Artificial Intelligence in Dermatology Image Analysis: Current Developments and Future Trends
Abstract
1. Introduction
2. Overview of AI
2.1. What Is AI?
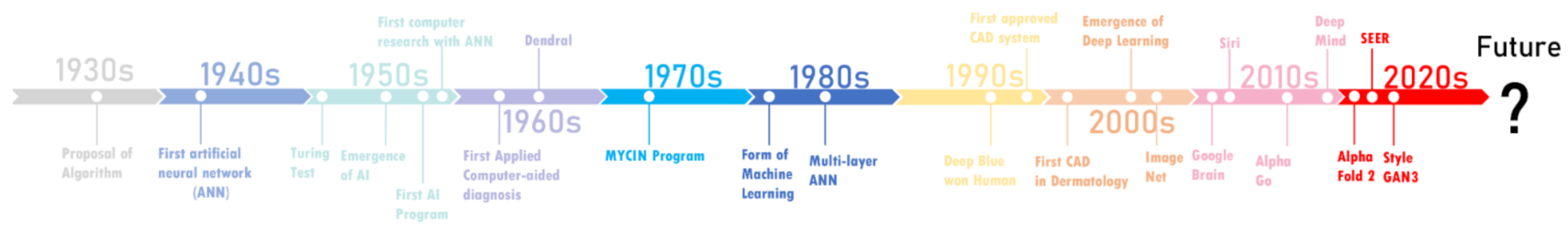
2.2. The History of AI and Its Development Path in Medicine
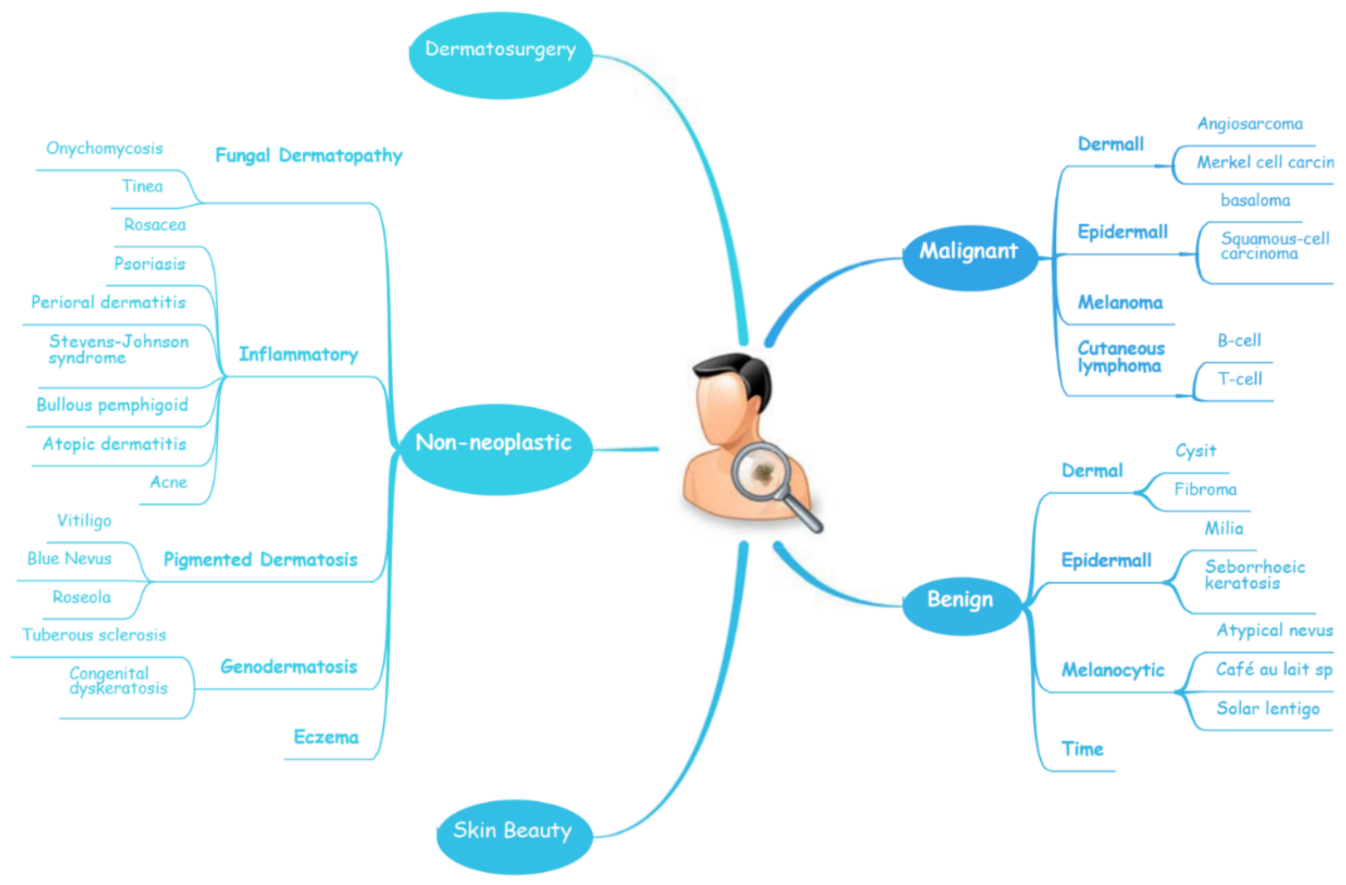
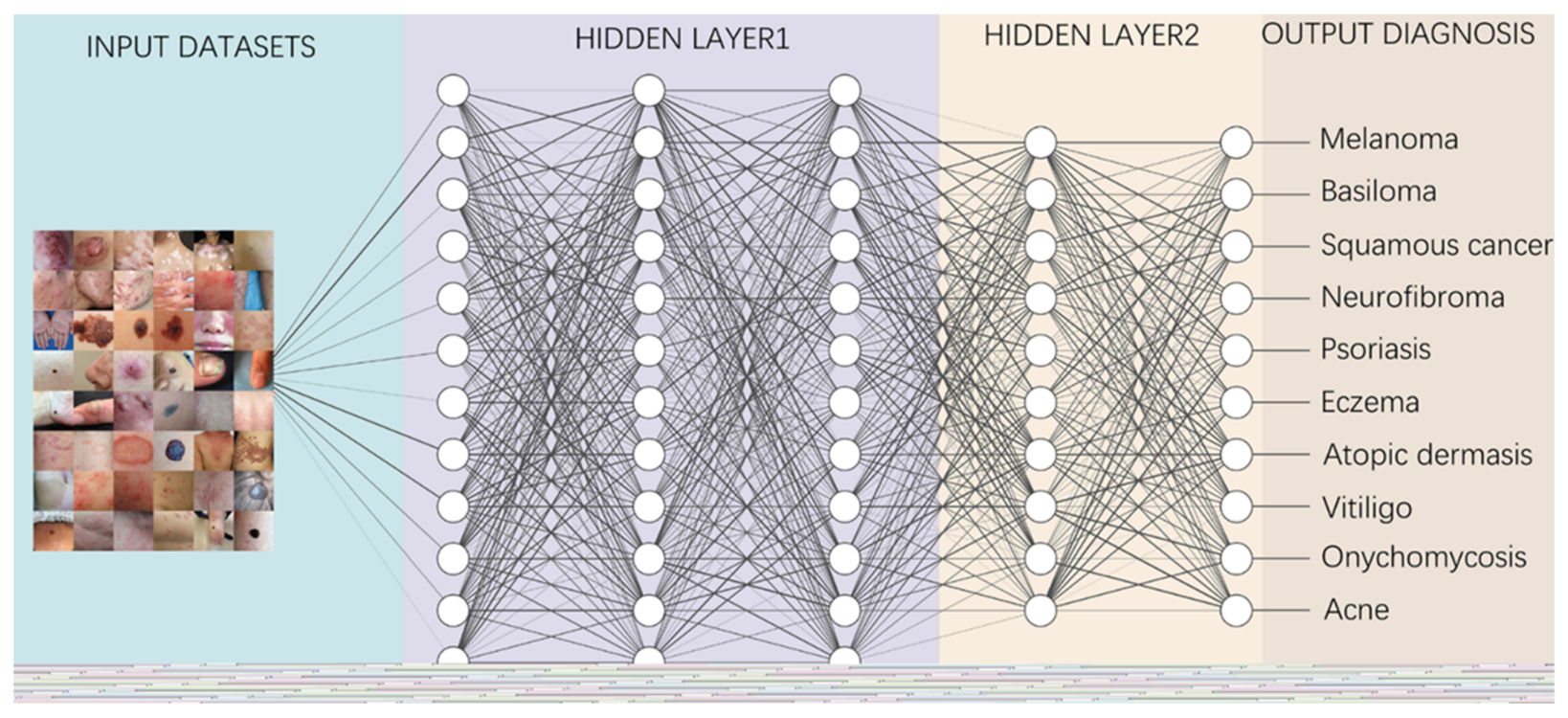
2.3. Relevant Concept of AI in Dermatology
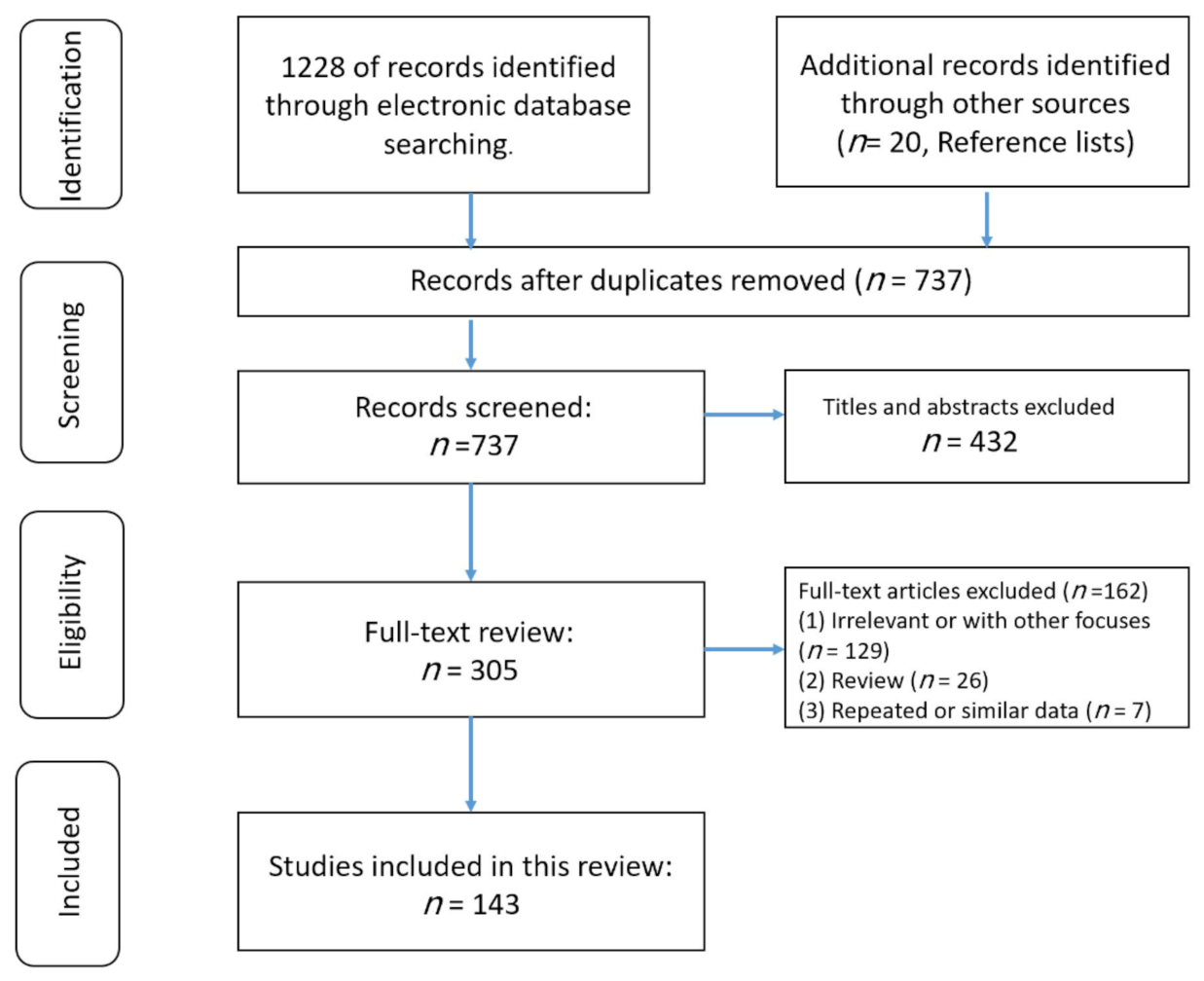
3. Method
3.1. Search Strategy
3.2. Studies Selection
3.3. Data Extraction
4. The Implementation of AI in Dermatology
4.1. AI in Aid-Diagnosis and Multi-Classification for Skin Lesions
4.1.1. Multi-Classification for Skin Lesions in ISIC Challenges
4.1.2. Multi-Classification for Skin Lesions in Specific Dermatosis
Melanocytic Skin Lesions
Benign Pigmented Skin Lesions
Inflammatory Dermatoses
4.2. AI in Aid-Diagnosis and Binary-Classification for Specific Dermatosis
4.2.1. Skin Cancer
Melanoma
Non-Melanoma Skin Cancer
Neurofibroma
4.2.2. Application of AI for Inflammatory Dermatosis
Psoriasis
Eczema
Atopic Dermatitis
Acne
Vitiligo
Fungal Dermatosis
4.3. Application of AI for Aesthetic Dermatology
4.4. Applications of AI for Skin Surgery
5. Computer-Aided Dermatology AI Systems on Market
| Name | Manufacturer | Country | On Market Year | Platform | Application | Reference |
|---|---|---|---|---|---|---|
| Moleanalyzer pro | Fotofinder | Germany | 2018 | Windows | Analyzes melanocytic as well as non-melanocytic skin lesions and calculates an AI score for mole risk assessment | [97,137] |
| Vectra WBS 360 | Canfiield | USA | 2017 | Windows | Capturing the entire skin surface in macro quality resolution with a single capture, to identify and monitors pigment lesions automatically or mannually | [102,103,138] |
| Visia skin | Canfiield | USA | 2007 | Windows | Capturing key visual information for eight areas affecting complexion health and appearance and to provide an informative comparison of patient’s complexion’s characteristics to others of same age and skin type | [173,174,175] |
| Antera 3D | Miravex | Ireland | 2011 | Windows | Analysis and measurement of wrinkles, texture, pigmentation, redness and other lesions | [176] |
| Dermoscan X2 | Dermoscan | Germany | 2017 | Windows | Identification of the new or modified lesions with digital photo documentations and makes automatic comparison of pigmentation marks | [177] |
| AIDERMA | Dingxiangyuan | China | 2018 | Online | Automatic identification of skin disorders and stores patient’s medical record in the cloud safely | [178,179] |
| DermEngine | MetaOptima Technology Inc. | Canada | 2015 | Android and iOS | Imaging, documentation and analysis of skin conditions including skin cancer; offers business intelligence features designed for practice management | [71] |
| Skin-App | Swiss4ward | Switzerland | 2017 | Android and iOS | Detection of hand eczema automatically | [71] |
| Neurodermitis Helferin|Nia | Nia Health | Germany | 2019 | Android and iOS | Marks affected areas on the clear body diagram, takes photos and documents of the current severity of the neurodermatitis and gives personalized suggestions after further analysis | [157] |
| DermoScanner | Neat Technology lnc. | N/A | 2019 | Android | Analysis of skin moles and detects skin cancers at an early stage when it is most treatable. | [159] |
| Dermacompass | Swiss4ward | Switzerland | 2017 | Android and iOS | It contains skin diseases, pictures and algorithms for treatment and provides individual case diagnosis and image comparison for dermatologists | [180] |
6. Attitudes of Different Groups of People towards AI in Dermatology
7. Current Limitations of the Application of AI in the Field of Dermatology
8. Future Trends of Artificial Intelligence in Medical Field and Dermatology
9. The Challenge Posed to Humanity by the Development of AI
10. Prospects of the Application of AI in the Field of Dermatology
11. Conclusions and Perspective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bellman, R. An Introduction to Artificial Intelligence: Can Computers Think? 1st ed.; Boyd & Fraser Publishing Company: San Francisco, CA, USA, 1978. [Google Scholar]
- Litjens, G.; Kooi, T.; Bejnordi, B.E.; Setio, A.A.A.; Ciompi, F.; Ghafoorian, M.; van der Laak, J.A.W.M.; van Ginneken, B.; Sánchez, C.I. A Survey on Deep Learning in Medical Image Analysis. Med. Image Anal. 2017, 42, 60–88. [Google Scholar] [CrossRef] [PubMed]
- Laino, M.E.; Cancian, P.; Politi, L.S.; Della Porta, M.G.; Saba, L.; Savevski, V. Generative Adversarial Networks in Brain Imaging: A Narrative Review. J. Imaging 2022, 8, 83. [Google Scholar] [CrossRef] [PubMed]
- Lassau, N.; Bousaid, I.; Chouzenoux, E.; Lamarque, J.P.; Charmettant, B.; Azoulay, M.; Cotton, F.; Khalil, A.; Lucidarme, O.; Pigneur, F.; et al. Three Artificial Intelligence Data Challenges Based on CT and MRI. Diagn. Interv. Imaging 2020, 101, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Celebi, M.E.; Zhang, Y.D.; Yu, X.; Lu, S.; Yao, X.; Zhou, Q.; Miguel, M.G.; Tian, Y.; Gorriz, J.M.; et al. Advances in Data Preprocessing for Bio-Medical Data Fusion: An Overview of the Methods, Challenges, and Prospects. Inf. Fusion 2021, 76, 376–421. [Google Scholar] [CrossRef]
- von Itzstein, M.S.; Hullings, M.; Mayo, H.; Beg, M.S.; Williams, E.L.; Gerber, D.E. Application of Information Technology to Clinical Trial Evaluation and Enrollment: A Review. JAMA Oncol. 2021, 7, 1559–1566. [Google Scholar] [CrossRef]
- Xu, Y.; Su, G.-H.; Ma, D.; Xiao, Y.; Shao, Z.-M.; Jiang, Y.-Z. Technological Advances in Cancer Immunity: From Immunogenomics to Single-Cell Analysis and Artificial Intelligence. Signal Transduct. Target. Ther. 2021, 6, 312. [Google Scholar] [CrossRef]
- Barisoni, L.; Lafata, K.J.; Hewitt, S.M.; Madabhushi, A.; Balis, U.G.J. Digital Pathology and Computational Image Analysis in Nephropathology. Nat. Rev. Nephrol. 2020, 16, 669–685. [Google Scholar] [CrossRef]
- Ho, D.; Quake, S.R.; McCabe, E.R.B.; Chng, W.J.; Chow, E.K.; Ding, X.; Gelb, B.D.; Ginsburg, G.S.; Hassenstab, J.; Ho, C.-M.; et al. Enabling Technologies for Personalized and Precision Medicine. Trends Biotechnol. 2020, 38, 497–518. [Google Scholar] [CrossRef]
- Bajaj, S.; Marchetti, M.A.; Navarrete-Dechent, C.; Dusza, S.W.; Kose, K.; Marghoob, A.A. The Role of Color and Morphologic Characteristics in Dermoscopic Diagnosis. JAMA Dermatol. 2016, 152, 676–682. [Google Scholar] [CrossRef]
- Perednia, D.A. What Dermatologists Should Know about Digital Imaging. J. Am. Acad. Dermatol. 1991, 25, 89–108. [Google Scholar] [CrossRef]
- Møllersen, K.; Kirchesch, H.; Zortea, M.; Schopf, T.R.; Hindberg, K.; Godtliebsen, F. Computer-Aided Decision Support for Melanoma Detection Applied on Melanocytic and Nonmelanocytic Skin Lesions: A Comparison of Two Systems Based on Automatic Analysis of Dermoscopic Images. BioMed Res. Int. 2015, 2015, 579282. [Google Scholar] [CrossRef] [PubMed]
- Cazzaniga, S.; Sassi, F.; Mercuri, S.R.; Naldi, L. Prediction of Clinical Response to Excimer Laser Treatment in Vitiligo by Using Neural Network Models. Dermatology 2009, 219, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Khozeimeh, F.; Alizadehsani, R.; Roshanzamir, M.; Khosravi, A.; Layegh, P.; Nahavandi, S. An Expert System for Selecting Wart Treatment Method. Comput. Biol. Med. 2017, 81, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.I.; Lee, S.; Jeong, C.W.; Kim, H.S. Robot-Assisted Anterior Pelvic Exenteration in Vulvovaginal Malignant Melanoma. Gynecol. Oncol. 2018, 148, 430–431. [Google Scholar] [CrossRef]
- Rose, P.T.; Nusbaum, B. Robotic Hair Restoration. Dermatol. Clin. 2014, 32, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Du-Harpur, X.; Watt, F.M.; Luscombe, N.M.; Lynch, M.D. What Is AI? Applications of Artificial Intelligence to Dermatology. Br. J. Dermatol. 2020, 183, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Young, A.T.; Xiong, M.; Pfau, J.; Keiser, M.J.; Wei, M.L. Artificial Intelligence in Dermatology: A Primer. J. Investig. Dermatol. 2020, 140, 1504–1512. [Google Scholar] [CrossRef]
- Hogarty, D.T.; Su, J.C.; Phan, K.; Attia, M.; Hossny, M.; Nahavandi, S.; Lenane, P.; Moloney, F.J.; Yazdabadi, A. Artificial Intelligence in Dermatology—Where We Are and the Way to the Future: A Review. Am. J. Clin. Dermatol. 2020, 21, 41–47. [Google Scholar] [CrossRef]
