Efficacy of Fu’s Subcutaneous Needling in Treating Soft Tissue Pain of Knee Osteoarthritis: A Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
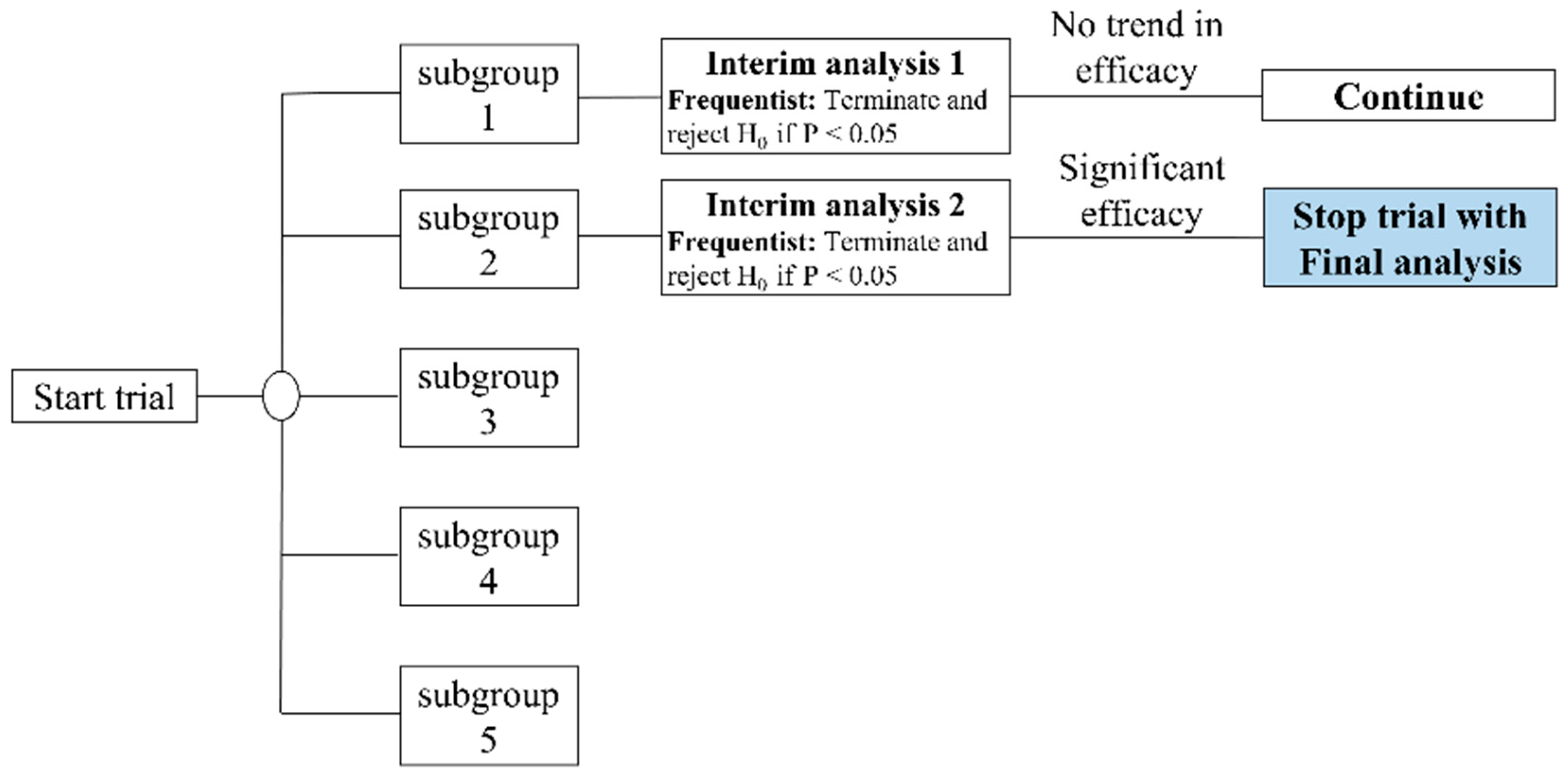
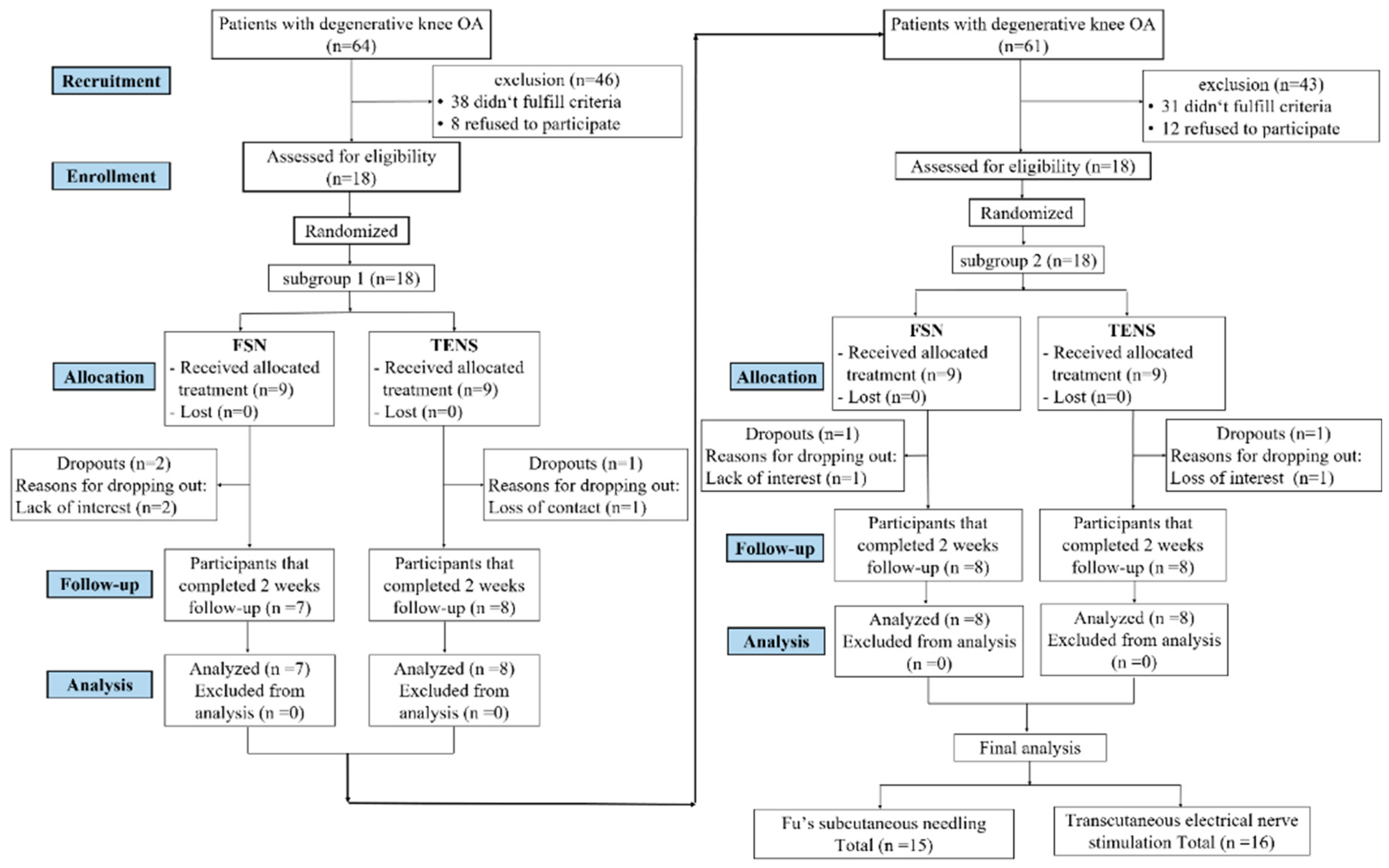
2.1. Study Design
2.2. Participants
2.3. Outcome Measurements
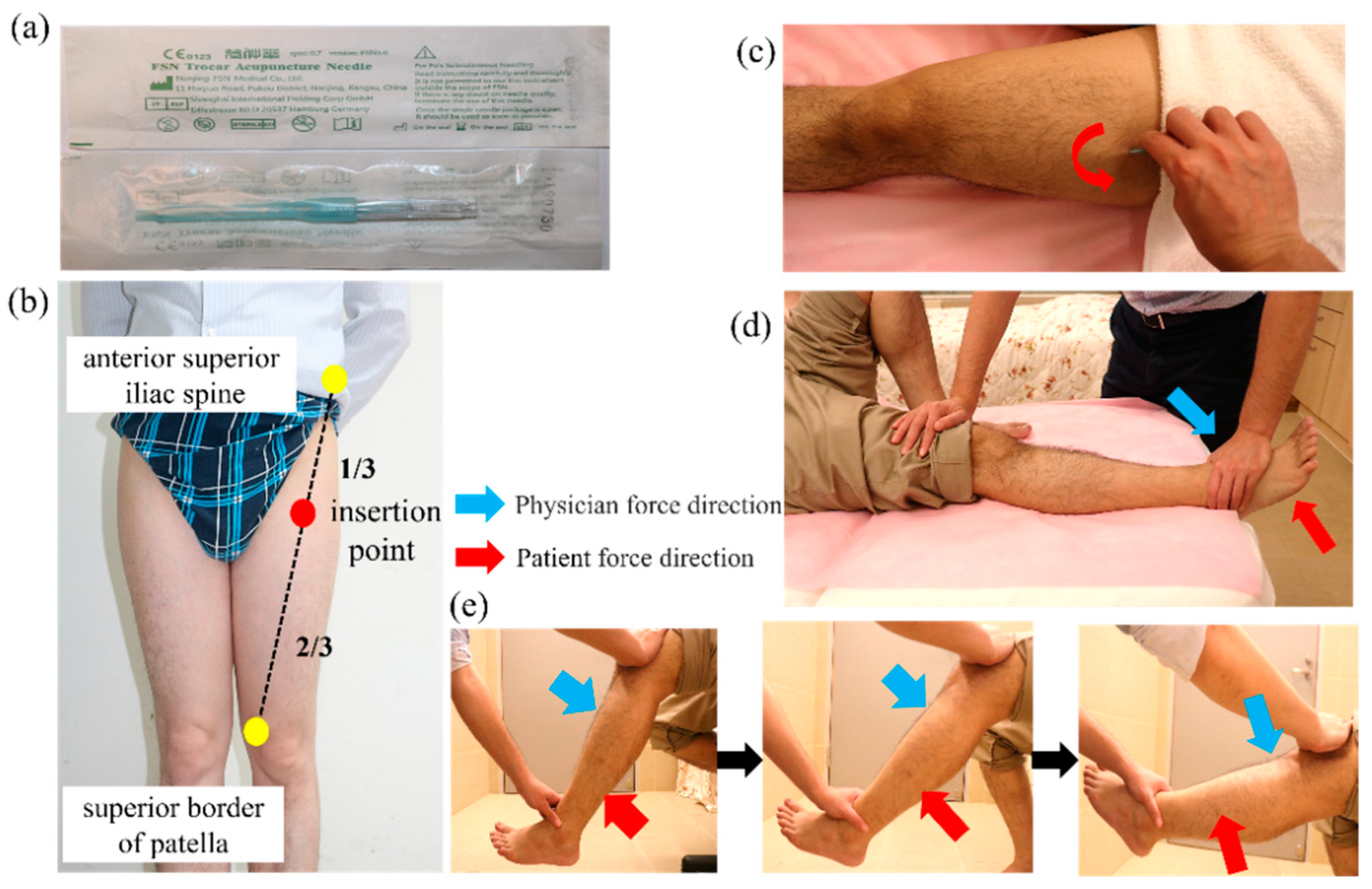
2.4. Procedure and Intervention
2.4.1. Selection of Needle Site for Experimental Group (FSN Group)
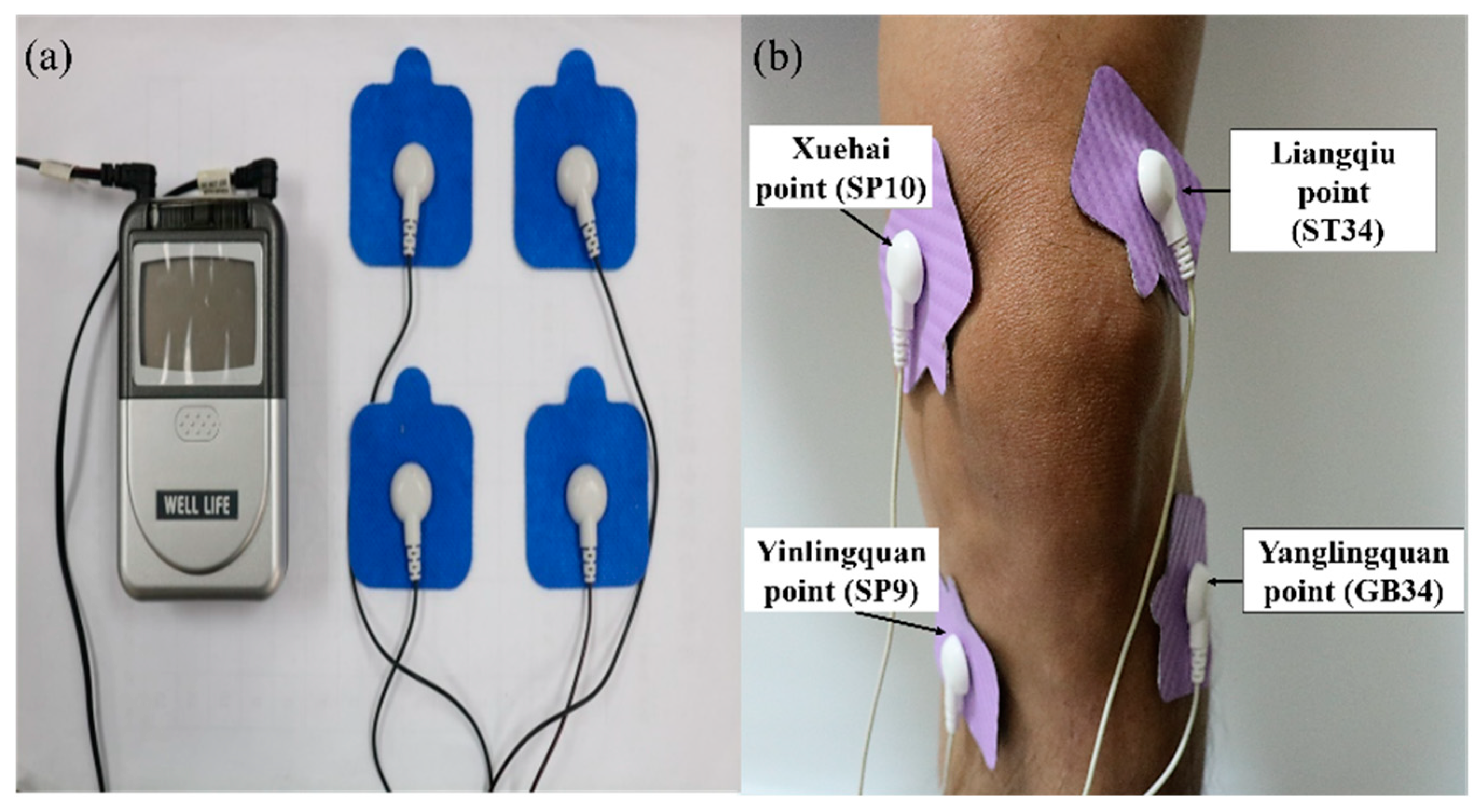
2.4.2. Selection of Electrical Stimulation Points for Control Group (TENS Group)
2.5. Statistical Analysis
3. Results
3.1. Study and Patient Characteristics
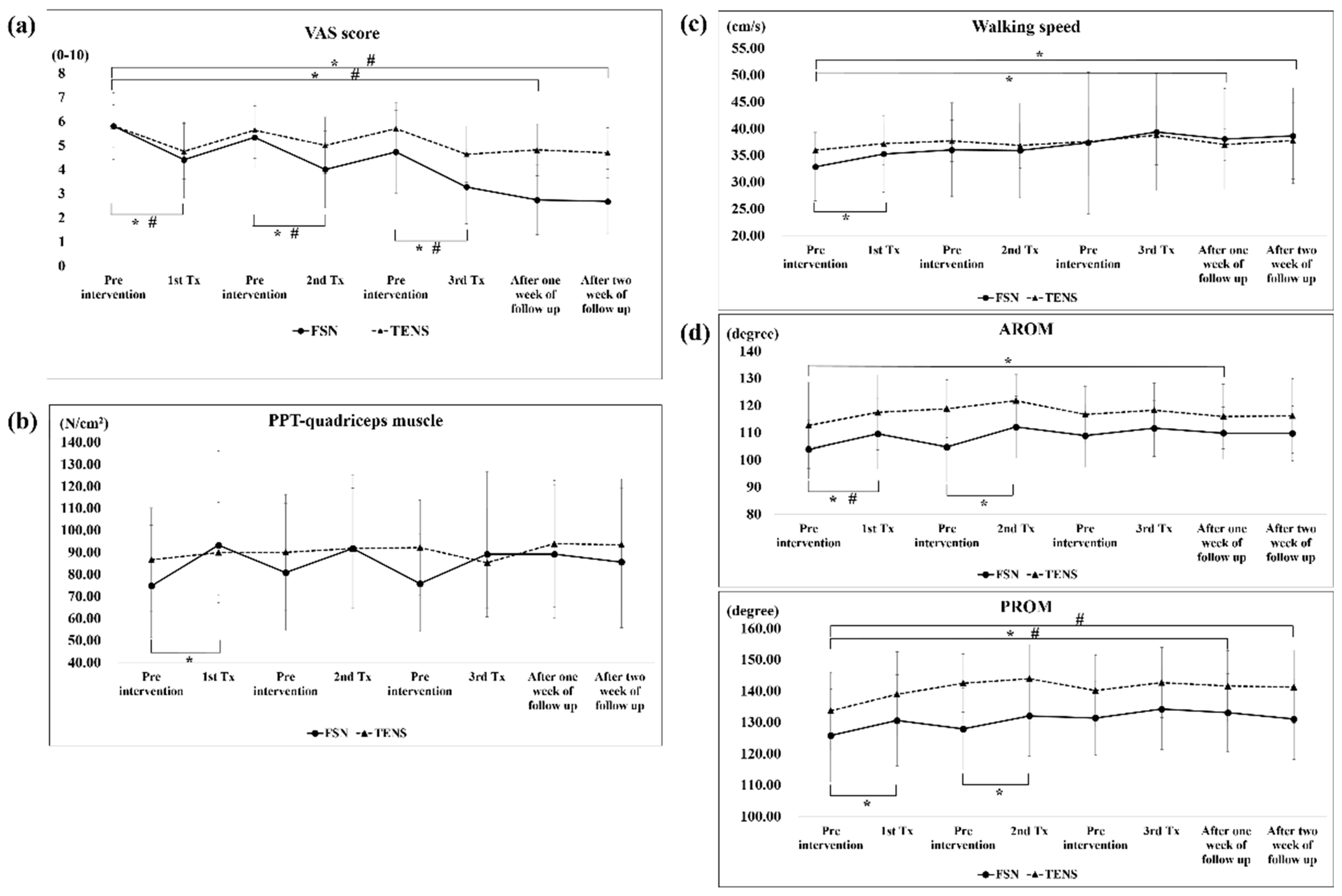
3.2. Pain Qualities
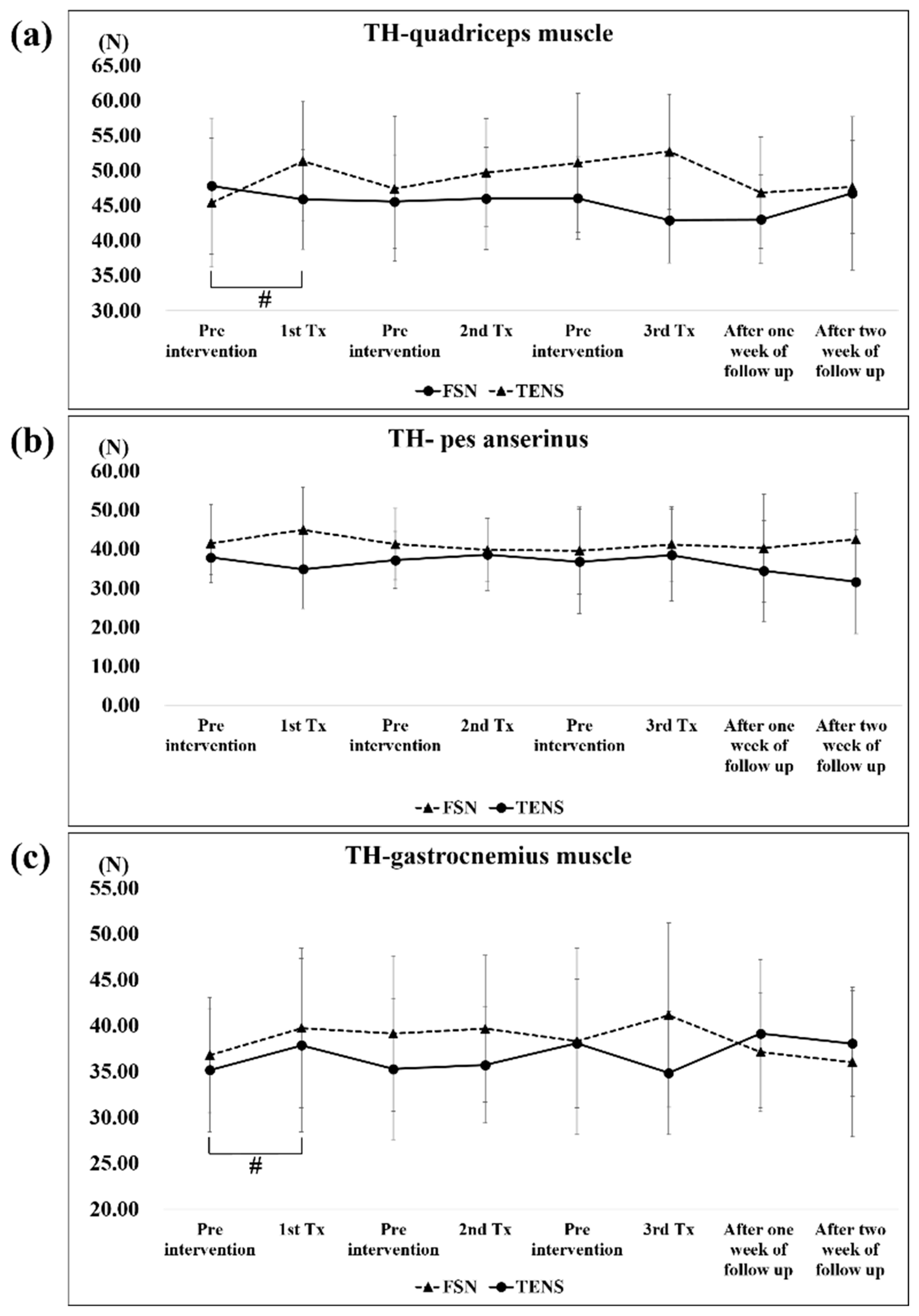
3.3. Muscle and Tendon Qualities
| Day 1 | Day 2 | Day 4 | Day 8 | Day 15 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-tx | Post-tx | P | Pre-tx | Post-tx | P | Pre-tx | Post-tx | P | 1-Week F/U | P | 2-Week F/U | P | |
| VAS | |||||||||||||
| FSN group | 5.80 ± 1.42 | 4.40 ± 1.58 | <0.05 * | 5.33 ± 1.30 | 4.00 ± 1.59 | <0.05 * | 4.73 ± 1.73 | 3.27 ± 1.53 | <0.05 * | 2.73 ± 1.44 | <0.05 * | 2.67 ± 1.35 | <0.05 * |
| TENS group | 5.81 ± 0.91 | 4.75 ± 1.15 | <0.05 * | 5.63 ± 1.17 | 5.00 ± 1.17 | <0.05 * | 5.69 ± 1.10 | 4.63 ± 1.17 | <0.05 * | 4.81 ± 1.07 | <0.05 * | 4.69 ± 1.04 | <0.05 * |
| PPT of quadriceps muscle (N/cm2) | |||||||||||||
| FSN group | 74.73 ± 28.63 | 93.20 ± 42.84 | <0.05 * | 80.80 ± 31.40 | 91.80 ± 33.42 | 0.06 | 75.73 ± 22.51 | 89.13 ± 37.55 | 0.13 | 89.13 ± 31.37 | 0.07 | 85.60 ± 33.37 | 0.31 |
| TENS group | 86.56 ± 24.35 | 89.88 ± 22.76 | 0.57 | 90.06 ± 26.26 | 91.81 ± 27.35 | 0.66 | 92.13 ± 21.66 | 85.31 ± 24.61 | 0.08 | 93.88 ± 28.77 | 0.18 | 93.44 ± 29.95 | 0.24 |
| Walking speed (cm/s) | |||||||||||||
| FSN group | 32.80 ± 6.60 | 35.25 ± 7.18 | <0.05 * | 36.00 ± 8.76 | 35.87 ± 8.87 | 0.96 | 37.34 ± 13.25 | 39.34 ± 10.94 | 0.36 | 38.02 ± 9.41 | <0.05 * | 38.61 ± 8.94 | <0.05 * |
| TENS group | 35.96 ± 3.20 | 37.16 ± 3.90 | 0.15 | 37.66 ± 3.88 | 36.84 ± 4.23 | 0.50 | 37.57 ± 6.51 | 38.74 ± 5.57 | 0.44 | 36.98 ± 4.98 | 0.47 | 37.74 ± 7.17 | 0.38 |
| AROM of knee (degrees) | |||||||||||||
| FSN group | 103.87 ± 11.17 | 109.53 ± 12.86 | <0.05 * | 104.67 ± 12.85 | 112.07 ± 11.34 | <0.05 * | 108.87 ± 11.45 | 111.60 ± 10.30 | 0.27 | 109.80 ± 9.55 | <0.05 * | 109.73 ± 10.02 | 0.09 |
| TENS group | 112.63 ± 16.31 | 117.44 ± 13.73 | <0.05 * | 118.81 ± 10.64 | 121.75 ± 9.59 | 0.29 | 116.63 ± 10.33 | 118.25 ± 9.91 | 0.76 | 115.94 ± 11.85 | 0.57 | 116.13 ± 13.66 | 0.55 |
| PROM of knee (degrees) | |||||||||||||
| FSN group | 125.80 ± 15.33 | 130.60 ± 14.55 | <0.05 * | 127.87 ± 13.05 | 132.07 ± 12.94 | <0.05 * | 131.40 ± 11.80 | 134.20 ± 12.90 | 0.23 | 133.07 ± 12.42 | <0.05 * | 131.07 ± 12.90 | 0.25 |
