In-Hospital and One-Year Outcomes of Patients after Early and Late Resuscitated Cardiac Arrest Complicating Acute Myocardial Infarction—Data from a Nationwide Database
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Definitions
2.3. Statistical Analysis
3. Results
3.1. Study Population
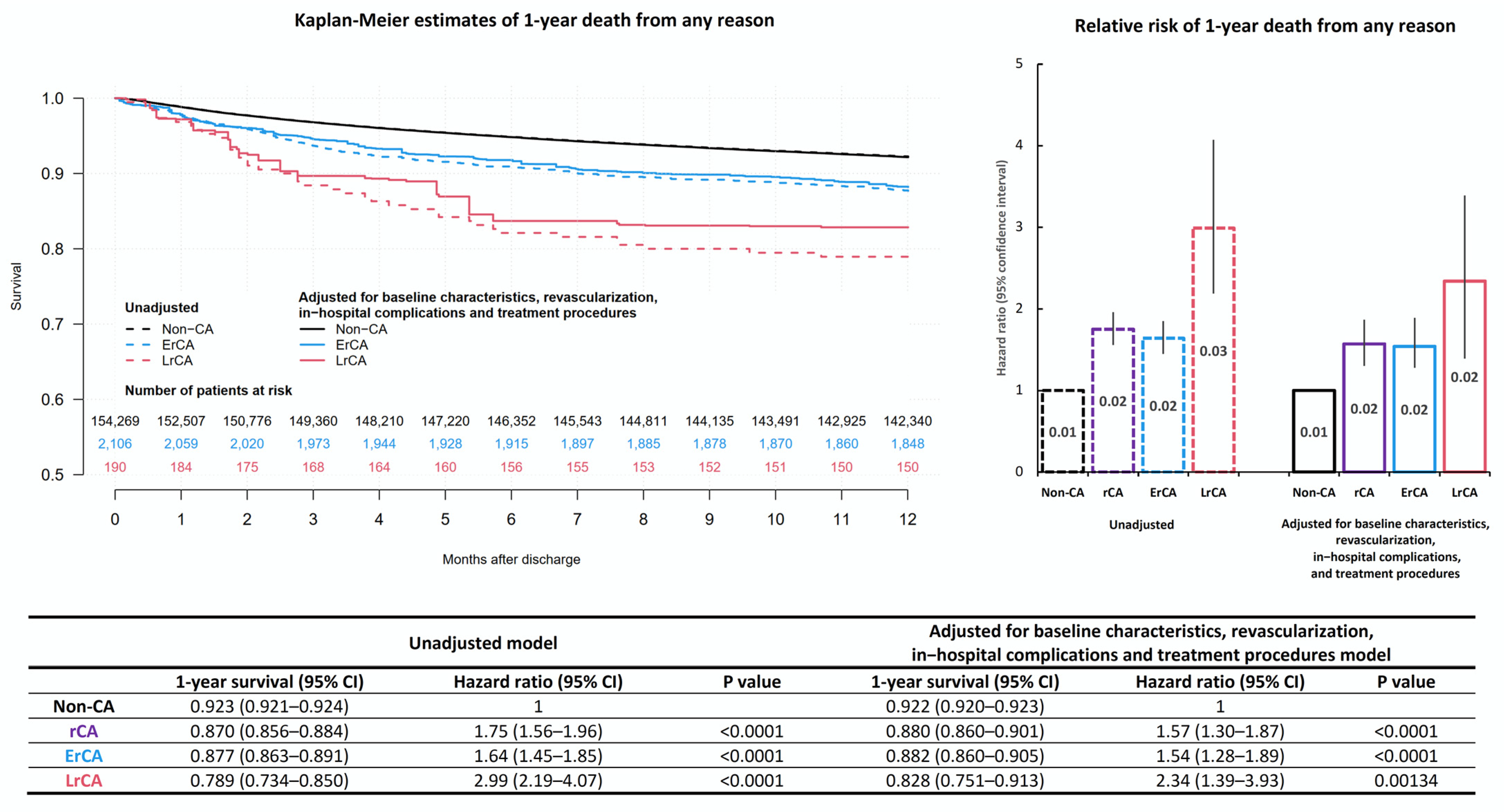
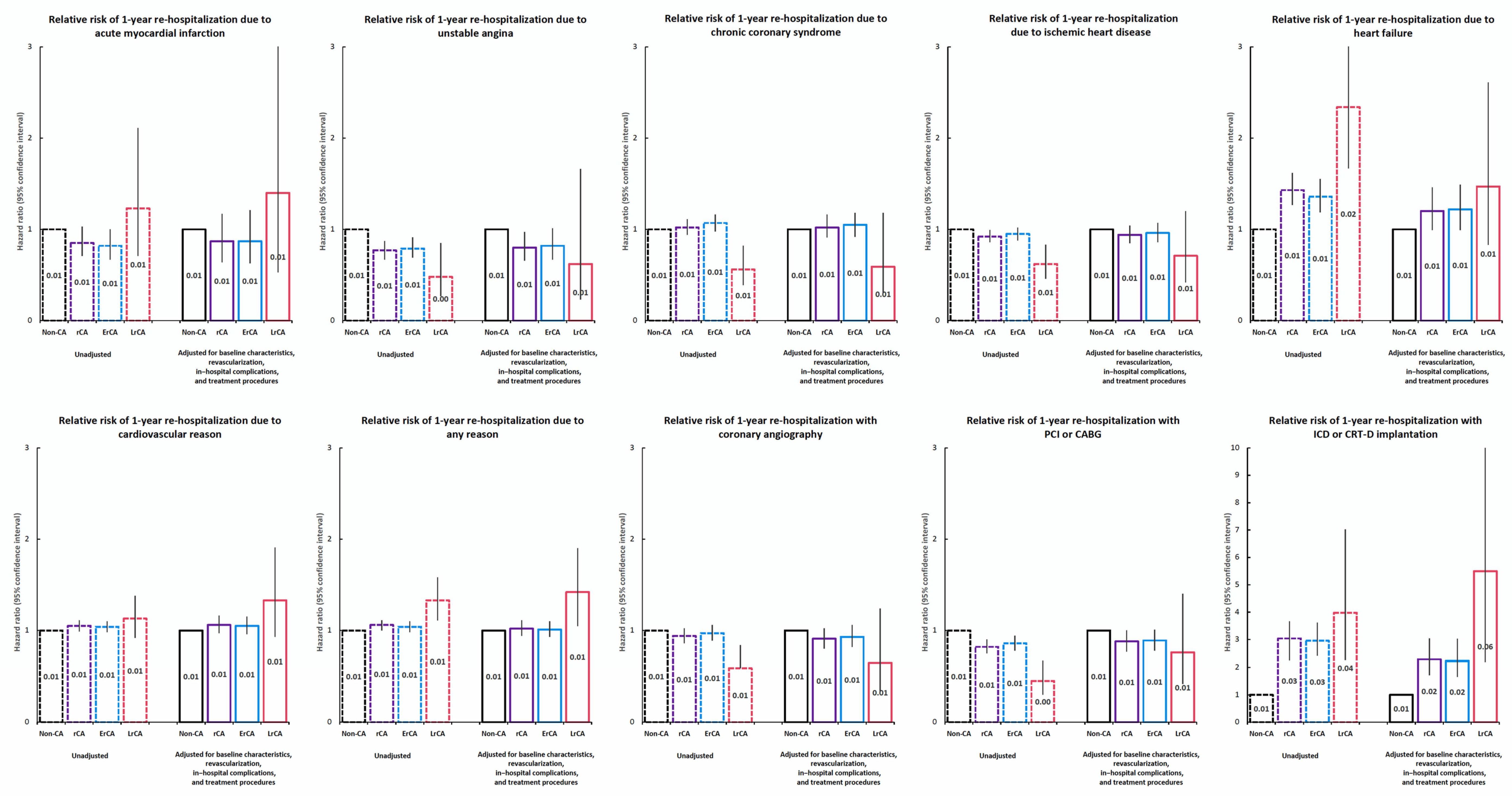
3.2. In-Hospital and One-Year Observation Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Widimský, P. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poloński, L.; Gasior, M.; Gierlotka, M.; Kalarus, Z.; Cieśliński, A.; Dubiel, J.S.; Opolski, G. Polish Registry of Acute Coronary Syndromes (PL-ACS). Characteristics, treatments and outcomes of patients with acute coronary syndromes in Poland. Kardiol. Pol. 2007, 65, 861–872. [Google Scholar] [PubMed]
- Nadolny, K.; Zyśko, D.; Obremska, M.; Wierzbik-Strońska, M.; Ładny, J.R.; Podgorski, M.; Gałązkowski, R. Analysis of out-of-hospital cardiac arrest in Poland in a 1-year period: Data from the POL-OHCA registry. Kardiol. Pol. 2020, 78, 404–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kowalik, R.J.; Fojt, A.; Ozierański, K.; Peller, M.; Andruszkiewicz, P.; Banaszewski, M.; Opolski, G. Results of targeted temperature management of patients after sudden out-of-hospital cardiac arrest: A comparison between intensive general and cardiac care units. Kardiol. Pol. 2020, 78, 30–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piccini, J.P.; Zhang, M.; Pieper, K.; Solomon, S.D.; Al-Khatib, S.M.; Van de Werf, F.; Pfeffer, M.A.; McMurray, J.J.; Califf, R.M.; Velazquez, E.J. Predictors of sudden cardiac death change with time after myocardial infarction: Results from the VALIANT trial. Eur. Heart J. 2010, 31, 211–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wojtyniak, B.; Gierlotka, M.; Opolski, G.; Rabczenko, D.; Ozierański, K.; Gąsior, M.; Zdrojewski, T. Observed and relative survival and 5-year outcomes of patients discharged after acute myocardial infarction: The nationwide AMI-PL database. Kardiol. Pol. 2020, 78, 990–998. [Google Scholar] [CrossRef] [PubMed]
- Gorenek, B. Blomstrom Lundqvist C, European Heart Rhythm Association, Acute Cardiovascular Care Association, European Association of Percutaneous Cardiovascular Interventions. Cardiac arrhythmias in acute coronary syndromes: Position paper from the joint EHRA, ACCA, and EAPCI task force. Europace 2014, 16, 1655–1673. [Google Scholar] [PubMed]
