Abstract
Objective: Venous thromboembolism (VTE) is a life threating complication in intensive care units (ICUs). This study aimed to pool the prevalence of VTE and examined the risk factors of VTE in intensive care patients worldwide. Methods: A systematic search in PubMed, EMBASE and Web of Science databases was performed. Studies reported that the data on the prevalence of VTE or relevant information were synthesized using a random-effects model. Results: A total of 42 studies reporting on 27,344 patients were included. The pooled prevalence of VTE was 10.0% (95% CI: 7.0–14.0%). Subgroup and metaregression analyses found that thromboprophylaxis strategy, simplified acute physiology score (SAPS II), age, study quality, sample size, malignancy, sex, spinal cord injury and injury severity score (ISS) moderated the prevalence of VTE in intensive care patients. Conclusions: The present meta-analysis revealed a high prevalence of VTE in critically ill patients. The risk factors of VTE included thromboprophylaxis strategy, SAPS II, age, malignancy, sex, spinal cord injury and ISS. Therefore, we need to pay more attention to high-risk populations of VTE in intensive care patients.
1. Introduction
Venous thromboembolism (VTE) driven by dysregulated coagulation, including deep-vein thrombosis (DVT) of the leg or pelvis and pulmonary embolism (PE), is a life-threating complication leading to morbidity and mortality all over the world, especially in critically ill patients. Similarly, it has also remained one of the most common unsuspected diagnoses found at autopsy in intensive care unit patients [1,2,3].
Afflicting approximately 10 million persons worldwide in all countries every year, VTE was a substantial contributor to the global burden of disease [4]. The prevalence of VTE in ICU patients ranged from 0.4% to 82.3% worldwide, which was the highest in Canada (400 in 100,000 persons) and the lowest in Thailand (82,300 in 100,000 persons) [5,6]. Baylis et al. indicated that VTE increased steadily over the last two decades [7]. In addition, Nobre et al. showed that 30% of patients had a recurrence of VTE in the last 10 years [8].
Previous studies have demonstrated that many factors could increase the risk of VTE in critically ill patients. Gregson et al. showed that older age, smoking and adiposity were consistently associated with higher VTE risk [9], and Krenitsky et al. suggested that factors with the highest VTE risk included transfusion and infection [10]. Furthermore, data showed that other factors, including trauma, major surgeries, malignancy, the inability of free movement, abnormal coagulation and indwelling venous catheters, were related with the increasing risk of VTE [11,12,13,14,15]. VTE is a fatal complication that, once occurred, can finally lead to a rise in mortality and disability, increase substantial healthcare costs and even sudden death [16,17]. Lutsey et al. showed that 3.5% (5943 in 170,021) developed pulmonary hypertension (PH) in the 2 years after their first VTE incident [18]. Makedonov et al. indicated that 20 to 50% of patients developed post-thrombotic syndrome (PTS) after a proximal VTE, and patients with critical PTS can have a quality of life similar to those with malignancy, angina, and congestive heart failure [19].
VTE has been documented among critically ill patients in various studies; however, it was likely due to the disparities in screening methods, among other study-specific features, which left VTE’s accurate prevalence unknown. Therefore, this study aimed to pool the prevalence of VTE and examine the risk factors of VTE in ICU patients.
2. Methods
2.1. Literature Search
This meta-analysis was conducted by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20]. Two investigators (XYG and LNZ) independently and systematically searched the databases, including PubMed, EMBASE and Web of Science, from their inception to 26 September 2022, using the following search terms: “venous thrombosis” OR “venous thromboembolic” OR “venous thromboembolism” OR VTE OR “deep venous thrombosis” OR DVT OR “lung embolism” OR “pulmonary embolism” OR PE AND “critical care” OR “critically ill” OR “intensive care” OR ICU AND “rate OR prevalence OR percentage”. We registered our protocol on PROSPERO accessed on 16 February 2022. (https://www.crd.york.ac.uk/PROSPERO/#index.php).
2.2. Study Selection and Data Extraction
Original studies were included if they met the following criteria: (1) observational studies including cross-sectional, case-control or cohort studies (only the baseline data were extracted for analyses in the last) conducted among ICU patents; (2) reported the data on prevalence of venous thromboembolism or relevant information that could generate the prevalence of venous thromboembolism in ICU departments; (3) being published in English; (4) studies in a special period (Corona Virus Disease 2019 and Severe Acute Respiratory Syndrome) or on special populations (the infants and adolescents) were excluded. The study selection and data extraction were performed by the same two investigators (XYG and LNZ) independently. Any disagreements were consulted by a third author (TMP). The first step was to screen the titles and abstracts independently to identify the relevant articles. Then, the full texts were reviewed for eligibility. If more than one study was published on the same data set, the one with more information or the larger sample size was included for analysis. A standardized Excel sheet was used to extract the following demographic and clinical characteristics: the first author, year of publication, country, year of survey, sampling method, department, sample size, age, male, body mass index (BMI), obesity, malignancy, abnormal coagulation, lower extremity fracture, pelvic fracture, spinal cord injury, thromboprophylaxis strategy, operations, central venous catheter (CVC), intensive care unit (ICU) length of stay (LOS), acute physiology and chronic health evaluation (APACHE II score), injury severity score (ISS), simplified acute physiology score (SAPS II) and quality score.
2.3. Quality Evaluation
The study quality was assessed by two independent investigators (XYG and LNZ) using the instrument for evaluating the methodological quality of epidemiological studies [21] with the following items: sampling methods; response rate; the definition and representative of targeted population; definition of VTE and validation of assessment instrument.