- Codella, N.C.F.; Gutman, D.; Celebi, M.E.; Helba, B.; Marchetti, M.A.; Dusza, S.W.; Kalloo, A.; Liopyris, K.; Mishra, N.; Kittler, H.; et al. Skin Lesion Analysis toward Melanoma Detection: A Challenge at the 2017 International Symposium on Biomedical Imaging (ISBI), Hosted by the International Skin Imaging Collaboration (ISIC). In Proceedings of the 2018 IEEE 15th International Symposium on Biomedical Imaging (ISBI 2018), Washington, DC, USA, 4–7 April 2018; pp. 168–172. [Google Scholar] [CrossRef]
- Codella, N.; Rotemberg, V.; Tschandl, P.; Celebi, M.E.; Dusza, S.; Gutman, D.; Helba, B.; Kalloo, A.; Liopyris, K.; Marchetti, M.; et al. Skin Lesion Analysis Toward Melanoma Detection 2018: A Challenge Hosted by the International Skin Imaging Collaboration (ISIC). In Proceedings of the 2018 IEEE 15th International Symposium on Biomedical Imaging (ISBI 2018), Washington, DC, USA, 4–7 April 2018; pp. 1–12. [Google Scholar]
- Marchetti, M.A.; Liopyris, K.; Dusza, S.W.; Codella, N.C.F.; Gutman, D.A.; Helba, B.; Kalloo, A.; Halpern, A.C. International Skin Imaging Collaboration. Computer algorithms show potential for improving dermatologists’ accuracy to diagnose cutaneous melanoma: Results of the International Skin Imaging Collaboration 2017. J. Am. Acad. Dermatol. 2020, 82, 622–627. [Google Scholar] [CrossRef]
- Kassem, M.A.; Hosny, K.M.; Fouad, M.M. Skin Lesions Classification into Eight Classes for ISIC 2019 Using Deep Convolutional Neural Network and Transfer Learning. IEEE Access 2020, 8, 114822–114832. [Google Scholar] [CrossRef]
- Gottfredson, L.S. Mainstream Science on Intelligence: An Editorial With 52 Signatories, History, and Bibliography. Intelligence 1994, 24, 13–23. [Google Scholar] [CrossRef]
- Russell, S.; Norvig, P. Artificial Intelligence: A Modern Approach, 4th ed.; Prentice Hall: Hoboken, NJ, USA, 2020. [Google Scholar]
- Monett, D.; Lewis, C.W.P.; Thórisson, K.R.; Bach, J.; Baldassarre, G.; Granato, G.; Berkeley, I.S.N.; Chollet, F.; Crosby, M.; Shevlin, H.; et al. Special Issue “On Defining Artificial Intelligence”—CommentarJohn McCarthy’s Definition of Intelligence.Ies and Author’s Response. J. Artif. Gen. Intell. 2020, 11, 1–100. [Google Scholar] [CrossRef]
- Kaplan, A.; Haenlein, M. Siri, Siri, in My Hand: Who’s the Fairest in the Land? On the Interpretations, Illustrations, and Implications of Artificial Intelligence. Bus. Horiz. 2019, 62, 15–25. [Google Scholar] [CrossRef]
- Turing, A.M. On Computable Numbers, with an Application to the Entscheidungsproblem. J. Math. 1936, 58, 5. [Google Scholar]
- McCulloch, W.S.; Pitts, W. A Logical Calculus of the Ideas Immanent in Nervous Activity. Bull. Math. Biophys. 1943, 5, 115–133. [Google Scholar] [CrossRef]
- McCorduck, P. Machines Who Think: A Personal Inquiry into the History and Prospects of Artificial Intelligence, 2nd ed.; AK Peters Ltd.: Natick, MA, USA, 2004. [Google Scholar]
- Widrow, B.; Lehr, M.A. 30 Years of Adaptive Neural Networks: Perceptron, Madaline, and Backpropagation. Proc. IEEE 1990, 78, 1415–1442. [Google Scholar] [CrossRef]
- Lodwick, G.S.; Keats, T.E.; Dorst, J.P. The Coding of Roentgen Images for Computer Analysis as Applied to Lung Cancer. Radiology 1963, 81, 185–200. [Google Scholar] [CrossRef]
- Lindsay, R.K.; Buchanan, B.G.; Feigenbaum, E.A.; Lederberg, J. Applications of Artificial Intelligence for Organic Chemistry: The DENDRAL Project, 1st ed.; McGraw-Hill: New York, NY, USA, 1980. [Google Scholar]
- Gao, Y.; Geras, K.J.; Lewin, A.A.; Moy, L. New Frontiers: An Update on Computer-Aided Diagnosis for Breast Imaging in the Age of Artificial Intelligence. Am. J. Roentgenol. 2019, 212, 300–307. [Google Scholar] [CrossRef]
- Gutkowicz-Krusin, D.; Elbaum, M.; Jacobs, A.; Keem, S.; Kopf, A.W.; Kamino, H.; Wang, S.; Rubin, P.; Rabinovitz, H.; Oliviero, M. Precision of Automatic Measurements of Pigmented Skin Lesion Parameters with a MelaFindTM Multispectral Digital Dermoscope. Melanoma Res. 2000, 10, 563–570. [Google Scholar] [CrossRef]
- Esteva, A.; Robicquet, A.; Ramsundar, B.; Kuleshov, V.; DePristo, M.; Chou, K.; Cui, C.; Corrado, G.; Thrun, S.; Dean, J. A Guide to Deep Learning in Healthcare. Nat. Med. 2019, 25, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Jumper, J.; Evans, R.; Pritzel, A.; Green, T.; Figurnov, M.; Ronneberger, O.; Tunyasuvunakool, K.; Bates, R.; Žídek, A.; Potapenko, A.; et al. Highly Accurate Protein Structure Prediction with AlphaFold. Nature 2021, 596, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Karras, T.; Aittala, M.; Laine, S.; Härkönen, E.; Hellsten, J.; Lehtinen, J.; Aila, T. Alias-Free Generative Adversarial Networks. Adv. Neural Inf. Process. Syst. 2021, 34, 852–863. [Google Scholar]
- Goyal, P.; Caron, M.; Lefaudeux, B.; Xu, M.; Wang, P.; Pai, V.; Singh, M.; Liptchinsky, V.; Misra, I.; Joulin, A. Self-Supervised Pretraining of Visual Features in the Wild. arXiv 2021, arXiv:2103.01988. [Google Scholar]
- Russell, S.J.; Norvig, P. Artificial Intelligence. In The ACM Computing Classification System 1998; Association for Computing Machinery Inc.: New York, NY, USA, 2007; pp. 320–363. [Google Scholar]
- Mitchell, T. Machine Learning, 1st ed.; McGraw-Hill Education Ltd.: New York, NY, USA, 1997. [Google Scholar]
- Yegnanarayana, B. Artificial Neural Networks, 1st ed.; Prentice-Hall of India Pvt. Ltd.: Chennai, India, 2004. [Google Scholar]
- Erickson, B.J.; Korfiatis, P.; Kline, T.L.; Akkus, Z.; Philbrick, K.; Weston, A.D. Deep Learning in Radiology: Does One Size Fit All? J. Am. Coll. Radiol. 2018, 15, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Manne, R.; Kantheti, S.; Kantheti, S. Classification of Skin Cancer Using Deep Learning, Convolutional Neural Networks—Opportunities and Vulnerabilities—A Systematic Review. Int. J. Mod. Trends Sci. Technol. 2020, 6, 101–108. [Google Scholar] [CrossRef]
- Dildar, M.; Akram, S.; Irfan, M.; Khan, H.U.; Ramzan, M.; Mahmood, A.R.; Alsaiari, S.A.; Saeed, A.H.M.; Alraddadi, M.O.; Mahnashi, M.H. Skin Cancer Detection: A Review Using Deep Learning Techniques. Int. J. Environ. Res. Public Health 2021, 18, 5479. [Google Scholar] [CrossRef] [PubMed]
- Fink, C.; Blum, A.; Buhl, T.; Mitteldorf, C.; Hofmann-Wellenhof, R.; Deinlein, T.; Stolz, W.; Trennheuser, L.; Cussigh, C.; Deltgen, D.; et al. Diagnostic Performance of a Deep Learning Convolutional Neural Network in the Differentiation of Combined Naevi and Melanomas. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 1355–1361. [Google Scholar] [CrossRef]
- Alzubaidi, L.; Zhang, J.; Humaidi, A.J.; Al-Dujaili, A.; Duan, Y.; Al-Shamma, O.; Santamaría, J.; Fadhel, M.A.; Al-Amidie, M.; Farhan, L. Review of Deep Learning: Concepts, CNN Architectures, Challenges, Applications, Future Directions; Springer International Publishing: Cham, Switzerland, 2021; Volume 8, ISBN 4053702100444. [Google Scholar]
- Ghosh, A.; Sufian, A.; Sultana, F.; Chakrabarti, A.; De, D. Fundamental Concepts of Convolutional Neural Network. In Recent Trends and Advances in Artificial Intelligence and Internet of Things; Springer: Berlin/Heidelberg, Germany, 2020; pp. 519–567. [Google Scholar]
- Daneshjou, R.; Vodrahalli, K.; Novoa, R.A.; Jenkins, M.; Liang, W.; Rotemberg, V.; Ko, J.; Swetter, S.M.; Bailey, E.E.; Gevaert, O. Disparities in Dermatology AI Performance on a Diverse, Curated Clinical Image Set. arXiv 2022, arXiv:2203.08807. [Google Scholar] [CrossRef]
- Zhao, Z.-Q.; Xu, S.-T.; Liu, D.; Tian, W.-D.; Jiang, Z.-D. A Review of Image Set Classification. Neurocomputing 2019, 335, 251–260. [Google Scholar] [CrossRef]
- Rebouças Filho, P.P.; Peixoto, S.A.; Medeiros da Nóbrega, R.V.; Hemanth, D.J.; Medeiros, A.G.; Sangaiah, A.K.; de Albuquerque, V.H.C. Automatic Histologically-Closer Classification of Skin Lesions. Comput. Med. Imaging Graph. 2018, 68, 40–54. [Google Scholar] [CrossRef]
- Rezvantalab, A.; Safigholi, H.; Karimijeshni, S. Dermatologist Level Dermoscopy Skin Cancer Classification Using Different Deep Learning Convolutional Neural Networks Algorithms. arXiv 2018, arXiv:1810.10348. [Google Scholar]
- Gessert, N.; Sentker, T.; Madesta, F.; Schmitz, R.; Kniep, H.; Baltruschat, I.; Werner, R.; Schlaefer, A. Skin Lesion Diagnosis Using Ensembles, Unscaled Multi-Crop Evaluation and Loss Weighting. arXiv 2018, arXiv:1808.01694. [Google Scholar]