- Tymińska, A.; Kapłon-Cieślicka, A.; Ozierański, K.; Budnik, M.; Wancerz, A.; Sypień, P.; Filipiak, K.J. Association of galectin-3 and soluble ST2 with in-hospital and 1-year outcomes in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. Pol. Arch. Intern. Med. 2019, 129, 770–780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alahmar, A.E.; Nelson, C.P.; Snell, K.I.; Yuyun, M.F.; Musameh, M.D.; Timmis, A.; Samani, N.J. Resuscitated cardiac arrest and prognosis following myocardial infarction. Heart 2014, 100, 1125–1132. [Google Scholar] [CrossRef] [PubMed]
- Gierlotka, M.; Gasior, M.; Poloński, L.; Piekarski, M.; Kamiński, M. Projekt, załozenia metodyczne oraz logistyka Ogólnopolskiego Rejestru Ostrych Zespołów Wieńcowych (PL-ACS) [Project, logistics and methodology of the National Registry of Acute Coronary Syndrome (PL-ACS)]. Kardiol. Pol. 2005, 62 (Suppl. 1), I13–I21. [Google Scholar] [PubMed]
- Volpi, A.; Cavalli, A.; Santoro, L.; Negri, E.; GISSI-2 Investigators. Incidence and prognosis of early primary ventricular fibrillation in acute myocardial infarction—Results of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI-2) database. Am. J. Cardiol. 1998, 82, 265–271. [Google Scholar] [CrossRef]
- Bougouin, W.; Marjon, E.; Puymirat, E.; Defaye, P.; Celermajer, D.S.; Le Heuzey, J.Y.; FAST-MI Registry Investigators. Incidence of sudden cardiac death after ventricular fibrillation complicating acute myocardial infarction: A 5—years cause-of-death anlysis of the FAST-AMI 2005 registry. Eur. Heart J. 2014, 35, 116–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nair, S.U.; Lundbye, J.B. The use of hypothermia therapy in cardiac arrest survivors. Ther. Hypothermia Temp. Manag. 2011, 1, 9–21. [Google Scholar] [CrossRef]
- Podolecki, T.S.; Lenarczyk, R.K.; Kowalczyk, J.P.; Jedrzejczyk-Patej, E.K.; Chodor, P.K.; Mazurek, M.H.; Kalarus, Z.F. Risk stratification for complex ventricular arrhythmia complicating ST-segment elevation myocardial infarction. Coron. Artery Dis. 2018, 29, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Piccini, J.P.; Berger, J.S.; Brown, D.L. Early sustained ventricular arrhythmias complicating acute myocardial infarction. Am. J. Med. 2008, 121, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.J.; Fender, E.A.; Cha, Y.M.; Lennon, R.J.; Prasad, A.; Barsness, G.W. Long-term outcomes in survivor of early ventricular arrhythmias after acute ST-elevation and non-ST-elevation myocardial infarction treated with percutaneous coronary interventions. Am. J. Cardiol. 