Clinical Characteristics and Predictors of All-Cause Mortality in Patients with Hypertensive Urgency at an Emergency Department
Abstract
:1. Introduction
2. Materials and Methods
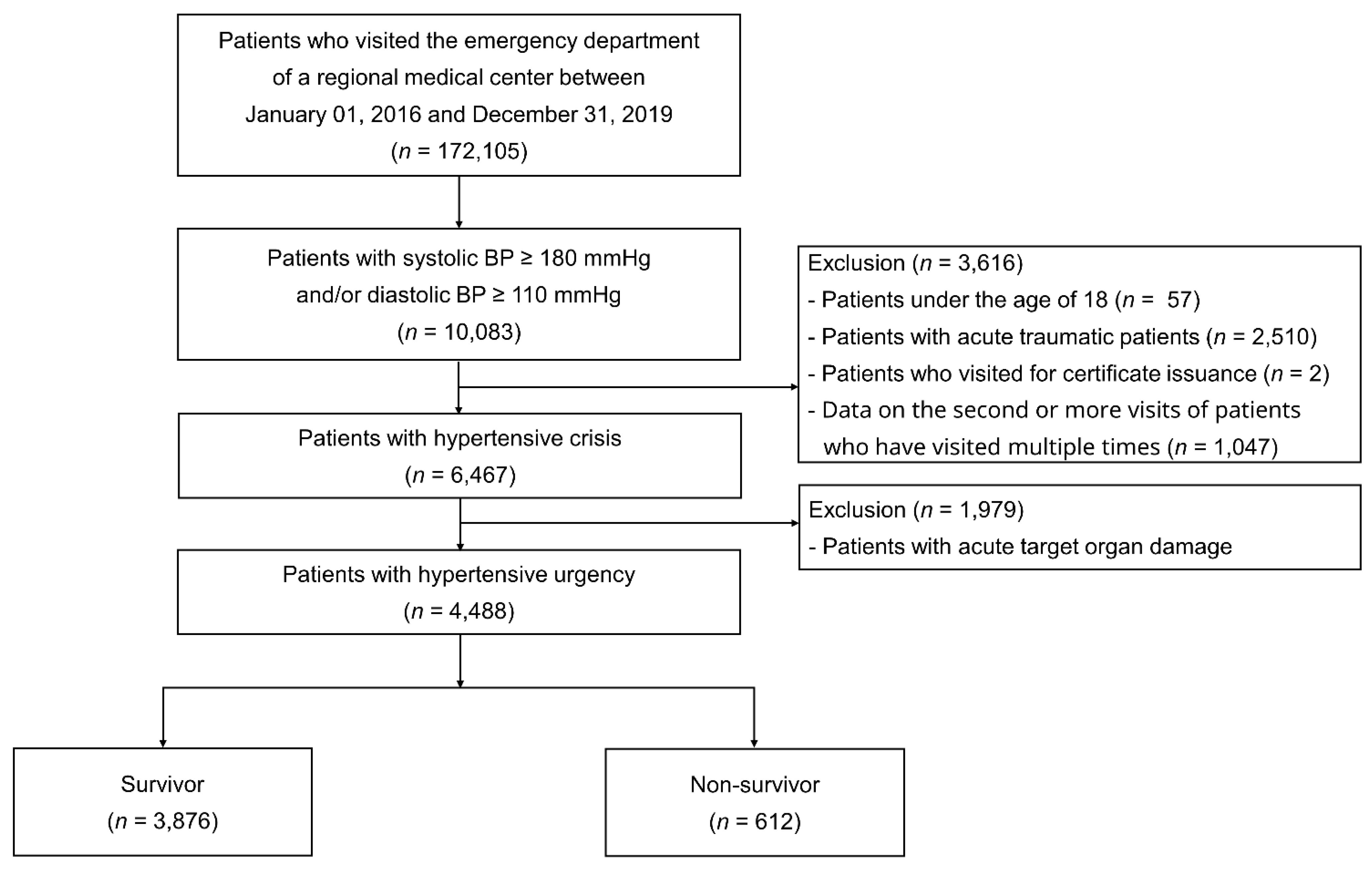
2.1. Study Population
2.2. Data Collection and Outcomes
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Outcomes of the Index Visit and during the Follow-Up Period
3.3. Predictors of All-Cause Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [CrossRef] [PubMed]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef] [PubMed]
- van den Born, B.-J.H.; Lip, G.Y.H.; Brguljan-Hitij, J.; Cremer, A.; Segura, J.; Morales, E.; Mahfoud, F.; Amraoui, F.; Persu, A.; Kahan, T.; et al. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur. Heart J. Cardiovasc. Pharmacother. 2018, 5, 37–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peixoto, A.J. Acute Severe Hypertension. N. Engl. J. Med. 2019, 381, 1843–1852. [Google Scholar] [CrossRef] [PubMed]
- Muiesan, M.L.; Salvetti, M.; Amadoro, V.; di Somma, S.; Perlini, S.; Semplicini, A.; Borghi, C.; Volpe, M.; Saba, P.S.; Cameli, M.; et al. An update on hypertensive emergencies and urgencies. J. Cardiovasc. Med. 2015, 16, 372–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, B.S.; Kim, H.-J.; Lyu, M.; Kim, W.-D.; Lee, Y.; Kim, M.; Lee, S.; Park, J.-K.; Shin, J.; Shin, H.; et al. Clinical characteristics, practice patterns, and outcomes of patients with acute severe hypertension visiting the emergency department. J. Hypertens. 2021. [Google Scholar] [CrossRef]
- White, S.L.; Yu, R.; Craig, J.C.; Polkinghorne, K.R.; Atkins, R.C.; Chadban, S.J. Diagnostic accuracy of urine dipsticks for detection of albuminuria in the general community. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2011, 58, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Janke, A.T.; McNaughton, C.D.; Brody, A.M.; Welch, R.D.; Levy, P.D. Trends in the Incidence of Hypertensive Emergencies in US Emergency Departments From 2006 to 2013. J. Am. Heart Assoc. 2016, 5. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.; Beevers, M.; Beevers, G. The failure of malignant hypertension to decline: A survey of 24 years’ experience in a multiracial population in England. J. Hypertens. 1994, 12, 1297–1305. [Google Scholar] [CrossRef] [PubMed]