- Gessert, N.; Nielsen, M.; Shaikh, M.; Werner, R.; Schlaefer, A. Skin Lesion Classification Using Ensembles of Multi-Resolution EfficientNets with Meta Data. MethodsX 2020, 7, 100864. [Google Scholar] [CrossRef] [PubMed]
- Haenssle, H.A.; Fink, C.; Schneiderbauer, R.; Toberer, F.; Buhl, T.; Blum, A.; Kalloo, A.; Ben Hadj Hassen, A.; Thomas, L.; Enk, A.; et al. Man against Machine: Diagnostic Performance of a Deep Learning Convolutional Neural Network for Dermoscopic Melanoma Recognition in Comparison to 58 Dermatologists. Ann. Oncol. 2018, 29, 1836–1842. [Google Scholar] [CrossRef]
- Haenssle, H.A.; Fink, C.; Toberer, F.; Winkler, J.; Stolz, W.; Deinlein, T.; Hofmann-Wellenhof, R.; Lallas, A.; Emmert, S.; Buhl, T.; et al. Man against Machine Reloaded: Performance of a Market-Approved Convolutional Neural Network in Classifying a Broad Spectrum of Skin Lesions in Comparison with 96 Dermatologists Working under Less Artificial Conditions. Ann. Oncol. 2020, 31, 137–143. [Google Scholar] [CrossRef]
- Berk-Krauss, J.; Polsky, D.; Stein, J.A. Mole Mapping for Management of Pigmented Skin Lesions. Dermatol. Clin. 2017, 35, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Demers, A.A.; Nugent, Z.; Mihalcioiu, C.; Wiseman, M.C.; Kliewer, E.V. Trends of Nonmelanoma Skin Cancer from 1960 through 2000 in a Canadian Population. J. Am. Acad. Dermatol. 2005, 53, 320–328. [Google Scholar] [CrossRef]
- Weinberg, J.; Kaddu, S.; Gabler, G.; Kovarik, C. The African Teledermatology Project: Providing Access to Dermatologic Care and Education in Sub-Saharan Africa. Pan Afr. Med. J. 2009, 3, 16. [Google Scholar]
- Gaffney, R.; Rao, B. Global Teledermatology. Glob. Dermatol. 2015, 2, 209–214. [Google Scholar] [CrossRef]
- Kaliyadan, F.; Ashique, K.T. Use of Mobile Applications in Dermatology. Indian J. Dermatol. 2020, 65, 371–376. [Google Scholar] [CrossRef]
- Freeman, K.; Dinnes, J.; Chuchu, N.; Takwoingi, Y.; Bayliss, S.E.; Matin, R.N.; Jain, A.; Walter, F.M.; Williams, H.C.; Deeks, J.J. Algorithm Based Smartphone Apps to Assess Risk of Skin Cancer in Adults: Systematic Review of Diagnostic Accuracy Studies. BMJ 2020, 368, m127. [Google Scholar] [CrossRef] [PubMed]
- Veronese, F.; Branciforti, F.; Zavattaro, E.; Tarantino, V.; Romano, V.; Meiburger, K.M.; Salvi, M.; Seoni, S.; Savoia, P. The Role in Teledermoscopy of an Inexpensive and Easy-to-Use Smartphone Device for the Classification of Three Types of Skin Lesions Using Convolutional Neural Networks. Diagnostics 2021, 11, 451. [Google Scholar] [CrossRef] [PubMed]
- Eisentha, Y.; Dror, G.; Ruppin, E. Facial Attractiveness: Beauty and the Machine. Neural Comput. 2006, 18, 119–142. [Google Scholar] [CrossRef] [PubMed]
- Kagian, A.; Dror, G.; Leyvand, T.; Meilijson, I.; Cohen-Or, D.; Ruppin, E. A Machine Learning Predictor of Facial Attractiveness Revealing Human-like Psychophysical Biases. Vis. Res. 2008, 48, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Esteva, A.; Kuprel, B.; Novoa, R.A.; Ko, J.; Swetter, S.M.; Blau, H.M.; Thrun, S. Dermatologist-Level Classification of Skin Cancer with Deep Neural Networks. Nature 2017, 542, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Mahbod, A.; Tschandl, P.; Langs, G.; Ecker, R.; Ellinger, I. The Effects of Skin Lesion Segmentation on the Performance of Dermatoscopic Image Classification. Comput. Methods Programs Biomed. 2020, 197, 105725. [Google Scholar] [CrossRef]
- Mahbod, A.; Schaefer, G.; Wang, C.; Dorffner, G.; Ecker, R.; Ellinger, I. Transfer Learning Using a Multi-Scale and Multi-Network Ensemble for Skin Lesion Classification. Comput. Methods Programs Biomed. 2020, 193, 105475. [Google Scholar] [CrossRef]
- Mirikharaji, Z.; Abhishek, K.; Izadi, S.; Hamarneh, G. D-LEMA: Deep Learning Ensembles from Multiple Annotations-Application to Skin Lesion Segmentation. In Proceedings of the 2021 IEEE/CVF Conference on Computer Vision and Pattern Recognition Workshops (CVPRW), Nashville, TN, USA, 19–25 June 2021; pp. 1837–1846. [Google Scholar] [CrossRef]
- Yang, C.-H.; Ren, J.-H.; Huang, H.-C.; Chuang, L.-Y.; Chang, P.-Y. Deep Hybrid Convolutional Neural Network for Segmentation of Melanoma Skin Lesion. Comput. Intell. Neurosci. 2021, 2021, 9409508. [Google Scholar] [CrossRef]
- Iqbal, I.; Younus, M.; Walayat, K.; Kakar, M.U.; Ma, J. Automated Multi-Class Classification of Skin Lesions through Deep Convolutional Neural Network with Dermoscopic Images. Comput. Med. Imaging Graph. 2021, 88, 101843. [Google Scholar] [CrossRef]
- Mirikharaji, Z.; Yan, Y.; Hamarneh, H. Learning to Segment Skin Lesions from Noisy Annotations; Springer International Publishing: Cham, Switzerland, 2019; Volume 4, ISBN 9783030333911. [Google Scholar]
- Qin, Z.; Liu, Z.; Zhu, P.; Xue, Y. A GAN-Based Image Synthesis Method for Skin Lesion Classification. Comput. Methods Programs Biomed. 2020, 195, 105568. [Google Scholar] [CrossRef]
- Cano, E.; Mendoza-Avilés, J.; Areiza, M.; Guerra, N.; Mendoza-Valdés, J.L.; Rovetto, C.A. Multi Skin Lesions Classification Using Fine-Tuning and Data-Augmentation Applying Nasnet. PeerJ Comput. Sci. 2021, 7, e371. [Google Scholar] [CrossRef]
- Barhoumi, W.; Khelifa, A. Skin Lesion Image Retrieval Using Transfer Learning-Based Approach for Query-Driven Distance Recommendation. Comput. Biol. Med. 2021, 137, 104825. [Google Scholar] [CrossRef] [PubMed]
- Ratul, M.A.R.; Mozaffari, M.H.; Lee, W.-S.; Parimbelli, E. Skin Lesions Classification Using Deep Learning Based on Dilated Convolution. bioRxiv 2020. [Google Scholar] [CrossRef]
- Rashid, H.; Tanveer, M.A.; Aqeel Khan, H. Skin Lesion Classification Using GAN Based Data Augmentation. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 916–919. [Google Scholar] [CrossRef]
- Maron, R.C.; Weichenthal, M.; Utikal, J.S.; Hekler, A.; Berking, C.; Hauschild, A.; Enk, A.H.; Haferkamp, S.; Klode, J.; Schadendorf, D.; et al. Systematic Outperformance of 112 Dermatologists in Multiclass Skin Cancer Image Classification by Convolutional Neural Networks. Eur. J. Cancer 2019, 119, 57–65. [Google Scholar] [CrossRef]
- Sun, Q.; Huang, C.; Chen, M.; Xu, H.; Yang, Y. Skin Lesion Classification Using Additional Patient Information. BioMed Res. Int. 2021, 2021, 6673852. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Singhania, U.; Tripathy, B.; Nasr, E.A.; Aboudaif, M.K.; Kamrani, A.K. Deep Learning-Based Transfer Learning for Classification of Skin Cancer. Sensors 2021, 21, 8142. [Google Scholar] [CrossRef] [PubMed]
- Winkler, J.K.; Sies, K.; Fink, C.; Toberer, F.; Enk, A.; Deinlein, T.; Hofmann-Wellenhof, R.; Thomas, L.; Lallas, A.; Blum, A.; et al. Melanoma Recognition by a Deep Learning Convolutional Neural Network—Performance in Different Melanoma Subtypes and Localisations. Eur. J. Cancer 2020, 127, 21–29. [Google Scholar] [CrossRef]
- Binder, M.; Steiner, A.; Schwarz, M.; Knollmayer, S.; Wolff, K.; Pehamberger, H. Application of an Artificial Neural Network in Epiluminescence Microscopy Pattern Analysis of Pigmented Skin Lesions: A Pilot Study. Br. J. Dermatol. 1994, 130, 460–465. [Google Scholar] [CrossRef]
- Sies, K.; Winkler, J.K.; Fink, C.; Bardehle, F.; Toberer, F.; Buhl, T.; Enk, A.; Blum, A.; Rosenberger, A.; Haenssle, H.A. Past and Present of Computer-Assisted Dermoscopic Diagnosis: Performance of a Conventional Image Analyser versus a Convolutional Neural Network in a Prospective Data Set of 1,981 Skin Lesions. Eur. J. Cancer 2020, 135, 39–46. [Google Scholar] [CrossRef]
- Yang, Y.; Ge, Y.; Guo, L.; Wu, Q.; Peng, L.; Zhang, E.; Xie, J.; Li, Y.; Lin, T. Development and Validation of Two Artificial Intelligence Models for Diagnosing Benign, Pigmented Facial Skin Lesions. Ski. Res. Technol. 2021, 27, 74–79. [Google Scholar] [CrossRef]
- Lyakhov, P.A.; Lyakhova, U.A.; Nagornov, N.N. System for the Recognizing of Pigmented Skin Lesions with Fusion and Analysis of Heterogeneous Data Based on a Multimodal Neural Network. Cancers 2022, 14, 1819. [Google Scholar] [CrossRef] [PubMed]
- De Guzman, L.C.; Maglaque, R.P.C.; Torres, V.M.B.; Zapido, S.P.A.; Cordel, M.O. Design and Evaluation of a Multi-Model, Multi-Level Artificial Neural Network for Eczema Skin Lesion Detection. In Proceedings of the 2015 3rd International Conference on Artificial Intelligence, Modelling and Simulation (AIMS), Kota Kinabalu, Malaysia, 2–4 December 2015; pp. 42–47. [Google Scholar] [CrossRef]
