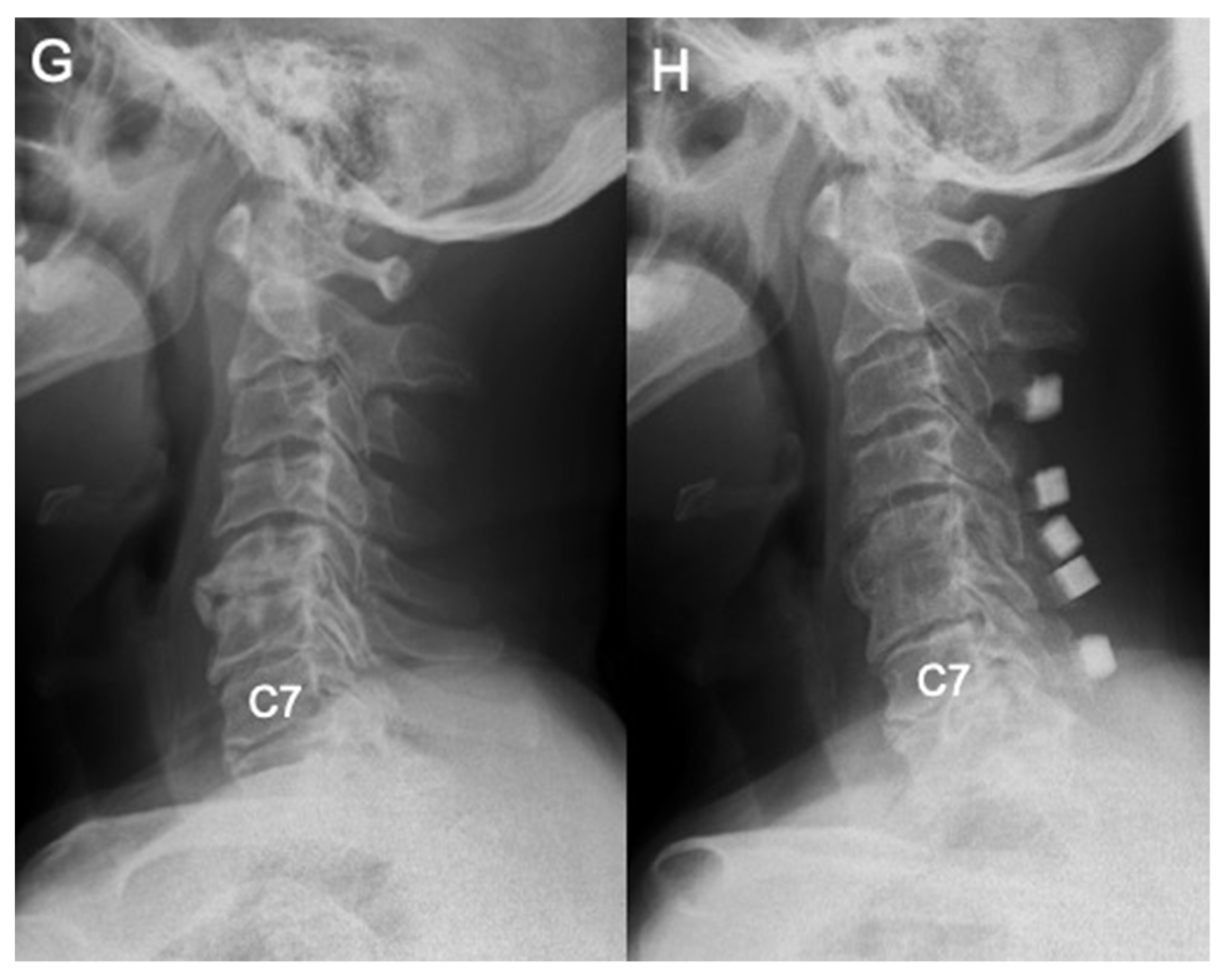
Differences in Demographic and Radiographic Characteristics between Patients with Visible and Invisible T1 Slopes on Lateral Cervical Radiographic Images
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics Approval
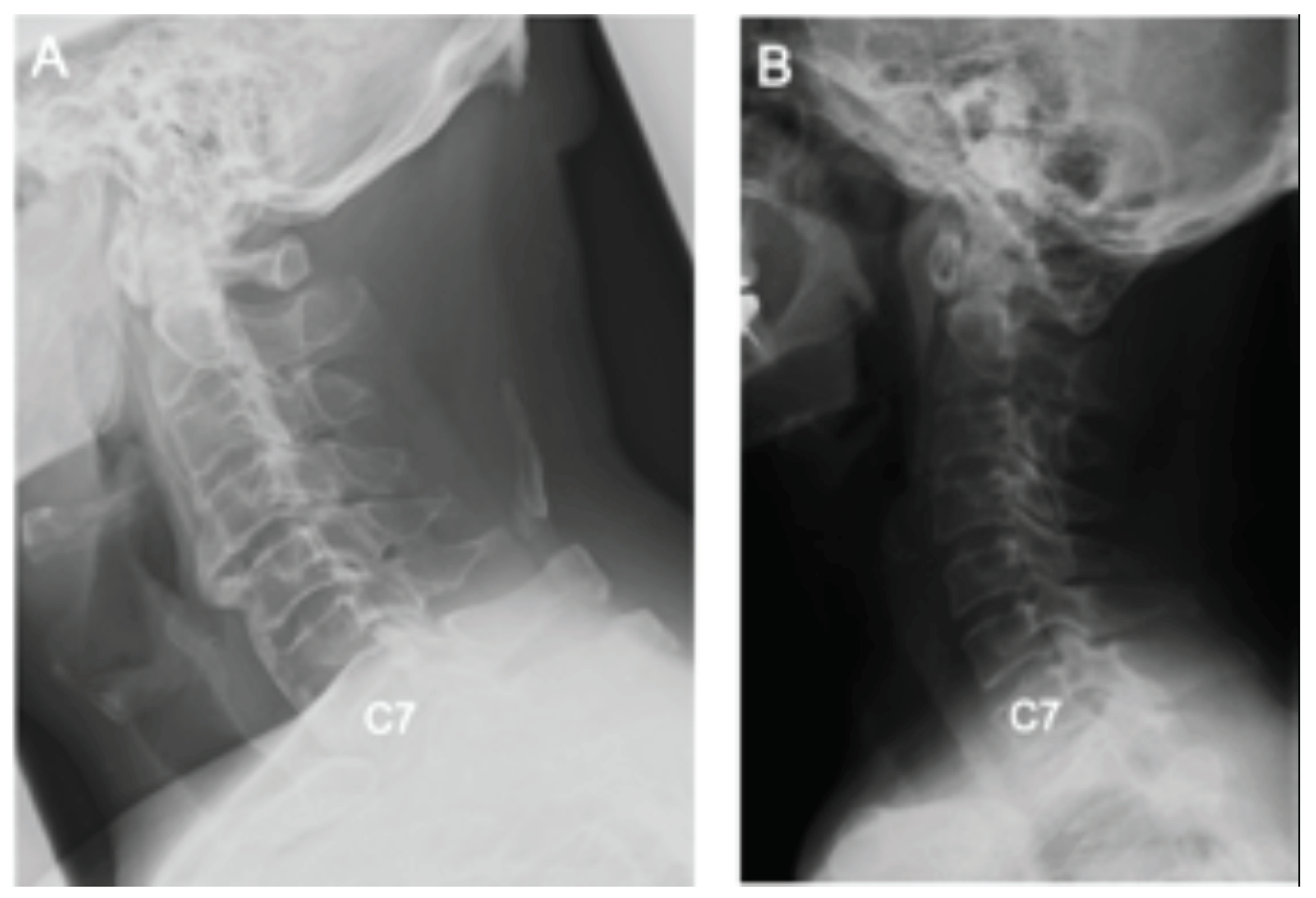
2.2. Radiological Assessment
2.3. Statistical Analyses
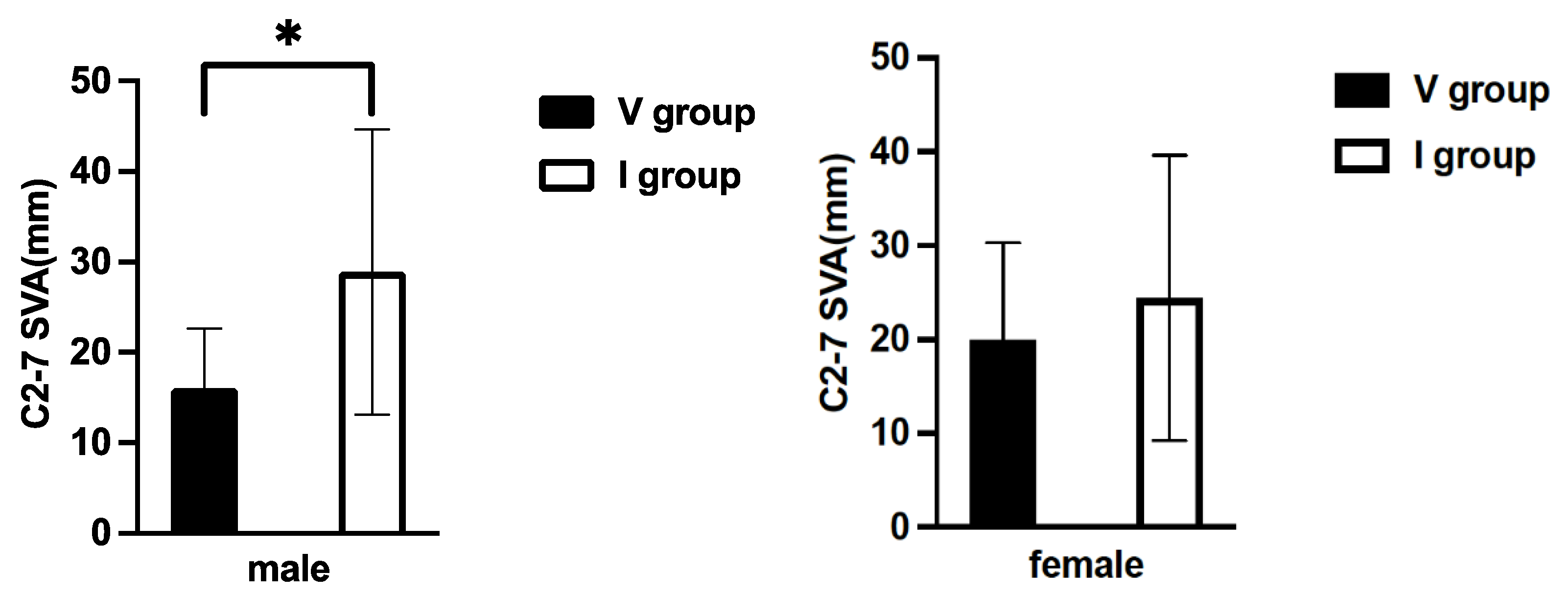
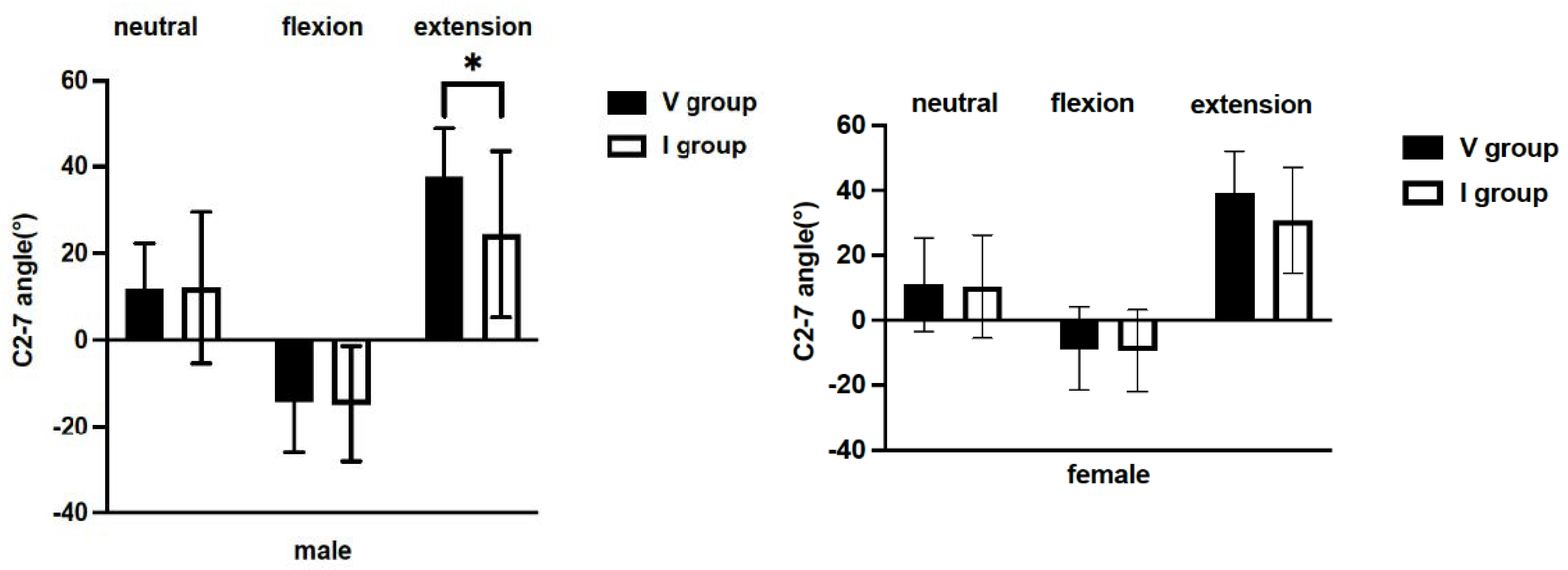
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Knott, P.T.; Mardjetko, S.M.; Techy, F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010, 10, 994–998. [Google Scholar] [CrossRef] [PubMed]
- Jun, H.S.; Kim, J.H.; Ahn, J.H.; Chang, I.B.; Song, J.H.; Kim, T.H.; Park, M.S.; Kim, Y.C.; Kim, S.W.; Oh, J.K. T1 slope and degenerative cervical spondylolisthesis. Spine 2015, 40, E220–E226. [Google Scholar] [CrossRef]
- Lee, S.H.; Son, E.S.; Seo, E.M.; Suk, K.S.; Kim, K.T. Factors determining cervical spine sagittal balance in asymptomatic adults: Correlation with spinopelvic balance and thoracic inlet alignment. Spine J. 2015, 15, 705–712. [Google Scholar] [CrossRef]
- Protopsaltis, T.S.; Soroceanu, A.; Tishelman, J.C.; Buckland, A.J.; Mundis, G.M., Jr.; Smith, J.S.; Daniels, A.; Lenke, L.G.; Kim, H.J.; Klineberg, E.O.; et al. Should Sagittal Spinal Alignment Targets for Adult