- Vlcek, M.; Bur, A.; Woisetschläger, C.; Herkner, H.; Laggner, A.N.; Hirschl, M.M. Association between hypertensive urgencies and subsequent cardiovascular events in patients with hypertension. J. Hypertens. 2008, 26, 657–662. [Google Scholar] [CrossRef] [PubMed]
- Merlo, C.; Bally, K.; Tschudi, P.; Martina, B.; Zeller, A. Management and outcome of severely elevated blood pressure in primary care: A prospective observational study. Swiss Med. Wkly. 2012, 142, w13507. [Google Scholar] [CrossRef] [PubMed]
- Guiga, H.; Decroux, C.; Michelet, P.; Loundou, A.; Cornand, D.; Silhol, F.; Vaisse, B.; Sarlon-Bartoli, G. Hospital and out-of-hospital mortality in 670 hypertensive emergencies and urgencies. J. Clin. Hypertens. 2017, 19, 1137–1142. [Google Scholar] [CrossRef] [PubMed]
- Grassi, D.; O’Flaherty, M.; Pellizzari, M.; Bendersky, M.; Rodriguez, P.; Turri, D.; Forcada, P.; Ferdinand, K.C.; Kotliar, C. Hypertensive urgencies in the emergency department: Evaluating blood pressure response to rest and to antihypertensive drugs with different profiles. J. Clin. Hypertens. 2008, 10, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Levy, P.D.; Mahn, J.J.; Miller, J.; Shelby, A.; Brody, A.; Davidson, R.; Burla, M.J.; Marinica, A.; Carroll, J.; Purakal, J.; et al. Blood pressure treatment and outcomes in hypertensive patients without acute target organ damage: A retrospective cohort. Am. J. Emerg. Med. 2015, 33, 1219–1224. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.K.; Young, L.; Howell, E.H.; Hu, B.; Rutecki, G.; Thomas, G.; Rothberg, M.B. Characteristics and Outcomes of Patients Presenting With Hypertensive Urgency in the Office Setting. JAMA Intern. Med. 2016, 176, 981–988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.-Y.; Shin, J.; Kim, G.-H.; Park, S.; Ihm, S.-H.; Kim, H.C.; Kim, K.-i.; Kim, J.H.; Lee, J.H.; Park, J.-M.; et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: Part II-diagnosis and treatment of hypertension. Clin. Hypertens. 2019, 25, 20. [Google Scholar] [CrossRef] [PubMed]
- Couser, W.G.; Remuzzi, G.; Mendis, S.; Tonelli, M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011, 80, 1258–1270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2002, 39, S1–S266.
