Usefulness of Cardiac Computed Tomography in Coronary Risk Prediction: A Five-Year Follow-Up of the SPICA Study (Secure Prevention with Imaging of the Coronary Arteries)
Abstract
1. Introduction
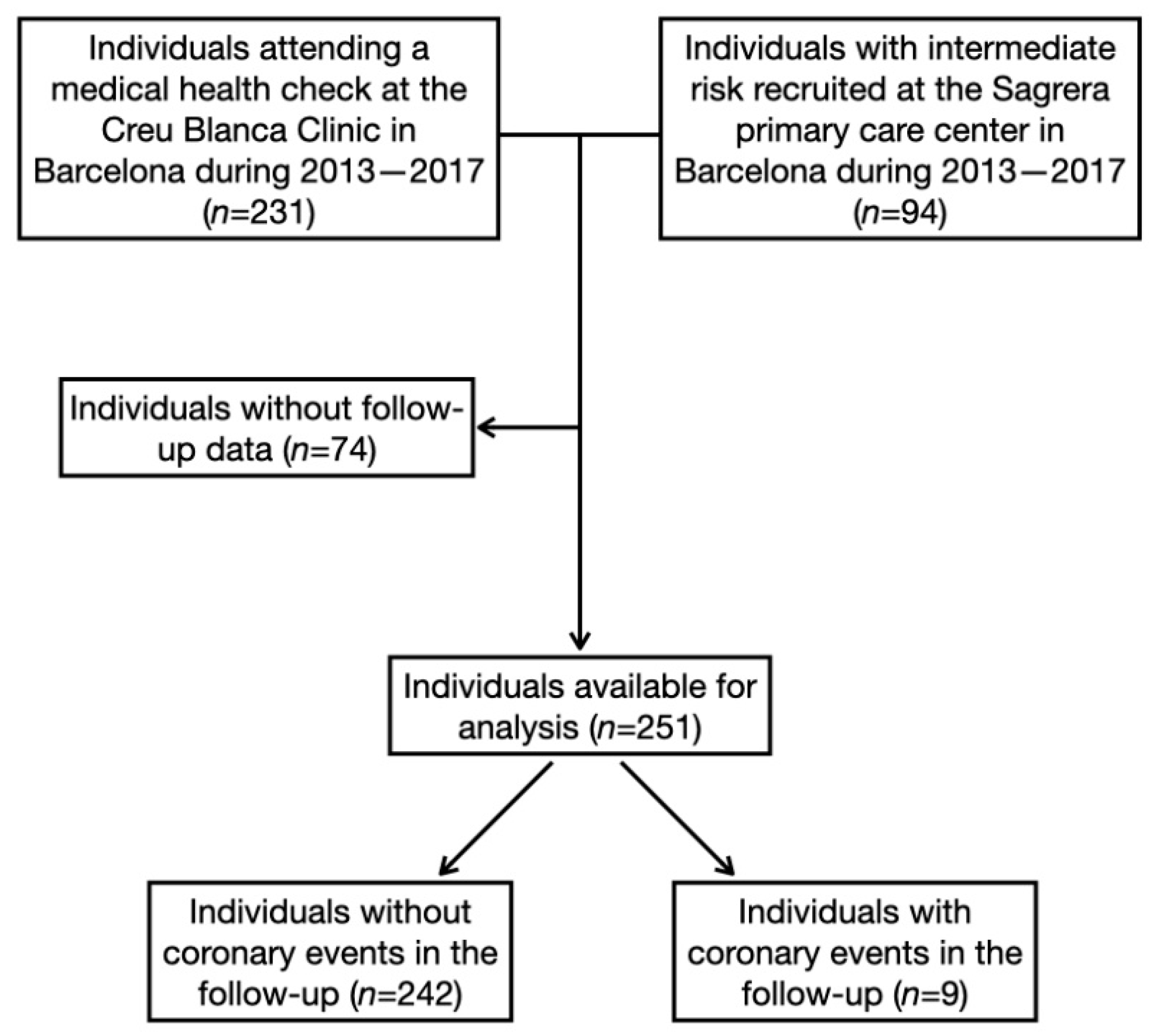
2. Methods
2.1. Cardiac Computed Tomography Acquisition Protocol
2.2. Follow-Up and Outcome of the Study
2.3. Measurements
2.4. Statistical Analysis
2.5. Ethical Aspects
3. Results
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Dégano, I.R.; Elosua, R.; Marrugat, J. Epidemiología del síndrome coronario agudo en España: Estimación del número de casos y la tendencia de 2005 a 2049. Rev. Esp. Cardiol. 2013, 66, 472–481. [Google Scholar] [CrossRef]
- Emberson, J.; Whincup, P.; Morris, R. Evaluating the impact of population and high-risk strategies for the primary prevention of cardiovascular disease. Eur. Heart J. 2004, 25, 484–491. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- SCORE2 Working Group; ESC Cardiovascular Risk Collaboration. SCORE2 risk prediction algorithms: New models to estimate 10-year risk of cardiovascular disease in Europe. Eur. Heart J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef] [PubMed]
- SCORE2 Working Group; ESC Cardiovascular Risk Collaboration. SCORE2-OP risk prediction algorithms: Estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur. Heart J. 2021, 42, 2455–2467. [Google Scholar] [CrossRef]
- Marrugat, J.; Subirana, I.; Comín, E. Validity of an adaptation of the Framingham cardiovascular risk function: The VERIFICA study. J. Epidemiol. Community Health 2007, 61, 40–47. [Google Scholar] [CrossRef]
- Marrugat, J.; Vila, J.; Baena-Díez, J.M. Validez relativa de la estimación del riesgo cardiovascular a 10 años en una cohorte poblacional del estudio REGICOR. Rev. Esp. Cardiol. 2011, 64, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Yeboah, J.; McClelland, R.L.; Polonsky, T. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA 2012, 308, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.J.; Gona, P.; Larson, M.G. Multiple biomarkers for the prediction of first major cardiovascular events and death. N. Engl. J. Med. 2006, 355, 2631–2639. [Google Scholar] [CrossRef]
- Eldrup, N.; Sillesen, H.; Prescott, E. Ankle brachial index, C-reactive protein, and central augmentation index to identify individuals with severe atherosclerosis. Eur. Heart J. 2006, 27, 316–322. [Google Scholar] [CrossRef][Green Version]
- Velescu, A.; Clara, A.; Peñafiel, J. Adding low ankle brachial index to classical risk factors improves the prediction of major cardiovascular events. The REGICOR study. Atherosclerosis 2015, 241, 357–363. [Google Scholar] [CrossRef]
- Simon, A.; Chironi, G.; Levenson, J. Comparative performance of subclinical atherosclerosis tests in predicting coronary heart disease in asymptomatic individuals. Eur. Heart J. 2007, 28, 2967–2971. [Google Scholar] [CrossRef]
- Budoff, M.J.; Young, R.; Burke, G. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: The multi-ethnic study of atherosclerosis (MESA). Eur. Heart J. 2018, 39, 2401–2408. [Google Scholar] [CrossRef] [PubMed]