| TENS group | 135.69 ± 16.80 | 138.94 ± 13.60 | 0.12 | 142.50 ± 9.26 | 143.94 ± 10.83 | 0.27 | 140.19 ± 11.32 | 142.69 ± 11.22 | 0.06 | 141.56 ± 11.32 | <0.05 * | 141.25 ± 11.50 | <0.05 * |
| Day 1 | Day 2 | Day 4 | Day 8 | Day 15 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-tx | Post-tx | P | Pre-tx | Post-tx | P | Pre-tx | Post-tx | P | 1-Week F/U | P | 2-Week F/U | P | |
| PPT of quadriceps muscle (N/cm2) | |||||||||||||
| FSN group | 74.73 ± 28.63 | 93.20 ± 42.84 | <0.05 * | 80.80 ± 31.40 | 91.80 ± 33.42 | 0.06 | 75.73 ± 22.51 | 89.13 ± 37.55 | 0.13 | 89.13 ± 31.37 | 0.07 | 85.60 ± 33.37 | 0.31 |
| TENS group | 86.56 ± 24.35 | 89.88 ± 22.76 | 0.57 | 90.06 ± 26.26 | 91.81 ± 27.35 | 0.66 | 92.13 ± 21.66 | 85.31 ± 24.61 | 0.08 | 93.88 ± 28.77 | 0.18 | 93.44 ± 29.95 | 0.24 |
| PPT of pes anserinus (N/cm2) | |||||||||||||
| FSN group | 66.53 ± 34.06 | 61.47 ± 26.26 | 0.75 | 60.87 ± 28.69 | 65.93 ± 23.37 | 0.16 | 63.80 ± 25.19 | 66.07 ± 25.65 | 0.33 | 61.60 ± 22.81 | 0.73 | 65.40 ± 22.55 | 0.22 |
| TENS group | 63.38 ± 17.76 | 64.25 ± 17.79 | 0.78 | 72.06 ± 25.33 | 72.44 ± 24.35 | 0.87 | 68.00 ± 21.48 | 67.25 ± 19.51 | 0.78 | 71.00 ± 24.01 | 0.36 | 76.44 ± 24.08 | <0.05 * |
| PPT of gastrocnemius muscle (N/cm2) | |||||||||||||
| FSN group | 88.47 ± 34.05 | 88.87 ± 37.90 | 0.87 | 84.13 ± 32.79 | 94.67 ± 34.56 | 0.16 | 93.73 ± 29.34 | 89.07 ± 29.12 | 0.37 | 91.53 ± 24.25 | 0.49 | 87.93 ± 20.03 | 0.69 |
| TENS group | 82.13 ± 24.97 | 91.06 ± 26.58 | <0.05 * | 92.75 ± 27.66 | 89.19 ± 24.62 | 0.28 | 93.50 ± 28.64 | 88.13 ± 29.51 | 0.13 | 92.38 ± 37.91 | 0.24 | 87.38 ± 30.41 | 0.78 |
| TH of quadriceps muscle (N) | |||||||||||||
| FSN group | 47.79 ± 10.04 | 45.89 ± 7.11 | 0.26 | 45.55 ± 6.64 | 45.98 ± 7.29 | 0.91 | 46.01 ± 5.86 | 42.87 ± 6.04 | 0.31 | 42.99 ± 6.29 | 0.07 | 46.73 ± 10.94 | 0.61 |
| TENS group | 45.39 ± 9.51 | 51.31 ± 8.47 | <0.05 * | 47.36 ± 10.33 | 49.67 ± 7.73 | 0.29 | 51.05 ± 9.92 | 52.66 ± 8.22 | 0.76 | 46.79 ± 7.93 | 0.57 | 47.61 ± 6.64 | 0.55 |
| TH of pes anserinus (N) | |||||||||||||
| FSN group | 41.44 ± 9.94 | 44.92 ± 10.90 | 0.39 | 41.23 ± 9.12 | 39.75 ± 8.19 | 0.69 | 39.61 ± 11.14 | 41.17 ± 9.64 | 0.31 | 40.23 ± 13.78 | 0.32 | 42.49 ± 11.95 | 0.78 |
| TENS group | 37.80 ± 4.40 | 34.81 ± 9.98 | 0.33 | 37.16 ± 7.32 | 38.59 ± 9.15 | 0.45 | 36.76 ± 13.40 | 38.47 ± 11.72 | 0.65 | 34.41 ± 12.89 | 0.24 | 31.57 ± 13.22 | 0.09 |
| TH of gastrocnemius muscle (N) | |||||||||||||
| FSN group | 36.79 ± 6.30 | 39.75 ± 8.70 | 0.50 | 39.15 ± 8.46 | 39.67 ± 7.98 | 0.80 | 38.13 ± 10.18 | 41.15 ± 10.02 | 0.29 | 37.13 ± 6.50 | 0.82 | 36.04 ± 8.16 | 0.69 |
