An Indication-Based Concept for Stepwise Spinal Orthosis in Low Back Pain According to the Current Literature
Abstract
:1. Introduction
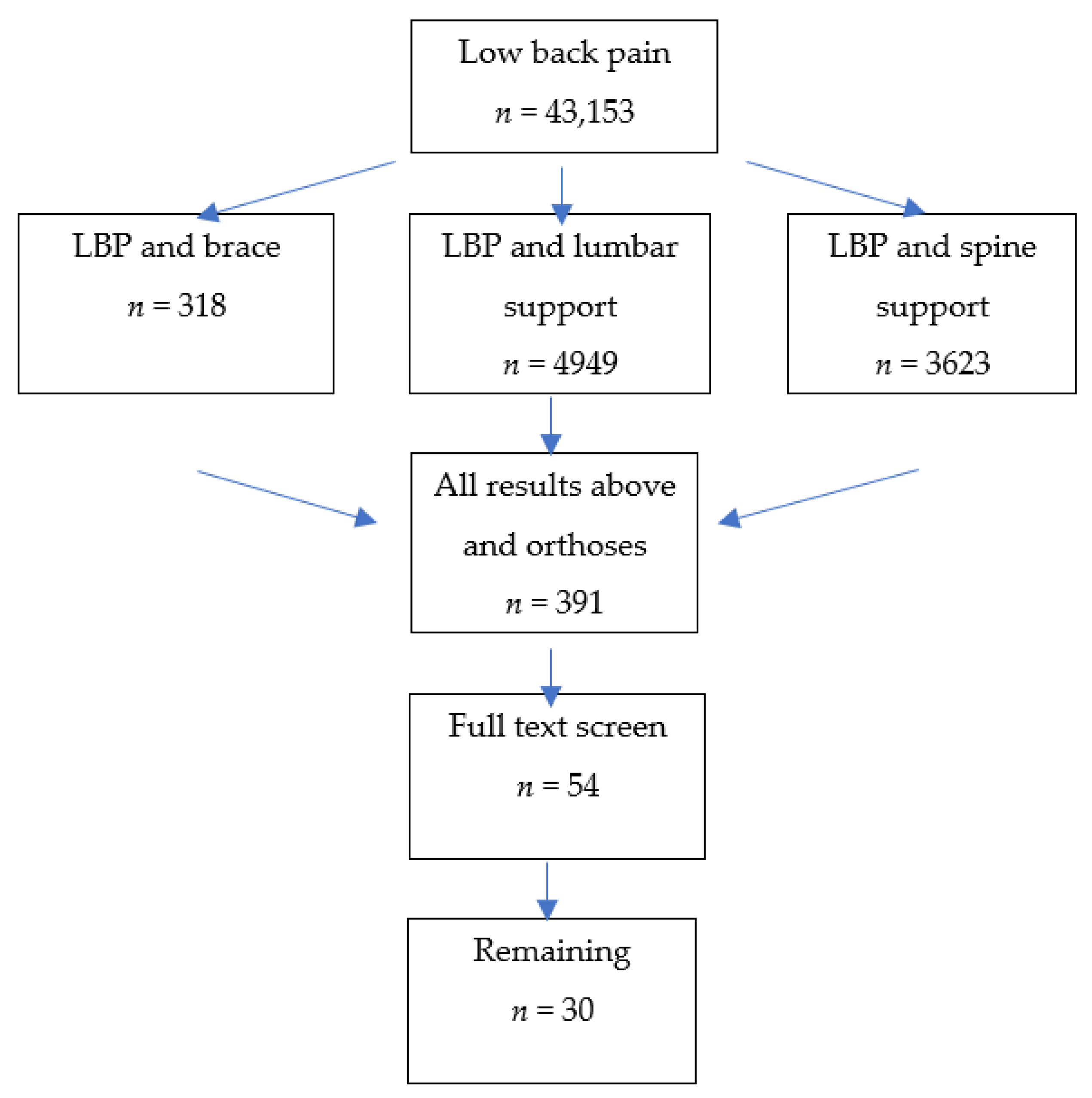
2. Methods
3. Results
3.1. Overview of the Current Literature
| Diagnosis | Orthosis | |
|---|---|---|
| Group A According to specific diagnosis | With effect [2,5,9,22,30] (retrospective study 28) | Group C Diagnosis based Orthosis |
| Without effect [20,23,25] | ||
| Group B Specific diagnosis is not given | With effect [3,4,7,21] | Group D Orthosis as unspecific treatment |
| Without effect [1,6,8,11,14,17,18,19] |
| Diagnosis | Orthosis | |
|---|---|---|
| Group A According to specific diagnosis | With effect [10] | Group C Diagnosis based Orthosis |
| Without effect [29] | ||
| Group B Specific diagnosis is not given | With effect - | Group D Orthosis as unspecific treatment |
| Without effect [12,13,15,16,24,26,27] |