- Min, J.K.; Labounty, T.M.; Gomez, M.J. Incremental prognostic value of coronary computed tomographic angiography over coronary artery calcium score for risk prediction of major adverse cardiac events in asymptomatic diabetic individuals. Atherosclerosis 2014, 232, 298–304. [Google Scholar] [CrossRef]
- Cho, I.; Chang, H.J.; Sung, J.M. Coronary computed tomographic angiography and risk of all-cause mortality and nonfatal myocardial infarction in subjects without chest pain syndrome from the CONFIRM Registry (coronary CT angiography evaluation for clinical outcomes: An international multicenter registry). Circulation 2012, 126, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Oudkerk, M.; Stillman, A.E.; Halliburton, S. Coronary artery calcium screening: Current status and recommendations from the European Society of Cardiac Radiology and North American Society for Cardiovascular Imaging. Int. J. Cardiovasc. Imaging 2008, 18, 2785–2807. [Google Scholar] [CrossRef]
- Hausleiter, J.; Meyer, T.; Hermann, F. Estimated radiation dose associated with cardiac CT angiography. JAMA 2009, 301, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Marrugat, J.; D’Agostino, R.; Sullivan, L. An adaptation of the Framingham coronary heart disease risk function to European Mediterranean areas. J. Epidemiol. Community Health 2003, 57, 634–638. [Google Scholar] [CrossRef]
- Cook, N.R.; Ridker, P.M. Advances in measuring the effect of individual predictors of cardiovascular risk: The role of reclassification measures. Ann. Intern. Med. 2009, 150, 795–802. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2019. [Google Scholar]
- World Medical Association. World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Erbel, R.; Möhlenkamp, S.; Moebus, S. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of Subclinical coronary atherosclerosis: The Heinz Nixdorf Recall study. J. Am. Coll. Cardiol. 2010, 56, 1397–1406. [Google Scholar] [CrossRef]
- Detrano, R.; Guerci, A.D.; Carr, J.J. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N. Engl. J. Med. 2008, 358, 336–345. [Google Scholar] [CrossRef]
- Budoff, M.J.; Shaw, L.J.; Liu, S.T. Long-Term Prognosis Associated With Coronary Calcification. Observations from a Registry of 25,253 Patients. J. Am. Coll. Cardiol. 2007, 49, 1860–1870. [Google Scholar] [CrossRef]
- Cho, I.; Al’Aref, S.J.; Berger, A. Prognostic value of coronary computed tomographic angiography findings in asymptomatic individuals: A 6-year follow-up from the prospective multicentre international CONFIRM study. Eur. Heart J. 2018, 39, 934–941. [Google Scholar] [CrossRef]
- Blaha, M.J.; Cainzos-Achirica, M.; Greenland, P. Role of Coronary Artery Calcium Score of Zero and Other Negative Risk Markers for Cardiovascular Disease: The Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 2016, 133, 849–858. [Google Scholar] [CrossRef]
- Virmani, R.; Burke, A.P.; Farb, A. Pathology of the vulnerable plaque. J. Am. Coll. Cardiol. 2006, 47, C13–C18. [Google Scholar] [CrossRef]
- Cho, I.; Chang, H.; Hartaigh, B.Ó. Incremental prognostic utility of coronary CT angiography for asymptomatic patients based upon extent and severity of coronary artery calcium: Results from the COronary CT Angiography EvaluatioN for Clinical Outcomes InteRnational Multicenter (CONFIRM). Eur. Heart J. 2015, 36, 501–508. [Google Scholar] [CrossRef]