- Han, S.S.; Park, G.H.; Lim, W.; Kim, M.S.; Na, J.I.; Park, I.; Chang, S.E. Deep Neural Networks Show an Equivalent and Often Superior Performance to Dermatologists in Onychomycosis Diagnosis: Automatic Construction of Onychomycosis Datasets by Region-Based Convolutional Deep Neural Network. PLoS ONE 2018, 13, e0191493. [Google Scholar] [CrossRef]
- Blum, A.; Luedtke, H.; Ellwanger, U.; Schwabe, R.; Rassner, G.; Garbe, C. Digital Image Analysis for Diagnosis of Cutaneous Melanoma. Development of a Highly Effective Computer Algorithm Based on Analysis of 837 Melanocytic Lesions. Br. J. Dermatol. 2004, 151, 1029–1038. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, M.A.; Codella, N.C.F.; Dusza, S.W.; Gutman, D.A.; Helba, B.; Kalloo, A.; Mishra, N.; Carrera, C.; Celebi, M.E.; DeFazio, J.L.; et al. Results of the 2016 International Skin Imaging Collaboration International Symposium on Biomedical Imaging Challenge: Comparison of the Accuracy of Computer Algorithms to Dermatologists for the Diagnosis of Melanoma from Dermoscopic Images. J. Am. Acad. Dermatol. 2018, 78, 270–277.e1. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Zhang, J.; Yan, C.; Zhou, H. An Automatic Diagnosis Method of Facial Acne Vulgaris Based on Convolutional Neural Network. Sci. Rep. 2018, 8, 5839. [Google Scholar] [CrossRef] [PubMed]
- Seité, S.; Khammari, A.; Benzaquen, M.; Moyal, D.; Dréno, B. Development and Accuracy of an Artificial Intelligence Algorithm for Acne Grading from Smartphone Photographs. Exp. Dermatol. 2019, 28, 1252–1257. [Google Scholar] [CrossRef]
- Zhao, S.; Xie, B.; Li, Y.; Zhao, X.; Kuang, Y.; Su, J.; He, X.; Wu, X.; Fan, W.; Huang, K.; et al. Smart Identification of Psoriasis by Images Using Convolutional Neural Networks: A Case Study in China. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 518–524. [Google Scholar] [CrossRef]
- Han, S.S.; Park, I.; Eun Chang, S.; Lim, W.; Kim, M.S.; Park, G.H.; Chae, J.B.; Huh, C.H.; Na, J.I. Augmented Intelligence Dermatology: Deep Neural Networks Empower Medical Professionals in Diagnosing Skin Cancer and Predicting Treatment Options for 134 Skin Disorders. J. Investig. Dermatol. 2020, 140, 1753–1761. [Google Scholar] [CrossRef]
- Roffman, D.; Hart, G.; Girardi, M.; Ko, C.J.; Deng, J. Predicting Non-Melanoma Skin Cancer via a Multi-Parameterized Artificial Neural Network. Sci. Rep. 2018, 8, 1701. [Google Scholar] [CrossRef]
- Alzubaidi, L.; Al-Amidie, M.; Al-Asadi, A.; Humaidi, A.J.; Al-Shamma, O.; Fadhel, M.A.; Zhang, J.; Santamaría, J.; Duan, Y. Novel Transfer Learning Approach for Medical Imaging with Limited Labeled Data. Cancers 2021, 13, 1590. [Google Scholar] [CrossRef]
- Guimarães, P.; Batista, A.; Zieger, M.; Kaatz, M.; Koenig, K. Artificial Intelligence in Multiphoton Tomography: Atopic Dermatitis Diagnosis. Sci. Rep. 2020, 10, 7968. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.Y.; Kindler, J.M.; Persohn, S.; Kralik, S.F.; Robertson, K.A.; Territo, P.R. Image Segmentation of Plexiform Neurofibromas from a Deep Neural Network Using Multiple B-Value Diffusion Data. Sci. Rep. 2020, 10, 17857. [Google Scholar] [CrossRef] [PubMed]
- Fink, C.; Fuchs, T.; Enk, A.; Haenssle, H.A. Design of an Algorithm for Automated, Computer-Guided PASI Measurements by Digital Image Analysis. J. Med. Syst. 2018, 42, 248. [Google Scholar] [CrossRef] [PubMed]
- Fink, C.; Alt, C.; Uhlmann, L.; Klose, C.; Enk, A.; Haenssle, H.A. Precision and Reproducibility of Automated Computer-Guided Psoriasis Area and Severity Index Measurements in Comparison with Trained Physicians. Br. J. Dermatol. 2019, 180, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Schnürle, S.; Pouly, M.; Vor Der Brück, T.; Navarini, A.; Koller, T. On Using Support Vector Machines for the Detection and Quantification of Hand Eczema. In Proceedings of the 9th International Conference on Agents and Artificial Intelligence (ICAART 2017), Porto, Portugal, 24–26 February 2017; Volume 2, pp. 75–84. [Google Scholar] [CrossRef]
- Gao, W.; Li, M.; Wu, R.; Du, W.; Zhang, S.; Yin, S.; Chen, Z.; Huang, H. The Design and Application of an Automated Microscope Developed Based on Deep Learning for Fungal Detection in Dermatology. Mycoses 2021, 64, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Bashat, D.B.; Artzi, M.; Ganut, T.; Vitinshtein, F.; Ben-Sira, L.; Bokstein, F. Differentiation between Plexiform Neurofibromas and Malignant Nerve Sheath Tumors in Patients with Neurofibromatosis Type 1 (NF1) Using Radiomics Analysis of MRI. In Proceedings of the European Congress of Radiology-ECR 2019, Vienna, Austria, 27 February–3 March 2019. [Google Scholar]
- Duarte, J.V.; Ribeiro, M.J.; Violante, I.R.; Cunha, G.; Silva, E.; Castelo-Branco, M. Multivariate Pattern Analysis Reveals Subtle Brain Anomalies Relevant to the Cognitive Phenotype in Neurofibromatosis Type 1. Hum. Brain Mapp. 2014, 35, 89–106. [Google Scholar] [CrossRef]
- Meienberger, N.; Anzengruber, F.; Amruthalingam, L.; Christen, R.; Koller, T.; Maul, J.T.; Pouly, M.; Djamei, V.; Navarini, A.A. Observer-Independent Assessment of Psoriasis-Affected Area Using Machine Learning. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 1362–1368. [Google Scholar] [CrossRef]
- Gustafson, E.; Pacheco, J.; Wehbe, F.; Silverberg, J.; Thompson, W. A Machine Learning Algorithm for Identifying Atopic Dermatitis in Adults from Electronic Health Records. In Proceedings of the 2017 IEEE International Conference on Healthcare Informatics (ICHI), Park City, UT, USA, 23–26 August 2017; pp. 83–90. [Google Scholar] [CrossRef]
- Luo, W.; Liu, J.; Huang, Y.; Zhao, N. An Effective Vitiligo Intelligent Classification System. J. Ambient Intell. Humaniz. Comput. 2020. [Google Scholar] [CrossRef]
- Low, M.; Huang, V.; Raina, P. Automating Vitiligo Skin Lesion Segmentation Using Convolutional Neural Networks. In Proceedings of the 2020 IEEE 17th International Symposium on Biomedical Imaging (ISBI), Iowa City, IA, USA, 3–7 April 2020; pp. 1992–1995. [Google Scholar] [CrossRef]
- Zhang, L.; Zhang, D.; Sun, M.M.; Chen, F.M. Facial Beauty Analysis Based on Geometric Feature: Toward Attractiveness Assessment Application. Expert Syst. Appl. 2017, 82, 252–265. [Google Scholar] [CrossRef]
- Cassidy, B.; Kendrick, C.; Brodzicki, A.; Jaworek-Korjakowska, J.; Yap, M.H. Analysis of the ISIC Image Datasets: Usage, Benchmarks and Recommendations. Med. Image Anal. 2022, 75, 102305. [Google Scholar] [CrossRef]
- Garcia-Arroyo, J.L.; Garcia-Zapirain, B. Segmentation of Skin Lesions in Dermoscopy Images Using Fuzzy Classification of Pixels and Histogram Thresholding. Comput. Methods Programs Biomed. 2019, 168, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Lucius, M.; De All, J.; De All, J.A.; Belvisi, M.; Radizza, L.; Lanfranconi, M.; Lorenzatti, V.; Galmarini, C.M. Deep Neural Frameworks Improve the Accuracy of General Practitioners in the Classification of Pigmented Skin Lesions. Diagnostics 2020, 10, 969. [Google Scholar] [CrossRef] [PubMed]
- Minagawa, A.; Koga, H.; Sano, T.; Matsunaga, K.; Teshima, Y.; Hamada, A.; Houjou, Y.; Okuyama, R. Dermoscopic Diagnostic Performance of Japanese Dermatologists for Skin Tumors Differs by Patient Origin: A Deep Learning Convolutional Neural Network Closes the Gap. J. Dermatol. 2021, 48, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Al-masni, M.A.; Kim, D.-H.H.; Kim, T.-S.S. Multiple Skin Lesions Diagnostics via Integrated Deep Convolutional Networks for Segmentation and Classification. Comput. Methods Programs Biomed. 2020, 190, 105351. [Google Scholar] [CrossRef]
- Singhal, A.; Shukla, R.; Kankar, P.K.; Dubey, S.; Singh, S.; Pachori, R.B. Comparing the Capabilities of Transfer Learning Models to Detect Skin Lesion in Humans. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2020, 234, 1083–1093. [Google Scholar] [CrossRef]
- Le, D.N.T.; Le, H.X.; Ngo, L.T.; Ngo, H.T. Transfer Learning with Class-Weighted and Focal Loss Function for Automatic Skin Cancer Classification. arXiv 2020, arXiv:2009.05977. [Google Scholar]
- Lei, B.; Xia, Z.; Jiang, F.; Jiang, X.; Ge, Z.; Xu, Y.; Qin, J.; Chen, S.; Wang, T.; Wang, S. Skin Lesion Segmentation via Generative Adversarial Networks with Dual Discriminators. Med. Image Anal. 2020, 64, 101716. [Google Scholar] [CrossRef]
- International Skin Imaging Collaboration (ISIC) Sixth ISIC Skin Image Analysis Workshop@ CVPR 2021 Virtual. Available online: https://workshop2021.isic-archive.com (accessed on 15 October 2022).
