Antihypertensive Therapy and Incidence of Cancer
Abstract
1. Introduction
2. Methods
2.1. Database
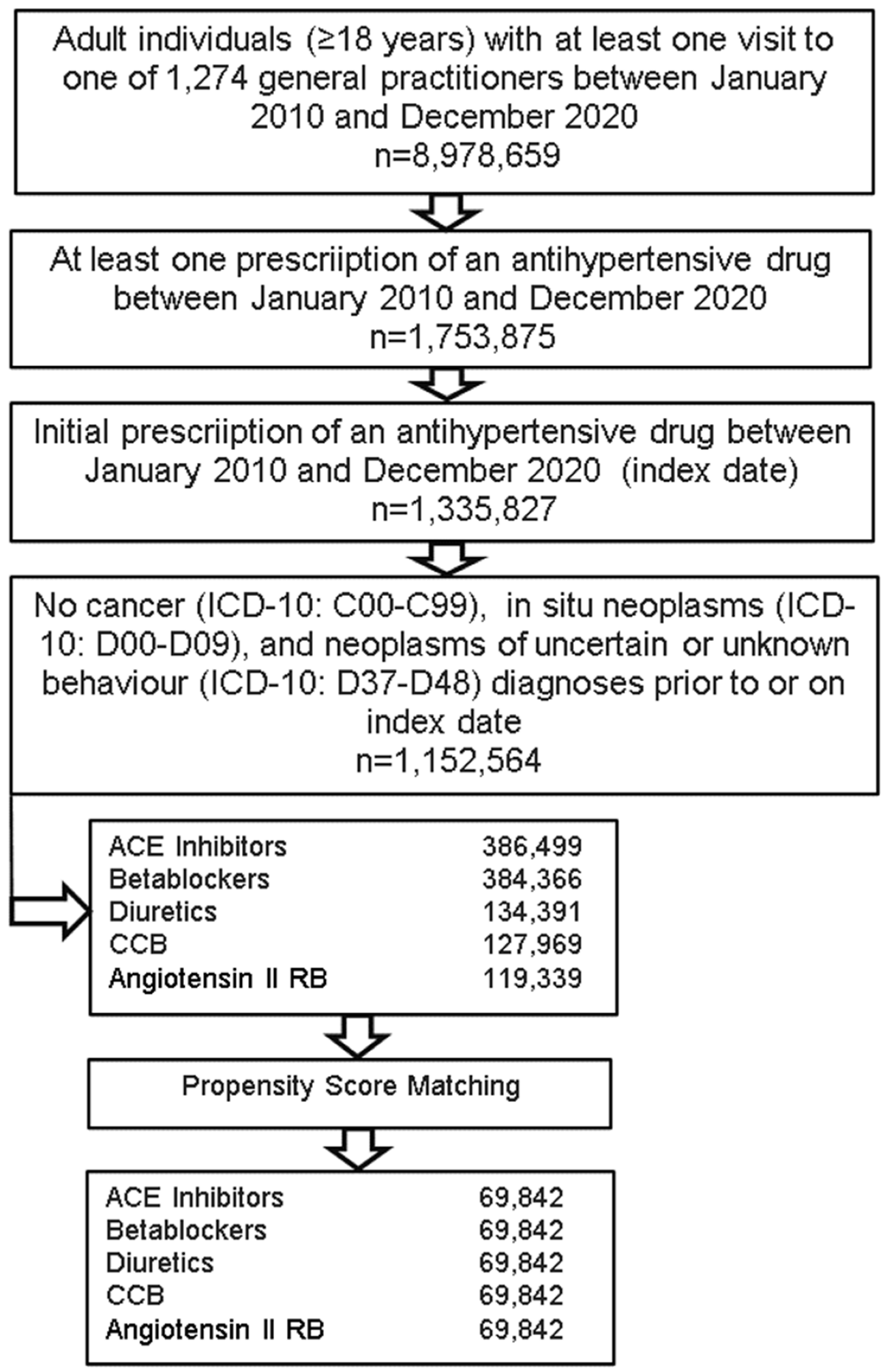
2.2. Study Population
2.3. Study Outcomes and Covariates
2.4. Statistical Analyses
3. Results
3.1. Basic Characteristics of the Study Sample
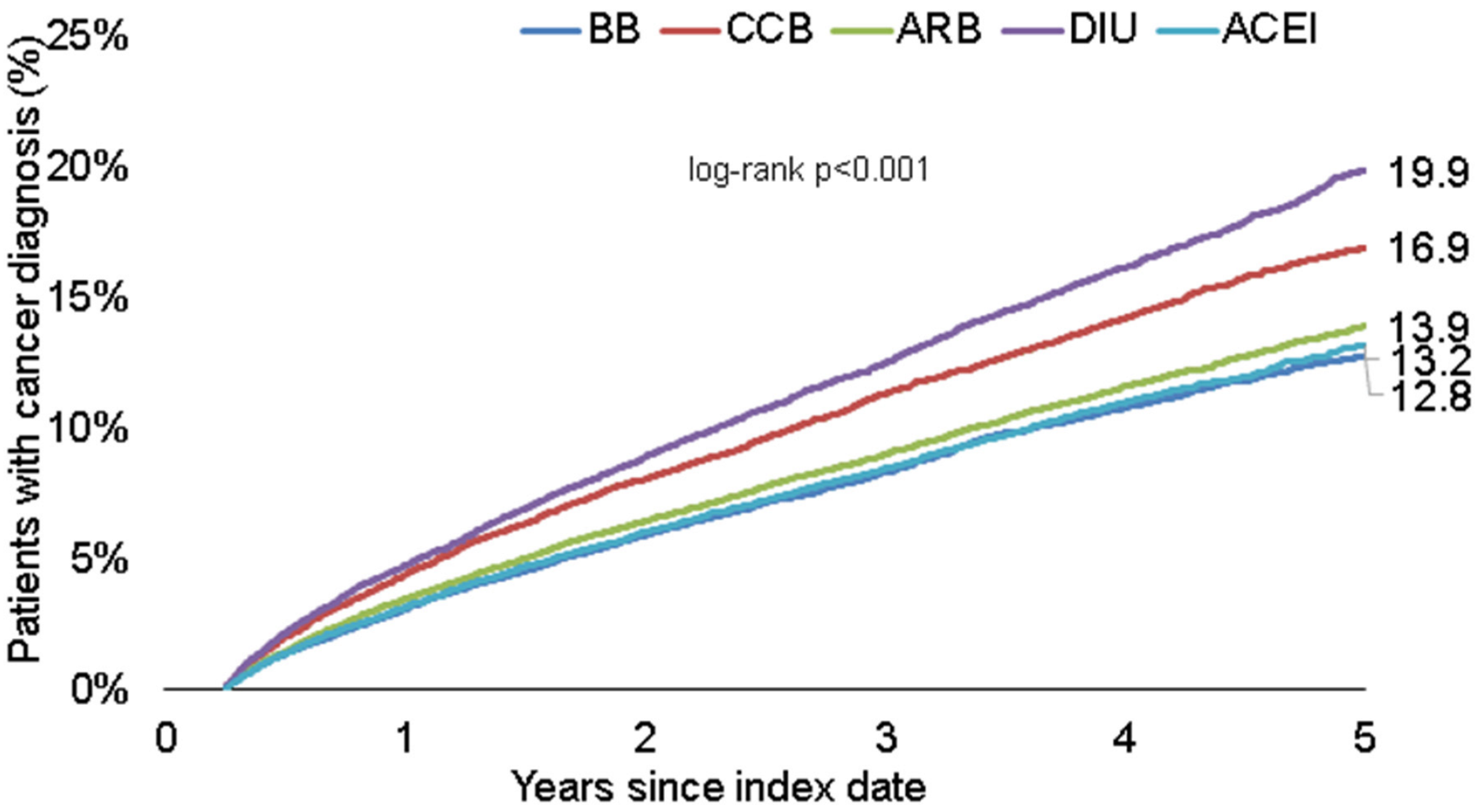
3.2. Cumulative Incidence of Cancer Diagnoses
3.3. Antihypertensive Therapy and Specific Cancer Site Incidences
4. Discussion
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K.; et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Hajjar, I.; Kotchen, J.M.; Kotchen, T.A. Hypertension: Trends in prevalence, incidence, and control. Annu. Rev. Public Health 2006, 27, 465–490. [Google Scholar] [CrossRef] [PubMed]
- Battistoni, A.; Tocci, G.; Presta, V.; Volpe, M. Antihypertensive drugs and the risks of cancer: More fakes than facts. Eur. J. Prev. Cardiol. 2021, 28, 1323–1326. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Bangalore, S. Which, if any, antihypertensive agents cause cancer? Curr. Opin. Cardiol. 2012, 27, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Copland, E.; Canoy, D.; Nazarzadeh, M.; Bidel, Z.; Ramakrishnan, R.; Woodward, M.; Chalmers, J.; Teo, K.K.; Pepine, C.J.; Davis, B.R.; et al. Antihypertensive treatment and risk of cancer: An individual participant data meta-analysis. Lancet Oncol. 2021, 22, 558–570. [Google Scholar] [CrossRef]
- Rathmann, W.; Bongaerts, B.; Carius, H.J.; Kruppert, S.; Kostev, K. Basic characteristics and representativeness of the German Disease Analyzer database. Int. J. Clin. Pharmacol. Ther. 2018, 56, 459–466. [Google Scholar] [CrossRef]
- Jacob, L.; Kostev, K. Persistence with antihypertensive drugs in patients with depression in Germany. Int. J. Clin. Pharmacol. Ther. 2018, 56, 162–168. [Google Scholar] [CrossRef]