3.2. Summary of the Literature and Whether It Supports the Indication of Spinal Orthosis Treatment in Low Back Pain
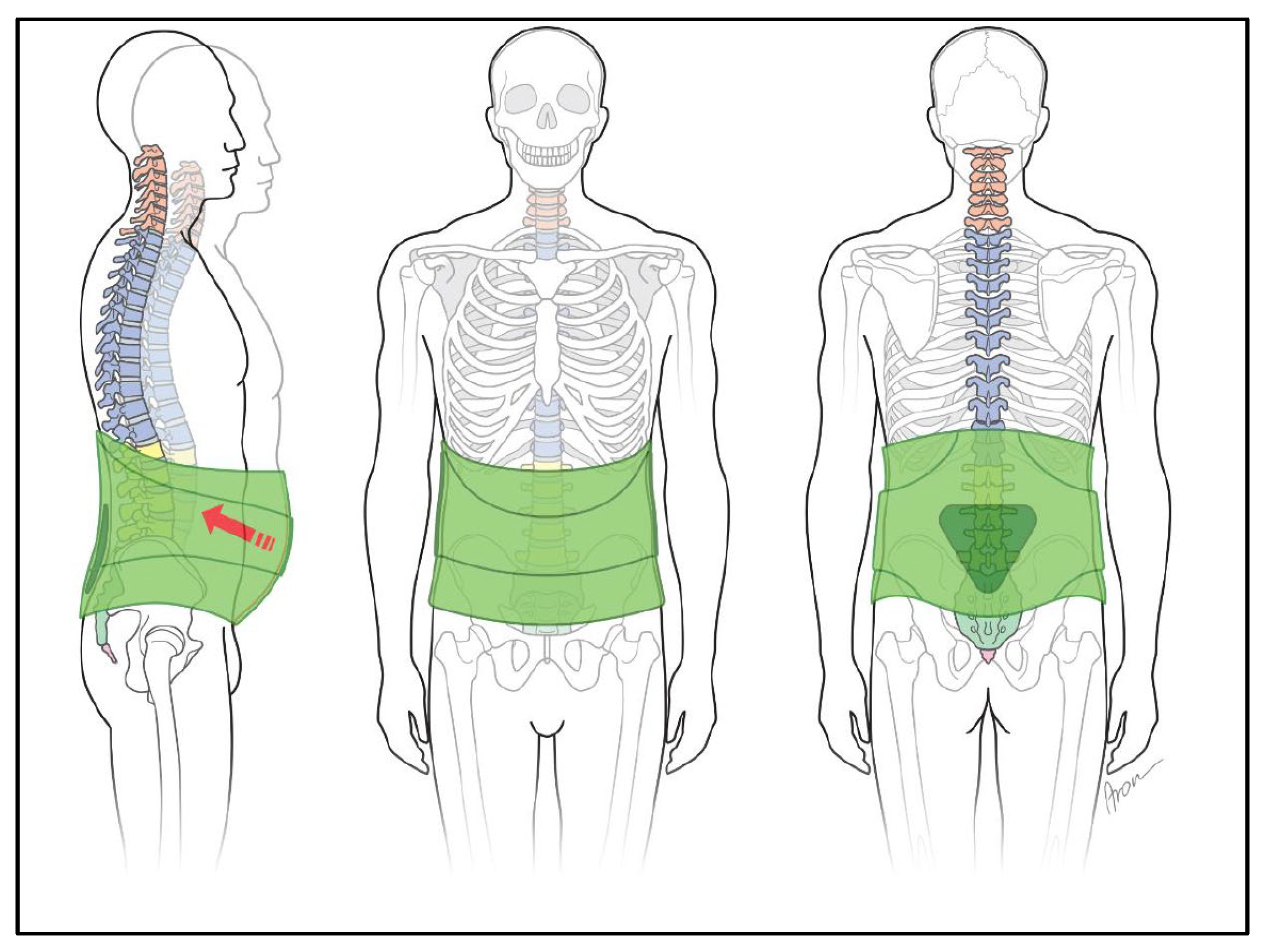
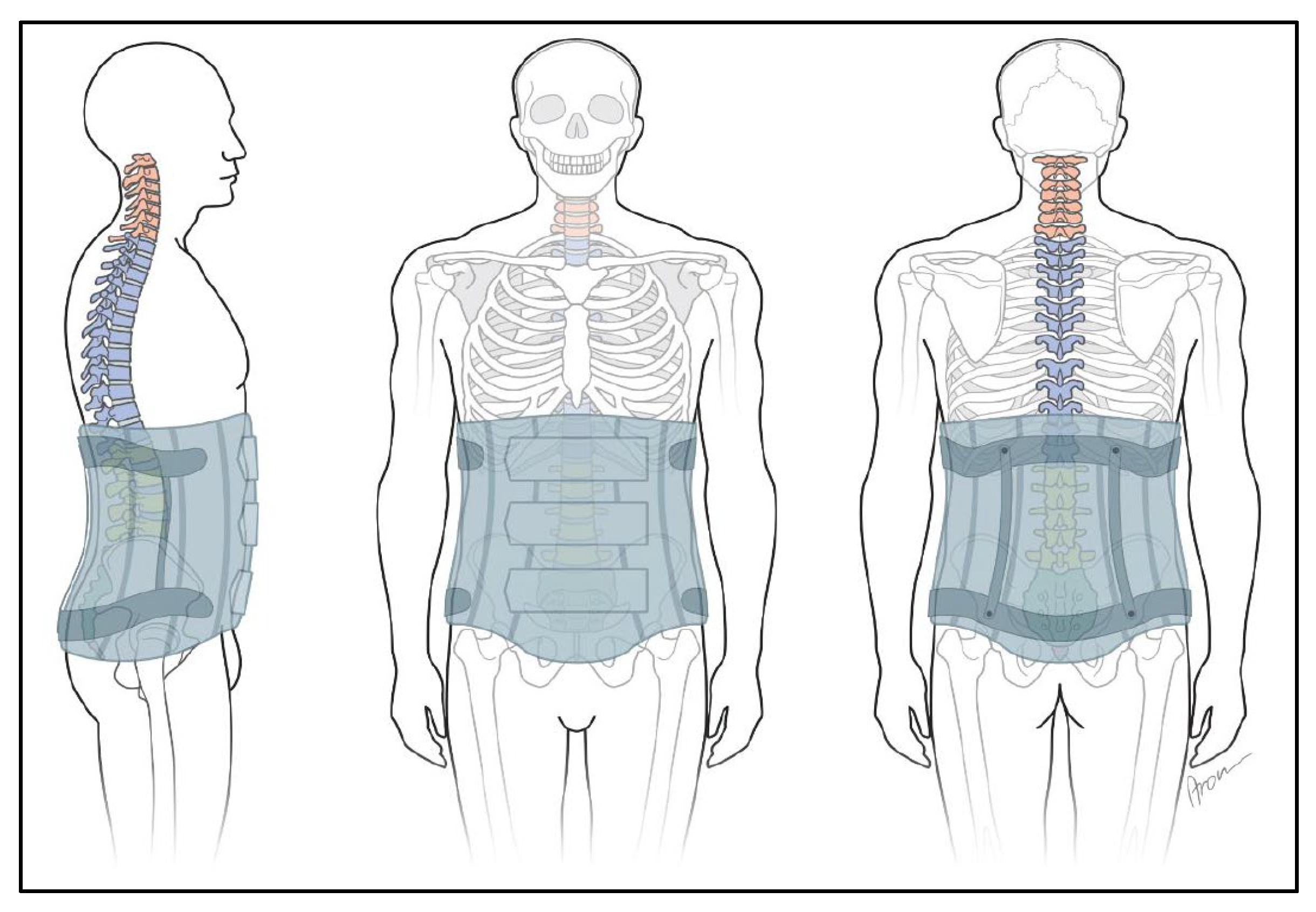
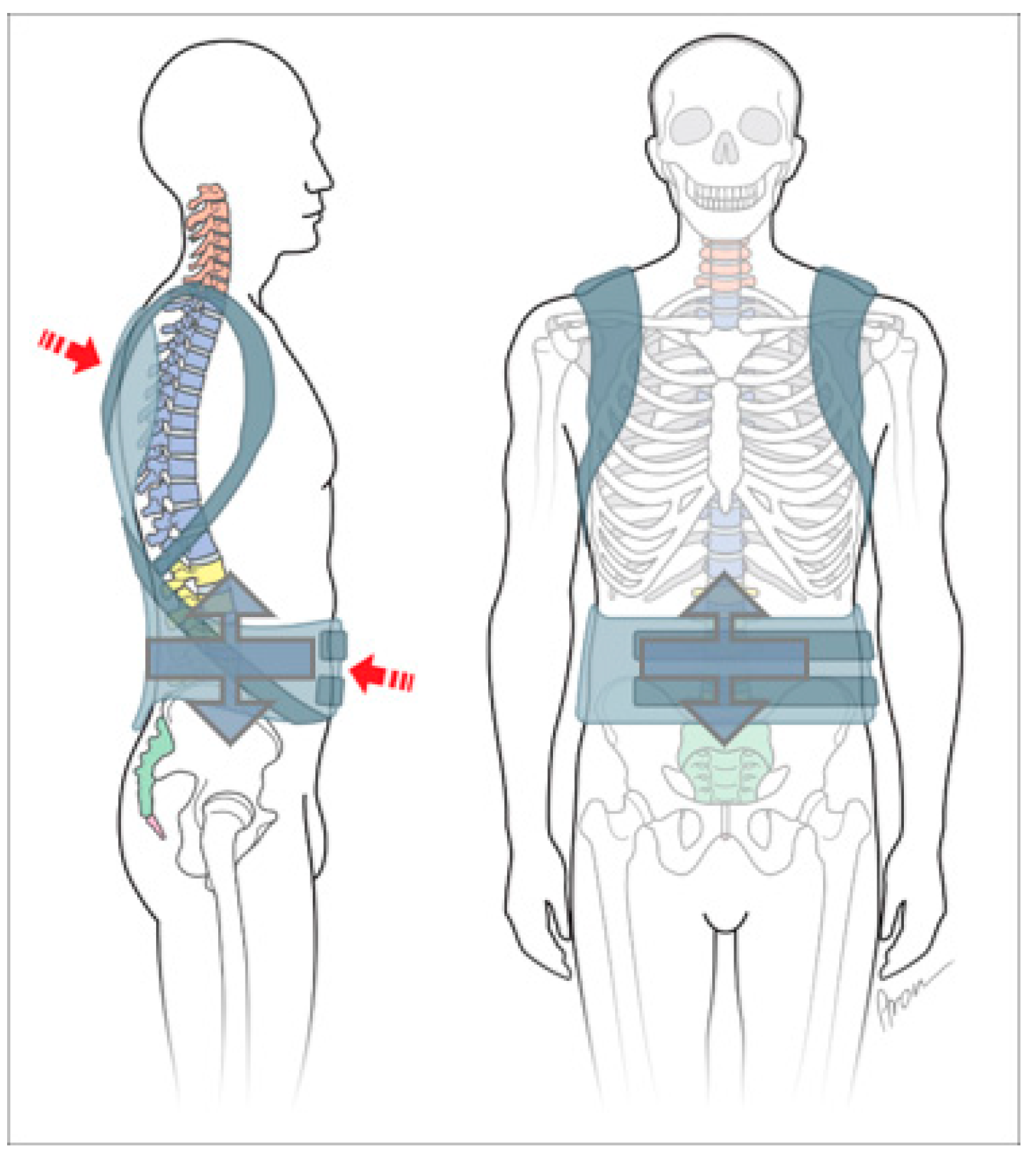
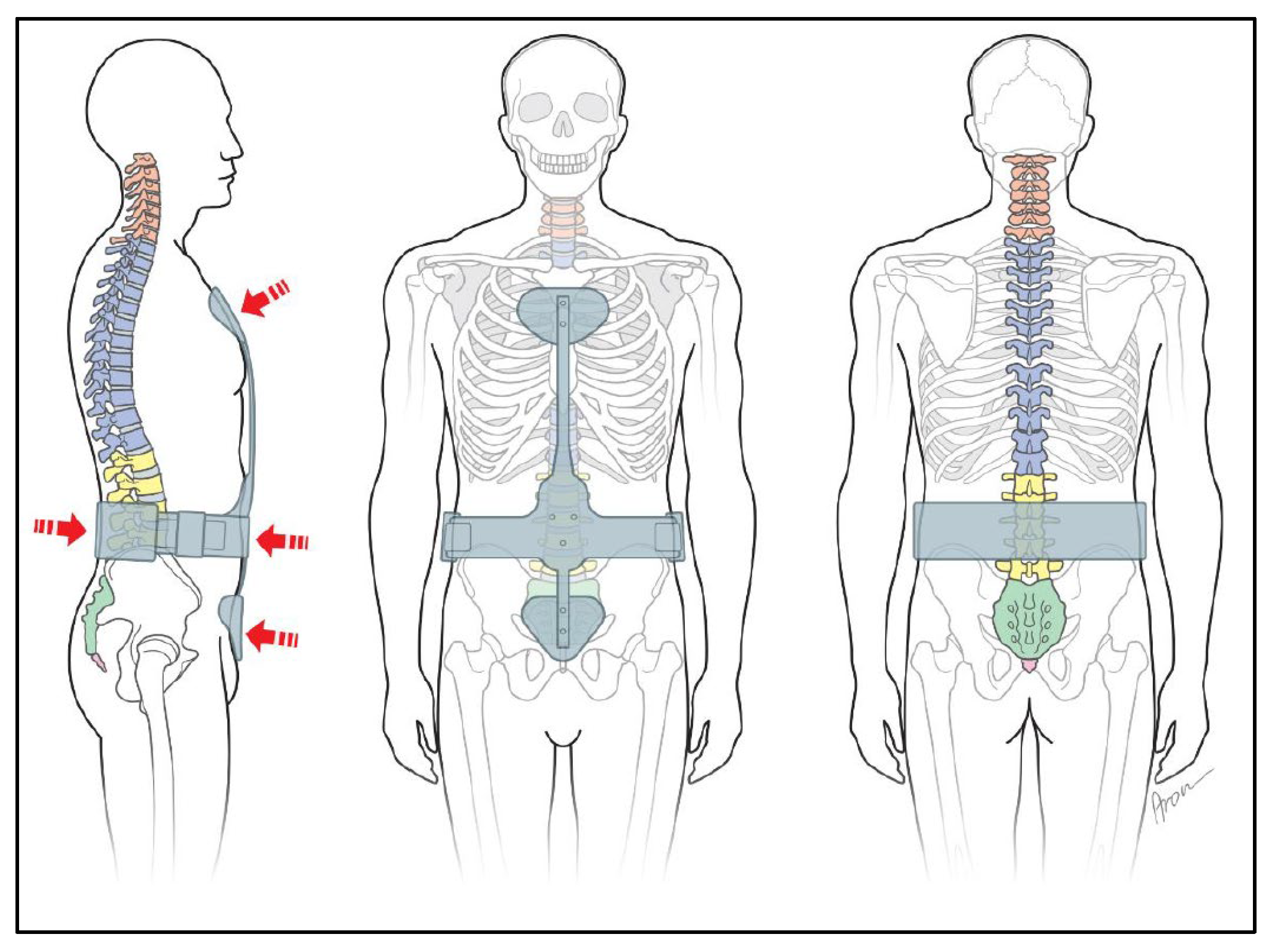
3.3. Differentiation of Spine Orthoses
| Diagnosis | Orthosis | ||||
|---|---|---|---|---|---|
| Summary | Back pain | Spinal orthosis | |||
| Local distribution | Cervical syndrome Dorsalgia Lumbalgia Sacralgia | Cervical orthosis (CO) Thoracic orthosis (TO) Lumbo-sacral orthosis (LSO) Sacro-iliac orthosis (SIO) | |||
| Combination | Thoraco-lumbar-sacral orthosis (TLSO) Cervico-thoraco-lumbo-sacral orthosis (CTLSO) | ||||
| Pathology | Diagnosis | Therapy | Mode of action | Product | |
| Muscle | Lumbalgia | Relief | Targeted force application via pads | Bandage | |