| TENS group | 35.15 ± 6.97 | 37.87 ± 9.47 | 0.26 | 35.29 ± 7.71 | 35.71 ± 6.33 | 0.57 | 38.08 ± 6.99 | 34.84 ± 6.72 | 0.07 | 39.13 ± 8.04 | 0.07 | 38.05 ± 5.77 | 0.16 |
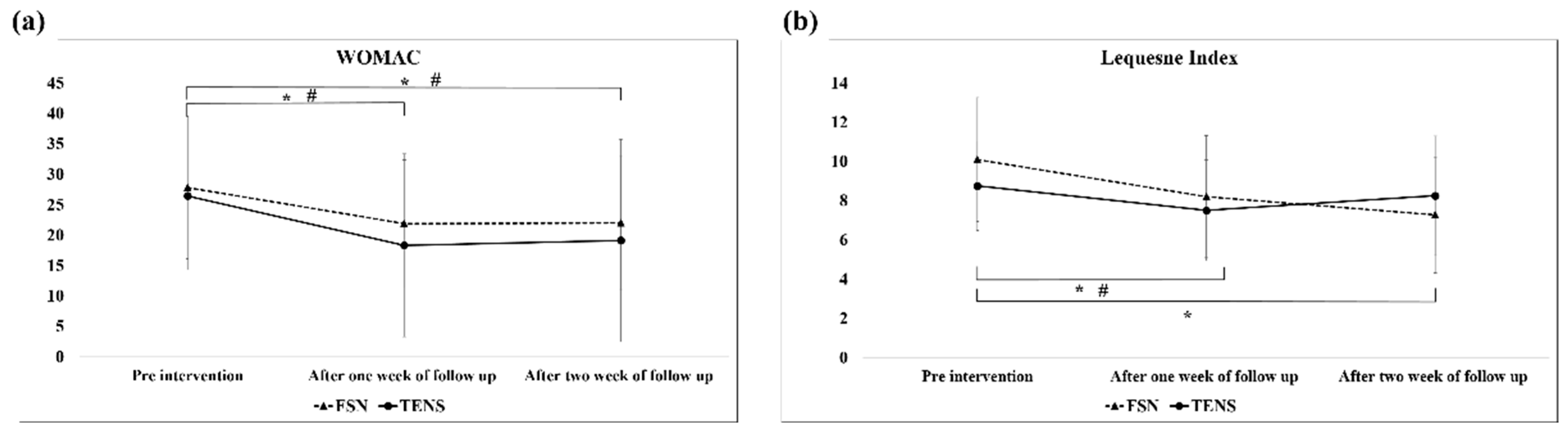
3.4. Functional Index Questionnaire Assessment
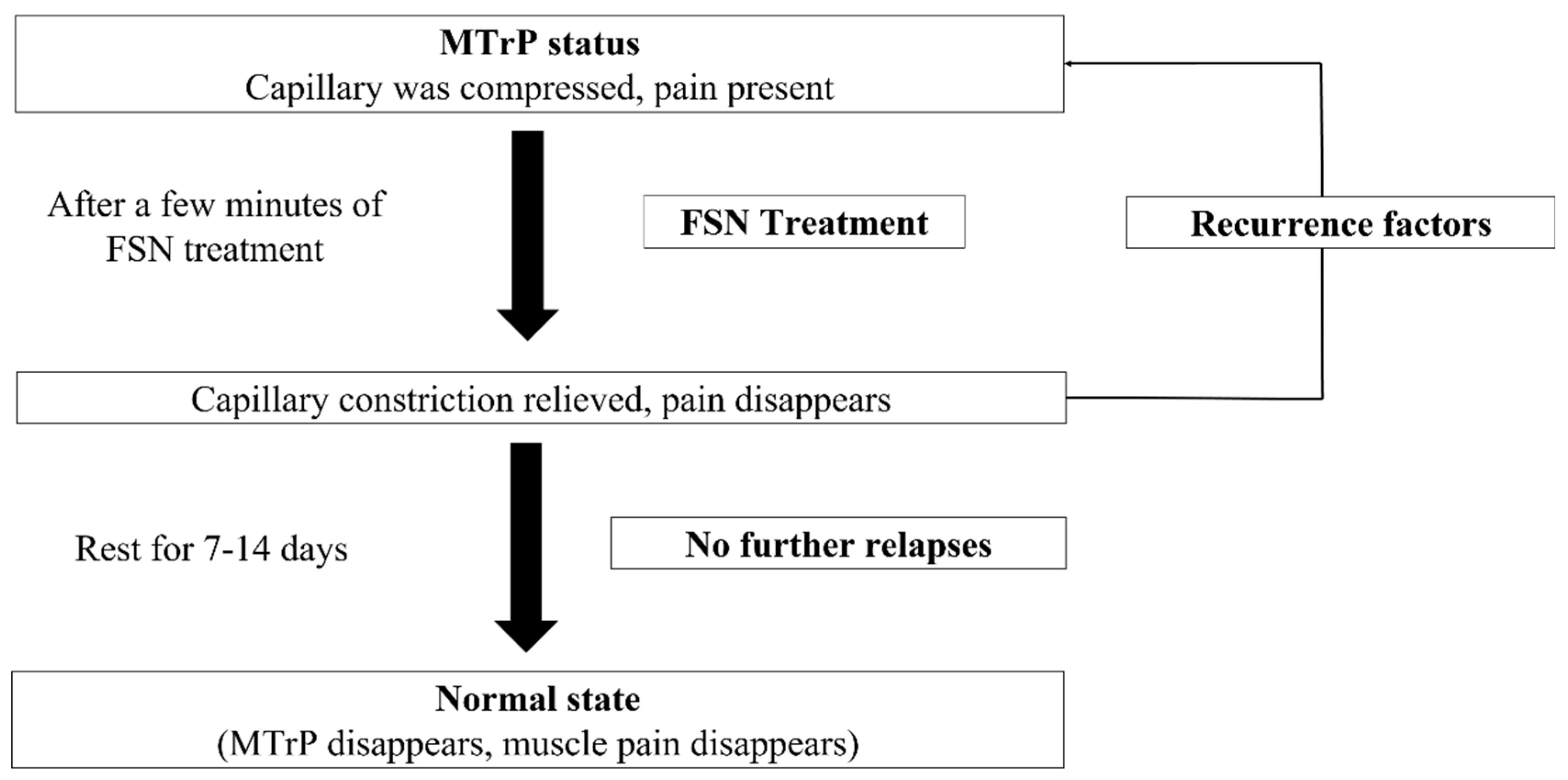
4. Discussion
4.1. Pain Qualities (Including VAS, PPT, Walking Speed, and ROM of Knee)
4.2. Muscle and Tendon Qualities
4.3. Functional Index Questionnaire Assessment
4.4. Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wick, M.C.; Kastlunger, M.; Weiss, R.J. Clinical imaging assessments of knee osteoarthritis in the elderly: A mini-review. Gerontology 2014, 60, 386–394. [Google Scholar] [CrossRef] [PubMed]
- Lespasio, M.J.; Piuzzi, N.S.; Husni, M.E.; Muschler, G.F.; Guarino, A.J.; Mont, M.A. Knee osteoarthritis: A primer. Perm. J. 2017, 21, 16–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [Green Version]
- Woolf, A.D.; Pfleger, B. Burden of major musculoskeletal conditions. Bull. World Health Organ. 2003, 81, 646–656. [Google Scholar] [PubMed]
- Wallace, I.J.; Worthington, S.; Felson, D.T.; Jurmain, R.D.; Wren, K.T.; Maijanen, H.; Woods, R.J.; Lieberman, D.E. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc. Natl. Acad. Sci. USA 2017, 114, 9332–9336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deshpande, B.R.; Katz, J.N.; Solomon, D.H.; Yelin, E.H.; Hunter, D.J.; Messier, S.P.; Suter, L.G.; Losina, E. Number of persons with symptomatic knee osteoarthritis in the US: Impact of race and ethnicity, age, sex, and obesity. Arthritis Care Res. 2016, 68, 1743–1750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, Z.L.; Hou, S.M.; Chen, Z.G.; Ye, K.L.; Shi, G.S.; Hong, L.W.; Xu, H.W.; Li, D.P. Evolution of osteoarthritis treatment: Mesenchymal stem cells of autologous fat. J. Taipei Med. Assoc. 2019, 63, 42–59. [Google Scholar]
- Dor, A.; Kalichman, L. A myofascial component of pain in knee osteoarthritis. J. Bodyw. Mov. Ther. 2017, 21, 642–647. [Google Scholar] [CrossRef]
- Hunter, D.J. Osteoarthritis. Best Pract. Res. Clin. Rheumatol. 2011, 25, 801–814. [Google Scholar] [CrossRef]
- Kornaat, P.R.; Bloem, J.L.; Ceulemans, R.Y.; Riyazi, N.; Rosendaal, F.R.; Nelissen, R.G.; Carter, W.O.; Hellio Le Graverand, M.P.; Kloppenburg, M. Osteoarthritis of the knee: Association between clinical features and MR imaging findings. Radiology 2006, 239, 811–817. [Google Scholar] [CrossRef]
- Sánchez Romero, E.A.; Fernández-Carnero, J.; Calvo-Lobo, C.; Ochoa Sáez, V.; Burgos Caballero, V.; Pecos-Martín, D. Is a Combination of Exercise and Dry Needling Effective for Knee OA? Pain Med. 2020, 21, 349–363. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, A.H. Myofascial pain disorders: Theory to therapy. Drugs 2004, 64, 45–62. [Google Scholar] [CrossRef] [PubMed]
