Adverse Birth and Child Outcomes in Children Fathered by Men Treated with Antidiabetics Prior to Conception: A Nationwide Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Setting
2.2. Study Population
2.3. Exposed Cohorts
2.4. Unexposed Cohort
2.5. Birth and Child Outcomes
2.6. Confounders
2.7. Statistical Analyses
2.8. Approvals and Ethics
2.9. Patient and Public Involvement
3. Results
3.1. Preconception Paternal Use of Insulin
3.2. Preconception Paternal Use of Non-Insulin Anti-Hyperglycemic Agents
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Braun, J.M.; Messerlian, C.; Hauser, R. Fathers Matter: Why It’s Time to Consider the Impact of Paternal Environmental Expo-sures on Children’s Health. Curr. Epidemiol. Rep. 2017, 4, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Lane, M.; Robker, R.L.; Robertson, S.A. Parenting from before conception. Science 2014, 345, 756–760. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, T.G.; Aston, K.I.; James, E.R.; Carrell, D.T. Sperm epigenetics in the study of male fertility, offspring health, and potential clinical applications. Syst. Biol. Reprod. Med. 2017, 63, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Soubry, A.; Hoyo, C.; Jirtle, R.L.; Murphy, S.K. A paternal environmental legacy: Evidence for epigenetic inheritance through the male germ line. BioEssays 2014, 36, 359–371. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Hauser, R.; Krawetz, S.A.; Pilsner, J.R. Environmental Susceptibility of the Sperm Epigenome During Windows of Male Germ Cell Development. Curr. Environ. Health Rep. 2015, 2, 356–366. [Google Scholar] [CrossRef]
- Fullston, T.; McPherson, N.O.; Owens, J.A.; Kang, W.X.; Sandeman, L.Y.; Lane, M. Paternal obesity induces metabolic and sperm disturbances in male offspring that are exacerbated by their exposure to an “obesogenic” diet. Physiol. Rep. 2015, 3, e12336. [Google Scholar] [CrossRef]
- Kalagiri, R.R.; Carder, T.; Choudhury, S.; Vora, N.; Ballard, A.R.; Govande, V.; Drever, N.; Beeram, M.R.; Uddin, M.N. Inflammation in Complicated Pregnancy and Its Outcome. Am. J. Perinatol. 2016, 33, 1337–1356. [Google Scholar] [CrossRef]
- Moss, J.L.; Harris, K.M. Impact of maternal and paternal preconception health on birth outcomes using prospective couples’ data in Add Health. Arch. Gynecol. Obstet. 2014, 291, 287–298. [Google Scholar] [CrossRef]
- Zhou, Q.; Song, L.; Chen, J.; Wang, Q.; Shen, H.; Zhang, S.; Li, X. Association of Preconception Paternal Alcohol Consumption with Increased Fetal Birth Defect Risk. JAMA Pediatr. 2021, 175, 742–743. [Google Scholar] [CrossRef]
- Wensink, M.J.; Lu, Y.; Tian, L.; Shaw, G.M.; Rizzi, S.; Jensen, T.K.; Mathiesen, E.R.; Skakkebæk, N.E.; Lindahl-Jacobsen, R.; Eisenberg, M.L. Preconception Antidiabetic Drugs in Men and Birth Defects in Offspring: A Nationwide Cohort Study. Obstet. Gynecol. Surv. 2022, 77, 413–414. [Google Scholar] [CrossRef]
- Agbaje, I.; Rogers, D.; McVicar, C.; McClure, N.; Atkinson, A.; Mallidis, C.; Lewis, S. Insulin dependant diabetes mellitus: Implications for male reproductive function. Hum. Reprod. 2007, 22, 1871–1877. [Google Scholar] [CrossRef]
- Imani, M.; Talebi, A.R.; Fesahat, F.; Rahiminia, T.; Seifati, S.M.; Dehghanpour, F. Sperm parameters, DNA integrity, and protamine expression in patients with type II diabetes mellitus. J. Obstet. Gynaecol. J. Inst. Obstet. Gynaecol. 2021, 41, 439–446. [Google Scholar] [CrossRef]
- Ferreira, C.; Sousa, M.; Rabaça, A.; Oliveira, P.F.; Alves, M.; Sá, R. Impact of Metformin on Male Reproduction. Curr. Pharm. Des. 2015, 21, 3621–3633. [Google Scholar] [CrossRef]