Spinal Deformity Correction Depend on Pelvic Incidence and Age? Spine 2020, 45, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Terran, J.; Schwab, F.; Shaffrey, C.I.; Smith, J.S.; Devos, P.; Ames, C.P.; Fu, K.M.; Burton, D.; Hostin, R.; Klineberg, E.; et al. The SRS-Schwab adult spinal deformity classification: Assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery 2013, 73, 559–568. [Google Scholar] [CrossRef] [Green Version]
- Protopsaltis, T.; Schwab, F.; Bronsard, N.; Smith, J.S.; Klineberg, E.; Mundis, G.; Ryan, D.J.; Hostin, R.; Hart, R.; Burton, D.; et al. TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J. Bone Jt. Surg. Am. 2014, 96, 1631–1640. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Lee, S.Y.; Kim, Y.C.; Park, M.S.; Kim, S.W. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine 2013, 38, E992–E997. [Google Scholar] [CrossRef] [PubMed]
- Oe, S.; Yamato, Y.; Togawa, D.; Kurosu, K.; Mihara, Y.; Banno, T.; Yasuda, T.; Kobayashi, S.; Hasegawa, T.; Matsuyama, Y. Preoperative T1 Slope More Than 40° as a Risk Factor of Correction Loss in Patients with Adult Spinal Deformity. Spine 2016, 41, E1168–E1176. [Google Scholar] [CrossRef]
- Cho, J.H.; Ha, J.K.; Kim, D.G.; Song, K.Y.; Kim, Y.T.; Hwang, C.J.; Lee, C.S.; Lee, D.H. Does preoperative T1 slope affect radiological and functional outcomes after cervical laminoplasty? Spine 2014, 39, E1575–E1581. [Google Scholar] [CrossRef]