| Disc | Lumbalgia Lumboischialgia Instability | Stabilization Positioning | Delordosization through dorsal bridging | Bodice Corset Back brace Spinal orthosis | Depending on the necessary stability |
| Bone | Spondylarthrosis Baastrup | Position change | Delordosis | ||
| Osteochondrosis Osteoporosis | Stabilization | ||||
| Fracture Metastases | Stabilization Prevention | ||||
| Static | Hyperkyphosis Hyperlordosis Scoliosis | Position correction | |||
| Postoperative | Post segmental fusion | Stabilization Protect the adjacent segment Rapid mobilization | Local relief | Soft orthosis with struts | |
| Training device | Long-term treatment or prevention | Activation | Stimulators Assistive products | Wearables | |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bataller-Cervero, A.V.; Rabal-Pelay, J.; Roche-Seruendo, L.E.; Lacárcel-Tejero, B.; Alcázar-Crevillén, A.; Villalba-Ruete, J.A.; Cimarras-Otal, C. Effectiveness of lumbar supports in low back functionality and disability in assembly-line workers. Ind. Health 2019, 57, 588–595. [Google Scholar] [CrossRef] [Green Version]
- Junji, K.; Ko, M.; Tadashi, Y.; Shinno, I.; Akihiro, I. Efficacy of a trunk orthosis with joints providing resistive force on low-back load in elderly persons during static standing. Clin. Interv. Aging. 2015, 10, 1413–1420. [Google Scholar]
- Pape, J.L.; Brism, J.M.; Sizer, P.S.; Matthijs, O.C.; Browne, K.L.; Dewan, B.M.; Sobczak, S. Increased spinal height using propped slouched sitting postures: Innovative ways to rehydrate intervertebral discs. Appl. Ergon. 2018, 66, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Shahvarpoura, A.; Preuss, R.; Sullivanc, M.J.; Negrinia, A.; Larivièrea, C. The effect of wearing a lumbar belt on biomechanical and psychological outcomes related to maximal flexion-extension motion and manual material handling. Appl. Ergon. 