- Warda, A.; Reese, J.P.; Tanislav, C.; Kostev, K. The association between antihypertensive therapy and the incidence of Parkinson’s disease in patients followed in general practices in Germany. Int. J. Clin. Pharmacol. Ther. 2019, 57, 483–488. [Google Scholar] [CrossRef]
- Loosen, S.H.; Jördens, M.S.; Luedde, M.; Modest, D.P.; Labuhn, S.; Luedde, T.; Kostev, K.; Roderburg, C. Incidence of Cancer in Patients with Irritable Bowl Syndrome. J. Clin. Med. 2021, 10, 5911. [Google Scholar] [CrossRef]
- Loosen, S.H.; Roderburg, C.; Jördens, M.S.; Fluegen, G.; Luedde, T.; Kostev, K. Overweight and Obesity Determine the Risk for Gastrointestinal Cancer in a Sex-Dependent Manner: A Retrospective Cohort Study of 287,357 Outpatients in Germany. Cancers 2022, 14, 931. [Google Scholar] [CrossRef]
- Natarajan, Y.; Kramer, J.R.; Yu, X.; Li, L.; Thrift, A.P.; El-Serag, H.B.; Kanwal, F. Risk of Cirrhosis and Hepatocellular Cancer in Patients With NAFLD and Normal Liver Enzymes. Hepatology 2020, 72, 1242–1252. [Google Scholar] [CrossRef] [PubMed]
- Largent, J.A.; McEligot, A.J.; Ziogas, A.; Reid, C.; Hess, J.; Leighton, N.; Peel, D.; Anton-Culver, H. Hypertension, diuretics and breast cancer risk. J. Hum. Hypertens. 2006, 20, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Garrido, P.M.; Borges-Costa, J. Hydrochlorothiazide treatment and risk of non-melanoma skin cancer: Review of the literature. Rev. Port. Cardiol. 2020, 39, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Santosa, D.; Castoldi, M.; Paluschinski, M.; Sommerfeld, A.; Häussinger, D. Hyperosmotic stress activates the expression of members of the miR-15/107 family and induces downregulation of anti-apoptotic genes in rat liver. Sci. Rep. 2015, 5, 12292. [Google Scholar] [CrossRef]
- Bardeck, N.; Paluschinski, M.; Castoldi, M.; Kordes, C.; Görg, B.; Stindt, J.; Luedde, T.; Dahl, S.V.; Häussinger, D.; Schöler, D. Swelling-induced upregulation of miR-141-3p inhibits hepatocyte proliferation. JHEP Rep. 2022, 4, 100440. [Google Scholar] [CrossRef]