- Jun, H.S.; Chang, I.B.; Song, J.H.; Kim, T.H.; Park, M.S.; Kim, S.W.; Oh, J.K. Is it possible to evaluate the parameters of cervical sagittal alignment on cervical computed tomographic scans? Spine 2014, 39, E630–E636. [Google Scholar] [CrossRef]
- Park, J.H.; Cho, C.B.; Song, J.H.; Kim, S.W.; Ha, Y.; Oh, J.K. T1 Slope and Cervical Sagittal Alignment on Cervical CT Radiographs of Asymptomatic Persons. J. Korean Neurosurg. Soc. 2013, 53, 356–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inoue, T.; Ando, K.; Kobayashi, K.; Nakashima, H.; Ito, K.; Katayama, Y.; Machino, M.; Kanbara, S.; Ito, S.; Yamaguchi, H.; et al. Age-related Changes in T1 and C7 Slope and the Correlation Between Them in More Than 300 Asymptomatic Subjects. Spine 2021, 46, E474–E481. [Google Scholar] [CrossRef] [PubMed]
- Park, B.J.; Gold, C.J.; Woodroffe, R.W.; Yamaguchi, S. What is the most accurate substitute for an invisible T1 slope in cervical radiographs? A comparative study of a novel method with previously reported substitutes. J. Neurosurg. Spine 2021, 1, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Weng, C.; Wang, J.; Tuchman, A.; Wang, J.; Fu, C.; Hsieh, P.C.; Buser, Z.; Wang, J.C. Influence of T1 Slope on the Cervical