2018, 69, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Klima, S.; Grunert, R.; Ondruschka, B.; Scholze, M.; Seidel, T.; Werner, M.; Hammer, N. Pelvic orthosis effects on posterior pelvis kinematics: An in-vitro biomechanical study. Sci. Rep. 2018, 8, 15980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mi, J.; Ye, J.; Zhao, X.; Zhao, J. Effects of lumbosacral orthoses on postural control in individuals with or without non-specific low back pain. Eur. Spine J. 2018, 27, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Lamers, E.P.; Soltys, J.C.; Keaton, L.; Scherpereel, K.L.; Yang, A.J.; Zelik, K.E. Low-profile elastic exosuit reduces back muscle fatigue. Sci. Rep. 2020, 10, 15958. [Google Scholar] [CrossRef]
- Annaswamy, T.; Cunniff, K.; Kroll, M.; Yap, L.; Hasley, M.; Lin, C.; Petrasic, J. Lumbar Bracing for Chronic Low Back Pain. Am. J. Phys. Med. Rehabil. 2021, 100, 742–749. [Google Scholar] [CrossRef]
- Urquhart, J.C.; Alrehaili, O.A.; Fisher, C.G.; Fleming, A.; Rasoulinejad, P.; Gurr, K.; Bailey, S.I.; Siddiqi, F.; Bailey, C.S. Treatment of thoracolumbar burst fractures: Extended follow-up of a randomized clinical trial comparing orthosis versus no orthosis. J. Neurosurg. Spine 2017, 27, 42–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulcahy, M.J.; Dower, A.; Tait, M. Orthosis versus no orthosis for the treatment of thoracolumbar burst fractures: A systematic review. J. Clin. Neurosci. 2021, 85, 49–56. [Google Scholar] [CrossRef]
- Ballard, M.T.; Drury, C.; Bazrgari, B. Changes in Lumbo-Pelvic Coordination of Individuals with and without Low Back Pain When Wearing a Hip Orthosis Frontiers in Sports and Active Living. Available online: www.frontiersin.org (accessed on 1 July 2020).