2016, 117, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.H.; Harjai, K.J.; Grines, C.L.; Stone, G.W.; Boura, J.; Cox, D. Primary Angioplasty in Myocardial Infarction (PAMI) Investigators. Sustained ventricular tachycardia or fibrillation in the cardiac catheterization laboratory among patients receiving primary percutaneous coronary intervention: Incidence, predictors, and outcomes. J. Am. Coll. Cardiol. 2004, 43, 1765–1772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orvin, K.; Eisen, A.; Goldenberg, I.; Gottlieb, S.; Kornowski, R.; Matetzky, S.; Haim, M. Outcome of contemporary acute coronary syndrome complicated by ventricular tachyarrhythmia. Europace 2016, 18, 219–226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehta, R.H.; Yu, J.; Piccini, J.P.; Tcheng, J.E.; Farkouh, M.E.; Reiffel, J.; Stone, G.W. Prognostic significance of postprocedural sustained ventricular tachycardia or fibrillation in patients undergoing primary percutaneous coronary intervention (from the HORIZONS-AMI Trial). Am. J. Cardiol. 2012, 109, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Sulzgruber, P.; Schnaubelt, S.; Koller, L.; Goliasch, G.; Niederdöckl, J.; Simon, A.; Niessner, A. Cardiac arrest as an age-dependent prognosticator for long-term mortality after acute myocardial infarction: The potential impact of infarction size. Eur. Heart J. Acute Cardiovasc. Care 2019, 8, 153–160. [Google Scholar] [CrossRef] [PubMed]
| Variable | Non-CA N = 154,266 | rCA N = 2296 | p Value | ErCA N = 2106 | LrCA N = 190 | p Value |
|---|---|---|---|---|---|---|
| Age, years, mean (SD) | 65.8 (11.9) | 63.5 (11.7) | <0.0001 | 63.1 (11.5) | 67.9 (12.3) | <0.0001 |
| Age ≥ 65 years | 80,187 (52%) | 990 (43.1%) | <0.0001 | 875 (41.6%) | 115 (60.5%) | <0.0001 |
| Age ≥ 75 years | 41,892 (27.2%) | 476 (20.7%) | <0.0001 | 413 (19.6%) | 63 (33.2%) | <0.0001 |
| Age ≥ 85 years | 7548 (4.9%) | 68 (3%) | <0.0001 | 52 (2.5%) | 16 (8.4%) | <0.0001 |
| Male gender | 98,794 (64.1%) | 1578 (68.9%) | <0.0001 | 1449 (68.9%) | 129 (67.9%) | 0.77 |
| From home admission | 88,130 (57.2%) | 1461 (63.7%) | <0.0001 | 1344 (63.9%) | 117 (61.6%) | 0.53 |
| Transfer from other hospital | 66,041 (42.8%) | 834 (36.3%) | <0.0001 | 761 (36.2%) | 73 (38.4%) | 0.53 |
| Hipercholesterolemia | 64,577 (41.9%) | 879 (38.3%) | 0.0006 | 798 (37.9%) | 81 (42.6%) | 0.2 |
| Hypertension | 112,427 (72.9%) | 1440 (62.7%) | <0.0001 | 1311 (62.3%) | 129 (67.9%) | 0.12 |
