Glycated Haemoglobin A1c Variability Score Elicits Kidney Function Decline in Chinese People Living with Type 2 Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Study Population
2.2. Data Collection and Calculation
2.3. Outcomes
2.4. Statistical Methods
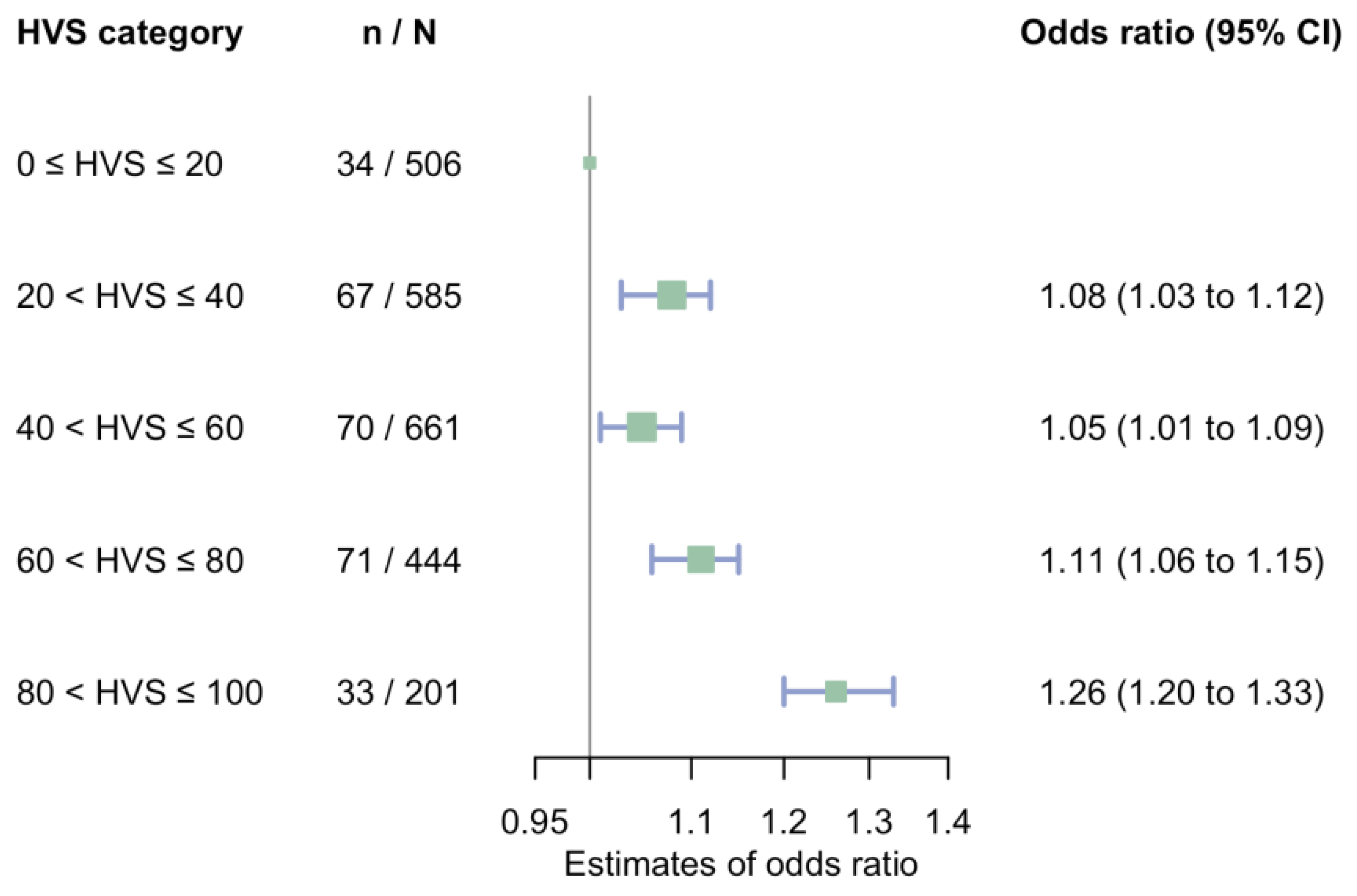
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Thomas, M.C.; Cooper, M.E.; Zimmet, P. Changing epidemiology of type 2 diabetes mellitus and associated chronic kidney disease. Nat. Rev. Nephrol. 2016, 12, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Fioretto, P.; Vettor, R.; Pontremoli, R. SGLT2 inhibitors to prevent diabetic kidney disease. Lancet Diabetes Endocrinol 2020, 8, 4–5. [Google Scholar] [CrossRef]
- Grams, M.E.; Sang, Y.; Ballew, S.H.; Matsushita, K.; Astor, B.C.; Carrero, J.J.; Chang, A.R.; Inker, L.A.; Kenealy, T.; Kovesdy, C.P.; et al. Evaluating Glomerular Filtration Rate Slope as a Surrogate End Point for ESKD in Clinical Trials: An Individual Participant Meta-Analysis of Observational Data. J. Am. Soc. Nephrol. 2019, 30, 1746–1755. [Google Scholar] [CrossRef] [PubMed]
- Inker, L.A.; Heerspink, H.J.L.; Tighsiouart, H.; Levey, A.S.; Coresh, J.; Gansevoort, R.T.; Simon, A.L.; Ying, J.; Beck, G.J.; Wanner, C.; et al. GFR Slope as a Surrogate End Point for Kidney Disease Progression in Clinical Trials: A Meta-Analysis of Treatment Effects of Randomized Controlled Trials. J. Am. Soc. Nephrol. 2019, 30, 1735–1745. [Google Scholar] [CrossRef]
- Neuen, B.L.; Weldegiorgis, M.; Herrington, W.G.; Ohkuma, T.; Smith, M.; Woodward, M. Changes in GFR and Albuminuria in Routine Clinical Practice and the Risk of Kidney Disease Progression. Am. J. Kidney Dis. 2021, 78, 350–360.e1. [Google Scholar] [CrossRef]
- Greene, T.; Ying, J.; Vonesh, E.F.; Tighiouart, H.; Levey, A.S.; Coresh, J.; Herrick, J.S.; Imai, E.; Jafar, T.H.; Maes, B.D.; et al. Performance of GFR Slope as a Surrogate End Point for Kidney Disease Progression in Clinical Trials: A Statistical Simulation. J. Am. Soc. Nephrol. 2019, 30, 1756–1769. [Google Scholar] [CrossRef]
- Levey, A.S.; Gansevoort, R.T.; Coresh, J.; Inker, L.A.; Heerspink, H.L.; Grams, M.E.; Greene, T.; Tighiouart, H.; Matsushita, K.; Ballew, S.H.; et al. Change in Albuminuria and GFR as End Points for Clinical Trials in Early Stages of CKD: A Scientific Workshop Sponsored by the National Kidney Foundation in Collaboration With the US Food and Drug Administration and European Medicines Agency. Am. J. Kidney Dis. 2020, 75, 84–104. [Google Scholar] [CrossRef]
