass index, kg/m2 | 23.8 ± 3.4 | 24.9 ± 4.7 | 0.375 b |
| Nitroglycerin infusion, mg | |||
| Before cessation of CPB | 3.5 ± 1.9 | 0.2 ± 0.3 | <0.001 b |
| Total, until the end of surgery | 9.8 ± 8.3 | 2.1 ± 4.0 | <0.001 b |
| Duration of general anesthesia, min | 348.9 ± 64.7 | 347.3 ± 87.9 | 0.736 b |
| Duration of operation, min | 291.7 ± 63.9 | 289.6 ± 82.5 | 0.680 b |
| Duration of CPB, min | 133.3 ± 48.4 | 123.3 ± 28.4 | 0.874 b |
| Duration of aortic clamping, min | 86.8 ± 36.0 | 78.6 ± 22.2 | 0.523 b |
| Lowest temperature during CPB, °C | 27.2 ± 1.2 | 27.6 ± 2.3 | 0.951 b |
| Temperature at start of rewarming, °C | 28.8 ± 1.3 | 27.6 ± 2.3 | 0.563 b |
| Temperature at end of rewarming, °C | 36.4 ± 0.8 | 36.4 ± 0.9 | 0.700 b |
| Duration of rewarming, min | 30.5 ± 7.9 | 34.2 ± 8.5 | 0.057 b |
| Rate of rewarming, °C/min | 0.3 ± 0.1 | 0.2 ± 0.1 | 0.314 b |
| Fentanyl, mcg/kg | 6.5 ± 3.2 | 4.5 ± 2.2 | 0.007 b |
| Packed red blood cell, unit | 4.1 ± 1.6 | 5.0 ± 3.5 | 0.361 b |
| Single donor platelet, unit | 1.2 ± 0.5 | 1.2 ± 0.5 | 0.819 b |
| Fresh frozen plasma, unit | 8.1 ± 0.8 | 8.1 ± 1.7 | 0.649 b |
| Left ventricular ejection fraction, % | 57.8 ± 16.1 | 53.3 ± 14.6 | 0.166 b |
| Coronary artery graft in bypass surgery, n | 0.9 ± 1.3 | 0.9 ± 1.3 | 0.847 b |
| Valvular heart disease, n | 24 | 22 | 0.782 a |
| Hypertension with medication, n | 19 | 18 | 0.916 a |
| Diabetes mellitus, n | 8 | 9 | 0.782 a |
| Perioperative use of insulin, n | 3 | 6 | 0.302 a |
| Nitroglycerin 1–5 mcg/kg/min (n = 32) | Nitroglycerin 0–0.1 mcg/kg/min (n = 31) | p-Value | |
|---|---|---|---|
| Plasma lactate level, mmol/L | |||
| Before incision | 1.1 ± 0.5 | 1.0 ± 0.4 | 0.921 b |
| Before start of CPB | 1.4 ± 0.7 | 1.6 ± 0.7 | 0.315 b |
| Release of aortic clamp | 3.1 ± 1.2 | 2.6 ± 1.0 | 0.081 b |
| After protamine administration | 3.3 ± 1.2 | 3.0 ± 1.1 | 0.496 b |
| Upon arrival at ICU | 3.4 ± 1.6 | 3.2 ± 1.5 | 0.492 b |
| Peak level in ICU | 5.0 ± 3.0 | 4.1 ± 2.2 | 0.189 b |
| Time to peak level in ICU, hour | 5.1 ± 5.6 | 5.0 ± 5.8 | 0.889 b |
| Plasma lactate level ≥4.0 mmol/L, n | |||
| Before incision | 0 | 0 | - |
| Before start of CPB | 0 | 0 | - |
| Release of aortic clamp | 7 | 4 | 0.509 a |
| After protamine administration | 8 | 6 | 0.763 a |
| Upon arrival at ICU | 10 | 8 | 0.782 a |
| Plasma bicarbonate level, mmol/L | |||
| Before incision | 25.9 ± 2.8 | 26.3 ± 2.2 | 0.842 b |
| Before start of CPB | 23.9 ± 3.3 | 23.8 ± 2.9 | 0.864 b |
| Release of aortic clamp | 22.8 ± 1.8 | 23.2 ± 1.6 | 0.441 b |
| After protamine administration | 24.0 ± 2.2 | 24.3 ± 1.9 | 0.527 b |
| Upon arrival at ICU | 26.3 ± 2.9 | 25.1 ± 3.4 | 0.137 b |
| Plasma base excess level, mmol/L | |||