2.4. Statistical Analyses
The Comprehensive Meta-Analysis statistical software version 2.0 was used for the statistical analyses. The random-effect model was used to pool the prevalence of VTE [22]. Heterogeneity across studies was measured with I2 statistic (a significant heterogeneity was considered when I2 > 50%) [23]. Subgroup analyses and metaregression were conducted to explore the possible sources of heterogeneity. The following categorical variables were analyzed in subgroup analyses, in which the numeric categorical variables were categorized by the median splitting method: (1) year of survey: before 2013 vs. after 2013; (2) geographic region: Asia vs. European vs. North America vs. Oceania; (3) percentage of obesity: >26.8 vs. ≤26.8; (4) percentage of abnormal coagulation: >39.18 vs. ≤39.18; (5) percentage of lower extremity fracture: >23.04 vs. ≤23.04; (6) percentage of pelvic fracture: >20.10 vs. ≤20.10; (7) percentage of operations: >28.74 vs. ≤28.74; (8) percentage of CVC: >54.29 vs. ≤54.29; (9) ICU LOS: <8 vs. ≥8; (10) type of thromboprophylaxis strategy: pharmacological prophylaxis vs. mechanical prophylaxis vs. both; (11) SAPS II: >40.4 vs. ≤40.4. Continuous variables, including age, study quality, sample size, malignancy, male, spinal cord injury and ISS, were analyzed by meta regression analysis. Funnel plot and Egger’s regression model [24] was used to assess publication bias. Sensitivity analyses were performed by excluding one study in each turn to test the robustness of the overall pooled estimates. Statistical significance was defined as p < 0.05 (two-tailed).
3. Results
3.1. Characteristics of Included Studies and Quality Assessment
The details of the literature search and study selection is shown in Figure 1. Initially, 6726 papers were identified. After reviewing titles and abstracts, the full texts of 297 papers were read for eligibility. Finally, 42 studies covering 27,344 individuals were included in the meta-analysis (Table 1). Among these, 22 studies enrolled 8837 patients conducted in ICUs and 20 studies enrolled 18,507 patients conducted in specialist ICUs (including two in CICUs, seven in SICUs, two in TICUs, two in NICUs, five in MICUs, one in EICUs and one in LICUs). The percentage of males ranged from 25.45% to 100% and the mean age ranged from 31 to 64 years.
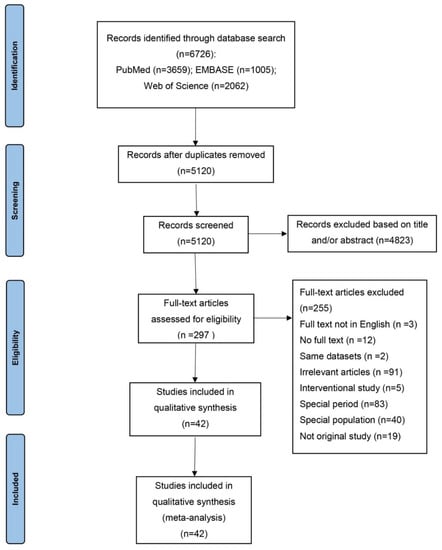
Figure 1.
Flowchart of study selection.

Table 1.
Characteristics of studies included in this meta-analysis.
The quality assessment revealed that the mean score was 4.70 (ranging from 3 to 6). The targeted population was defined clearly in all articles, and the definition of VTE in 8 studies was not defined, while 24 studies did not provide sampling methods and 19 studies had no response rate or the response rate was lower than 70%. The study population in all studies was representative.
3.2. Prevalence of VTE in ICU Patients
The pooled prevalence of VTE in ICU patients from 42 studies while using the random-effect model was 10.0% (95% CI: 7.0–14.0%, I2 was 97.84%; Figure 2).
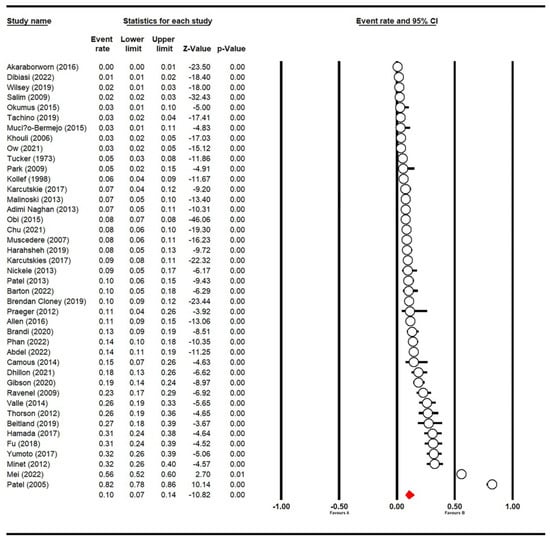
Figure 2.
Forest plot of prevalence of VTE in ICU patients (n = 42) [5,6,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64]. The red symbol indicated the prevalence of VTE in ICU patients.
3.3. Subgroup Analyses and Meta-Regression
Results of subgroup analyses are shown in Table 2. Thromboprophylaxis strategy and SAPS II were significantly associated with the prevalence of VTE. The prevalence of VTE was highest in mechanical prophylaxis (31.9%, 95% CI: 25.8–38.6%) followed by used simultaneously (13.4%, 95% CI: 7.6–22.7%) and pharmacological prophylaxis (9.3%, 95% CI: 6.0–14.1%), while the VTE prevalence in ICU patients with mean SAPS II ≤ 40.4 (29.6%, 95% CI: 24.0–36.0%) was higher than that in those with SAPS II > 40.4 (13.0%, 95% CI: 8.8–18.8%). Year of survey, country, obesity, abnormal coagulation, lower extremity fracture, pelvic fracture, operations, CVC and ICU LOS were not associated with the prevalence of VTE (all p values > 0.05).