- Al-Mallah, M.H.; Qureshi, W.; Lin, F.Y. Does coronary CT angiography improve risk stratification over coronary calcium scoring in symptomatic patients with suspected coronary artery disease? Results from the prospective multicenter international CONFIRM registry. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Ayoub, C.; Erthal, F.; Abdelsalam, M.A. Prognostic value of segment involvement score compared to other measures of coronary atherosclerosis by computed tomography: A systematic review and meta-analysis. J. Cardiovasc. Comput. Tomogr. 2017, 11, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Bittencourt, M.S.; Hulten, E.; Ghoshhajra, B. Prognostic value of nonobstructive and obstructive coronary artery disease detected by coronary computed tomography angiography to identify cardiovascular events. Circ. Cardiovasc. Imaging 2014, 7, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Chow, B.J.W.; Small, G.; Yam, Y. Prognostic and therapeutic implications of statin and aspirin therapy in individuals with nonobstructive coronary artery disease: Results from the confirm (coronary CT angiography evaluation for clinical outcomes: An international multicenter registry) registry. Arterioscler. Thromb. Vasc. Biol. 2015, 35, 981–989. [Google Scholar] [CrossRef] [PubMed]
- Hulten, E.; Bittencourt, M.S.; Singh, A. Coronary artery disease detected by coronary computed tomographic angiography is associated with intensifcation of preventive medical therapy and lower low-density lipoprotein cholesterol. Circ. Cardiovasc. Imaging 2014, 7, 629–638. [Google Scholar] [CrossRef] [PubMed]
- LaBounty, T.M.; Devereux, R.B.; Lin, F.Y. Impact of Coronary Computed Tomographic Angiography Findings on the Medical Treatment and Control of Coronary Artery Disease and Its Risk Factors. Am. J. Cardiol. 2009, 104, 873–877. [Google Scholar] [CrossRef] [PubMed]
| All n = 251 | No CAD Event in the Follow-Up n = 242 | CAD Event in the Follow-Up n = 9 | Standardized Differences | p-Value | |
|---|---|---|---|---|---|
| Age (years) | 58.4 (11.2) | 58.3 (11.3) | 60.8 (8.83) | 0.245 | 0.525 |
| Gender (% female) | 64 (25.5%) | 64 (25.5%) | 0.0 (0.0%) | 0.848 | 0.080 |
| Total cholesterol (mgr/dL) | 201 (39.7) | 202 (39.4) | 178 (45.0) | 0.567 | 0.082 |
| HDL cholesterol (mgr/dL) | 53.4 (18.7) | 53.8 (18.9) | 42.7 (6.98) | 0.782 | 0.045 |
| Systolic blood pressure (mm Hg) | 134 (17.7) | 133 (17.4) | 149 (18.4) | 0.887 | 0.007 |
| Dyastolic blood pressure (mm Hg) | 83.1 (10.8) | 82.9 (10.6) | 88.4 (13.8) | 0.454 | 0.117 |
| Diabetes (%) | 57 (23.0%) | 51 (21.3%) | 6 (66.7%) | 1.026 | 0.002 |
| Smoking (%) | 72 (28.7%) | 69 (28.5%) | 3 (33.3%) | 0.104 | 0.790 |
| Framingham-REGICOR risk | 12.8 (7.68) | 12.5 (7.5) | 20.0 (8.96) | 0.905 | 0.006 |
| CAC (Arbitrary units) | 220 (605) | 176 (427) | 1232 (1980) | 0.737 | <0.001 |
| Percent CAC = 0 | 94 (43.5%) | 94 (45.4%) | 0.0 (0.0%) | 1.290 | 0.009 |
| Segment Involvement Score (number of segments with coronary artery plaques) | 2.79 (3.17) | 2.59 (3.01) | 7.89 (2.93) | 1.782 | <0.001 |
| Percent SIS < 5 | 170 (73.0%) | 169 (75.4%) | 1 (11.1%) | 1.707 | <0.001 |
| Sommer’s D (95% CI) | p-Value * | |
|---|---|---|