| Before incision | 2.9 ± 2.4 | 2.4 ± 2.1 | 0.153 b |
| Before start of CPB | −1.3 ± 4.4 | −0.7 ± 3.7 | 0.564 b |
| Release of aortic clamp | −1.4 ± 1.9 | −1.2 ± 1.8 | 0.869 b |
| After protamine administration | −0.3 ± 1.9 | 0.4 ± 2.0 | 0.263 b |
| Upon arrival of ICU | 1.5 ± 3.1 | 0.2 ± 3.0 | 0.052 b |
| Plasma glucose level, mg/dL | |||
| Before incision | 139.4 ± 47.7 | 124.2 ± 32.0 | 0.248 b |
| Before start of CPB | 179.2 ± 62.3 | 165.7 ± 46.2 | 0.583 b |
| Release of aortic clamp | 174.5 ± 49.5 | 165.0 ± 29.3 | 0.487 b |
| After protamine administration | 196.9 ± 53.8 | 205.7 ± 41.1 | 0.574 b |
| Upon arrival at ICU | 206.4 ± 55.7 | 214.8 ± 46.3 | 0.514 b |
| Hematocrit, % | |||
| Before incision | 38.4 ± 5.9 | 38.9 ± 5.2 | 0.853 b |
| Before start of CPB | 28.4 ± 8.3 | 32.4 ± 8.7 | 0.036 b |
| Release of aortic clamp | 23.2 ± 2.5 | 23.5 ± 4.0 | 0.994 b |
| After protamine administration | 27.7 ± 2.6 | 29.0 ± 3.7 | 0.067 b |
| Upon arrival at ICU | 30.8 ± 3.9 | 31.1 ± 4.2 | 0.918 b |
| Activated clotting time | |||
| Before incision, sec | 158.9 ± 19.8 | 153.1 ± 18.1 | 0.350 b |
| After protamine administration, sec | 144.2 ± 15.9 | 138.2 ± 15.3 | 0.212 b |
| Serum creatinine level, mg/dL | |||
| Preoperative | 1.0 ± 0.3 | 1.0 ± 0.6 | 0.728 b |
| Postoperative, upon arrival at ICU | 0.9 ± 0.2 | 1.0 ± 0.5 | 0.728 b |
| Postoperative, the next day in ICU | 1.1 ± 0.4 | 1.2 ± 0.6 | 0.934 b |
| Intraoperative total furosemide, mg/kg | 1.1 ± 0.3 | 1.2 ± 0.6 | 0.772 b |
| Urine output during CPB, mL/kg/h | 5.9 ± 3.4 | 4.6 ± 3.0 | 0.099 b |
| Urine output within 8 h after surgery, mL/kg/h | 6.3 ± 3.8 | 5.0 ± 2.4 | 0.157 b |
| Postoperative dopamine, mcg/kg/min | 3.7 ± 1.8 | 4.7 ± 2.0 | 0.053 b |
| Postoperative dobutamine, mcg/kg/min | 0.7 ± 1.7 | 1.4 ± 2.6 | 0.406 b |
| Time to extubation since arrival at ICU, hour | 43.6 ± 33.7 | 45.8 ± 34.8 | 0.816 b |
| Length of ICU stay, day | 4.1 ± 1.8 | 4.0 ± 2.0 | 0.665 b |
| Length of hospital stay, day | 15.6 ± 9.0 | 14.6 ± 7.4 | 0.745 b |
| Postoperative events | |||
| Resternotomy for bleeding, n | 1 | 0 | 0.508 a |
| Mediastinitis with septic shock, n | 1 | 0 | 0.508 a |
| Pneumonia, n | 0 | 1 | 0.492 a |
| Massive hemothorax | 0 | 1 | 0.492 a |
| Mortality in 30 days, n | 1 | 0 | 0.508 a |
| Nitroglycerin 1–5 mcg/kg/min (n = 32) | Nitroglycerin 0–0.1 mcg/kg/min (n = 31) | p-Value | |
|---|---|---|---|
| Cardiac index, L/min/m2 | |||
| Before start of CPB | 3.0 ± 1.3 | 2.8 ± 1.1 | 0.755 b |
| Cessation of CPB | 2.6 ± 1.0 | 2.7 ± 0.6 | 0.411 b |
| After protamine administration | 3.2 ± 1.0 | 3.1 ± 0.7 | 0.860 b |
| Upon arrival at ICU | 3.3 ± 0.9 | 3.3 ± 1.3 | 0.540 b |