Table 2.
Subgroup analyses of prevalence of VTE in ICU patients.
Meta regression analyses revealed that age (B = 0.04455, z = 11.99, p < 0.001), study quality (B = −0.09251, z = −3.36, p < 0.001), sample size (B = −0.00030, z = −22.41, p < 0.001), malignancy (B = −0.01705, z = −8.23, p < 0.001), sex (B = −0.00984, z = −4.08, p < 0.001), spinal cord injury (B = 0.07058, z = 7.45, p < 0.001) and ISS (B = 0.16487, z = 12.99, p < 0.001) were identified as significant moderators which contributed to heterogeneity cross-studies (Supplementary Materials Table S1).
3.4. Publication Bias and Sensitivity Analysis
Egger’s test (t = 0.60, 95% CI: −6.55–3.56%, p = 0.55) and funnel plot (Figure 3) did not detect publication bias. Sensitivity analyses showed no outlying study could change the robustness of results (Supplementary Materials Figure S1).
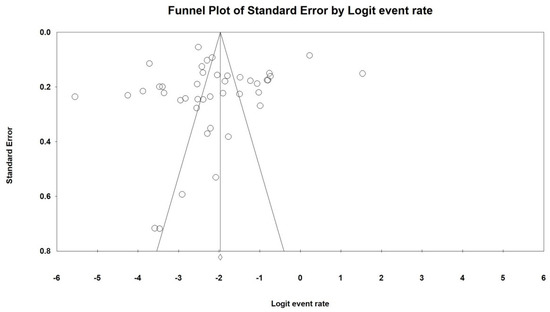
Figure 3.
Funnel plot of publication bias on prevalence of VTE in ICU patients.
4. Discussion
VTE has been documented among ICU patients in various studies. However, the reported prevalence of VTE in ICUs varied wildly, and the accurate prevalence of VTE remained unknown. In this meta-analysis, the overall prevalence of VTE among 27,344 individuals in ICUs was 10.0% (95% CI: 7.0–14.0%), ranging from 0.4% to 82.3%. This result showed a high rate of VTE in critically ill patients, which increases the mortality. The prevalence of VTE among ICU patients varied substantially, with the highest rate of 82.3% in SICUs [38]. It indicated that patients with surgical disease were more likely to develop thrombosis. Apart from the impact of different departments, discrepancy in diagnosis methods and socio-demographic characteristics could partly account for the differences between studies.
In this meta-analysis, the prevalence of VTE was moderated by different thromboprophylaxis strategy and SAPS II. Thromboprophylaxis strategies to prevent VTE were common in clinical work. However, the best strategy to prevent VTE remained controversial. In this study, pharmacological prophylaxis was associated with lower prevalence of VTE, which might show that pharmacological prophylaxis was more effective than mechanical prophylaxis or use in both to prevent VTE. The results were similar to the existing research, which indicated that anticoagulants can effectively prevent blood hypercoagulability via the inhibition of thrombin and coagulation factors, and consequently prevent VTE [65]. As also found in previous studies, the SAPS II was associated with disease severity, and the higher the SAPS II score, the more serious the disease [66]. However, in our study, the SAPS II ≤ 40.4 was associated with higher prevalence of VTE. This was partly because few studies were included in these subgroup analyses, and this finding needs to be re-examined in future studies.
Meta-regression analyses found that studies with a larger sample size (B = −0.00030, z = −22.41) were associated with a lower prevalence of VTE in this study. There was no explanation for this result except that the findings of the studies with a larger sample size might be more stable. In this study, malignancy (B = −0.01705, z = −8.23) was associated with a lower prevalence of VTE. This finding seemed unexpected, since malignancy was reported as a risk factor of VTE. However, it might be attributed to patients with malignancy often receiving more attention from medical staff, and they may also have received more preventive treatments [67]. In addition, studies with a higher percentage of males (B = −0.00984, z = −4.08) had a lower prevalence of VTE. Unlike males, this was probably because females often experienced pregnancy and puerperium, oral contraception and hormone therapy [15], which put female blood into a hypercoagulable state, thereby becoming more prone to develop VTE when ill.
This study found that older age (B = 0.04455, z = 11.99) was associated with a higher prevalence of VTE. It indicated that patients with older age were more likely to develop chronic disease and disability, which leads to hypercoagulability and limited bodily movement [68,69,70,71] when suffering from diseases such as trauma, major surgeries and malignancy, and which increased the prevalence of VTE. Thus, we should pay more attention to this special group. The prevalence of VTE was higher in patients with spinal cord injuries (B = 0.07058, z = 7.45). Stasis and hypercoagulability were two major risk factors for spinal-cord-injured patients [72]. In addition, spinal-cord-injured patients often needed a prolonged bed stay to reach neurological and functional recovery. All these factors might eventually lead to them developing thrombosis [73]. This study also showed that high ISS (B = 0.16487, z = 12.99) was associated with a higher prevalence of VTE, owing to the fact that a higher ISS often indicated more severe injury, which might increase the prevalence of VTE [74].