- Chou, L.W.; Kao, M.J.; Lin, J.G. Probable mechanisms of needling therapies for myofascial pain control. Evid.-Based Complement. Altern. Med. 2012, 2012, 705327. [Google Scholar] [CrossRef] [PubMed]
- Chou, L.W.; Hsieh, Y.L.; Kuan, T.S.; Hong, C.Z. Needling therapy for myofascial pain: Recommended technique with multiple rapid needle insertion. BioMedicine 2014, 4, 39–46. [Google Scholar] [CrossRef]
- Navarro-Santana, M.J.; Sanchez-Infante, J.; Fernández-de-Las-Peñas, C.; Cleland, J.A.; Martín-Casas, P.; Plaza-Manzano, G. Effectiveness of dry needling for myofascial trigger points associated with neck pain symptoms: An updated systematic review and meta-analysis. J. Clin. Med. 2020, 9, 3300. [Google Scholar] [CrossRef]
- Dorsher, P.T. Can classical acupuncture points and trigger points be compared in the treatment of pain disorders? Birch’s analysis revisited. J. Altern. Complement. Med. 2008, 14, 353–359. [Google Scholar] [CrossRef]
- Lo, P.C.; Lin, F.C.; Tsai, Y.C.; Lin, S.K. Traditional Chinese medicine therapy reduces the risk of total knee replacement in patients with knee osteoarthritis. Medicine 2019, 98, e15964. [Google Scholar] [CrossRef]
- Fu, Z.H. The Foundation of Fu’s Subcutaneous Needling; People’s Medical Publishing House Co., Ltd.: Beijing, China, 2016. [Google Scholar]
- Li, K.; Wu, W.T.; Fu, Z.H.; Chou, L.W. Fu’s subcutaneous needling, modern acupuncture. J. Chin. Med. Assoc. Acupunct. 2016, 19, 45–52. [Google Scholar]
- Fu, Z.; Chou, L.W. Chapter 16 Fu’s Subcutaneous Needling, Trigger Point Dry Needling: An Evidence and Clinical-Based Approach, 2nd ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Muraki, S.; Akune, T.; Oka, H.; En-yo, Y.; Yoshida, M.; Saika, A.; Suzuki, T.; Yoshida, H.; Ishibashi, H.; Tokimura, F.; et al. Association of radiographic and symptomatic knee osteoarthritis with health-related quality of life in a population-based cohort study in Japan: The ROAD study. Osteoarthr. Cartil. 2010, 18, 1227–1234. [Google Scholar] [CrossRef] [Green Version]
- Chiu, P.E.; Fu, Z.; Jian, G.W.; Huang, C.H.; Li, T.M.; Chou, L.W. Evaluating effectiveness of Fu’s subcutaneous needling for the pain nature and quality of life in patients with knee osteoarthritis: A study protocol of randomized clinical trial. J. Pain Res. 2021, 14, 3163–3172. [Google Scholar] [CrossRef]
- Fischer, A.A. Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain 1987, 30, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.A. Pressure threshold meter: Its use for quantification of tender spots. Arch. Phys. Med. Rehabil. 1986, 67, 836–838. [Google Scholar] [PubMed]