| PaO2/FiO2 ratio | |||
| Before start of CPB | 420.3 ± 75.6 | 356.1 ± 90.0 | 0.010 b |
| Release of aortic clamp | 322.0 ± 93.2 | 317.7 ± 102.4 | 0.694 b |
| After protamine administration | 309.1 ± 106.0 | 311.4 ± 126.6 | 0.929 b |
| Upon arrival at ICU | 220.1 ± 126.0 | 194.5 ± 92.4 | 0.406 b |
| Cerebral oximetry | |||
| Before start of CPB | |||
| Left | 74.4 ± 4.8 | 76.8 ± 6.9 | 0.118 b |
| Right | 74.9 ± 4.6 | 77.9 ± 6.0 | 0.025 b |
| Beginning rewarming | |||
| Left | 68.0 ± 5.7 | 68.4 ± 7.8 | 0.968 b |
| Right | 67.9 ± 7.2 | 69.5 ± 8.3 | 0.476 b |
| Rewarming to 32 °C | |||
| Left | 67.1 ± 5.6 | 65.6 ± 6.8 | 0.315 b |
| Right | 67.2 ± 6.7 | 66.9 ± 7.9 | 0.813 b |
| 5 min after rewarming to 32 °C | |||
| Left | 67.4 ± 5.1 | 65.5 ± 6.9 | 0.260 b |
| Right | 67.9 ± 5.8 | 66.9 ± 7.5 | 0.457 b |
| Release of aortic clamp | |||
| Left | 67.4 ± 5.6 | 66.8 ± 5.8 | 0.423 b |
| Right | 68.2 ± 6.1 | 67.9 ± 6.7 | 0.804 b |
| Cessation of CPB | |||
| Left | 71.1 ± 4.0 | 69.8 ± 5.8 | 0.451 b |
| Right | 71.4 ± 4.9 | 70.0 ± 6.6 | 0.471 b |
| After protamine administration | |||
| Left | 74.9 ± 4.3 | 72.1 ± 6.9 | 0.173 b |
| Right | 75.0 ± 4.7 | 74.3 ± 7.3 | 0.823 b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, J.-L.; Hsu, Y.-C.; Huang, G.-S.; Lin, C.-Y.; Ke, H.-Y.; Hsu, P.-S.; Chung, C.-H.; Tsai, C.-S.; Lin, T.-C. Cerebral Oximetry-Monitored Nitroglycerin Infusion and Tissue Perfusion during Rewarming of Cardiopulmonary Bypass in Cardiac Surgery: A Prospective Randomized Trial. J. Clin. Med. 2022, 11, 712. https://doi.org/10.3390/jcm11030712
Chen J-L, Hsu Y-C, Huang G-S, Lin C-Y, Ke H-Y, Hsu P-S, Chung C-H, Tsai C-S, Lin T-C. Cerebral Oximetry-Monitored Nitroglycerin Infusion and Tissue Perfusion during Rewarming of Cardiopulmonary Bypass in Cardiac Surgery: A Prospective Randomized Trial. Journal of Clinical Medicine. 2022; 11(3):712. https://doi.org/10.3390/jcm11030712
Chicago/Turabian StyleChen, Jia-Lin, Yung-Chi Hsu, Go-Shine Huang, Chih-Yuan Lin, Hung-Yen Ke, Po-Shun Hsu, Chi-Hsiang Chung, Chien-Sung Tsai, and Tso-Chou Lin. 2022. "Cerebral Oximetry-Monitored Nitroglycerin Infusion and Tissue Perfusion during Rewarming of Cardiopulmonary Bypass in Cardiac Surgery: A Prospective Randomized Trial" Journal of Clinical Medicine 11, no. 3: 712. https://doi.org/10.3390/jcm11030712
APA StyleChen, J.-L., Hsu, Y.-C., Huang, G.-S., Lin, C.-Y., Ke, H.-Y., Hsu, P.-S., Chung, C.-H., Tsai, C.-S., & Lin, T.-C. (2022). Cerebral Oximetry-Monitored Nitroglycerin Infusion and Tissue Perfusion during Rewarming of Cardiopulmonary Bypass in Cardiac Surgery: A Prospective Randomized Trial. Journal of Clinical Medicine, 11(3), 712. https://doi.org/10.3390/jcm11030712