- Oh, J.S.; Lee, C.H.; Park, J.I.; Park, H.K.; Hwang, J.K. Hypertension-Mediated Organ Damage and Long-term Cardiovascular Outcomes in Asian Hypertensive Patients without Prior Cardiovascular Disease. J. Korean Med. Sci. 2020, 35, e400. [Google Scholar] [CrossRef] [PubMed]
| All Patients (n = 4488) | Survivors (n = 3876) | Non-Survivors (n = 612) | p-Value | |
|---|---|---|---|---|
| Age, years, mean (SD) | 59.0 (17.3) | 56.6 (16.7) | 74.2 (12.9) | <0.001 |
| Males, n (%) | 2200 (49.0) | 1866 (48.1) | 334 (54.6) | 0.003 |
| Medical history, n (%) | ||||
| Hypertension | 2073 (48.4) | 1688 (45.8) | 385 (64.5) | <0.001 |
| Diabetes mellitus | 985 (23.3) | 748 (20.6) | 237 (40.3) | <0.001 |
| Dyslipidemia | 351 (8.4) | 323 (9.0) | 28 (4.8) | <0.001 |
| Ischemic stroke | 267 (6.4) | 176 (4.9) | 91 (15.6) | <0.001 |
| Hemorrhagic stroke | 98 (2.4) | 71 (2.0) | 27 (4.7) | <0.001 |
| Coronary artery disease | 277 (6.7) | 219 (6.1) | 58 (10.0) | <0.001 |
| Peripheral artery disease | 39 (0.9) | 28 (0.8) | 11 (1.9) | 0.010 |
| Heart failure | 72 (1.7) | 43 (1.2) | 29 (5.0) | <0.001 |
| Chronic kidney disease | 253 (6.1) | 151 (4.2) | 102 (17.5) | <0.001 |
| Social history, n (%) | ||||
| Cigarette smoking | 545 (22.8) | 479 (24.3) | 66 (15.8) | <0.001 |
| Alcohol consumption | 822 (33.5) | 745 (36.8) | 77 (18.2) | <0.001 |
| Triage vitals, mean (SD) | ||||
| SBP, mmHg | 186 (20.1) | 186 (19.9) | 191 (20.9) | <0.001 |
| DBP, mmHg | 108 (16.1) | 109 (15.7) | 102 (17.3) | <0.001 |
| Laboratory tests done, n (%) | 3579 (79.7) | 3061 (79.0) | 518 (84.6) | 0.001 |
| Serum creatinine, mg/dL, mean (SD) | 1.12 (1.5) | 1.04 (1.3) | 1.62 (2.0) | <0.001 |
| eGFR, mL/min/1.73 m2, mean (SD) | 84.6 (29.0) | 88.0 (27.0) | 66.0 (32.2) | <0.001 |
| Urinary analysis done, n (%) | 2194 (48.9) | 1862 (48.0) | 332 (54.2) | 0.004 |
| Proteinuria, n (%) | 626 (28.5) | 463 (24.9) | 163 (49.1) | <0.001 |
| Chest radiography done, n (%) | 3392 (75.6) | 2885 (74.4) | 507 (82.8) | <0.001 |
| Cardiomegaly, n (%) | 449 (12.9) | 340 (11.4) | 109 (21.1) | <0.001 |
| Congestion/fluid overload, n (%) | 4 (0.1) | 3 (0.1) | 1 (0.2) | 0.565 |
| ECG done, n (%) | 3094 (68.9) | 2585 (66.7) | 509 (83.2) | <0.001 |
| LVH, n (%) | 300 (9.7) | 232 (9.0) | 68 (13.4) | 0.002 |