VTE was a fatal complication of patients with trauma, major surgeries, malignancy, the inability to free movement, and the like. Once VTE happened, it would increase the mortality and disability, increase substantial healthcare costs and even sudden death. Therefore, it was vitally importance to prevent and treat VTE in clinical work. Helms et al. [75] indicated that mechanical and pharmacological prophylaxis was suggested for critically ill patients. Current mechanical strategies include graduated compression stockings (GCS) and active devices such as intermittent pneumatic compression (IPC) [76,77,78]. With regard to the type of pharmacological thromboprophylaxis, low-molecular-weight heparin (LMWH) might have superior efficacy compared to unfractionated heparin (UFH) [79]. However, a high bleeding risk was considered a contraindication to anticoagulation. It was necessary to developed safety thromboprophylaxis strategies to prevent VTE.
There were several limitations to this meta-analysis. First, some of the sample sizes of the included studies were generally small, and most of the studies were retrospective studies. Second, the thromboprophylaxis strategy of VTE was different across the studies, which might influence the pooled prevalence of VTE. However, subgroup analyses could solve this confounding effect. Finally, heterogeneity in subgroup analyses remained, as it was unavoidable in meta-analysis of epidemiological surveys [80,81].
In conclusion, the prevalence of VTE was particularly high, especially in surgical disease patients. VTE was common in intensive care units worldwide and moderated by certain demographics and clinical factors, including age, sex, thromboprophylaxis strategy, SAPS II, malignancy, spinal cord injury and ISS. Considering the negative impacts of VTE on diagnosis, treatment, mortality and prognosis, we need to pay more attention to the high-risk populations of VTE. Methods to prevent VTE are now pharmacological and/or mechanical, such as GCS, IPC and LMWH, and they require the right time, dosage and duration, while also needing to be accompanied by good clinical care. However, more effective, detailed and individualized measures, such as an early assessment scale and specialized rehabilitation, should be taken to reduce VTE in intensive care units.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11226691/s1, Figure S1: Sensitive analysis on prevalence of VTE in intensive care patients; Table S1: Meta regression analyses of prevalence of VTE in intensive care patients.
Author Contributions
Study design: X.G., L.Z., L.C. and T.P. Data collection, analysis and interpretation: X.G., L.Z., T.P., H.W., S.Z. and J.T. Drafting of the manuscript: X.G., L.Z. and L.C. Critical revision of the manuscript: T.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Science and Technology foundation of Sichuan (2021YJ0430); Luzhou Municipal People’s Government–Southwest Medical University Joint Project (2020LZXNYDJ33).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors have no conflict of interest concerning this article.
References
- Tritschler, T.; Salvatore, S.P.; Kahn, S.R.; Garcia, D.; Delluc, A.; Kraaijpoel, N.; Langlois, N.; Girard, P.; Le Gal, G. ISTH definition of pulmonary embolism-related death and classification of the cause of death in venous thromboembolism studies: Validation in an autopsy cohort. J. Thromb. Haemost. JTH 2021, 19, 2514–2521. [Google Scholar] [CrossRef]
- Wichmann, D.; Sperhake, J.P.; Lütgehetmann, M.; Steurer, S.; Edler, C.; Heinemann, A.; Heinrich, F.; Mushumba, H.; Kniep, I.; Schröder, A.S.; et al. Autopsy Findings and Venous Thromboembolism in Patients with COVID-19: A Prospective Cohort Study. Ann. Intern. Med. 2020, 173, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Wickham, N.; Gallus, A.S.; Walters, B.N.; Wilson, A.; NHMRC VTE Prevention Guideline Adaptation Committee. Prevention of venous thromboembolism in patients admitted to Australian hospitals: Summary of national health and medical research council clinical practice guideline. Intern. Med. J. 2012, 42, 698–708. [Google Scholar] [CrossRef] [PubMed]
- Scheres, L.J.J.; Lijfering, W.M.; Cannegieter, S.C. Current and future burden of venous thrombosis: Not simply predictable. Res. Pract. Thromb. Haemost. 2018, 2, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.; Cook, D.J.; Meade, M.O.; Griffith, L.E.; Mehta, G.; Rocker, G.M.; Marshall, J.C.; Hodder, R.; Martin, C.M.; Heyland, D.K.; et al. Burden of illness in venous thromboembolism in critical care: A multicenter observational study. J. Crit. Care 2005, 20, 341–347. [Google Scholar] [CrossRef]
- Akaraborworn, O.; Chittawatanarat, K.; Chatmongkolchart, S.; Kitsiripant, C. Modalities in venous thromboembolism prophylaxis and symptomatic venous thromboembolism occurrence in critically ill surgical patients (THAI-SICU Study). J. Med. Assoc. Thail. 2016, 99 (Suppl. S6), S112–S117. [Google Scholar]