- César, K.R.; Magaldi, A.J. Thiazide induces water absorption in the inner medullary collecting duct of normal and Brattleboro rats. Am. J. Physiol. 1999, 277, F756–F760. [Google Scholar] [CrossRef]
- Mackenzie, I.S.; Morant, S.V.; Wei, L.; Thompson, A.M.; MacDonald, T.M. Spironolactone use and risk of incident cancers: A retrospective, matched cohort study. Br. J. Clin. Pharmacol. 2017, 83, 653–663. [Google Scholar] [CrossRef]
- Hiebert, B.M.; Janzen, B.W.; Sanjanwala, R.M.; Ong, A.D.; Feldman, R.D.; Kim, J.O. Impact of spironolactone exposure on prostate cancer incidence amongst men with heart failure: A Pharmacoepidemiological study. Br. J. Clin. Pharmacol. 2021, 87, 1801–1813. [Google Scholar] [CrossRef]
- Cao, L.; Zhang, S.; Jia, C.M.; He, W.; Wu, L.T.; Li, Y.Q.; Wang, W.; Li, Z.; Ma, J. Antihypertensive drugs use and the risk of prostate cancer: A meta-analysis of 21 observational studies. BMC Urol. 2018, 18, 17. [Google Scholar] [CrossRef]
- Uemura, H.; Ishiguro, H.; Nagashima, Y.; Sasaki, T.; Nakaigawa, N.; Hasumi, H.; Kato, S.; Kubota, Y. Antiproliferative activity of angiotensin II receptor blocker through cross-talk between stromal and epithelial prostate cancer cells. Mol. Cancer Ther. 2005, 4, 1699–1709. [Google Scholar] [CrossRef]
- Rao, G.A.; Mann, J.R.; Bottai, M.; Uemura, H.; Burch, J.B.; Bennett, C.L.; Haddock, K.S.; Hébert, J.R. Angiotensin receptor blockers and risk of prostate cancer among united states veterans. J. Clin. Pharmacol. 2013, 53, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Franceschini, N.; Chasman, D.I.; Cooper-DeHoff, R.M.; Arnett, D.K. Genetics, ancestry, and hypertension: Implications for targeted antihypertensive therapies. Curr. Hypertens. Rep. 2014, 16, 461. [Google Scholar] [CrossRef] [PubMed]