| Obesity | 31,882 (20.7%) | 445 (19.4%) | 0.13 | 402 (19.1%) | 43 (22.6%) | 0.24 |
| Diabetes mellitus | 38,799 (25.9%) | 474 (21.5%) | <0.0001 | 406 (20.1%) | 68 (37%) | <0.0001 |
| Smoking (current or past) | 91,654 (59.4%) | 1480 (64.5%) | <0.0001 | 1371 (65.1%) | 109 (57.4%) | 0.033 |
| Current smoker | 45,942 (29.8%) | 800 (34.8%) | <0.0001 | 761 (36.1%) | 39 (20.5%) | <0.0001 |
| Ischemic heart disease diagnosed before AMI | 21,800 (14.1%) | 394 (17.2%) | <0.0001 | 347 (16.5%) | 47 (24.7%) | 0.004 |
| Family history of CAD | 17,452 (11.3%) | 266 (11.6%) | 0.68 | 239 (11.4%) | 27 (14.2%) | 0.24 |
| History of heart failure | 11,821 (7.7%) | 215 (9.4%) | 0.002 | 182 (8.6%) | 33 (17.4%) | <0.0001 |
| History of stroke | 5689 (3.7%) | 114 (5%) | 0.001 | 104 (4.9%) | 10 (5.3%) | 0.84 |
| Chronic kidney disease | 9256 (6%) | 149 (6.5%) | 0.33 | 122 (5.8%) | 27 (14.2%) | <0.0001 |
| Peripheral artery disease | 7026 (4.6%) | 122 (5.3%) | 0.084 | 111 (5.3%) | 11 (5.8%) | 0.76 |
| Chronic obstructive pulmonary disease | 6031 (3.9%) | 120 (5.2%) | 0.0013 | 107 (5.1%) | 13 (6.8%) | 0.3 |
| Prior myocardial infarction | 19,708 (12.8%) | 259 (11.3%) | 0.036 | 364 (17.3%) | 39 (20.5%) | 0.26 |
| Prior PCI | 27,128 (17.6%) | 403 (17.6%) | 0.97 | 232 (11%) | 27 (14.2%) | 0.18 |
| Prior CABG | 5090 (3.3%) | 80 (3.5%) | 0.62 | 72 (3.4%) | 8 (4.2%) | 0.57 |
| NSTEMI | 83,073 (53.9%) | 721 (31.4%) | <0.0001 | 645 (30.6%) | 76 (40%) | 0.008 |
| STEMI | 71,194 (46.1%) | 1575 (68.6%) | <0.0001 | 1461 (69.4%) | 114 (60%) | 0.008 |
| CA before admission | 0 (0%) | 1169 (50.9%) | <0.0001 | 1160 (55.1%) | 9 (4.7%) | <0.0001 |
| ECG heart rate, bpm, mean (SD) | 79.1 (24.3) | 846 (27.7) | <0.0001 | 84.3 (27.7) | 88 (28.1) | 0.078 |
| Sinus rhythm | 140,391 (91.6%) | 1918 (83.6%) | <0.0001 | 1775 (84.4%) | 143 (75.3%) | 0.0012 |
| Atrial fibrillation | 8692 (5.7%) | 197 (8.6%) | <0.0001 | 167 (7.9%) | 30 (15.8%) | 0.0002 |
| Other rhythm | 2421 (1.6%) | 147 (6.4%) | <0.0001 | 136 (6.5%) | 11 (5.8%) | 0.72 |
| Normal QRS | 127,755 (83.5%) | 1765 (77.4%) | 0.0012 | 1625 (77.7%) | 140 (74.1%) | 0.25 |
| LBBB | 5843 (3.8%) | 117 (5.1%) | 0.057 | 106 (5.1%) | 11 (5.8%) | 0.65 |
| RBBB | 5255 (3.4%) | 95 (4.2%) | <0.0001 | 81 (3.9%) | 14 (7.4%) | 0.02 |
| Other QRS abnormalities | 14,184 (9.3%) | 303 (13.3%) | <0.0001 | 279 (13.3%) | 24 (12.7%) | 0.8 |
| Normal ST segment | 12,279 (8%) | 79 (3.4%) | <0.0001 | 66 (3.1%) | 13 (6.8%) | 0.007 |