| Myocardial ischemia, n (%) | 117 (3.8) | 85 (3.3) | 32 (6.3) | 0.001 |
| Atrial fibrillation, n (%) | 102 (3.3) | 67 (2.6) | 35 (6.9) | <0.001 |
| Brain imaging done, n (%) | 1246 (27.8) | 1089 (28.1) | 157 (25.7) | 0.210 |
| Abnormal findings, n (%) | 85 (5.4) | 71 (5.2) | 14 (6.8) | 0.340 |
| Chest and abdomen CT done, n (%) | 437 (9.7) | 320 (8.3) | 117 (19.1) | <0.001 |
| Echocardiography done, n (%) | 20 (0.4) | 17 (0.4) | 3 (0.5) | 0.859 |
| Fundoscopy done, n (%) | 71 (1.6) | 65 (1.7) | 6 (1.0) | 0.199 |
| Abnormal findings, n (%) | 7 (1.7) | 6 (1.7) | 1 (1.9) | 0.918 |
| Current antihypertensive medication, n (%) | 1149 (55.4) | 921 (54.5) | 228 (59.2) | 0.212 |
| ED antihypertensive medication, n (%) | 836 (18.6) | 710 (18.3) | 126 (20.6) | 0.180 |
| IV nicardipine | 381 (8.5) | 316 (8.2) | 65 (10.6) | 0.042 |
| IV labetalol | 13 (0.3) | 11 (0.3) | 2 (0.3) | 0.854 |
| IV esmolol | 5 (0.1) | 4 (0.1) | 1 (0.2) | 0.678 |
| IV nitroglycerin | 124 (2.8) | 91 (2.4) | 33 (5.4) | <0.001 |
| Oral calcium-channel blocker * | 395 (8.8) | 355 (9.2) | 40 (6.5) | 0.033 |
| Oral beta-blocker † | 66 (1.5) | 57 (1.5) | 9 (1.5) | 1 |
| Oral renin-angiotensin system inhibitor ↑ | 19 (0.4) | 16 (0.4) | 3 (0.5) | 0.784 |
| Oral nitroglycerin | 108 (2.4) | 98 (2.5) | 10 (1.6) | 0.180 |
| All Patients (n = 4488) | Survivor (n = 3876) | Non-Survivor (n = 612) | p-Value | |
|---|---|---|---|---|
| Hospital outcomes, n (%) | ||||
| Admission | 1200 (26.7) | 901 (23.2) | 299 (48.9) | <0.001 |
| Discharge | 2795 (62.3) | 2564 (66.2) | 231 (37.7) | <0.001 |
| Discharge against medical advice | 490 (10.9) | 411 (10.6) | 79 (12.9) | 0.089 |
| ED revisit within the time period, n (%) | ||||
| 1 month | 349 (10.6) | 279 (10.0) | 70 (14.4) | 0.004 |
| 3 months | 582 (17.7) | 448 (16.0) | 134 (27.5) | <0.001 |
| 1 year | 999 (30.4) | 774 (27.6) | 225 (46.2) | <0.001 |
| Readmission within the time period, n (%) | ||||
| 1 month | 237 (7.2) | 196 (7.0) | 41 (8.4) | 0.272 |
| 3 months | 327 (9.9) | 261 (9.3) | 66 (13.5) | 0.004 |
| 1 year | 485 (14.7) | 376 (13.4) | 109 (22.3) | <0.001 |
| Mortality within the time period, n (%) | ||||
| 1 month | 79 (1.8) | |||
| 3 months | 134 (3.0) | |||
| 1 year | 303 (6.8) | |||
| 3 years | 542 (12.1) |
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| HR (95% CI) | p-Value | Adjusted HR (95% CI) | p-Value | |