| Variable | Proportion Affected among Patients Treated with ACEI (%) | Proportion Affected among Patients Treated with BB (%) | Proportion Affected among Patients Treated with DIU (%) | Proportion Affected among Patients Treated with CCB (%) | Proportion Affected among Patients Treated with ARB (%) | p-Value |
|---|---|---|---|---|---|---|
| N | 69,842 | 69,842 | 69,842 | 69,842 | 69,842 | |
| Age (Mean, SD) | 65.8 (13.8) | 65.8 (13.8) | 65.8 (13.8) | 65.8 (13.8) | 65.8 (13.8) | 1.000 |
| Age ≤ 60 | 34.6 | 34.6 | 34.6 | 34.6 | 34.6 | 1.000 |
| Age 61–70 | 24.0 | 24.0 | 24.0 | 24.0 | 24.0 | |
| Age 71–80 | 26.9 | 26.9 | 26.9 | 26.9 | 26.9 | |
| Age > 80 | 14.5 | 14.5 | 14.5 | 14.5 | 14.5 | |
| Women | 56.7 | 56.7 | 56.7 | 56.7 | 56.7 | 1.000 |
| Men | 43.3 | 43.3 | 43.3 | 43.3 | 43.3 | |
| Diabetes | 18.4 | 18.4 | 18.4 | 18.4 | 18.4 | 1.000 |
| Obesity | 11.7 | 11.7 | 11.7 | 11.7 | 11.7 | 1.000 |
| Lipid metabolism disorder | 20.9 | 20.9 | 20.9 | 20.9 | 20.9 | 1.000 |
| Hypertension | 58.1 | 58.1 | 58.1 | 58.1 | 58.1 | 1.000 |
| Ischemic heart diseases | 12.8 | 12.8 | 12.8 | 12.8 | 12.8 | 1.000 |
| Heart failure | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 1.000 |
| COPD | 6.6 | 6.6 | 6.6 | 6.6 | 6.6 | 1.000 |
| Liver diseases | 5.1 | 5.1 | 5.1 | 5.1 | 5.1 | 1.000 |
| Cancers Site | BB vs. Rest | CCB vs. Rest | ARB vs. Rest | DIU vs. Rest | ACEI vs. Rest |
|---|---|---|---|---|---|
| Cancer total | 0.88 (0.83–0.93) | 1.03 (0.98–1.09) | 1.10 (1.04–1.16) | 0.98 (0.93–1.04) | 1.00 (0.95–1.06) |
| Prostate (men) | 0.85 (0.70–1.02) | 1.01 (0.85–1.20) | 1.50 (1.28–1.65) | 0.64 (0.53–0.78) | 1.08 (0.91–1.28) |
| Breast (women) | 0.78 (0.62–0.92) | 0.93 (0.80–1.08) | 1.15 (0.99–1.32) | 1.05 (0.91–1.22) | 1.10 (0.95–1.26) |
| Female genital organs (women) | 0.70 (0.51–0.97) | 0.94 (0.71–1.23) | 1.10 (0.84–1.43) | 1.36 (1.06–1.74) | 0.91 (0.69–1.21) |