- Han, T.I.; Hong, C.Z.; Kuo, F.C.; Hsieh, Y.L.; Chou, L.W.; Kao, M.J. Mechanical pain sensitivity of deep tissues in children—Possible development of myofascial trigger points in children. BMC Musculoskelet. Disord. 2012, 13, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jaworski, J.; Ambroży, T.; Lech, G.; Spieszny, M.; Bujas, P.; Żak, M.; Chwała, W. Absolute and relative reliability of several measures of static postural stability calculated using a GYKO inertial sensor system. Acta. Bioeng. Biomech. 2020, 22, 94–99. [Google Scholar] [CrossRef]
- Hamersma, D.T.; Hofste, A.; Rijken, N.H.; Rohé, M.R.; Oosterveld, F.G.; Soer, R. Reliability and validity of the Microgate Gyko for measuring range of motion of the low back. Musculoskelet. Sci. Pract. 2020, 45, 102091. [Google Scholar] [CrossRef]
- Soucie, J.M.; Wang, C.; Forsyth, A.; Funk, S.; Denny, M.; Roach, K.E.; Boone, D.; Hemophilia Treatment Center Network. Range of motion measurements: Reference values and a database for comparison studies. Haemophilia 2011, 17, 500–507. [Google Scholar] [CrossRef]
- Stathokostas, L.; McDonald, M.W.; Little, R.; Paterson, D.H. Flexibility of older adults aged 55-86 years and the influence of physical activity. J. Aging Res. 2013, 2013, 743843. [Google Scholar] [CrossRef] [Green Version]
- Hancock, G.E.; Hepworth, T.; Wembridge, K. Accuracy and reliability of knee goniometry methods. J. Exp. Orthop. 2018, 5, 46. [Google Scholar] [CrossRef] [Green Version]
- Aird, L.; Samuel, D.; Stokes, M. Quadriceps muscle tone, elasticity and stiffness in older males: Reliability and symmetry using the MyotonPRO. Arch. Gerontol. Geriatr. 2012, 55, e31–e39. [Google Scholar] [CrossRef]
- Pruyn, E.C.; Watsford, M.L.; Murphy, A.J. Validity and reliability of three methods of stiffness assessment. J. Sport Health Sci. 2016, 5, 476–483. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.S.; Um, G.M.; Choi, J.H. Immediate effects of kinematic taping on lower extremity muscle tone and stiffness in flexible flat feet. J. Phys. Ther. Sci. 2016, 28, 1339–1342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Symonds, T.; Hughes, B.; Liao, S.; Ang, Q.; Bellamy, N. Validation of the chinese western ontario and mcmaster universities osteoarthritis index in patients from mainland china with osteoarthritis of the knee. Arthritis Care Res. 2015, 67, 1553–1560. [Google Scholar] [CrossRef]
- Stucki, G.; Sangha, O.; Stucki, S.; Michel, B.A.; Tyndall, A.; Dick, W.; Theiler, R. Comparison of the WOMAC (Western Ontario and McMaster Universities) osteoarthritis index and a self-report format of the self-administered Lequesne-Algofunctional index in patients with knee and hip osteoarthritis. Osteoarthr. Cartil. 1998, 6, 79–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vance, C.G.; Dailey, D.L.; Rakel, B.A.; Sluka, K.A. Using TENS for pain control: The state of the evidence. Pain Manag. 2014, 4, 197–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osiri, M.; Welch, V.; Brosseau, L.; Shea, B.; McGowan, J.L.; Tugwell, P.; Wells, G.A. Transcutaneous electrical nerve stimulation for knee osteoarthritis. Cochrane Database Syst. Rev. 2000, CD002823. [Google Scholar] [CrossRef]