| ST-segment elevation | 69,412 (45.2%) | 1526 (66.5%) | <0.0001 | 1422 (67.6%) | 104 (54.7%) | 0.0003 |
| ST-segment depression | 36,818 (24%) | 359 (15.6%) | <0.0001 | 320 (15.2%) | 39 (20.5%) | 0.053 |
| Negative T waves | 14,164 (9.2%) | 87 (3.8%) | <0.0001 | 77 (3.7%) | 10 (5.3%) | 0.27 |
| Other ST-segment abnormalities | 19,835 (12.9%) | 233 (10.2%) | <0.0001 | 209 (9.9%) | 24 (12.6%) | 0.24 |
| Systolic BP, mmHg, median (IQR) | 140 (120–155) | 120 (100–140) | <0.0001 | 120 (100–140) | 130 (110–142) | 0.11 |
| Killip class 1 | 12,1579 (79.3%) | 1217 (53.1%) | <0.0001 | 1107 (52.6%) | 110 (57.9%) | 0.16 |
| Killip class 2 | 20,415 (13.3%) | 501 (21.8%) | <0.0001 | 451 (21.4%) | 50 (26.3%) | 0.12 |
| Killip class 3 | 3728 (2.4%) | 118 (5.1%) | <0.0001 | 106 (5%) | 12 (6.3%) | 0.45 |
| Killip class 4 | 1988 (1.3%) | 370 (16.1%) | <0.0001 | 361 (17.2%) | 9 (4.7%) | <0.0001 |
| Variable | Non-CA N = 154,266 | rCA N = 2296 | p Value | ErCA N = 2106 | LrCA N = 190 | p Value |
|---|---|---|---|---|---|---|
| Thrombolysis | 521 (0.4%) | 23 (11%) | <0.0001 | 20 (1%) | 3 (1.7%) | 0.39 |
| Glycoprotein IIb/IIIa inhibitors | 33,532 (21.7%) | 881 (38.4%) | 0.0032 | 814 (38.7%) | 67 (35.3%) | 0.36 |
| Anticoagulation (not associated with PCI) | 79,366 (51.8%) | 1259 (54.9%) | 0.013 | 1147 (54.5%) | 112 (59%) | 0.24 |
| Coronary angiography | 141,438 (91.7%) | 2137 (93.2%) | 0.7 | 1967 (93.5%) | 170 (89.5%) | 0.036 |
| Infarct-related artery—RCA | 42,924 (30.3%) | 759 (35.5%) | <0.0001 | 708 (36%) | 51 (30%) | 0.2 |
| Infarct-related artery—LM | 2877 (2%) | 74 (3.5%) | 0.00031 | 63 (3.2%) | 11 (6.5%) | 0.025 |
| Infarct-related artery—LAD | 48,046 (34%) | 806 (37.7%) | <0.0001 | 730 (37.1%) | 76 (44.7%) | 0.049 |
| Infarct-related artery—Cx | 27,891 (19.7%) | 342 (16%) | 0.29 | 321 (16.3%) | 21 (12.4%) | 0.18 |
| Infarct-related artery—bypass | 1530 (1.1%) | 18 (0.8%) | <0.0001 | 16 (0.8%) | 2 (1.2%) | 0.62 |
| PCI | 118,119 (76.6%) | 1956 (85.2%) | <0.0001 | 1802 (85.6%) | 154 (81.1%) | 0.096 |
| TIMI 1 before PCI | 72,425 (63.1%) | 1450 (77.7%) | <0.0001 | 1344 (78.5%) | 106 (68.8%) | 0.006 |
| TIMI 3 after PCI | 107,885 (93.6%) | 1704 (91.3%) | 0.044 | 1569 (91.6%) | 135 (87.7%) | 0.098 |
| CABG | 4297 (2.8%) | 48 (2.1%) | <0.0001 | 46 (2.2%) | 2 (1.1%) | 0.44 |
| Pacemaker | 810 (0.5%) | 36 (1.6%) | <0.0001 | 28 (1.3%) | 8 (4.2%) | 0.0022 |
| ICD | 243 (0.2%) | 60 (2.6%) | <0.0001 | 34 (1.6%) | 26 (13.7%) | <0.0001 |