- Ferrara, G.; Argenziano, G. The WHO 2018 Classification of Cutaneous Melanocytic Neoplasms: Suggestions from Routine Practice. Front. Oncol. 2021, 11, 675296. [Google Scholar] [CrossRef]
- Braun, R.P.; Rabinovitz, H.S.; Oliviero, M.; Kopf, A.W.; Saurat, J.-H. Dermoscopy of Pigmented Skin Lesions. J. Am. Acad. Dermatol. 2005, 52, 109–121. [Google Scholar] [CrossRef]
- Tschandl, P.; Codella, N.; Akay, B.N.; Argenziano, G.; Braun, R.P.; Cabo, H.; Gutman, D.; Halpern, A.; Helba, B.; Hofmann-wellenhof, R.; et al. Comparison of the Accuracy of Human Readers versus Machine-Learning Algorithms for Pigmented Skin Lesion Classification: An Open, Web-Based, International, Diagnostic Study. Lancet Oncol. 2019, 20, 938–947. [Google Scholar] [CrossRef]
- Penn, L.; Rothman, L.; Sutton, A.M.; Brinster, N.K.; Vidal, C.I. What’s New in Dermatopathology: Inflammatory Dermatoses. Adv. Anat. Pathol. 2019, 26, 40–55. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the Global Cancer Incidence and Mortality in 2018: GLOBOCAN Sources and Methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Leiter, U.; Keim, U.; Garbe, C. Epidemiology of Skin Cancer: Update 2019. In Sunlight, Vitamin D and Skin Cancer; Reichrath, J., Ed.; Springer: Cham, Switzerland, 2020; ISBN 9780123819789. [Google Scholar]
- Lomas, A.; Leonardi-Bee, J.; Bath-Hextall, F. A Systematic Review of Worldwide Incidence of Nonmelanoma Skin Cancer. Br. J. Dermatol. 2012, 166, 1069–1080. [Google Scholar] [CrossRef] [PubMed]
- Schadendorf, D.; van Akkooi, A.C.J.; Berking, C.; Griewank, K.G.; Gutzmer, R.; Hauschild, A.; Stang, A.; Roesch, A.; Ugurel, S. Melanoma. Lancet 2018, 392, 971–984. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Friedman, R.J.; Rigel, D.S.; Kopf, A.W. Early Detection of Malignant Melanoma: The Role of Physician Examination and Self-Examination of the Skin. CA Cancer J. Clin. 1985, 35, 130–151. [Google Scholar] [CrossRef] [PubMed]
- Magro, C.M.; Neil Crowson, A.; Mihm, M.C. Unusual Variants of Malignant Melanoma. Mod. Pathol. 2006, 19, 41–70. [Google Scholar] [CrossRef]
- Tang, P.; Liang, Q.; Yan, X.; Xiang, S.; Sun, W.; Zhang, D.; Coppola, G. Efficient Skin Lesion Segmentation Using Separable-Unet with Stochastic Weight Averaging. Comput. Methods Programs Biomed. 2019, 178, 289–301. [Google Scholar] [CrossRef]
- MacLellan, A.N.; Price, E.L.; Publicover-Brouwer, P.; Matheson, K.; Ly, T.Y.; Pasternak, S.; Walsh, N.M.; Gallant, C.J.; Oakley, A.; Hull, P.R.; et al. The Use of Non-Invasive Imaging Techniques in the Diagnosis of Melanoma: A Prospective Diagnostic Accuracy Study. J. Am. Acad. Dermatol. 2020, 85, 353–359. [Google Scholar] [CrossRef]
- Winkler, J.K.; Sies, K.; Fink, C.; Toberer, F.; Enk, A.; Abassi, M.S.; Fuchs, T.; Haenssle, H.A. Association between Different Scale Bars in Dermoscopic Images and Diagnostic Performance of a Market-Approved Deep Learning Convolutional Neural Network for Melanoma Recognition. Eur. J. Cancer 2021, 145, 146–154. [Google Scholar] [CrossRef]
- Sinclair, R.; Meah, N.; Arasu, A. Skin Checks in Primary Care. Aust. J. Gen. Pract. 2019, 48, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Rayner, J.E.; Laino, A.M.; Nufer, K.L.; Adams, L.; Raphael, A.P.; Menzies, S.W.; Soyer, H.P. Clinical Perspective of 3D Total Body Photography for Early Detection and Screening of Melanoma. Front. Med. 2018, 5, 152. [Google Scholar] [CrossRef] [PubMed]
- Primiero, C.A.; McInerney-Leo, A.M.; Betz-Stablein, B.; Whiteman, D.C.; Gordon, L.; Caffery, L.; Aitken, J.F.; Eakin, E.; Osborne, S.; Gray, L.; et al. Evaluation of the Efficacy of 3D Total-Body Photography with Sequential Digital Dermoscopy in a High-Risk Melanoma Cohort: Protocol for a Randomised Controlled Trial. BMJ Open 2019, 9, e032969. [Google Scholar] [CrossRef] [PubMed]
- McClatchey, A.I. Neurofibromatosis. Annu. Rev. Pathol. 2007, 2, 191–216. [Google Scholar] [CrossRef] [PubMed]
- Boyd, K.P.; Korf, B.R.; Theos, A. Neurofibromatosis Type 1. J. Am. Acad. Dermatol. 2009, 61, 1–14; quiz 15–16, quiz 15–16. [Google Scholar] [CrossRef] [PubMed]
- Wei, C.J.; Yan, C.; Tang, Y.; Wang, W.; Gu, Y.H.; Ren, J.Y.; Cui, X.W.; Lian, X.; Liu, J.; Wang, H.J.; et al. Computed Tomography–Based Differentiation of Benign and Malignant Craniofacial Lesions in Neurofibromatosis Type I Patients: A Machine Learning Approach. Front. Oncol. 2020, 10, 1192. [Google Scholar] [CrossRef]
- Parisi, R.; Symmons, D.P.M.; Griffiths, C.E.M.; Ashcroft, D.M. Global Epidemiology of Psoriasis: A Systematic Review of Incidence and Prevalence. J. Investig. Dermatol. 2013, 133, 377–385. [Google Scholar] [CrossRef]
- van de Kerkhof, P.C. the Psoriasis Area and Severity Index and Alternative Approaches for the Assessment of Severity: Persisting Areas of Confusion. Br. J. Dermatol. 1997, 137, 661–662. [Google Scholar] [CrossRef][Green Version]
- Walsh, J.A.; McFadden, M.; Woodcock, J.; Clegg, D.O.; Helliwell, P.; Dommasch, E.; Gelfand, J.M.; Krueger, G.G.; Duffin, K.C. Product of the Physician Global Assessment and Body Surface Area: A Simple Static Measure of Psoriasis Severity in a Longitudinal Cohort. J. Am. Acad. Dermatol. 2013, 69, 931–937. [Google Scholar] [CrossRef]
- Bozek, A.; Reich, A. The Reliability of Three Psoriasis Assessment Tools: Psoriasis Area and Severity Index, Body Surface Area and Physician Global Assessment. Adv. Clin. Exp. Med. 2017, 26, 851–856. [Google Scholar] [CrossRef]
- Pal, A.; Chaturvedi, A.; Garain, U.; Chandra, A.; Chatterjee, R. Severity Grading of Psoriatic Plaques Using Deep CNN Based Multi-Task Learning. In Proceedings of the 2016 23rd International Conference on Pattern Recognition (ICPR), Cancun, Mexico, 4–8 December 2016; pp. 1478–1483. [Google Scholar] [CrossRef]
- Pal, A.; Chaturvedi, A.; Chandra, A.; Chatterjee, R.; Senapati, S.; Frangi, A.F.; Garain, U. MICaps: Multi-Instance Capsule Network for Machine Inspection of Munro’s Microabscess. Comput. Biol. Med. 2022, 140, 105071. [Google Scholar] [CrossRef] [PubMed]
- Emam, S.; Du, A.X.; Surmanowicz, P.; Thomsen, S.F.; Greiner, R.; Gniadecki, R. Predicting the Long-Term Outcomes of Biologics in Patients with Psoriasis Using Machine Learning. Br. J. Dermatol. 2020, 182, 1305–1307. [Google Scholar] [CrossRef] [PubMed]
- Diepgen, T.L.; Andersen, K.E.; Chosidow, O.; Coenraads, P.J.; Elsner, P.; English, J.; Fartasch, M.; Gimenez-Arnau, A.; Nixon, R.; Sasseville, D.; et al. Guidelines for Diagnosis, Prevention and Treatment of Hand Eczema—Short Version. JDDG—J. Ger. Soc. Dermatol. 2015, 13, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Garzorz-Stark, N.; Eyerich, K. Molecular Diagnostics of Hand Eczema. Hautarzt 2019, 70, 760–765. [Google Scholar] [CrossRef] [PubMed]
- Weidinger, S.; Novak, N. Atopic Dermatitis. Lancet 2016, 387, 1109–1122. [Google Scholar] [CrossRef]
- Drucker, A.M.; Wang, A.R.; Li, W.Q.; Sevetson, E.; Block, J.K.; Qureshi, A.A. The Burden of Atopic Dermatitis: Summary of a Report for the National Eczema Association. J. Investig. Dermatol. 2017, 137, 26–30. [Google Scholar] [CrossRef]
- Patella, V.; Florio, G.; Palmieri, M.; Bousquet, J.; Tonacci, A.; Giuliano, A.; Gangemi, S. Atopic Dermatitis Severity during Exposure to Air Pollutants and Weather Changes with an Artificial Neural Network (ANN) Analysis. Pediatr. Allergy Immunol. 2020, 31, 938–945. [Google Scholar] [CrossRef]
- Melina, A.; Dinh, N.N.; Tafuri, B.; Schipani, G.; Nisticò, S.; Cosentino, C.; Amato, F.; Thiboutot, D.; Cherubini, A. Artificial Intelligence for the Objective Evaluation of Acne Investigator Global Assessment. J. Drugs Dermatol. 2018, 17, 1006–1009. [Google Scholar]
- Maul, L.V.; Meienberger, N.; Kaufmann, L. Role of Artificial Intelligence in Assessing the Extent and Progression of Dermatoses. Hautarzt 2020, 71, 677–685. [Google Scholar] [CrossRef]
- Brewer, A.C.; Endly, D.C.; Henley, J.; Amir, M.; Sampson, B.P.; Moreau, J.F.; Dellavalle, R.P. Mobile Applications in Dermatology. JAMA Dermatol. 2013, 149, 1300–1304. [Google Scholar] [CrossRef]
- De, A. Next-Generation Technologies in Dermatology: Use of Artificial Intelligence and Mobile Applications. Indian J. Dermatol. 2020, 65, 351. [Google Scholar] [CrossRef] [PubMed]
- Swetter, S.M.; Tsao, H.; Bichakjian, C.K.; Curiel-Lewandrowski, C.; Elder, D.E.; Gershenwald, J.E.; Guild, V.; Grant-Kels, J.M.; Halpern, A.C.; Johnson, T.M.; et al. Guidelines of Care for the Management of Primary Cutaneous Melanoma. J. Am. Acad. Dermatol. 2019, 80, 208–250. [Google Scholar] [CrossRef] [PubMed]
- Tintle, S.M.; Keeling, J.J.; Shawen, S.B.; Forsberg, J.A.; Potter, B.K. Traumatic and Trauma-Related Amputations: Part I: General Principles and Lower-Extremity Amputations. J. Bone Jt. Surg. Am. 2010, 92, 2852–2868. [Google Scholar] [CrossRef] [PubMed]
- Tintle, S.M.; Baechler, M.F.; Nanos, G.P., 3rd; Forsberg, J.A.; Potter, B.K. Traumatic and Trauma-Related Amputations: Part II: Upper Extremity and Future Directions. J. Bone Jt. Surg. Am. 2010, 92, 2934–2945. [Google Scholar] [CrossRef]
- Harwell, R.C.; Ferguson, R.L. Physiologic Tremor and Microsurgery. Microsurgery 1983, 4, 187–192. [Google Scholar] [CrossRef]
- Bodenstedt, S.; Wagner, M.; Müller-Stich, B.P.; Weitz, J.; Speidel, S. Artificial Intelligence-Assisted Surgery: Potential and Challenges. Visc. Med. 2020, 36, 450–455. [Google Scholar] [CrossRef]
- Fagius, J.; Nordin, M.; Wall, M. Sympathetic Nerve Activity to Amputated Lower Leg in Humans: Evidence of Altered Skin Vasoconstrictor Discharge. Pain 2002, 98, 37–45. [Google Scholar] [CrossRef]
- Cutrone, A.; Micera, S. Implantable Neural Interfaces and Wearable Tactile Systems for Bidirectional Neuroprosthetics Systems. Adv. Healthc. Mater. 2019, 8, e1801345. [Google Scholar] [CrossRef]