- Faulk, D. VA/DoD Clinical Practice Guideline for the Management of Type 2 Diabetes Mellitus In Primary Care 2017. Available online: https://www.healthquality.va.gov/guidelines/CD/diabetes/VADoDDMCPGFinal508.pdf (accessed on 6 September 2022).
- Qu, F.; Shi, Q.; Wang, Y.; Shen, Y.; Zhou, K.; Pearson, E.R.; Li, S. Visit-to-visit glycated hemoglobin A1c variability in adults with type 2 diabetes: A systematic review and meta-analysis. Chin. Med. J. 2022; publish ahead of print. [Google Scholar] [CrossRef]
- Gorst, C.; Kwok, C.S.; Aslam, S.; Buchan, I.; Kontopantelis, E.; Myint, P.K.; Heatlie, G.; Loke, Y.; Rutter, M.K.; Mamas, M.A. Long-term Glycemic Variability and Risk of Adverse Outcomes: A Systematic Review and Meta-analysis. Diabetes Care 2015, 38, 2354–2369. [Google Scholar] [CrossRef]
- Li, S.; Nemeth, I.; Donnelly, L.; Hapca, S.; Zhou, K.; Pearson, E.R. Visit-to-Visit HbA1c Variability Is Associated With Cardiovascular Disease and Microvascular Complications in Patients with Newly Diagnosed Type 2 Diabetes. Diabetes Care 2020, 43, 426–432. [Google Scholar] [CrossRef]
- Forbes, A.; Murrells, T.; Mulnier, H.; Sinclair, A.J. Mean HbA1c, HbA1c variability, and mortality in people with diabetes aged 70 years and older: A retrospective cohort study. Lancet Diabetes Endocrinol. 2018, 6, 476–486. [Google Scholar] [CrossRef]
- Zhou, Y.-L.; Zhang, Y.-G.; Zhang, R.; Zhou, Y.-L.; Li, N.; Wang, M.-Y.; Tian, H.-M.; Li, S.-Y. Population diversity of cardiovascular outcome trials and real-world patients with diabetes in a Chinese tertiary hospital. Chin. Med. J. 2021, 134, 1317–1323. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Golin, C.E.; DiMatteo, M.R.; Gelberg, L. The Role of Patient Participation in the Doctor Visit: Implications for adherence to diabetes care. Diabetes Care 1996, 19, 1153–1164. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zuo, H.; Chen, X.; Hou, L.; Ma, J. Analysis of factors influencing the frequency of primary care visits among diabetic patients in two provinces in China. BMC Public Health 2019, 19, 1267. [Google Scholar] [CrossRef]
- Ahmed, S.T.; Mahtta, D.; Rehman, H.; Akeroyd, J.; Al Rifai, M.; Rodriguez, F.; Jneid, H.; Nasir, K.; Samad, Z.; Alam, M.; et al. Association between frequency of primary care provider visits and evidence-based statin prescribing and statin adherence: Findings from the Veterans Affairs system. Am. Heart J. 2020, 221, 9–18. [Google Scholar] [CrossRef]
- Levin, A.; Stevens, P.E.; Bilous, R.W.; Coresh, J.; De Francisco, A.L.M.; De Jong, P.E.; Griffith, K.E.; Hemmelgarn, B.R.; Iseki, K.; Lamb, E.J.; et al. Chapter 2: Definition, identification, and prediction of CKD progression. Kidney Int. Suppl. 2013, 3, 63–72. [Google Scholar] [CrossRef]