- Zeng, C.; Yang, T.; Deng, Z.H.; Yang, Y.; Zhang, Y.; Lei, G.H. Electrical stimulation for pain relief in knee osteoarthritis: Systematic review and network meta-analysis. Osteoarthr. Cartil. 2015, 23, 189–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, E.D.; Won, Y.H.; Park, S.H.; Seo, J.H.; Kim, D.S.; Ko, M.H.; Kim, G.W. Efficacy and safety of a stimulator using low-intensity pulsed ultrasound combined with transcutaneous electrical nerve stimulation in patients with painful knee osteoarthritis. Pain Res. Manag. 2019, 2019, 7964897. [Google Scholar] [CrossRef]
- Kumar, A.; Chakraborty, B.S. Interim analysis: A rational approach of decision making in clinical trial. J. Adv. Pharm. Technol. Res. 2016, 7, 118–122. [Google Scholar]
- Iijima, H.; Eguchi, R.; Shimoura, K.; Yamada, K.; Aoyama, T.; Takahashi, M. Transcutaneous electrical nerve stimulation improves stair climbing capacity in people with knee osteoarthritis. Sci. Rep. 2020, 10, 7294. [Google Scholar] [CrossRef]
- Takla, M.K.N.; Rezk-Allah, S.S. Immediate effects of simultaneous application of transcutaneous electrical nerve stimulation and ultrasound phonophoresis on active myofascial trigger points. Am. J. Phys. Med. Rehabil. 2018, 97, 332–338. [Google Scholar] [CrossRef]
- Fu, Z.; Shepherd, R. Fu’s subcutaneous needling, a modern style of ancient acupuncture? In Acupuncture in Modern Medicine [Internet]; Chen, L.L., Cheng, T.O., Eds.; IntechOpen: London, UK, 2013. [Google Scholar]
- Fu, Z.H.; Wang, J.H.; Sun, J.H.; Chen, X.Y.; Xu, J.G. Fu’s subcutaneous needling: Possible clinical evidence of the subcutaneous connective tissue in acupuncture. J. Altern. Complement. Med. 2007, 13, 47–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Purser, J.L.; Golightly, Y.M.; Feng, Q.; Helmick, C.G.; Renner, J.B.; Jordan, J.M. Association of slower walking speed with incident knee osteoarthritis-related outcomes. Arthritis Care Res. 2012, 64, 1028–1035. [Google Scholar]
- Roos, E.M.; Grønne, D.T.; Skou, S.T.; Zywiel, M.G.; McGlasson, R.; Barton, C.J.; Kemp, J.L.; Crossley, K.M.; Davis, A.M. Immediate outcomes following the GLA:D® program in Denmark, Canada and Australia. A longitudinal analysis including 28,370 patients with symptomatic knee or hip osteoarthritis. Osteoarthr. Cartil. 2021, 29, 502–506. [Google Scholar] [CrossRef] [PubMed]