Sagittal Balance in Degenerative Cervical Spine: An Analysis Using Kinematic MRI. Spine 2016, 41, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Yang, C.; Zhai, X.; Zhao, J.; Zhu, X.; Li, M. Analysis of Factors Associated With Sagittal Balance in Normal Asymptomatic Individuals: A Retrospective Study in a Population of East China. Spine 2017, 42, E219–E225. [Google Scholar] [CrossRef]
- Lee, D.H.; Park, S.; Kim, D.G.; Hwang, C.J.; Lee, C.S.; Hwang, E.S.; Cho, J.H. Cervical spine lateral radiograph versus whole spine lateral radiograph: A retrospective comparative study to identify a better modality to assess cervical sagittal alignment. Medicine 2021, 100, e25987. [Google Scholar] [CrossRef]
- Gelb, D.E.; Lenke, L.G.; Bridwell, K.H.; Blanke, K.; McEnery, K.W. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine 1995, 20, 1351–1358. [Google Scholar] [CrossRef]
- Lee, H.J.; You, S.T.; Sung, J.H.; Kim, I.S.; Hong, J.T. Analyzing the Significance of T1 Slope minus Cervical Lordosis in Patients with Anterior Cervical Discectomy and Fusion Surgery. J. Korean Neurosurg. Soc. 2021, 64, 913–921. [Google Scholar] [CrossRef]
- Xing, R.; Zhou, G.; Chen, Q.; Liang, Y.; Dong, J. MRI to measure cervical sagittal parameters: A comparison with plain radiographs. Arch. Orthop. Trauma Surg. 2017, 137, 451–455. [Google Scholar] [CrossRef]