- Vegetabile, B.G.; Griffin, B.A.; Coffman, D.L.; Cefalu, M.; Robbins, M.W.; McCaffrey, D.F. Nonparametric estimation of population average dose-response curves using entropy balancing weights for continuous exposures. Health Serv. Outcomes Res. Methodol. 2021, 21, 69–110. [Google Scholar] [CrossRef]
- Nissenson, A.R.; Chertow, G.M.; Conway, P.T. Breaking the Barriers to Innovation in Kidney Care: The Time is Now. Clin. J. Am. Soc. Nephrol. CJASN 2022, 17, 591–593. [Google Scholar] [CrossRef]
- Luk, A.O.Y.; Ma, R.C.W.; Lau, E.S.H.; Yang, X.; Lau, W.W.Y.; Yu, L.W.L.; Chow, F.C.C.; Chan, J.C.N.; So, W.-Y. Risk association of HbA 1c variability with chronic kidney disease and cardiovascular disease in type 2 diabetes: Prospective analysis of the Hong Kong Diabetes Registry: HbA1c Variability and Diabetes Complications. Diabetes Metab. Res. Rev. 2013, 29, 384–390. [Google Scholar] [CrossRef]
- Yang, Y.-F.; Li, T.-C.; Li, C.-I.; Liu, C.-S.; Lin, W.-Y.; Yang, S.-Y.; Chiang, J.-H.; Huang, C.-C.; Sung, F.-C.; Lin, C.-C. Visit-to-Visit Glucose Variability Predicts the Development of End-Stage Renal Disease in Type 2 Diabetes: 10-Year Follow-Up of Taiwan Diabetes Study. Medicine 2015, 94, e1804. [Google Scholar] [CrossRef]
- Cardoso, C.R.L.; Leite, N.C.; Moram, C.B.M.; Salles, G.F. Long-term visit-to-visit glycemic variability as predictor of micro- and macrovascular complications in patients with type 2 diabetes: The Rio de Janeiro Type 2 Diabetes Cohort Study. Cardiovasc Diabetol 2018, 17, 33. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.-Y.; Huang, J.-C.; Chen, S.-C.; Chiou, H.-Y.; Wu, P.-Y. Association of HbA1C Variability and Renal Progression in Patients with Type 2 Diabetes with Chronic Kidney Disease Stages 3–4. Int. J. Mol. Sci. 2018, 19, 4116. [Google Scholar] [CrossRef] [PubMed]
- Takenouchi, A.; Tsuboi, A.; Terazawa-Watanabe, M.; Kurata, M.; Fukuo, K.; Kazumi, T. Direct association of visit-to-visit HbA1c variation with annual decline in estimated glomerular filtration rate in patients with type 2 diabetes. J. Diabetes Metab. Disord. 2015, 14, 69. [Google Scholar] [CrossRef][Green Version]
- Lee, C.-L.; Chen, C.-H.; Wu, M.-J.; Tsai, S.-F. The variability of glycated hemoglobin is associated with renal function decline in patients with type 2 diabetes. Ther. Adv. Chronic. Dis. 2020, 11, 2040622319898370. [Google Scholar] [CrossRef] [PubMed]