- Tani, K.; Kola, I.; Dhamaj, F.; Shpata, V.; Zallari, K. Physiotherapy effects in gait speed in patients with knee osteoarthritis. Open Access Maced. J. Med. Sci. 2018, 6, 493–497. [Google Scholar] [CrossRef]
- Iwata, M.; Yamamoto, A.; Matsuo, S.; Hatano, G.; Miyazaki, M.; Fukaya, T.; Fujiwara, M.; Asai, Y.; Suzuki, S. Dynamic stretching has sustained effects on range of motion and passive stiffness of the hamstring muscles. J. Sports Sci. Med. 2019, 18, 13–20. [Google Scholar] [PubMed]
- Chen, C.H.; Xin, Y.; Lee, K.W.; Lin, M.J.; Lin, J.J. Acute effects of different dynamic exercises on hamstring strain risk factors. PLoS ONE 2018, 13, e0191801. [Google Scholar] [CrossRef] [Green Version]
- Bricca, A.; Roos, E.M.; Juhl, C.B. Infographic. Therapeutic exercise relieves pain and dose not harm knee cartilage nor trigger inflammation. Br. J. Sports Med. 2020, 54, 118–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plaut, S. Scoping review and interpretation of myofascial pain/fibromyalgia syndrome: An attempt to assemble a medical puzzle. PLoS ONE 2022, 17, e0263087. [Google Scholar] [CrossRef]
- Okada-Ogawa, A.; Sekine, N.; Watanabe, K.; Kohashi, R.; Asano, S.; Iwata, K.; Imamura, Y. Change in muscle hardness after trigger point injection and physiotherapy for myofascial pain syndrome. J. Oral Sci. 2019, 61, 36–44. [Google Scholar] [CrossRef] [Green Version]
- Hara, K.; Shinozaki, T.; Okada-Ogawa, A.; Matsukawa, Y.; Dezawa, K.; Nakaya, Y.; Chen, J.Y.; Noma, N.; Oka, S.; Iwata, K.; et al. Headache attributed to temporomandibular disorders and masticatory myofascial pain. J. Oral Sci. 2016, 58, 195–204. [Google Scholar] [CrossRef] [Green Version]
- Terwee, C.B.; van der Slikke, R.M.; van Lummel, R.C.; Benink, R.J.; Meijers, W.G.; de Vet, H.C. Self-reported physical functioning was more influenced by pain than performance-based physical functioning in knee-osteoarthritis patients. J. Clin. Epidemiol. 2006, 59, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Bedson, J.; Croft, P.R. The discordance between clinical and radiographic knee osteoarthritis: A systematic search and summary of the literature. BMC Musculoskelet. Disord. 2008, 9, 116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Q.; Bensamoun, S.; Basford, J.R.; Thompson, J.M.; An, K.N. Identification and quantification of myofascial taut bands with magnetic resonance elastography. Arch. Phys. Med. Rehabil. 2007, 88, 1658–1661. [Google Scholar] [CrossRef] [PubMed]
- Cowled, P.; Fitridge, R. Pathophysiology of reperfusion injury. In Mechanisms of Vascular Disease: A Reference Book for Vascular Specialists [Internet]; Fitridge, R., Thompson, M., Eds.; University of Adelaide Press: Adelaide, AU, USA, 2011; p. 18. [Google Scholar]