- Tamai, K.; Buser, Z.; Paholpak, P.; Sessumpun, K.; Nakamura, H.; Wang, J.C. Can C7 Slope Substitute the T1 slope?: An Analysis Using Cervical Radiographs and Kinematic MRIs. Spine 2018, 43, 520–525. [Google Scholar] [CrossRef]
- Le Huec, J.C.; Demezon, H.; Aunoble, S. Sagittal parameters of global cervical balance using EOS imaging: Normative values from a prospective cohort of asymptomatic volunteers. Eur. Spine J. 2015, 24, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Garg, B.; Mehta, N.; Bansal, T.; Malhotra, R. EOS® imaging: Concept and current applications in spinal disorders. J. Clin. Orthop. Trauma 2020, 11, 786–793. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, J.; Marsh, D.; Koller, H.; Zenenr, J.; Bannister, G. Cervical range of movement in relation to neck dimension. Eur. Spine J. 2009, 18, 863–868. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ben-Noun, L.; Sohar, E.; Laor, A. Neck circumference as a simple screening measure for identifying overweight and obese patients. Obes Res. 2001, 9, 470–477. [Google Scholar] [CrossRef]
- Kato, M.; Namikawa, T.; Matsumura, A.; Konishi, S.; Nakamura, H. Effect of Cervical Sagittal Balance on Laminoplasty in Patients With Cervical Myelopathy. Glob. Spine J. 2017, 7, 154–161. [Google Scholar] [CrossRef] [Green Version]