| CRT-D | 25 (0%) | 7 (0.3%) | <0.0001 | 6 (0.3%) | 1 (0.5%) | 0.91 |
| ICD or CRT-D | 268 (0.2%) | 67 (2.9%) | <0.0001 | 40 (1.9%) | 27 (14.2%) | <0.0001 |
| Blood transfusion | 4912 (3.2%) | 213 (9.3%) | <0.0001 | 171 (8.1%) | 42 (22.1%) | <0.0001 |
| Ablation | 24 (0%) | 4 (0.2%) | 0.28 | 4 (0.2%) | 0 (0%) | 0.76 |
| Heart valve surgery | 286 (0.2%) | 2 (0.1%) | <0.0001 | 2 (0.1%) | 0 (0%) | 0.39 |
| IABP | 1382 (0.9%) | 167 (7.3%) | <0.0001 | 150 (7.1%) | 17 (9%) | 0.35 |
| Variable | Non-CA N = 154,266 | rCA N = 2296 | p Value | ErCA N = 2106 | LrCA N = 190 | p Value |
|---|---|---|---|---|---|---|
| Massive bleeding | 1638 (1.1%) | 114 (5%) | <0.0001 | 93 (4.4%) | 21 (11.1%) | <0.0001 |
| Recurrent myocardial infarction | 274 (0.2%) | 28 (1.2%) | <0.0001 | 19 (0.9%) | 9 (4.7%) | <0.0001 |
| Stroke | 241 (0.2%) | 31 (1.4%) | <0.0001 | 29 (1.4%) | 2 (1.1%) | 0.97 |
| Pulmonary edema | 1088 (0.7%) | 102 (4.4%) | <0.0001 | 87 (4.1%) | 15 (7.9%) | 0.016 |
| Cardiogenic shock | 661 (0.4%) | 227 (9.9%) | <0.0001 | 204 (9.7%) | 23 (12.1%) | 0.28 |
| Hospital CA | 0 (0%) | 1216 (53.0%) | <0.0001 | 1026 (48.7%) | 190 (100%) | <0.0001 |
| Mechanical complication: heart rupture | 28 (0%) | 5 (0.2%) | 0.0037 | 4 (0.2%) | 1 (0.5%) | 0.89 |
| Mechanical complication: mitral regurgitation | 42 (0%) | 3 (0.1%) | 0.54 | 3 (0.1%) | 0 (0%) | 0.6 |
| Mechanical complication: VSD | 25 (0%) | 0 (0%) | <0.0001 | 0 (0%) | 0 (0%) | 1.00 |
| Mechanical complication: heart rupture or VSD | 51 (0%) | 5 (0.2%) | <0.0001 | 4 (0.2%) | 1 (0.5%) | 0.89 |
| Mechanical complications (all) | 92 (0.1%) | 8 (0.4%) | <0.0001 | 7 (0.3%) | 1 (0.5%) | 0.84 |
| Variable | Non-CA N = 154,266 | rCA N = 2296 | p Value | ErCA N = 2106 | LrCA N = 190 | p Value |
|---|---|---|---|---|---|---|
| LVEF, %, mean (SD) | 47.9 (10.6) | 43.2 (12.0) | <0.0001 | 43.7 (11.8) | 38.4 (12.9) | <0.0001 |
| Hospitalisation length, days, median (IQR) | 5 (3–7) | 7 (4–11) | 0.0031 | 6 (4–10) | 12 (8–19) | <0.0001 |
| Aspirin at discharge | 141,512 (91.7%) | 2069 (90.1%) | 0.0052 | 1893 (89.9%) | 176 (92.6%) | 0.22 |
| P2Y12 inhibitor at discharge | 130,658 (84.7%) | 1955 (85.2%) | 0.55 | 1786 (84.8%) | 169 (89%) | 0.12 |
| Acenocoumarol/warfarin at discharge | 3727 (2.4%) | 68 (3%) | 0.091 | 57 (2.7%) | 11 (5.8%) | 0.016 |
| Beta-blocker at discharge | 128,332 (83.2%) | 1822 (79.4%) | <0.0001 | 1665 (79.1%) | 157 (82.6%) | 0.24 |
| LMWH at discharge | 7399 (4.8%) | 197 (8.6%) | <0.0001 | 176 (8.4%) | 21 (11.1%) | 0.2 |