- Baylis, R.A.; Smith, N.L.; Klarin, D.; Fukaya, E. Epidemiology and Genetics of Venous Thromboembolism and Chronic Venous Disease. Circ. Res. 2021, 128, 1988–2002. [Google Scholar] [CrossRef]
- Nobre, C.; Thomas, B. Analysis of National Trends in Admissions for Pulmonary Embolism. Chest 2016, 150, 250. [Google Scholar] [CrossRef][Green Version]
- Gregson, J.; Kaptoge, S.; Bolton, T.; Pennells, L.; Willeit, P.; Burgess, S.; Bell, S.; Sweeting, M.; Rimm, E.B.; Kabrhel, C.; et al. Cardiovascular Risk Factors Associated With Venous Thromboembolism. JAMA Cardiol. 2019, 4, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Krenitsky, N.; Friedman, A.M.; Yu, K.; Gyamfi-Bannerman, C.; Williams-Kane, J.; O’Shaugnessy, F.; Huang, Y.; Wright, J.D.; D’Alton, M.E.; Wen, T. Trends in Venous Thromboembolism and Associated Risk Factors During Delivery Hospitalizations from 2000 to 2018. Obstet. Gynecol. 2022, 139, 223–234. [Google Scholar] [CrossRef]
- Nemeth, B.; Lijfering, W.M.; Nelissen, R.; Schipper, I.B.; Rosendaal, F.R.; le Cessie, S.; Cannegieter, S.C. Risk and Risk Factors Associated With Recurrent Venous Thromboembolism Following Surgery in Patients with History of Venous Thromboembolism. JAMA Netw. Open 2019, 2, e193690. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.W.; Bang, S.M.; Kim, S.; Lee, H.J.; Shin, D.Y.; Koh, Y.; Lee, Y.G.; Cha, Y.; Kim, Y.J.; Kim, J.H.; et al. The incidence, risk factors and prognostic implications of venous thromboembolism in patients with gastric cancer. J. Thromb. Haemost. JTH 2010, 8, 540–547. [Google Scholar] [CrossRef] [PubMed]
- Tøndel, B.G.; Morelli, V.M.; Hansen, J.B.; Braekkan, S.K. Risk factors and predictors for venous thromboembolism in people with ischemic stroke: A systematic review. J. Thromb. Haemost. JTH 2022, 20, 2173–2186. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.T.; Jitaroon, K.; Song, S.; Roozdar, P.; Wangworat, Y.; Ibrahim, N.; Ma, Y.; Rao, V.K.; Chang, S.D.; Fernandez-Miranda, J.C.; et al. Venous thromboembolism rates and risk factors following endoscopic skull base surgery. Int. Forum Allergy Rhinol. 2022, 12, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Heit, J.A.; Spencer, F.A.; White, R.H. The epidemiology of venous thromboembolism. J. Thromb. Thrombolysis 2016, 41, 3–14. [Google Scholar] [CrossRef]
- Flinterman, L.E.; van Hylckama Vlieg, A.; Cannegieter, S.C.; Rosendaal, F.R. Long-term survival in a large cohort of patients with venous thrombosis: Incidence and predictors. PLoS Med. 2012, 9, e1001155. [Google Scholar] [CrossRef]
- Morange, P.E.; Suchon, P. Genetics of venous thrombosis: Update in 2015. Thromb. Haemost. 2015, 114, 910–919. [Google Scholar]
- Lutsey, P.L.; Evensen, L.H.; Thenappan, T.; Prins, K.W.; Walker, R.F.; Farley, J.F.; MacLehose, R.F.; Alonso, A.; Zakai, N.A. Incidence and Risk Factors of Pulmonary Hypertension After Venous Thromboembolism: An Analysis of a Large Health Care Database. J. Am. Heart Assoc. 2022, 11, e024358. [Google Scholar] [CrossRef]
- Makedonov, I.; Kahn, S.R.; Abdulrehman, J.; Schulman, S.; Delluc, A.; Gross, P.; Galanaud, J.P. Prevention of the Postthrombotic Syndrome with Anticoagulation: A Narrative Review. Thromb. Haemost. 2022, 122, 1255–1264. [Google Scholar] [CrossRef]
- Vrabel, M. Preferred Reporting Items for Systematic Reviews and Meta-Analyses. Oncol. Nurs. Forum 2015, 42, 552–554. [Google Scholar] [CrossRef]
- Parker, G.; Beresford, B.; Clarke, S.; Gridley, K.; Pitman, R.; Spiers, G.; Light, K. Technical Report for SCIE Research Review on the Prevalence and Incidence of Parental Mental Health Problems and the Detection, Screening and Reporting of Parental Mental Health Problems; University of York: Heslington, UK, 2008. [Google Scholar]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Tucker, H.H.; Carson, P.H.; Bass, N.M.; Sharratt, G.P.; Stock, J.P. Results of early mobilization and discharge after myocardial infarction. Br. Med. J. 1973, 1, 10–13. [Google Scholar] [CrossRef][Green Version]
- Kollef, M.H.; Eisenberg, P.R.; Shannon, W. A rapid assay for the detection of circulating D-dimer is associated with clinical outcomes among critically ill patients. Crit. Care Med. 1998, 26, 1054–1060. [Google Scholar] [CrossRef]
- Khouli, H.; Shapiro, J.; Pham, V.P.; Arfaei, A.; Esan, O.; Jean, R.; Homel, P. Efficacy of deep venous thrombosis prophylaxis in the medical intensive care unit. J. Intensive Care Med. 2006, 21, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Muscedere, J.G.; Heyland, D.K.; Cook, D. Venous thromboembolism in critical illness in a community intensive care unit. J. Crit. Care 2007, 22, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Salim, A.; Hadjizacharia, P.; Dubose, J.; Kobayashi, L.; Inaba, K.; Chan, L.S.; Margulies, D.R. What is the significance of thrombocytosis in patients with trauma? J. Trauma-Inj. Infect. Crit. Care 2009, 66, 1349–1354. [Google Scholar] [CrossRef]