| Age (vs. <40 years) | ||||
| 40 to 59 years | 4.05 (1.86–8.80) | <0.001 | 2.38 (0.83–6.82) | 0.106 |
| ≥60 years | 22.08 (10.47–46.57) | <0.001 | 16.66 (6.20–44.80) | <0.001 |
| Male sex | 1.33 (1.13–1.58) | <0.001 | 1.54 (1.22–1.94) | <0.001 |
| SBP (per 1 mmHg) | 1.01 (1.01–1.02) | <0.001 | ||
| History of hypertension | 2.03 (1.70–2.43) | <0.001 | ||
| History of diabetes mellitus | 2.24 (1.88–2.67) | <0.001 | ||
| History of ischemic stroke | 3.22 (2.55–4.07) | <0.001 | ||
| History of hemorrhagic stroke | 1.95 (1.27–2.99) | 0.002 | ||
| History of coronary artery disease | 1.58 (1.18–2.11) | 0.002 | ||
| History of chronic kidney disease | 4.08 (3.26–5.11) | <0.001 | 2.18 (1.53–3.09) | <0.001 |
| Creatinine (per 1 mg/dL) | 1.15 (1.11–1.20) | <0.001 | ||
| Proteinuria | 2.72 (2.17–3.42) | <0.001 | 1.94 (1.53–2.48) | <0.001 |
| Cardiomegaly on chest radiography | 1.94 (1.55–2.43) | <0.001 | ||
| LVH on ECG | 1.57 (1.20–2.05) | <0.001 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, J.-H.; Kim, B.S.; Lyu, M.; Kim, H.-J.; Lee, J.H.; Park, J.-k.; Lim, Y.-H.; Shin, J. Clinical Characteristics and Predictors of All-Cause Mortality in Patients with Hypertensive Urgency at an Emergency Department. J. Clin. Med. 2021, 10, 4314. https://doi.org/10.3390/jcm10194314
Shin J-H, Kim BS, Lyu M, Kim H-J, Lee JH, Park J-k, Lim Y-H, Shin J. Clinical Characteristics and Predictors of All-Cause Mortality in Patients with Hypertensive Urgency at an Emergency Department. Journal of Clinical Medicine. 2021; 10(19):4314. https://doi.org/10.3390/jcm10194314
Chicago/Turabian StyleShin, Jeong-Hun, Byung Sik Kim, Minhyung Lyu, Hyun-Jin Kim, Jun Hyeok Lee, Jin-kyu Park, Young-Hyo Lim, and Jinho Shin. 2021. "Clinical Characteristics and Predictors of All-Cause Mortality in Patients with Hypertensive Urgency at an Emergency Department" Journal of Clinical Medicine 10, no. 19: 4314. https://doi.org/10.3390/jcm10194314
APA StyleShin, J.-H., Kim, B. S., Lyu, M., Kim, H.-J., Lee, J. H., Park, J.-k., Lim, Y.-H., & Shin, J. (2021). Clinical Characteristics and Predictors of All-Cause Mortality in Patients with Hypertensive Urgency at an Emergency Department. Journal of Clinical Medicine, 10(19), 4314. https://doi.org/10.3390/jcm10194314