- Parajuli, N.; Sreenivasan, N.; Bifulco, P.; Cesarelli, M.; Savino, S.; Niola, V.; Esposito, D.; Hamilton, T.J.; Naik, G.R.; Gunawardana, U.; et al. Real-Time EMG Based Pattern Recognition Control for Hand Prostheses: A Review on Existing Methods, Challenges and Future Implementation. Sensors 2019, 19, 4596. [Google Scholar] [CrossRef]
- Sohn, W.; Finley, D.S.; Jakowatz, J.; Ornstein, D.K. Robot-Assisted Laparoscopic Transperitoneal Pelvic Lymphadenectomy and Metastasectomy for Melanoma: Initial Report of Two Cases. J. Robot. Surg. 2010, 4, 129–132. [Google Scholar] [CrossRef]
- Hyde, G.A.; Jung, N.L.; Valle, A.A.; Bhattacharya, S.D.; Keel, C.E. Robotic Inguinal Lymph Node Dissection for Melanoma: A Novel Approach to a Complicated Problem. J. Robot. Surg. 2018, 12, 745–748. [Google Scholar] [CrossRef] [PubMed]
- Miura, J.T.; Dossett, L.A.; Thapa, R.; Kim, Y.; Potdar, A.; Daou, H.; Sun, J.; Sarnaik, A.A.; Zager, J.S. Robotic-Assisted Pelvic Lymphadenectomy for Metastatic Melanoma Results in Durable Oncologic Outcomes. Ann. Surg. Oncol. 2020, 27, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Bicknell, L.M.; Kash, N.; Kavouspour, C.; Rashid, R.M. Follicular Unit Extraction Hair Transplant Harvest: A Review of Current Recommendations and Future Considerations. Dermatol. Online J. 2014, 20, doj_21754. [Google Scholar] [CrossRef]
- Wang, X.; Shu, X.; Li, Z.; Huo, W.; Zou, L.; Tang, Y.; Li, L. Comparison of Two Kinds of Skin Imaging Analysis Software: VISIA(®) from Canfield and IPP(®) from Media Cybernetics. Ski. Res. Technol. 2018, 24, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Holcomb, J.D. Helium Plasma Dermal Resurfacing: VISIA CR Assessment of Facial Spots, Pores, and Wrinkles-Preliminary Findings. J. Cosmet. Dermatol. 2021, 20, 1668–1678. [Google Scholar] [CrossRef] [PubMed]
- Goldsberry, A.; Hanke, C.W.; Hanke, K.E. VISIA System: A Possible Tool in the Cosmetic Practice. J. Drugs Dermatol. 2014, 13, 1312–1314. [Google Scholar] [PubMed]
- Šuchmannová, J.; Fikrle, T.; Pizinger, K. Diagnostika Maligního Melanomu s Využitím Celotělového Skenu. Czecho-Slovak Dermatol 2019, 94, 18–22. [Google Scholar]
- Linming, F.; Wei, H.; Anqi, L.; Yuanyu, C.; Heng, X.; Sushmita, P.; Yiming, L.; Li, L. Comparison of Two Skin Imaging Analysis Instruments: The VISIA® from Canfield vs. the ANTERA 3D®CS from Miravex. Ski. Res. Technol. 2018, 24, 3–8. [Google Scholar] [CrossRef]
- Messaraa, C.; Metois, A.; Walsh, M.; Flynn, J.; Doyle, L.; Robertson, N.; Mansfield, A.; O’Connor, C.; Mavon, A. Antera 3D Capabilities for Pore Measurements. Ski. Res. Technol. 2018, 24, 606–613. [Google Scholar] [CrossRef]
- Messaraa, C.; Metois, A.; Walsh, M.; Hurley, S.; Doyle, L.; Mansfield, A.; O’Connor, C.; Mavon, A. Wrinkle and Roughness Measurement by the Antera 3D and Its Application for Evaluation of Cosmetic Products. Ski. Res. Technol. 2018, 24, 359–366. [Google Scholar] [CrossRef]
- McKoy, K.; Halpern, S.; Mutyambizi, K. International Teledermatology Review. Curr. Dermatol. Rep. 2021, 10, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y. Telemedicine and AI for Dermatology Care in China. In Proceedings of the 8th World Congress of Imaging and AI for Skin Diseases, 5–6 November 2020; International Society of Teledermatology: Beijing, China, 2020. [Google Scholar]
- bei Riesenzellarteriitis, D. Kompass Autoimmun; Karger Publishers: Basel, Switzerland, 2020. [Google Scholar]
- Polesie, S.; Gillstedt, M.; Kittler, H.; Lallas, A.; Tschandl, P.; Zalaudek, I.; Paoli, J. Attitudes towards Artificial Intelligence within Dermatology: An International Online Survey. Br. J. Dermatol. 2020, 183, 159–161. [Google Scholar] [CrossRef] [PubMed]
- Ching, T.; Himmelstein, D.S.; Beaulieu-Jones, B.K.; Kalinin, A.A.; Do, B.T.; Way, G.P.; Ferrero, E.; Agapow, P.-M.; Zietz, M.; Hoffman, M.M.; et al. Opportunities and Obstacles for Deep Learning in Biology and Medicine. J. R. Soc. Interface 2018, 15, 20170387. [Google Scholar] [CrossRef] [PubMed]
- Winkler, J.K.; Fink, C.; Toberer, F.; Enk, A.; Deinlein, T.; Hofmann-Wellenhof, R.; Thomas, L.; Lallas, A.; Blum, A.; Stolz, W.; et al. Association between Surgical Skin Markings in Dermoscopic Images and Diagnostic Performance of a Deep Learning Convolutional Neural Network for Melanoma Recognition. JAMA Dermatol. 2019, 155, 1135–1141. [Google Scholar] [CrossRef] [PubMed]
- Haw, W.Y.D.; Al-janabi, A.D.; Arents, B.W.M.D.; Asfour, L.D.; Exton, L.S.D.; Grindlay, D.D.; Khan, S.S.D. Global Guidelines in Dermatology Mapping Project (GUIDEMAP): A Scoping Review of Dermatology Clinical Practice Guidelines. Br. J. Dermatol. 2021, 185, 736–744. [Google Scholar] [CrossRef] [PubMed]
- Bera, K.; Schalper, K.A.; Rimm, D.L.; Velcheti, V.; Haven, N. Artificial Intelligence in Digital Pathology—New Tools for Diagnosis and Precision Oncology. Nat. Rev. Clin. Oncol. 2019, 16, 703–715. [Google Scholar] [CrossRef] [PubMed]
- Polesie, S.; McKee, P.H.; Gardner, J.M.; Gillstedt, M.; Siarov, J.; Neittaanmäki, N.; Paoli, J. Attitudes Toward Artificial Intelligence Within Dermatopathology: An International Online Survey. Front. Med. 2020, 7, 591952. [Google Scholar] [CrossRef]
- Nelson, C.A.; Pérez-Chada, L.M.; Creadore, A.; Li, S.J.; Lo, K.; Manjaly, P.; Pournamdari, A.B.; Tkachenko, E.; Barbieri, J.S.; Ko, J.M.; et al. Patient Perspectives on the Use of Artificial Intelligence for Skin Cancer Screening: A Qualitative Study. JAMA Dermatol. 2020, 156, 501–512. [Google Scholar] [CrossRef]
- Khalid, M.; Niazi, K.; Parwani, A.V.; Gurcan, M. Digital Pathology and Artificial Intelligence. Lancet Oncol. 2021, 20, e253–e261. [Google Scholar] [CrossRef]
- Steele, L.; Velazquez-Pimentel, D.; Thomas, B.R. Do AI Models Recognise Rare, Aggressive Skin Cancers? An Assessment of a Direct-to-Consumer Application in the Diagnosis of Merkel Cell Carcinoma and Amelanotic Melanoma. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e877–e879. [Google Scholar] [CrossRef]
- Matrix AI Network. Built to Last: Data and Computing Power; Matrix AI Network: Hong Kong, China, 2019. [Google Scholar]
- Jaworek-Korjakowska, J.; Kłeczek, P. Automatic Classification of Specific Melanocytic Lesions Using Artificial Intelligence. BioMed Res. Int. 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- State Council of China. The Development Plan of the New Generation of Artificial Intelligence; State Council of China: Beijing, China, 2017. [Google Scholar]
- Liu, Y.; Jain, A.; Eng, C.; Way, D.H.; Lee, K.; Bui, P.; Kanada, K.; de Oliveira Marinho, G.; Gallegos, J.; Gabriele, S.; et al. A Deep Learning System for Differential Diagnosis of Skin Diseases. Nat. Med. 2020, 26, 900–908. [Google Scholar] [CrossRef] [PubMed]
- Tschandl, P.; Rinner, C.; Apalla, Z.; Argenziano, G.; Codella, N.; Halpern, A.; Janda, M.; Lallas, A.; Longo, C.; Malvehy, J.; et al. Human–Computer Collaboration for Skin Cancer Recognition. Nat. Med. 2020, 26, 1229–1234. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Yu, L.; Chen, H.; Fu, C.-W.; Xing, L.; Heng, P.-A. Transformation-Consistent Self-Ensembling Model for Semisupervised Medical Image Segmentation. IEEE Trans. Neural Netw. Learn. Syst. 2021, 32, 523–534. [Google Scholar] [CrossRef]
- Pachtrachai, K.; Vasconcelos, F.; Chadebecq, F.; Allan, M.; Hailes, S.; Pawar, V.; Stoyanov, D. Adjoint Transformation Algorithm for Hand-Eye Calibration with Applications in Robotic Assisted Surgery. Ann. Biomed. Eng. 2018, 46, 1606–1620. [Google Scholar] [CrossRef]
- Gao, Y.; Wang, S.; Li, J.; Li, A.; Liu, H.; Xing, Y. Modeling and Evaluation of Hand-Eye Coordination of Surgical Robotic System on Task Performance. Int. J. Med. Robot. 2017, 13, e1829. [Google Scholar] [CrossRef]
- Stefano, G.B.; Kream, R.M. The Micro-Hospital: 5G Telemedicine-Based Care. Med. Sci. Monit. Basic Res. 2018, 24, 103–104. [Google Scholar] [CrossRef]
- Spicher, N.; Schweins, M.; Thielecke, L.; Kurner, T.; Deserno, T.M. Feasibility Analysis of Fifth-Generation (5G) Mobile Networks for Transmission of Medical Imaging Data. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Mexico, 1–5 November 2021; pp. 1791–1795. [Google Scholar] [CrossRef]
- Yan, X.; Ren, X. 5G Edge Computing Enabled Directional Data Collection for Medical Community Electronic Health Records. J. Healthc. Eng. 2021, 2021, 5598077. [Google Scholar] [CrossRef]
- Psiha, M.M.; Vlamos, P. IoT Applications with 5G Connectivity in Medical Tourism Sector Management: Third-Party Service Scenarios. Adv. Exp. Med. Biol. 2017, 989, 141–154. [Google Scholar] [CrossRef]
- Jell, A.; Vogel, T.; Ostler, D.; Marahrens, N.; Wilhelm, D.; Samm, N.; Eichinger, J.; Weigel, W.; Feussner, H.; Friess, H.; et al. 5th-Generation Mobile Communication: Data Highway for Surgery 4.0. Surg. Technol. Int. 2019, 35, 36–42. [Google Scholar]
- Milletari, F.; Frei, J.; Aboulatta, M.; Vivar, G.; Ahmadi, S.-A. Cloud Deployment of High-Resolution Medical Image Analysis With TOMAAT. IEEE J. Biomed. Health Inform. 2019, 23, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Juyal, S.; Sharma, S.; Shukla, A.S. Smart Skin Health Monitoring Using AI-Enabled Cloud-Based IoT. Mater. Today Proc. 2021, 46, 10539–10545. [Google Scholar] [CrossRef]
- Juyal, S.; Sharma, S.; Harbola, A.; Shukla, A.S. Privacy and Security of IoT Based Skin Monitoring System Using Blockchain Approach. In Proceedings of the 2020 IEEE International Conference on Electronics, Computing and Communication Technologies (CONECCT), Bangalore, India, 2–4 July 2020; pp. 1–5. [Google Scholar]
- Bhadula, S.; Sharma, S. IoT-Based Skin Monitoring System. Int. J. Recent Technol. Eng. 2020, 8, 4258–4264. [Google Scholar] [CrossRef]
- Juyal, S.; Sharma, S.; Shukla, A.S. Security and Privacy Issues in Unified IoT-Based Skin Monitoring System. Mater. Today Proc. 2021, 46, 10815–10820. [Google Scholar] [CrossRef]