- Ames, C.P.; Smith, J.S.; Eastlack, R.; Blaskiewicz, D.J.; Shaffrey, C.I.; Schwab, F.; Bess, S.; Kim, H.J.; Mundis, G.M., Jr.; Klineberg, E.; et al. Reliability assessment of a novel cervical spine deformity classification system. J. Neurosurg. Spine 2015, 23, 673–683. [Google Scholar] [CrossRef] [Green Version]

| Total (n = 60) | Male (n = 30) | Female (n = 30) | p-Value | |
|---|---|---|---|---|
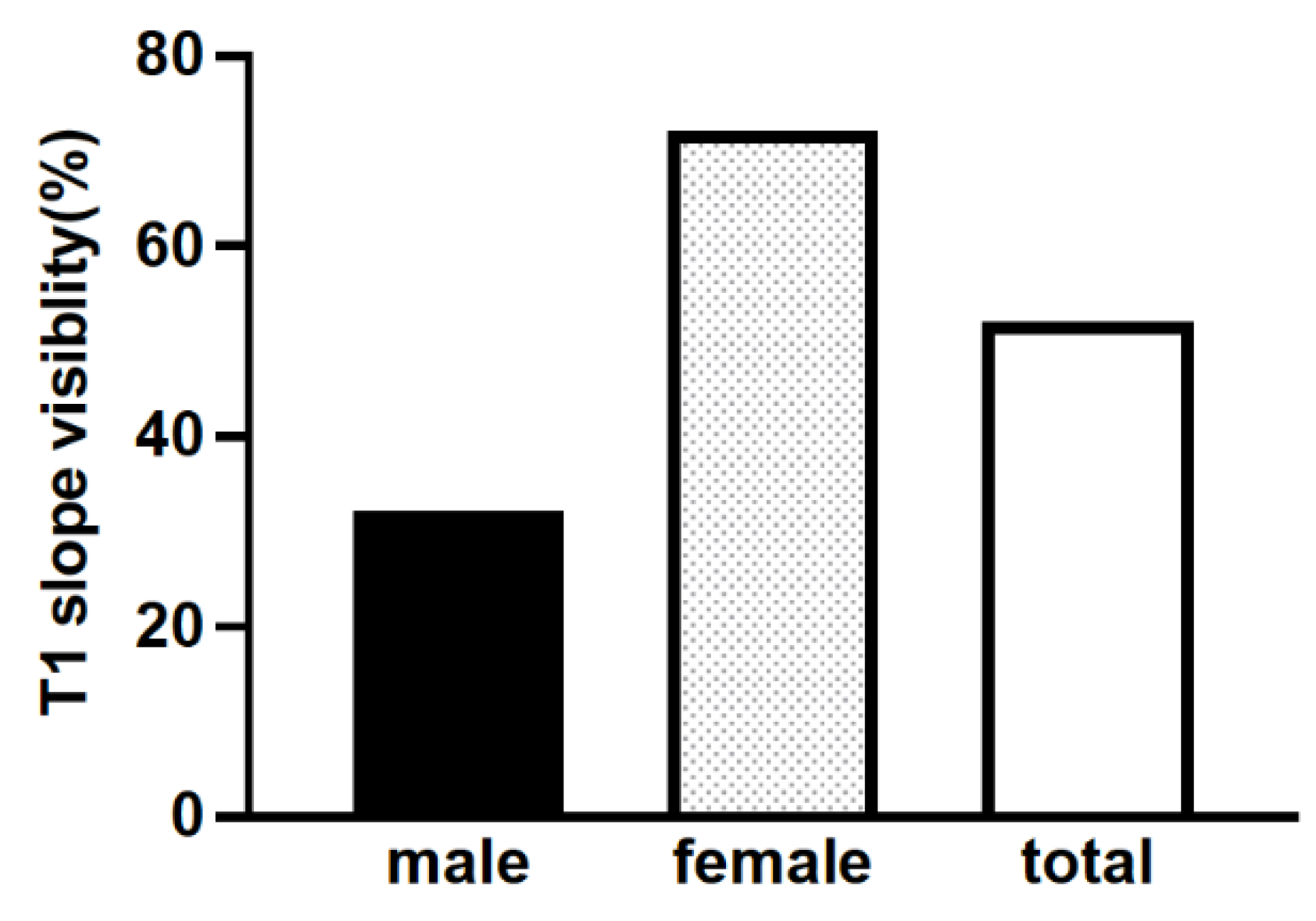
| T1 slope visibility (V group/I group) | 53.3% (32/28) | 33.3% (10/20) | 73.3% (22/8) | <0.05 |
| No. of Patients | |||
|---|---|---|---|
| Disorder | Total | V Group | I Group |
| Degenerative disorders | 28 | 15 | 13 |
| Spinal cord tumors | 9 | 5 | 4 |
| OPLL | 14 | 8 | 6 |
| Others | 9 | 4 | 5 |
| No. of Patients | |||
|---|---|---|---|
| Treatment | Total | V Group | I Group |
| Surgical treatment | 23 | 12 | 11 |
| Conservative treatment | 37 | 20 | 17 |
| Total | Visible (V group) | Invisible (I Group) | p-Value | |
|---|---|---|---|---|
| Age (years) | 44.5 ± 11.1 | 44.4 ± 12.5 | 44.6 ± 8.3 | n.s. |
| BMI | 21.6 ± 2.4 | 21.2 ± 2.3 | 22.1 ± 2.5 | n.s. |
| Male:Female | 30:30 | 10:22 | 20:8 | <0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ito, S.; Nakashima, H.; Matsumoto, A.; Ando, K.; Machino, M.; Segi, N.; Tomita, H.; Koshimizu, H.; Imagama, S. Differences