- Ravenel, J.G.; Northam, M.C.; Nguyen, S.A. Negative predictive value of computed tomography pulmonary angiography with indirect computed tomography venography in intensive care unit patients. J. Comput. Assist. Tomogr. 2009, 33, 739–742. [Google Scholar] [CrossRef]
- Park, M.S.; Martini, W.Z.; Dubick, M.A.; Salinas, J.; Butenas, S.; Kheirabadi, B.S.; Pusateri, A.E.; Vos, J.A.; Guymon, C.H.; Wolf, S.E.; et al. Thromboelastography as a better indicator of hypercoagulable state after injury than prothrombin time or activated partial thromboplastin time. J. Trauma 2009, 67, 266–275; discussion 275–276. [Google Scholar] [CrossRef]
- Thorson, C.M.; Ryan, M.L.; Van Haren, R.M.; Curia, E.; Barrera, J.M.; Guarch, G.A.; Busko, A.M.; Namias, N.; Livingstone, A.S.; Proctor, K.G. Venous thromboembolism after trauma: A never event?*. Crit. Care Med. 2012, 40, 2967–2973. [Google Scholar] [CrossRef] [PubMed]
- Praeger, A.J.; Westbrook, A.J.; Nichol, A.D.; Wijemunige, R.; Davies, A.R.; Lyon, S.M.; Wills, J.L.; Bailey, M.; Rosenfeld, J.V.; Cooper, D.J. Deep vein thrombosis and pulmonary embolus in patients with traumatic brain injury: A prospective observational study. Crit. Care Resusc. J. Australas. Acad. Crit. Care Med. 2012, 14, 10–13. [Google Scholar]
- Minet, C.; Lugosi, M.; Savoye, P.Y.; Menez, C.; Ruckly, S.; Bonadona, A.; Schwebel, C.; Hamidfar-Roy, R.; Dumanoir, P.; Ara-Somohano, C.; et al. Pulmonary embolism in mechanically ventilated patients requiring computed tomography: Prevalence, risk factors, and outcome. Crit. Care Med. 2012, 40, 3202–3208. [Google Scholar] [CrossRef] [PubMed]
- Adimi Naghan, P.; Malekmohammad, M.; Jamaati, H.; Sharifkashani, B.; Najafi, A.; Hashemian, S.M. Venous thromboembolism in medical critically ill patients: Prevalence and incidence. Acta Med. Iran. 2013, 51, 168–171. [Google Scholar] [PubMed]
- Malinoski, D.; Ewing, T.; Patel, M.S.; Jafari, F.; Sloane, B.; Nguyen, B.; Barrios, C.; Kong, A.; Cinat, M.; Dolich, M.; et al. Risk factors for venous thromboembolism in critically ill trauma patients who cannot receive chemical prophylaxis. Inj. Int. J. Care Inj. 2013, 44, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Nickele, C.M.; Kamps, T.K.; Medow, J.E. Safety of a DVT chemoprophylaxis protocol following traumatic brain injury: A single center quality improvement initiative. Neurocritical Care 2013, 18, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.S.; Ewing, T.; Kong, A.; Nguyen, D.; Lau, C.; Barrios, C.; Cinat, M.; Dolich, M.; Lekawa, M.; Malinoski, D. Risk factors for venous thromboembolism in critically ill nontrauma surgical patients who cannot receive chemical prophylaxis. Am. J. Surg. 2013, 206, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Camous, L.; Veyradier, A.; Darmon, M.; Galicier, L.; Mariotte, E.; Canet, E.; Parquet, N.; Azoulay, É. Macrovascular thrombosis in critically ill patients with thrombotic micro-angiopathies. Intern. Emerg. Med. 2014, 9, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Valle, E.J.; Van Haren, R.M.; Allen, C.J.; Jouria, J.M.; Bullock, M.R.; Schulman, C.I.; Namias, N.; Livingstone, A.S.; Proctor, K.G. Does traumatic brain injury increase the risk for venous thromboembolism in polytrauma patients? J. Trauma Acute Care Surg. 2014, 77, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Okumus, G.; Ozcelik, B.; Sasani, H.; Ozcan, P.E.; Kiyan, E.; Salmaslioglu, A.; Senturk, E.; Issever, H.; Arseven, O. Do appropriate thromboprophylaxis and routine physiotherapy prevent venous thromboembolism in intensive care unit? Turk. Gogus Kalp Damar Cerrahisi Derg. -Turk. J. Thorac. Cardiovasc. Surg. 2015, 23, 92–97. [Google Scholar] [CrossRef][Green Version]
- Obi, A.T.; Pannucci, C.J.; Nackashi, A.; Abdullah, N.; Alvarez, R.; Bahl, V.; Wakefield, T.W.; Henke, P.K. Validation of the Caprini venous thromboembolism risk assessment model in citically ill surgical patients. JAMA Surg. 2015, 150, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Muciño-Bermejo, J.; Carrillo-Esper, R.; Méndez-Sánchez, N.; Uribe, M. Thrombosis and hemorrhage in the critically ill cirrhotic patients: Five years retrospective prevalence study. Ann. Hepatol. 2015, 14, 93–98. [Google Scholar] [CrossRef]
- Allen, C.J.; Murray, C.R.; Meizoso, J.P.; Ginzburg, E.; Schulman, C.I.; Lineen, E.B.; Namias, N.; Proctor, K.G. Surveillance and early management of deep vein thrombosis decreases rate of pulmonary embolism in high-risk trauma patients. J. Am. Coll. Surg. 2016, 222, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Hamada, S.R.; Espina, C.; Guedj, T.; Buaron, R.; Harrois, A.; Figueiredo, S.; Duranteau, J. High level of venous thromboembolism in critically ill trauma patients despite early and well-driven thromboprophylaxis protocol. Ann. Intensive Care 2017, 7, 97. [Google Scholar] [CrossRef] [PubMed]