| ACE-I at discharge | 119,911 (77.7%) | 1693 (73.7%) | <0.0001 | 1554 (73.8%) | 139 (73.2%) | 0.85 |
| ARB at discharge | 3765 (2.4%) | 46 (2%) | 0.18 | 41 (2%) | 5 (2.6%) | 0.71 |
| Fibrate at discharge | 1688 (1.1%) | 18 (0.8%) | 0.16 | 18 (0.9%) | 0 (0%) | 0.39 |
| Statin at discharge | 135,497 (87.8%) | 1966 (85.6%) | 0.0014 | 1803 (85.6%) | 163 (85.8%) | 0.95 |
| Calcium channel blocker at discharge | 14,877 (9.6%) | 133 (5.8%) | <0.0001 | 116 (5.5%) | 17 (9%) | 0.052 |
| Nitrate at discharge | 17,305 (11.2%) | 188 (8.2%) | <0.0001 | 168 (8%) | 20 (10.5%) | 0.22 |
| Diuretic at discharge | 38,629 (25%) | 773 (33.7%) | <0.0001 | 675 (32.1%) | 98 (51.6%) | <0.0001 |
| Diabetes treated with insulin at discharge | 13,410 (8.7%) | 189 (8.2%) | 0.44 | 161 (7.6%) | 28 (14.7%) | 0.0007 |
| Diabetes treated with oral medication at discharge | 14,642 (9.5%) | 154 (6.7%) | <0.0001 | 132 (6.3%) | 22 (11.6%) | 0.0051 |
| Variable | Non-CA N = 154,266 | rCA N = 2296 | p Value | ErCA N = 2106 | LrCA N = 190 | p Value |
|---|---|---|---|---|---|---|
| Mortality after discharge | ||||||
| Death: 30 days | 1765 (1.1%) | 53 (2.3%) | <0.0001 | 47 (2.2%) | 6 (3.2%) | 0.42 |
| Death: 6 months | 7942 (5.2%) | 228 (9.9%) | <0.0001 | 194 (9.2%) | 34 (17.9%) | 0.0001 |
| Death: 12 months | 11,947 (7.7%) | 299 (13.0%) | <0.0001 | 259 (12.3%) | 40 (21.1%) | 0.0006 |
| Re-hospitalisation with main diagnosis | ||||||
| All cause | 88,016 (57.1%) | 1348 (58.7%) | 0.11 | 1224 (58.1%) | 124 (65.3%) | 0.055 |
| Cardiovascular cause | 71,290 (46.2%) | 1095 (47.7%) | 0.15810 | 1000 (47.5%) | 95 (50%) | 0.51 |
| Chronic coronary syndrome | 36,659 (23.8%) | 557 (24.3%) | 0.57925 | 530 (25.2%) | 27 (14.2%) | 0.0007 |
| Unstable angina | 19,390 (12.6%) | 225 (9.8%) | 0.00007 | 213 (10.1%) | 12 (6.3%) | 0.092 |
| Myocardial infarction | 8552 (5.5%) | 109 (4.8%) | 0.09758 | 96 (4.6%) | 13 (6.8%) | 0.16 |
| Chronic coronary syndrome or unstable angina or myocardial infarction | 55,008 (35.7%) | 766 (33.4%) | 0.02262 | 720 (34.2%) | 46 (24.2%) | 0.0052 |
| Heart failure | 12,491 (8.1%) | 262 (11.4%) | <0.0001 | 228 (10.8%) | 34 (17.9%) | 0.0033 |
| Stroke | 2205 (1.4%) | 23 (1%) | 0.08595 | 20 (1%) | 3 (1.6%) | 0.65 |
| Cardiac rehabilitation after 30 days | 32,079 (20.8%) | 541 (23.6%) | 0.00119 | 511 (24.3%) | 30 (15.8%) | 0.0084 |
| Cardiac rehabilitation after 6 months | 35,748 (23.2%) | 592 (25.8%) | 0.00326 | 561 (26.6%) | 31 (16.3%) | 0.0018 |