- Fenton, J.J.; Korff, M.V.; Lin, E.H.B.; Ciechanowski, P.; Young, B.A. Quality of Preventive Care for Diabetes: Effects of Visit Frequency and Competing Demands. Ann. Fam. Med. 2006, 4, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Ceriello, A.; Rossi, M.C.; De Cosmo, S.; Lucisano, G.; Pontremoli, R.; Fioretto, P.; Giorda, C.; Pacilli, A.; Viazzi, F.; Russo, G.; et al. Overall Quality of Care Predicts the Variability of Key Risk Factors for Complications in Type 2 Diabetes: An Observational, Longitudinal Retrospective Study. Diabetes Care 2019, 42, 514–519. [Google Scholar] [CrossRef]
- Li, S.; Vandvik, P.O.; Lytvyn, L.; Guyatt, G.H.; Palmer, S.C.; Rodriguez-Gutierrez, R.; Foroutan, F.; Agoritsas, T.; Siemieniuk, R.A.C.; Walsh, M.; et al. SGLT-2 inhibitors or GLP-1 receptor agonists for adults with type 2 diabetes: A clinical practice guideline. BMJ 2021, 373, n1091. [Google Scholar] [CrossRef]
- Monnier, L.; Mas, E.; Ginet, C.; Michel, F.; Villon, L.; Cristol, J.-P.; Colette, C. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 2006, 295, 1681–1687. [Google Scholar] [CrossRef]
- Ceriello, A.; Monnier, L.; Owens, D. Glycaemic variability in diabetes: Clinical and therapeutic implications. Lancet Diabetes Endocrinol. 2019, 7, 221–230. [Google Scholar] [CrossRef]
- Salvatore, T.; Pafundi, P.C.; Galiero, R.; Rinaldi, L.; Caturano, A.; Vetrano, E.; Aprea, C.; Albanese, G.; Di Martino, A.; Ricozzi, C.; et al. Can Metformin Exert as an Active Drug on Endothelial Dysfunction in Diabetic Subjects? Biomedicines 2020, 9, 3. [Google Scholar] [CrossRef]
- Reddy, M.A.; Zhang, E.; Natarajan, R. Epigenetic mechanisms in diabetic complications and metabolic memory. Diabetologia 2015, 58, 443–455. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Overall n = 2397 | HVS Category | ||||
|---|---|---|---|---|---|---|
| 0 to 20 n = 506 | 20 to 40 n = 585 | 40 to 60 n = 661 | 60 to 80 n = 444 | 80 to 100 n = 201 | ||
| Age, years | 58.5 [48.9, 67.1] | 60.3 [52.3, 68.9] | 61.2 [51.2, 68.9] | 57.5 [47.7, 67.0] | 54.9 [45.8, 64.4] | 53.4 [43.8, 62.4] |
| Sex, female, n (%) | 979 (40.8) | 237 (46.8) | 238 (40.7) | 254 (38.4) | 176 (39.6) | 74 (36.8) |
| Follow up, years | 4.7 [3.1, 6.3] | 4.9 [3.0, 6.6] | 4.9 [3.4, 6.7] | 4.8 [3.3, 6.2] | 4.4 [2.9, 5.8] | 4.4 [3.1, 6.0] |
| Average number of outpatient visits per year, n/year | 1.9 [1.3, 2.7] | 1.9 [1.3, 2.7] | 2.0 [1.4, 2.9] | 1.9 [1.3, 2.7] | 1.8 [1.3, 2.7] | 1.6 [1.2, 2.3] |
| HbA1c, % | 7.2 [6.7, 8.3] | 6.8 [6.6, 7.1] | 7.0 [6.6, 7.9] | 7.3 [6.7, 8.7] | 7.8 [6.9, 9.1] | 8.4 [7.2, 10.3] |
| HbA1c, mmol/mol | 55 [50, 67] | 51 [49, 54] | 53 [49, 63] | 56 [50, 72] | 62 [52, 76] | 68 [55, 89] |
| Time-weighted average HbA1c, % | 7.3 [6.8, 8.0] | 6.8 [6.6, 7.1] | 7.1 [6.8, 7.5] | 7.4 [7.0, 8.1] | 7.8 [7.3, 8.7] | 8.6 [7.7, 9.5] |