- Krismer, M.; van Tulder, M. Low back pain (non-specific). Best Pract. Res. Clin. Rheumatol. 2007, 21, 77–91. [Google Scholar] [CrossRef]
- Kreiner, D.S.; Matz, P.; Bono, C.M.; Cho, C.H.; Easa, J.E.; Ghiselli, G.; Ghogawala, Z.; Reitman, C.A.; Resnick, D.K.; Watters, W.C., III; et al. Guideline summary review: An evidence-based clinical guideline for the diagnosis and treatment of low back pain. Spine J. 2020, 20, 998–1024. [Google Scholar] [CrossRef]
- Azadinia, F.; Ebrahimi-Takamjani, I.; Kamyab, M.; Asgari, M.; Parnianpour, M. Effects of lumbosacral orthosis on dynamical structure of center of pressure fluctuations in patients with non-specific chronic low back pain: A randomized controlled trial. J. Bodyw. Mov. Ther. 2019, 23, 930–936. [Google Scholar] [CrossRef] [PubMed]
- Van Duijvenbode, I.; Jellema, P.; van Poppel, M.; van Tulder, M.W. Lumbar supports for prevention and treatment of low back pain. Cochrane Database Syst. Rev. 2008, 2, CD001823. [Google Scholar] [CrossRef] [PubMed]
- Takasaki, H.; Miki, T. The impact of continuous use of lumbosacral orthoses on trunk motor performance: A systematic review with meta-analysis. Spine J. 2017, 17, 889–900. [Google Scholar] [CrossRef] [PubMed]
- Samania, M.; Shirazib, Z.R.; Hadadic, M.; Sobhanib, S. A randomized controlled trial comparing the long-term use of soft lumbosacral orthoses at two different pressures in patients with chronic nonspecific low back pain. Clin. Biomech. 2019, 69, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Anders, C.; Agnes Hübner, A. Influence of elastic lumbar support belts on trunk muscle function in patients with nonspecific acute lumbar back pain. PLoS ONE 2019, 14, e0211042. [Google Scholar] [CrossRef]
- Azadinia, F.; Takamjani, I.E.; Kamyab, M.; Kalbassi, G.; Sarrafzadeh, J.; Parnianpour, M. The Effect of Lumbosacral Orthosis on the Thickness of Deep Trunk Muscles Using Ultrasound Imaging. Am. J. Phys. Med. Rehabil. 2019, 98, 536–544. [Google Scholar] [CrossRef]
- Zoia, C.; Bongetta, D.; Alicino, C.; Chimenti, M.; Pugliese, R.; Gaetani, P. Usefulness of corset adoption after single-level lumbar discectomy: A randomized controlled trial. J. Neurosurg. Spine 2018, 28, 481–485. [Google Scholar] [CrossRef]
- Goto, T.; Sakai, T.; Sugiura, K.; Manabe, H.; Tezuka, F.; Yamashita, K.; Takata, Y.; Katoh, S.; Sairyo, K. A semi-rigid thoracolumbar orthosis fitted immediately after spinal surgery: Stabilizing effects and patient satisfaction. J. Med. Investig. 2019, 66, 275–279. [Google Scholar] [CrossRef]
- Smits, A.J.; Deunk, J.; Stadhouder, A.; Altena, M.C.; Hendrik, D.; Kempen, R.; Willem Bloemers, F.W. Is postoperative bracing after pedicle screw fixation of spine fractures necessary? Study protocol of the ORNOT study: A randomised controlled multicentre trial. BMJ Open 2018, 8, 1–8. [Google Scholar] [CrossRef]