| Skin | 0.94 (0.83–1.07) | 1.09 (0.98–1.22) | 1.14 (1.02–1.27) | 0.81 (0.72–0.92) | 1.03 (0.92–1.16) |
| Respiratory organs | 0.97 (0.79.1.20) | 1.09 (0.90–1.35) | 0.91 (0.74–1.12) | 1.13 (0.94–1.37) | 0.89 (0.73–1.09) |
| Digestive organs excl. liver | 0.80 (0.69–0.93) | 1.14 (1.00–1.29) | 1.00 (0.87–1.14) | 0.97 (0.85–1.11) | 1.09 (0.95–1.24) |
| Liver | 1.22 (0.78–1.91) | 0.68 (0.40–1.14) | 0.79 (0.48–1.30) | 1.71 (1.12–2.63) | 0.78 (0.48–1.29) |
| Urinary tract | 0.78 (0.53–0.92) | 1.22 (1.01–1.48) | 1.22 (1.01–1.49) | 0.81 (0.66–1.00) | 1.05 (0.86–1.29) |
| Lymphoid and haematopoietic tissue | 0.96 (0.82–1.13) | 0.88 (0.75–1.03) | 1.03 (0.89–1.19) | 1.27 (1.10–1.46) | 0.88 (0.75–1.02) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loosen, S.H.; Schöler, D.; Luedde, M.; Eschrich, J.; Luedde, T.; Gremke, N.; Kalder, M.; Kostev, K.; Roderburg, C. Antihypertensive Therapy and Incidence of Cancer. J. Clin. Med. 2022, 11, 6624. https://doi.org/10.3390/jcm11226624
Loosen SH, Schöler D, Luedde M, Eschrich J, Luedde T, Gremke N, Kalder M, Kostev K, Roderburg C. Antihypertensive Therapy and Incidence of Cancer. Journal of Clinical Medicine. 2022; 11(22):6624. https://doi.org/10.3390/jcm11226624
Chicago/Turabian StyleLoosen, Sven H., David Schöler, Mark Luedde, Johannes Eschrich, Tom Luedde, Niklas Gremke, Matthias Kalder, Karel Kostev, and Christoph Roderburg. 2022. "Antihypertensive Therapy and Incidence of Cancer" Journal of Clinical Medicine 11, no. 22: 6624. https://doi.org/10.3390/jcm11226624
APA StyleLoosen, S. H., Schöler, D., Luedde, M., Eschrich, J., Luedde, T., Gremke, N., Kalder, M., Kostev, K., & Roderburg, C. (2022). Antihypertensive Therapy and Incidence of Cancer. Journal of Clinical Medicine, 11(22), 6624. https://doi.org/10.3390/jcm11226624