- Qian, H.; Dong, B.; Yuan, J.-J.; Yin, F.; Wang, Z.; Wang, H.-N.; Wang, H.-S.; Tian, D.; Li, W.-H.; Zhang, B.; et al. Pre-Consultation System Based on the Artificial Intelligence Has a Better Diagnostic Performance Than the Physicians in the Outpatient Department of Pediatrics. Front. Med. 2021, 8, 695185. [Google Scholar] [CrossRef]
- Mao, Y.; Zhang, L. Optimization of the Medical Service Consultation System Based on the Artificial Intelligence of the Internet of Things. IEEE Access 2021, 9, 98261–98274. [Google Scholar] [CrossRef]
- Manning, C.L. Artificial Intelligence Could Bring Relevant Guidelines into Every Consultation. BMJ 2019, 4788, 31196976. [Google Scholar] [CrossRef] [PubMed]
- Loftus, T.J.; Tighe, P.J.; Filiberto, A.C.; Efron, P.A.; Brakenridge, S.C.; Mohr, A.M.; Rashidi, P.; Upchurch, G.R.J.; Bihorac, A. Artificial Intelligence and Surgical Decision-Making. JAMA Surg. 2020, 155, 148–158. [Google Scholar] [CrossRef]
- Hinton, G.E.; Osindero, S.; Teh, Y.-W. A Fast Learning Algorithm for Deep Belief Nets. Neural Comput. 2006, 18, 1527–1554. [Google Scholar] [CrossRef]
- Talebi-Liasi, F.; Markowitz, O. Is Artificial Intelligence Going to Replace Dermatologists? Cutis 2019, 103, 25–27. [Google Scholar]
- Lucas, R.E. The Industrial Revolution: Past and Future. In Annual Report of the Federal Reserve Bank of Minneapolis; Federal Reserve Bank of Minneapolis: Minneapolis, MN, USA, 2004; Volume 18, pp. 5–20. [Google Scholar]
- Yampolskiy, R.V. Artificial Intelligence Safety and Security; CRC Press: Boca Raton, FL, USA, 2018; ISBN 1351251376. [Google Scholar]
- Lecun, Y.; Bengio, Y.; Hinton, G. Deep Learning. Nature 2015, 521, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Prasad, R.; Rohokale, V. Artificial Intelligence and Machine Learning in Cyber Security. In Cyber Security: The Lifeline of Information and Communication Technology; Springer: Berlin/Heidelberg, Germany, 2020; pp. 231–247. [Google Scholar]
- Rigby, M.J. Ethical Dimensions of Using Artificial Intelligence in Health Care. AMA J. Ethics 2019, 21, 121–124. [Google Scholar]
- Gomolin, A.; Netchiporouk, E.; Gniadecki, R.; Litvinov, I.V. Artificial Intelligence Applications in Dermatology: Where Do We Stand? Front. Med. 2020, 7, 100. [Google Scholar] [CrossRef]
- O’Sullivan, S.; Nevejans, N.; Allen, C.; Blyth, A.; Leonard, S.; Pagallo, U.; Holzinger, K.; Holzinger, A.; Sajid, M.I.; Ashrafian, H. Legal, Regulatory, and Ethical Frameworks for Development of Standards in Artificial Intelligence (AI) and Autonomous Robotic Surgery. Int. J. Med. Robot. Comput. Assist. Surg. 2019, 15, e1968. [Google Scholar] [CrossRef] [PubMed]
- Dave, P.; Nambudiri, V.; Grant-Kels, J.M. The Introduction of “Dr AI”: What Dermatologists Should Consider. J. Am. Acad. Dermatol. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Batbaatar, E.; Dorjdagva, J.; Luvsannyam, A.; Savino, M.M.; Amenta, P. Determinants of Patient Satisfaction: A Systematic Review. Perspect. Public Health 2017, 137, 89–101. [Google Scholar] [CrossRef]
- Khanna, S.; Sethi, Y.; Nambiar, A.R. ISkin Specialist—A Big Data Based Expert System for Dermatology. In Proceedings of the 2017 IEEE International Conference on Big Data (Big Data), Boston, MA, USA, 1–14 December 2017; pp. 4765–4767. [Google Scholar] [CrossRef]
- Muñoz-López, C.; Ramírez-Cornejo, C.; Marchetti, M.A.; Han, S.S.; Del Barrio-Díaz, P.; Jaque, A.; Uribe, P.; Majerson, D.; Curi, M.; Del Puerto, C.; et al. Performance of a Deep Neural Network in Teledermatology: A Single-Centre Prospective Diagnostic Study. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 546–553. [Google Scholar] [CrossRef]
- Coates, S.J.; Kvedar, J.; Granstein, R.D. Teledermatology: From Historical Perspective to Emerging Techniques of the Modern Era: Part I: History, Rationale, and Current Practice. J. Am. Acad. Dermatol. 2015, 72, 563–566. [Google Scholar] [CrossRef]
- Yu, K.-H.; Beam, A.L.; Kohane, I.S. Artificial Intelligence in Healthcare. Nat. Biomed. Eng. 2018, 2, 719–731. [Google Scholar] [CrossRef]
- Nagendran, M.; Chen, Y.; Lovejoy, C.A.; Gordon, A.C.; Komorowski, M.; Harvey, H.; Topol, E.J.; Ioannidis, J.P.A.; Collins, G.S.; Maruthappu, M. Artificial Intelligence versus Clinicians: Systematic Review of Design, Reporting Standards, and Claims of Deep Learning Studies. BMJ 2020, 368, m689. [Google Scholar] [CrossRef]
| Terminology | Paraphrase |
|---|---|
| Artificial Intelligence (AI) | The intelligence manifested by machines made by humans, i.e., the ability of the machine to simulate natural intelligence. |
| Knowledge Representation | It is the field of AI dedicated to representing information about the world in a form that a computer system can utilize to solve complex tasks such as diagnosing a medical condition or having a dialog in a natural language. |
| Representation Learning (Feature Learning) | A set of techniques that allows a system to automatically discover the representations needed for feature detection or classification from raw data. |
| Machine Learning | The study of computer algorithms that improve automatically through experience. The algorithms use computational methods to learn from data without being explicitly programmed. |
| Deep Learning | A branch of machine learning methods based on artificial neural networks with representation learning. |
| Supervised Learning | Refers to the machine learning task of learning a function that maps an input to an output based on example input–output pairs. It infers a function from labeled training data consisting of a set of training examples. |
| Transfer Learning | Transfer learning is a machine learning model that allows a model developed from one task to be transferred for another task after fine-tuning and augmentation. |
| Artificial Neural Networks (ANNs) | ANNs, usually simply called neural networks (NNs), are computing systems vaguely inspired by the biological neural networks that constitute animal brains. An ANN is based on a collection of connected units or nodes called artificial neurons, which loosely model the neurons in a biological brain |
| Convolutional Neural Networks (CNNs) | CNNs are a class of neural networks; they are feedforward neural networks. Their artificial neurons can respond to a part of the surrounding units in the coverage area, most commonly applied to analyzing visual imagery. |
| Generative Adversarial Networks (GANs) | GANs are a method of unsupervised learning that learn by playing two neural networks against each other. |
| Pattern Recognition | The automated recognition of patterns and regularities in data. The environment and objects are collectively referred to as patterns. |
| Image Set | An object stores information about an image data set or a collection of image data sets. It contains image descriptions, locations of images and the number of images in the collection. |
| Authors | Refer ence | Year | Country | AI Algorithm Model | The Purpose of AI Algorithm | Image (Datasets) Recourse | No. of Images in Datasets | Usage | Types of Images | Accuracy /Precision (%) | Sensitivity/Recall (%) | Specificity (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kassem et al. | [23] | 2020 | Egypt | Deep CNNs (modified GoogleNet) | Classification of multiple skin lesions | ISIC 2016–2019 | 25,331 | Multi-class (8) | Dermoscopy | 94.92 | 79.8 | 97 |
| Rezvantalab et al. | [52] | 2018 | Iran | Four deep learning convolutional neural networks (CNNs) | Investigating the ability of deep convolutional neural networks in classification of multiple skin lesion | HAM10000; PH2 | 10,135 | Multi-class (8) | Dermoscopy | 80.22–89.01 | 82.26–99.10 | 79.60–89.01 |
| Gessert et al. | [53] | 2018 | German y | Ensemble of CNN | Diagnosis of multiple skin lesions | ISIC-2018, HAM10000 | 23,515 | Multi-class (7) | Dermoscopy | 85.1 | 93.1–97.6 | N/A |
| Gessert et al. | [54] | 2020 | German y | Ensemble of multi-resolution CNN | Classification of multiple skin lesions | HAM10000, BCN20000, MSK,7- point, | 47,049 | Multi-class (8) | Dermoscopy | 80.5–96 | 72.5–74.2 | 94–99.9 |
| Haenssle et al. | [55] | 2018 | German y | Deep convolutional neural network (Google’s Inception v4 architecture) | Detection of melanoma and comparison of its performance with 58 dermatologists | ISIC archive, clinical images | >150,000 | Multi-class (20) | Macroscopy and Dermoscopy | 86 | 86.6–88.9 | 71.3–75.7 |
| Haenssle et al. | [56] | 2020 | Multi- country | FotoFinder® Moleanalyzer Pro | Classification of skin lesions and comparison of the performance of the AI model with 96 dermatologists | ISIC archive, clinical images | >150,000 | Multi-class (25) | Macroscopy and Dermoscopy | 84 | 95 | 76.7 |
| Esteva et al. | [66] | 2017 | USA | Deep convolutional neural networks (GoogleNet Inception v3) | Classification of skin cancer and comparison of the performance of AI model with 21 dermatologists | Online repositories and clinical data from | 129,450 | Multi-class (2032) | Macroscopy and Dermoscopy | 1: 72.1 ± 0.9; 2: 55.4 ± 1.7 | N/A | N/A |
| Mahbod et al. | [67] | 2020 | Austria | Multi-scale multi-convolutional neural networks (MSM-CNNs) | Investigating the effect of image size for skin lesion classification | ISIC-2016, 2017, 2018 HAM10000 | 12,927 | Multi-class (7) | Dermoscopy | 96.3 | N/A | N/A |
| Iqbal et al. | [71] | 2020 | China | Deep CNN | Classification of multiple skin lesion | ISIC-2017, 2018, 2019 | 25,331 | Multi-class (8) | Dermoscopy | 94 | 93 | 91 |
| Qin et al. | [73] | 2020 | China | Generative adversarial networks (GANs) | Classification of multiple skin lesion | ISIC-2018 | 10,015 | Multi-class (7) | Dermoscopy | 95.2 | 83.2 | 74.3 |
| Cano et al. | [74] | 2021 | Panama | NasNet | Classification of multiple skin lesions | ISIC-2019 | 25,331 | Multi-class (8) | Dermoscopy | 71–99 | 73–98 | 70–99 |
| Barhoumi et al. | [75] | 2021 | Tunisia | Transfer learning CNN model | Classification of multiple skin lesions | ISIC 2018 | 5057 | Multi-class (7) | Dermoscopy | 95 | 96 | N/A |