| Time-weighted average HbA1c, mmol/mol | 56 [51, 64] | 51 [49, 54] | 54 [51, 58] | 57 [53, 65] | 62 [56, 72] | 70 [61, 80] |
| eGFR, mL/min/1.73 m2 | 90.4 [74.3, 102.1] | 87.8 [73.4, 98.5] | 87.8 [72.5, 100.1] | 91.4 [75.8, 103.4] | 93.8 [77.3, 104.9] | 95.5 [78.6, 106.2] |
| eGFR ≥ 60 mL/min/1.73 m2, n (%) | 2 124 (88.6) | 445 (87.9) | 507 (86.7) | 588 (89.0) | 398 (89.6) | 186 (92.5) |
| LDL-c, mmol/L | 2.65 [2.03, 3.24] | 2.72 [2.09, 3.26] | 2.66 [1.92, 3.21] | 2.59 [2.06, 3.17] | 2.61 [2.01, 3.31] | 2.69 [2.02, 3.29] |
| Hypertension, n (%) | 1 661 (69.3) | 347 (68.6) | 444 (75.9) | 457 (69.1) | 292 (65.8) | 121 (60.2) |
| ASCVD, n (%) | 954 (39.8) | 220 (43.5) | 271 (46.3) | 251 (38.0) | 154 (34.7) | 58 (28.9) |
| Use of insulin, n (%) | 965 (40.3) | 104 (20.6) | 207 (35.4) | 305 (46.1) | 238 (53.6) | 111 (55.2) |
| Use of statins, n (%) | 1 624 (67.8) | 327 (64.6) | 408 (69.7) | 441 (66.7) | 308 (69.4) | 140 (69.7) |
| Use of ARB/ACEI, n (%) | 1 039 (43.3) | 213 (42.1) | 274 (46.8) | 295 (44.6) | 171 (38.5) | 86 (42.8) |
| Use of CCB, n (%) | 816 (34.0) | 173 (34.2) | 213 (36.4) | 236 (35.7) | 136 (30.6) | 58 (28.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, Y.; Huang, H.; Yan, X.; Hapca, S.; Bell, S.; Qu, F.; Liu, L.; Chen, X.; Zhang, S.; Shi, Q.; et al. Glycated Haemoglobin A1c Variability Score Elicits Kidney Function Decline in Chinese People Living with Type 2 Diabetes. J. Clin. Med. 2022, 11, 6692. https://doi.org/10.3390/jcm11226692
Zhou Y, Huang H, Yan X, Hapca S, Bell S, Qu F, Liu L, Chen X, Zhang S, Shi Q, et al. Glycated Haemoglobin A1c Variability Score Elicits Kidney Function Decline in Chinese People Living with Type 2 Diabetes. Journal of Clinical Medicine. 2022; 11(22):6692. https://doi.org/10.3390/jcm11226692
Chicago/Turabian StyleZhou, Yiling, Hongmei Huang, Xueqin Yan, Simona Hapca, Samira Bell, Furong Qu, Li Liu, Xiangyang Chen, Shengzhao Zhang, Qingyang Shi, and et al. 2022. "Glycated Haemoglobin A1c Variability Score Elicits Kidney Function Decline in Chinese People Living with Type 2 Diabetes" Journal of Clinical Medicine 11, no. 22: 6692. https://doi.org/10.3390/jcm11226692
APA StyleZhou, Y., Huang, H., Yan, X., Hapca, S., Bell, S., Qu, F., Liu, L., Chen, X., Zhang, S., Shi, Q., Zeng, X., Wang, M., Li, N., Du, H., Meng, W., Su, B., Tian, H., Li, S., & on behalf of the WECODe Study Group. (2022). Glycated Haemoglobin A1c Variability Score Elicits Kidney Function Decline in Chinese People Living with Type 2 Diabetes. Journal of Clinical Medicine, 11(22), 6692. https://doi.org/10.3390/jcm11226692