- Karcutskie, C.A.; Dharmaraja, A.; Patel, J.; Eidelson, S.A.; Martin, A.G.; Lineen, E.B.; Namias, N.; Schulman, C.I.; Proctor, K.G. Relation of antifactor-Xa peak levels and venous thromboembolism after trauma. J. Trauma Acute Care Surg. 2017, 83, 1102–1107. [Google Scholar] [CrossRef] [PubMed]
- Karcutskie, C.A.; Meizoso, J.P.; Ray, J.J.; Horkan, D.; Ruiz, X.D.; Schulman, C.I.; Namias, N.; Proctor, K.G. Association of mechanism of Injury with risk for venous thromboembolism after trauma. JAMA Surg. 2017, 152, 35–40. [Google Scholar] [CrossRef]
- Yumoto, T.; Naito, H.; Yamakawa, Y.; Iida, A.; Tsukahara, K.; Nakao, A. Venous thromboembolism in major trauma patients: A single-center retrospective cohort study of the epidemiology and utility of D-dimer for screening. Acute Med. Surg. 2017, 4, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Liu, Y.; Chen, S.; Jin, Y.; Jiang, H. The combination of Caprini risk assessment scale and thrombotic biomarkers to evaluate the risk of venous thromboembolism in critically ill patients. Medicine 2018, 97, e13232. [Google Scholar] [CrossRef] [PubMed]
- Wilsey, H.A.; Pandya, K.; Beavers, C.; Li, X.S.; Ather, A. Comparison of venous thromboembolism prophylactic measures post coronary artery bypass graft surgery. Am. J. Cardiovasc. Drugs 2019, 19, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Brendan Cloney, M.; Goergen, J.; Hopkins, B.S.; Dhillon, E.S.; Dahdaleh, N.S. Factors associated with venous thromboembolic events following ICU admission in patients undergoing spinal surgery: An analysis of 1269 consecutive patients. J. Neurosurg. Spine 2019, 30, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Beitland, S.; Wimmer, H.; Lorentsen, T.; Jacobsen, D.; Draegni, T.; Brunborg, C.; Klow, N.E.; Sandset, P.M.; Sunde, K. Venous thromboembolism in the critically ill: A prospective observational study of occurrence, risk factors and outcome. Acta Anaesthesiol. Scand. 2019, 63, 630–638. [Google Scholar] [CrossRef] [PubMed]
- Harahsheh, Y.; Duff, O.C.; Ho, K.M. Thromboelastography predicts thromboembolism in critically ill coagulopathic patients*. Crit. Care Med. 2019, 47, 826–832. [Google Scholar] [CrossRef]
- Tachino, J.; Yamamoto, K.; Shimizu, K.; Shintani, A.; Kimura, A.; Ogura, H.; Shimazu, T. Quick risk assessment profile (qRAP) is a prediction model for post-traumatic venous thromboembolism. Injury 2019, 50, 1540–1544. [Google Scholar] [CrossRef] [PubMed]
- Brandi, G.; Schmidlin, A.; Klinzing, S.; Schüpbach, R.; Unseld, S.; Pagnamenta, A. Delayed prophylaxis with unfractionated heparin increases the risk of venous thromboembolic events in patients with moderate to severe traumatic brain injury: A retrospective analysis. Anaesthesiol. Intensive Ther. 2020, 52, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Gibson, C.D.; Colvin, M.O.; Park, M.J.; Lai, Q.; Lin, J.; Negassa, A.; Shah, C.D.; Langston, M.D. Prevalence and predictors of deep vein thrombosis in critically ill medical patients who underwent diagnostic duplex ultrasonography. J. Intensive Care Med. 2020, 35, 1062–1066. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, N.K.; Hashim, Y.M.; Conde, G.; Phillips, G.; Fierro, N.M.; Yong, F.; Berezin, N.; Ley, E.J. Early propranolol is associated with lower risk of venous thromboembolism after traumatic brain injury. Am. Surg. 2021, 87, 1556–1560. [Google Scholar] [CrossRef] [PubMed]
- Chu, Q.; Liao, L.; Wei, W.; Ye, Z.; Zeng, L.; Qin, C.; Tang, Y. Venous thromboembolism in ICU patients with intracerebral hemorrhage: Risk factors and the prognosis after anticoagulation therapy. Int. J. Gen. Med. 2021, 14, 5397–5404. [Google Scholar] [CrossRef] [PubMed]
- Ow, T.W.; Fatourou, E.; Rabinowich, L.; van den Boom, B.P.; Nair, S.; Patel, V.C.; Hogan, B.; McPhail, M.; Roberts, L.N.; Bernal, W. Prevalence of bleeding and thrombosis in critically ill patients with chronic liver disease. Thromb. Haemost. 2021, 122, 1006–1016. [Google Scholar] [CrossRef]
- Phan, B.; Fagaragan, L.; Alaraj, A.; Kim, K.S. Multidisciplinary bundle approach in venous thromboembolism prophylaxis in patients with non-traumatic subarachnoid hemorrhage. Clin. Appl. Thromb. Hemost. 2022, 28, 10760296221074682. [Google Scholar] [CrossRef] [PubMed]
- Mei, R.; Wang, G.; Chen, R.; Wang, H. The ICU-venous thromboembolism score and tumor grade can predict inhospital venous thromboembolism occurrence in critical patients with tumors. World J. Surg. Oncol. 2022, 20, 245. [Google Scholar] [CrossRef] [PubMed]