| REGICOR CAD risk function alone | 0.74 (0.61, 0.87) | - |
| with coronary artery calcium | 0.79 (0.65, 0.92) | 0.074 |
| with segment involment score | 0.89 (0.83, 0.96) | 0.003 |
| with coronary artery calcium and segment involment scores | 0.89 (0.83, 0.96) | 0.004 |
| Continuous Net Reclassification Index (NRI) | Categorical Net Reclassification Index (NRI) | |||
|---|---|---|---|---|
| NRI Difference (%) * (95% CI) | p-Value | NRI Difference (%) * (95% CI) | p-Value | |
| REGICOR CAD risk function with CAC | ||||
| Total | 0.69 (0.07, 1.44) | 0.034 | 0.06 (−0.33, 0.45) | 0.773 |
| CAD cases | −0.11 (−0.71, 0.60) | 0.812 | −0.11 (−0.50, 0.28) | 0.577 |
| Non-cases | 0.80 (0.72, 0.87) | <0.001 | 0.17 (0.11, 0.22) | <0.001 |
| Intermediate risk group | - | - | 0.24 (0.05, 0.42) | 0.013 |
| REGICOR CAD risk function with Segment Involvement Score | ||||
| Total | 1.14 (0.48, 1.64) | 0.002 | 0.52 (0.17, 0.87) | 0.003 |
| CAD cases | 0.56 (−0.13 1.00) | 0.080 | 0.33 (−0.01, 0.67) | 0.050 |
| Non-cases | 0.59 (0.47, 0.69) | <0.001 | 0.19 (0.11, 0.27) | <0.001 |
| Intermediate risk group | - | - | 0.27 (0.08, 0.45) | 0.006 |
| REGICOR CAD risk function with CAC and Segment Involvement Scores | ||||
| Total | 1.17 (0.52, 1.66) | 0.006 | 0.42 (0.12, 0.71) | 0.005 |
| CAD cases | 0.56 (−0.10, 1.00) | 0.090 | 0.22 (−0.06, 0.50) | 0.122 |
| Non-cases | 0.62 (0.51, 0.72) | <0.001 | 0.20 (0.11, 0.28) | <0.001 |
| Intermediate risk group | - | - | 0.30 (0.12, 0.47) | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viladés-Medel, D.; Dégano, I.R.; Subirana, I.; Descalzo, M.; Padilla, M.; Mundet, X.; Carreras Costa, F.; Alomar Serrallach, X.; Camps, A.; Elosua, R.; et al. Usefulness of Cardiac Computed Tomography in Coronary Risk Prediction: A Five-Year Follow-Up of the SPICA Study (Secure Prevention with Imaging of the Coronary Arteries). J. Clin. Med. 2022, 11, 533. https://doi.org/10.3390/jcm11030533
Viladés-Medel D, Dégano IR, Subirana I, Descalzo M, Padilla M, Mundet X, Carreras Costa F, Alomar Serrallach X, Camps A, Elosua R, et al. Usefulness of Cardiac Computed Tomography in Coronary Risk Prediction: A Five-Year Follow-Up of the SPICA Study (Secure Prevention with Imaging of the Coronary Arteries). Journal of Clinical Medicine. 2022; 11(3):533. https://doi.org/10.3390/jcm11030533
Chicago/Turabian StyleViladés-Medel, David, Irene R. Dégano, Isaac Subirana, Martin Descalzo, Mireia Padilla, Xavier Mundet, Francesc Carreras Costa, Xavier Alomar Serrallach, Anna Camps, Roberto Elosua, and et al. 2022. "Usefulness of Cardiac Computed Tomography in Coronary Risk Prediction: A Five-Year Follow-Up of the SPICA Study (Secure Prevention with Imaging of the Coronary Arteries)" Journal of Clinical Medicine 11, no. 3: 533. https://doi.org/10.3390/jcm11030533
APA StyleViladés-Medel, D., Dégano, I. R., Subirana, I., Descalzo, M., Padilla, M., Mundet, X., Carreras Costa, F., Alomar Serrallach, X., Camps, A., Elosua, R., Marrugat, J., & Leta Petracca, R. (2022). Usefulness of Cardiac Computed Tomography in Coronary Risk Prediction: A Five-Year Follow-Up of the SPICA Study (Secure Prevention with Imaging of the Coronary Arteries). Journal of Clinical Medicine, 11(3), 533. https://doi.org/10.3390/jcm11030533