| Characteristics | FSN (N = 15) | TENS (N = 16) | p-Value |
|---|---|---|---|
| Age (years old) | 65.73 ± 6.79 (54–77) | 62.81 ± 5.72 (54–72) | 0.24 |
| Sex (M/F) | 4/11 | 6/10 | 0.70 |
| Affected side (Left/Right) | 9/6 | 8/8 | 0.58 |
| Height (cm) | 161.00 ± 6.11 | 158.69 ± 6.25 | 0.34 |
| Weight (kg) | 69.00 ± 13.17 | 59.50 ± 9.57 | 0.14 |
| VAS (0–10) | 5.80 ± 1.42 | 5.81 ± 0.91 | 0.98 |
| WOMAC-Total (0–96) | 27.80 ± 12.12 | 26.44 ± 12.54 | 0.61 |
| Lequesne index (0–24) | 10.13 ± 3.27 | 8.75 ± 2.35 | 0.26 |
| PPT (N/cm2) | |||
| Quadriceps muscle | 74.73 ± 28.63 | 86.56 ± 24.35 | 0.41 |
| Pes anserinus | 66.53 ± 34.06 | 63.38 ± 17.76 | 0.84 |
| Gastrocnemius muscle | 88.47 ± 34.05 | 82.13 ± 24.97 | 0.89 |
| TH (N) | |||
| Quadriceps muscle | 47.79 ± 10.04 | 45.39 ± 9.51 | 0.83 |
| Pes anserinus | 41.44 ± 9.94 | 37.80 ± 4.40 | 0.14 |
| Gastrocnemius muscle | 36.79 ± 6.30 | 35.15 ± 6.97 | 0.68 |
| ROM (degrees) | |||
| Active ROM | 103.87 ± 11.17 | 112.63 ± 16.31 | 0.07 |
| Passive ROM | 125.80 ± 15.33 | 135.69 ± 16.80 | 0.06 |
| Walking speed (cm/s) | 32.80 ± 6.60 | 35.96 ± 3.20 | 0.11 |
| Day 1 | Day 8 | Day 15 | |||
|---|---|---|---|---|---|
| Pre-tx | 1-Week Follow-Up | p-Value | 2-Week Follow-Up | p-Value | |
| WOMAC | |||||
| FSN group | 27.80 ± 12.12 | 21.87 ± 10.50 | <0.05 * | 22.00 ± 11.06 | <0.05 * |
| TENS group | 26.44 ± 12.54 | 18.31 ± 15.02 | <0.05 * | 19.13 ± 16.64 | <0.05 * |
| Lequesne index | |||||
| FSN group | 10.13 ± 3.27 | 8.20 ± 3.12 | <0.05 * | 7.27 ± 2.95 | <0.05 * |
| TENS group | 8.75 ± 2.25 | 7.50 ± 2.57 | <0.05 * | 8.25 ± 3.05 | 0.44 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiu, P.-E.; Fu, Z.; Sun, J.; Jian, G.-W.; Li, T.-M.; Chou, L.-W. Efficacy of Fu’s Subcutaneous Needling in Treating Soft Tissue Pain of Knee Osteoarthritis: A Randomized Clinical Trial. J. Clin. Med. 2022, 11, 7184. https://doi.org/10.3390/jcm11237184
Chiu P-E, Fu Z, Sun J, Jian G-W, Li T-M, Chou L-W. Efficacy of Fu’s Subcutaneous Needling in Treating Soft Tissue Pain of Knee Osteoarthritis: A Randomized Clinical Trial. Journal of Clinical Medicine. 2022; 11(23):7184. https://doi.org/10.3390/jcm11237184
Chicago/Turabian StyleChiu, Po-En, Zhonghua Fu, Jian Sun, Guan-Wei Jian, Te-Mao Li, and Li-Wei Chou. 2022. "Efficacy of Fu’s Subcutaneous Needling in Treating Soft Tissue Pain of Knee Osteoarthritis: A Randomized Clinical Trial" Journal of Clinical Medicine 11, no. 23: 7184. https://doi.org/10.3390/jcm11237184
APA StyleChiu, P.-E., Fu, Z., Sun, J., Jian, G.-W., Li, T.-M., & Chou, L.-W. (2022). Efficacy of Fu’s Subcutaneous Needling in Treating Soft Tissue Pain of Knee Osteoarthritis: A Randomized Clinical Trial. Journal of Clinical Medicine, 11(23), 7184. https://doi.org/10.3390/jcm11237184