- Dibiasi, C.; Gratz, J.; Wiegele, M.; Schaden, E. Anti-factor Xa activity is not associated with venous thromboembolism in critically ill patients receiving enoxaparin for thromboprophylaxis: A retrospective observational study. Front. Med. 2022, 9, 7. [Google Scholar] [CrossRef] [PubMed]
- Barton, C.; Shapiro, D. Safety of prophylactic anticoagulation during bedside procedures: A prospective multicenter observational study. World J. Surg. 2022, 46, 2625–2631. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Aziz, H.; Alikhan, R.; Arabi, Y.M. The association of timing of pharmacological prophylaxis and venous thromboembolism in patients with moderate-to-severe traumatic brain injury: A retrospective cohort study. Ann. Thorac. Med. 2022, 17, 102–109. [Google Scholar]
- Ajmal, F.; Haroon, M.; Kaleem, U.; Gul, A.; Khan, J. Comparison of chemical and mechanical prophylaxis of venous thromboembolism in non-surgical mechanically ventilated patients. Cureus 2021, 13, e19548. [Google Scholar] [CrossRef] [PubMed]
- Abizanda, R.; Marse, P.; Abadal, J.M. Simplified acute physiology score. Crit. Care Med. 1985, 13, 517. [Google Scholar] [CrossRef]
- Horinuki, F.; Noguchi-Watanabe, M.; Takai, Y.; Yamahana, R.; Ohno, N.; Okada, S.; Mori, S.I.; Yamamoto-Mitani, N. The experience of persons with hematological malignancy when communicating with health care professionals. Qual. Health Res. 2018, 28, 479–490. [Google Scholar] [CrossRef] [PubMed]
- Buja, A.; Damiani, G.; Gini, R.; Visca, M.; Federico, B.; Donato, D.; Francesconi, P.; Marini, A.; Donatini, A.; Brugaletta, S.; et al. Systematic age-related differences in chronic disease management in a population-based cohort study: A new paradigm of primary care is required. PLoS ONE 2014, 9, e91340. [Google Scholar] [CrossRef]
- Srivastava, I.; Thukral, N.; Hasija, Y. Genetics of human age related disorders. Adv. Gerontol. 2015, 28, 228–247. [Google Scholar]
- Outlaw, D.; Dai, C.; Al-Obaidi, M.; Harmon, C.; Giri, S.; Bhatia, S.; Williams, G.R. The association of polypharmacy with functional status impairments, frailty, and health-related quali ty of life in older adults with gastrointestinal malignancy—Results from the Cancer and Aging Resi lience Evaluation (CARE) registry. J. Geriatr. Oncol 2022, 38, 118. [Google Scholar]
- Roldn, V.; Marn, F.; Garca, A.; Tello-Montoliu, A.; Lip, G.Y. Is an advanced age an additive risk factor to the prothrombotic or hypercoagulable state in atrial fi brillation? Int. J. Cardiol. 2006, 110, 265–266. [Google Scholar] [CrossRef] [PubMed]
- Merli, G.J.; Crabbe, S.; Paluzzi, R.G.; Fritz, D. Etiology, incidence, and prevention of deep vein thrombosis in acute spinal cord injury. Arch. Phys. Med. Rehabil. 1993, 74, 1199–1205. [Google Scholar] [PubMed]
- Putz, C.; Schuld, C.; Gantz, S.; Grieser, T.; Akbar, M.; Moradi, B.; Wiedenhöfer, B.; Fürstenberg, C.H.; Gerner, H.J.; Rupp, R. The effect of polytrauma as a possible confounder in the outcome of monotraumatic vs polytraumatic pa raplegic patients: A clinical cohort study. Spinal Cord 2011, 49, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Ortego, A. Calculated Decisions: Injury Severity Score (ISS). Pediatr. Emerg. Med. Pract. 2019, 16, Cd1-2. [Google Scholar] [PubMed]
- Helms, J.; Middeldorp, S.; Spyropoulos, A.C. Thromboprophylaxis in critical care. Intensive Care Med. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Khatri, A.; Davies, A.H.; Shalhoub, J. Mechanical prophylaxis for venous thromboembolism prevention in obese individuals. Phlebology 2021, 36, 768–770. [Google Scholar] [CrossRef] [PubMed]
- Afshari, A.; Fenger-Eriksen, C.; Monreal, M.; Verhamme, P. European guidelines on perioperative venous thromboembolism prophylaxis: Mechanical prophylaxis. Eur. J. Anaesth. 2018, 35, 112–115. [Google Scholar] [CrossRef]
- Hong, Y.; Zhang, Y.; Xiang, Y.; Ye, Z.; Lu, X. Incidence of venous thromboembolism and hemorrhage in Chinese patients after pulmonary lobectomy: Mechanical prophylaxis or mechanical prophylaxis combined with pharmacological prophylaxis: A randomized controlled trial. Ann. Transl. Med. 2021, 9, 1478. [Google Scholar] [CrossRef]
- Kakkos, S.; Kirkilesis, G.; Caprini, J.A.; Geroulakos, G.; Nicolaides, A.; Stansby, G.; Reddy, D.J. Combined intermittent pneumatic leg compression and pharmacological prophylaxis for prevention of venous thromboembolism. Cochrane Database Syst. Rev. 2022, 1, Cd005258. [Google Scholar] [CrossRef]
- Long, J.; Huang, G.; Liang, W.; Liang, B.; Chen, Q.; Xie, J.; Jiang, J.; Su, L. The prevalence of schizophrenia in mainland China: Evidence from epidemiological surveys. Acta Psychiatr. Scand. 2014, 130, 244–256. [Google Scholar] [CrossRef]
- Winsper, C.; Ganapathy, R.; Marwaha, S.; Large, M.; Birchwood, M.; Singh, S.P. A systematic review and meta-regression analysis of aggression during the first episode of psychosis. Acta Psychiatr. Scand. 2013, 128, 413–421. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).