in Demographic and Radiographic Characteristics between Patients with Visible and Invisible T1 Slopes on Lateral Cervical Radiographic Images. J. Clin. Med. 2022, 11, 411. https://doi.org/10.3390/jcm11020411
Ito S, Nakashima H, Matsumoto A, Ando K, Machino M, Segi N, Tomita H, Koshimizu H, Imagama S. Differences in Demographic and Radiographic Characteristics between Patients with Visible and Invisible T1 Slopes on Lateral Cervical Radiographic Images. Journal of Clinical Medicine. 2022; 11(2):411. https://doi.org/10.3390/jcm11020411
Chicago/Turabian StyleIto, Sadayuki, Hiroaki Nakashima, Akiyuki Matsumoto, Kei Ando, Masaaki Machino, Naoki Segi, Hiroyuki Tomita, Hiroyuki Koshimizu, and Shiro Imagama. 2022. "Differences in Demographic and Radiographic Characteristics between Patients with Visible and Invisible T1 Slopes on Lateral Cervical Radiographic Images" Journal of Clinical Medicine 11, no. 2: 411. https://doi.org/10.3390/jcm11020411
APA StyleIto, S., Nakashima, H., Matsumoto, A., Ando, K., Machino, M., Segi, N., Tomita, H., Koshimizu, H., & Imagama, S. (2022). Differences in Demographic and Radiographic Characteristics between Patients with Visible and Invisible T1 Slopes on Lateral Cervical Radiographic Images. Journal of Clinical Medicine, 11(2), 411. https://doi.org/10.3390/jcm11020411