| Cardiac rehabilitation after 12 months | 37,258 (24.2%) | 614 (26.7%) | 0.00401 | 580 (27.5%) | 34 (17.9%) | 0.004 |
| Re-hospitalisation with procedure | ||||||
| Coronary angiography | 39,549 (25.6%) | 559 (24.4%) | 0.15983 | 528 (25.1%) | 31 (16.3%) | 0.0071 |
| PCI | 31,015 (20.1%) | 376 (16.4%) | 0.00001 | 361 (17.1%) | 15 (7.9%) | 0.001 |
| CABG | 8081 (5.2%) | 112 (4.9%) | 0.44160 | 103 (4.9%) | 9 (4.7%) | 0.92 |
| Pacemaker implantation | 1276 (0.8%) | 18 (0.8%) | 0.82060 | 17 (0.8%) | 1 (0.5%) | 0.99 |
| CRT-P implantation | 51 (0.03%) | 0 (0%) | 0.38355 | 0 (0%) | 0 (0%) | 1.00 |
| ICD implantation | 2171 (1.4%) | 94 (4.1%) | <0.0001 | 83 (3.9%) | 11 (5.8%) | 0.22 |
| CRT-D implantation | 365 (0.2%) | 18 (0.8%) | <0.0001 | 17 (0.8%) | 1 (0.5%) | 0.99 |
| ICD or CRT-D implantation | 2531 (1.6%) | 111 (4.8%) | <0.0001 | 99 (4.7%) | 12 (6.3%) | 0.32 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kowalik, R.; Gierlotka, M.; Ozierański, K.; Trzeciak, P.; Fojt, A.; Feusette, P.; Tycińska, A.; Opolski, G.; Grabowski, M.; Gąsior, M. In-Hospital and One-Year Outcomes of Patients after Early and Late Resuscitated Cardiac Arrest Complicating Acute Myocardial Infarction—Data from a Nationwide Database. J. Clin. Med. 2022, 11, 609. https://doi.org/10.3390/jcm11030609
Kowalik R, Gierlotka M, Ozierański K, Trzeciak P, Fojt A, Feusette P, Tycińska A, Opolski G, Grabowski M, Gąsior M. In-Hospital and One-Year Outcomes of Patients after Early and Late Resuscitated Cardiac Arrest Complicating Acute Myocardial Infarction—Data from a Nationwide Database. Journal of Clinical Medicine. 2022; 11(3):609. https://doi.org/10.3390/jcm11030609
Chicago/Turabian StyleKowalik, Robert, Marek Gierlotka, Krzysztof Ozierański, Przemysław Trzeciak, Anna Fojt, Piotr Feusette, Agnieszka Tycińska, Grzegorz Opolski, Marcin Grabowski, and Mariusz Gąsior. 2022. "In-Hospital and One-Year Outcomes of Patients after Early and Late Resuscitated Cardiac Arrest Complicating Acute Myocardial Infarction—Data from a Nationwide Database" Journal of Clinical Medicine 11, no. 3: 609. https://doi.org/10.3390/jcm11030609
APA StyleKowalik, R., Gierlotka, M., Ozierański, K., Trzeciak, P., Fojt, A., Feusette, P., Tycińska, A., Opolski, G., Grabowski, M., & Gąsior, M. (2022). In-Hospital and One-Year Outcomes of Patients after Early and Late Resuscitated Cardiac Arrest Complicating Acute Myocardial Infarction—Data from a Nationwide Database. Journal of Clinical Medicine, 11(3), 609. https://doi.org/10.3390/jcm11030609