| Ratul et al. | [76] | 2020 | Canada | Dilated CNNs (VGG-16,-19, MobileNet, Inception-V3) | Classification of multiple skin lesions | HAM10000 | 10,015 | Multi-class (7) | Dermoscopy | 87–89 | 87–89 | N/A |
| Rashid et al. | [77] | 2020 | Pakistan | Semi-supervised GANs | Classification of multiple skin lesions | ISIC 2018 | 10,000 | Multi-class (7) | Dermoscopy | 73–94 | 69–92 | N/A |
| Maron et al. | [78] | 2019 | German y | CNNs | Classification of multiple skin lesions and comparison of the performance of the AI model with 112 dermatologists | ISIC 2018, HAM10000 | 11,444 | Multi-class (5) | Dermoscopy | N/A | 90.2–97.7 | 94.2–99.5 |
| Sun et al. | [79] | 2021 | China | CNNs | Classification of multiple skin lesions | ISIC-2019, MED- NODE, PH2, 7- point | 18,460 | Multi-class (7) | Dermoscopy | 66.2–89.5 | 66.2–89.5 | 95.2–99.3 |
| Jain et al. | [80] | 2021 | India | Six transfer learning nets | Classification of multiple skin lesions | HAM10000 | 10,015 | Multi-class (7) | Dermoscopy | 66–90 | 66–90 | N/A |
| Winkler et al. | [81] | 2020 | Gemany | FotoFinder® Moleanalyzer Pro (CNN) | Detection of various melanoma localizations and subtypes | ISIC archive, clinical images | >150,000 | Multi-class (6) | Macroscopy and Dermoscopy | 50.8–95.4 | 53.3–100 | 65–94 |
| Binder et al. | [82] | 1994 | Austria | Artificial neural networks (ANNs) | Classification of naevi and malignant melanoma and comparison of the performance of AI model with 3 dermatologists | Oil immersion images of pigmented skin lesions | 200 | Multi-class (3) | Microscopy | 86 | 95 | 88 |
| Sies et al. | [83] | 2020 | German y | FotoFinder® Moleanalyzer Pro/FotoFinder®Moleanalyzer- 3, Dynamole | Detection of various melanoma localizations and subtypes | ISIC dermoscopic archive, multicentric clinical images | >150,000 | Multi-class (20) | Dermoscopy | 92.8 | 77.6 | 95.3 |
| Yang et al. | [84] | 2020 | China | CNNs (DenseNet-96, ResNet-152, ResNet-99) | Classification of multiple benign hyperpigmented dermatitis and comparison of the performance of AI model with 11 dermatologists | Clinical images | 12,816 | Multi-class (6) | Macroscopy | 75.3–97.8 | 75.5–94.4 | 95.6–99.8 |
| Lyakhov et al. | [85] | 2022 | Russia | Multimodal neural network | Recognition of multiple pigmented skin lesions | ISIC-2016–2021 | 41,725 | Multi-class (10) | Dermoscopy | 83.6 | N/A | N/A |
| Guzman et al. | [86] | 2015 | Philippin es | Singe/multi-level and multi-models ANN | Detection of eczema skin lesion | Clinical images | 504 | Multi-class (3) | Macroscopy | Single: 78.17–87.30 Multi: 81.34–85.71 | N/A | N/A |
| Han et al. | [87] | 2018 | Korea | Region-based convolutional deep neural networks | Diagnosis of onychomycosis and comparison of the performance of AI model with 42 dermatologists | Clinical images | 49,567 | Multi-class (6) | Macroscopy | 82–98 | 82.7–96 | 69.3–96.7 |
| A.Blum et al. | [88] | 2004 | Gemany | Vision algebra algorithms | Diagnosis of melanocytic lesions and validation of its diagnostic accuracy | Clinical images | 837 | Multi-class (20) | Dermoscopy | 82.3–84.1 | 80–88.1 | 82.4–82.7 |
| Marchetti et al. | [89] | 2020 | USA | CNNs and deep learning algorithms | Classification of melanoma and comparison of the performance of AI model with 17 dermatologists | ISIC-2017 | 2750 | Multi-class (3) | Dermoscopy | 86.8 | 76 | 85 |
| Shen et al. | [90] | 2018 | China | Convolutional neural networks | Diagnosing for facial acne vulgaris | Clinical images | Binary: 6000 Multi:42,000 | Binary-class/Multi-class (7) | Macroscopy | 88.7–89.5 | 81.7–92 | 87–95.7 |
| Seité et al. | [91] | 2019 | France | Deep learning algorithm | Determination of the severity of facial acne and identification of subtypes of acne lesion | Clinical images | 4958 | Multi-class (3) | Macroscopy | N/A | N/A | N/A |
| Zhao et al. | [92] | 2019 | China | CNNs | Identification of psoriasis | XiangyaDerm-Pso9 | 8021 | Multi-class (9) | Macroscopy | 88 | 83–95 | 96–98 |
| Han et al. | [93] | 2020 | Korea | Deep Neural Networks | Predicting malignancy and suggesting treatment option, as well as multi-classification for 134 skin disorders | Clinical images | 220,680 | 1:Binary- class 2:Multi-class (134) | Macroscopy | 1: 56.7–92 2: 44.8–78.1 | N/A | N/A |
| Authors | Reference | Year | Country | AI Algorithm Model | The Purpose of AI Algorithm | Image (Datasets) Recourse | No. of Images in Datasets | Types of Images | Accuracy/ Precision (%) | Sensitivity/Recall (%) | Specificity (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Filho et al. | [51] | 2018 | Germany | Structural Co-occurrence matrix | Classification of melanoma | ISIC-2016, 2017, PH2 | 3100 | Dermoscopy | 89.93–99 | 89.9–99.2 | 95.15–99.4 |
| Marchetti et al. | [89] | 2018 | USA | Non-learned approaches and machine learning methods | Classification of melanoma and comparison of the performance of AI model with 8 dermatologists | ISIC-2016 | 1279 | Dermoscopy | 85–86 | 46–70 | 88–92 |
| Roffman et al. | [94] | 2018 | USA | Artificial neural network | Detection of non-melanoma skin cancer | NHIS 1997–2015 | 462,630 | Macroscopy | 81 | 86.2–88.5 | 62.2–62.7 |
| Alzubaidi | [95] | 2021 | Australia | Transfer learning model | Discrimination of skin cancer and normal skin | ISIC-2016–2020, Med- Node, Dermofit | >200,000 | Dermoscopy | 89.69–98.57 | 85.60–97.90 | N/A |
| Guimarães et al. | [96] | 2020 | Germany | Convolutional neural networks | Diagnosis of atopic dermatitis | Multiphoton tomography Images | 3663 | Multiphoton tomograph | 97.0 ± 0.2 | 96.6 ± 0.2 | 97.7 ± 0.3 |
| Ho. et al. | [97] | 2020 | USA | Deep neural network | Image segmentation of plexiform neurofibromas | MRI images | 35 | MRI | N/A | N/A | N/A |
| Fink et al. | [98] | 2018 | Germany | Edge-preserving thresholding automated shape recognition | Classification of psoriasis and measurement of lesion area andseverity index | Clinical images | 10 patients | Macroscopy | N/A | N/A | N/A |
| Fink et al. | [99] | 2019 | Germany | Edge-preserving thresholding automated shape recognition | Validation of the precision and reproducibility of algorithm in PASI measurements | Clinical images | 120 patients | Macroscopy | N/A | N/A | N/A |
| Schnuerle et al. | [100] | 2017 | Switzerland | Support vector machines | Detection of hand eczema | Clinical images | N/A | Macroscopy | 74.5–89.29 | 48–71.43 | 77.24–93.63 |
| Gao et al. | [101] | 2020 | Chinas | Deep learning network architecture (ResNet-50) | Detection for fungal skin lesion | Clinical images | 292 | Macroscopy | N/A | 95.2–99.5 | 91.4–100 |
| Bashat et al. | [102] | 2018 | Israel | N/A | Differentiation of benign and malignant neurofibroma | MRI images | 30 | MRI | 80 | 72 | 87 |
| Duarte et al. | [103] | 2014 | Portugal | Support vector machines | Classification of whole-brain grey and white matter of MRI between NF1 patients and normal person | T1-weighted MRI scans | 99 | MRI Images | 94 | 92 | 96 |
| Meienberger et al. | [104] | 2019 | Switzerland | Convolutional neural networks (Net 16) | Establishment of an accurate and objective psoriasis assessment method | Clinical images | 203 | Macroscopy | 92 | N/A | N/A |
| Gustafson et al. | [105] | 2017 | USA | Electronic health record based phenotype algorithm | Identification of atopic dermatitis and comparison of the performance of AI model with 4 dermatologists | Clinical images | 562 | N/A | N/A | 53.6–75 | N/A |
| Luo et al. | [106] | 2020 | China | Cycle-consistent adversarial networks | Classification of vitiligo skin lesion | Clinical Images | 80,000 | Macroscopy | 85.69 | 80.73 | 66.2 |
| Makena et al. | [107] | 2019 | USA | Convolutional neural networks | Segmentation of vitiligo skin lesion | RGB images of vitiligo lesions | 308 | Macroscopy (UV/natural light) | 74–88.7 | N/A | N/A |
| Authors | Reference | Year | Country | AI Algorithm Model | The Purpose of AI Algorithm | Image (Datasets) Recourse | No. of Images in Datasets | Types of Images | Accuracy/Precision (%) |
|---|---|---|---|---|---|---|---|---|---|
| Eisentha et al. | [64] | 2006 | Israel | Deep learning algorithm | Predicting facial attractiveness ratings | Volunteer images | 194 | Macroscopy | 0.65 correlation with human |
| Kagian et al. | [65] | 2008 | Israel | Linear regression algorithm | Extraction of facial features from raw images and rating facial attractiveness | Volunteer images | 91 | Macroscopy | 0.82 correlation with human |
| Zhang et al. | [108] | 2017 | China | Hypergraph-based semi-supervised learning method (HSSL) | Analysis of human face attractiveness | Shanghai Database and celebrity portrait from Internet | 2354 | Macroscopy | 81.47–84.21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z.; Koban, K.C.; Schenck, T.L.; Giunta, R.E.; Li, Q.; Sun, Y. Artificial Intelligence in Dermatology Image Analysis: Current Developments and Future Trends. J. Clin. Med. 2022, 11, 6826. https://doi.org/10.3390/jcm11226826
Li Z, Koban KC, Schenck TL, Giunta RE, Li Q, Sun Y. Artificial Intelligence in Dermatology Image Analysis: Current Developments and Future Trends. Journal of Clinical Medicine. 2022; 11(22):6826. https://doi.org/10.3390/jcm11226826
Chicago/Turabian StyleLi, Zhouxiao, Konstantin Christoph Koban, Thilo Ludwig Schenck, Riccardo Enzo Giunta, Qingfeng Li, and Yangbai Sun. 2022. "Artificial Intelligence in Dermatology Image Analysis: Current Developments and Future Trends" Journal of Clinical Medicine 11, no. 22: 6826. https://doi.org/10.3390/jcm11226826
APA StyleLi, Z., Koban, K. C., Schenck, T. L., Giunta, R. E., Li, Q., & Sun, Y. (2022). Artificial Intelligence in Dermatology Image Analysis: Current Developments and Future Trends. Journal of Clinical Medicine, 11(22), 6826. https://doi.org/10.3390/jcm11226826