- Fujiwara, H.; Makino, T.; Yonenobu, K.; Moriguchi, Y.; Oda, T.; Kaito, T. Efficacy of lumbar orthoses after posterior lumbar interbody fusion—a prospective randomized study. Medicine 2019, 98, 1–7. [Google Scholar] [CrossRef]
- Bogaert, L.; Van Wambeke, P.; Thys, T.; Swinnen, T.W.; Dankaerts, W.; Brumagne, S.; Moke, L.; Peers, K.; Depreitere, B.; Janssens, L. Postoperative bracing after lumbar surgery: A survey amongst spinal surgeons in Belgium. Eur. Spine J. 2019, 28, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Soliman, H.A.; Barchi, S.; Parent, S.; Maurais, G.; Jodoin, A.; Mac-Thiong, J.M. Early Impact of Postoperative Bracing on Pain and Quality of Life After Posterior Instrumented Fusion for Lumbar Degenerative Conditions. Spine J. 2018, 43, 155–160. [Google Scholar] [CrossRef]
- Myung, E.; Neto, J.D.; Murta, G.A.; Vieira, A.; de Lima, P.R.G.; Lessa, L.; Bernardo, W.M. ANAMT Technical Guideline (DT 05): Prevention of occupational low back pain through back belts, lumbar support or braces. Rev. Bras. Med. Trab. 2018, 16, 524–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schott, C.; Zirke, S.; Schmelzle, J.M.; Kaiser, C.; Fernández, L.A. Effectiveness of lumbar orthoses in low back pain: Review of the literature and our results. Orthop. Rev. 2018, 10, 7791. [Google Scholar] [CrossRef] [Green Version]
- Boutevillain, L.; Bonnin, A.; Chabaud, A.; Morel, C.; Giustiniani, M.; Pereira, B.; Soubrier, M.; Coudeyre, E. Short-term pain evolution in chronic low back pain with Modic type 1 changes treated by a lumbar rigid brace: A retrospective study. Ann. Phys. Rehabil. Med. 2019, 62, 3–7. [Google Scholar] [CrossRef]
- Zaina, F.; Tomkins-Lane, C.; Carragee, E.; Negrini, S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst. Rev. 2016, 1, 1–49. [Google Scholar] [CrossRef]
- Alin, C.K.; Uzunel, E.; Kronhed, A.-C.G.; Alinaghizadeh, H.; Salminen, H. Effect of treatment on back pain and back extensor strength with a spinal orthosis in older women with osteoporosis: A randomized controlled trial. Arch. Osteoporos. 2019, 14, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landauer, F.; Trieb, K. An Indication-Based Concept for Stepwise Spinal Orthosis in Low Back Pain According to the Current Literature. J. Clin. Med. 2022, 11, 510. https://doi.org/10.3390/jcm11030510
Landauer F, Trieb K. An Indication-Based Concept for Stepwise Spinal Orthosis in Low Back Pain According to the Current Literature. Journal of Clinical Medicine. 2022; 11(3):510. https://doi.org/10.3390/jcm11030510
Chicago/Turabian StyleLandauer, Franz, and Klemens Trieb. 2022. "An Indication-Based Concept for Stepwise Spinal Orthosis in Low Back Pain According to the Current Literature" Journal of Clinical Medicine 11, no. 3: 510. https://doi.org/10.3390/jcm11030510
APA StyleLandauer, F., & Trieb, K. (2022). An Indication-Based Concept for Stepwise Spinal Orthosis in Low Back Pain According to the Current Literature. Journal of Clinical Medicine, 11(3), 510. https://doi.org/10.3390/jcm11030510