- Rama Raju, G.A.; Jaya Prakash, G.; Murali Krishna, K.; Madan, K.; Siva Narayana, T.; Ravi Krishna, C.H. Noninsulin-dependent diabetes mellitus: Effects on sperm morphological and functional characteristics, nuclear DNA integrity and outcome of as-sisted reproductive technique. Andrologia 2012, 44 (Suppl. 1), 490–498. [Google Scholar] [CrossRef]
- La Vignera, S.; Condorelli, R.; Vicari, E.; D’Agata, R.; Calogero, A.E. Diabetes mellitus and sperm parameters. J. Androl. 2012, 33, 145–153. [Google Scholar] [CrossRef]
- Sexton, W.J.; Jarow, J.P. Effect of diabetes mellitus upon male reproductive function. Urology 1997, 49, 508–513. [Google Scholar] [CrossRef]
- Schöffling, K.; Federlin, K.; Ditschuneit, H.; Pfeiffer, E.F. Disorders of Sexual Function in Male Diabetics. Diabetes 1963, 12, 519–527. [Google Scholar] [CrossRef]
- Bourne, R.B.; Kretzschmar, W.A.; Esser, J.H. Successful Artificial Insemination in a Diabetic with Retrograde Ejaculation. Fertil. Steril. 1971, 22, 275–277. [Google Scholar] [CrossRef]
- Fedele, D. Therapy Insight: Sexual and bladder dysfunction associated with diabetes mellitus. Nat. Clin. Pract. Urol. 2005, 2, 282–290. [Google Scholar] [CrossRef]
- De Young, L.; Yu, D.; Bateman, R.M.; Brock, G.B. Oxidative stress and antioxidant therapy: Their impact in diabetes-associated erectile dysfunction. J. Androl. 2004, 25, 830–836. [Google Scholar] [CrossRef]
- Fedder, J.; Kaspersen, M.D.; Brandslund, I.; Hojgaard, A. Retrograde ejaculation and sexual dysfunction in men with diabetes mellitus: A prospective, controlled study. Andrology 2013, 1, 602–606. [Google Scholar] [CrossRef]
- Hu, Y.; Ding, B.; Shen, Y.; Yan, R.-N.; Li, F.-F.; Sun, R.; Jing, T.; Lee, K.-O.; Ma, J.-H. Rapid Changes in Serum Testosterone in Men with Newly Diagnosed Type 2 Diabetes with Intensive Insulin and Metformin. Diabetes Care 2021, 44, 1059–1061. [Google Scholar] [CrossRef] [PubMed]
- Faure, M.; Bertoldo, M.J.; Khoueiry, R.; Bongrani, A.; Brion, F.; Giulivi, C.; Dupont, J.; Froment, P. Metformin in Reproductive Biology. Front. Endocrinol. 2018, 9, 675. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, J.; Langhoff-Roos, J.; Skovgaard, L.T.; Kristensen, F.B. Validation of the danish birth registration. J. Clin. Epidemiol. 1996, 49, 893–897. [Google Scholar] [CrossRef]
- Bliddal, M.; Broe, A.; Pottegård, A.; Olsen, J.; Langhoff-Roos, J. The Danish Medical Birth Register. Eur. J. Epidemiol. 2018, 33, 27–36. [Google Scholar] [CrossRef]
- Schmidt, M.; Schmidt, S.A.J.; Sandegaard, J.L.; Ehrenstein, V.; Pedersen, L.; Sørensen, H.T. The Danish National Patient Registry: A review of content, data quality, and research potential. Clin. Epidemiol. 2015, 7, 449–490. [Google Scholar] [CrossRef]
- Pottegård, A.; Schmidt, S.A.J.; Wallach-Kildemoes, H.; Sørensen, H.T.; Hallas, J.; Schmidt, M. Data Resource Profile: The Danish National Prescription Registry. Int. J. Epidemiol. 2017, 46, 798–798f. [Google Scholar] [CrossRef]
- Pedersen, C.B.; Gøtzsche, H.; Møller, J.O.; Mortensen, P.B. The Danish Civil Registration System. A cohort of eight million persons. Dan. Med. Bull. 2006, 53, 441–449. [Google Scholar]
- Maršál, K.; Persson, P.-H.; Larsen, T.; Lilja, H.; Selbing, A.; Sultan, B. Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr. 1996, 85, 843–848. [Google Scholar] [CrossRef]
- Damkier, P.; Bronniche, L.M.S.; Korch-Frandsen, J.F.B.; Broe, A. In utero exposure to antibiotics and risk of congenital malfor-mations: A population-based study. Am. J. Obs. Gynecol. 2019, 221, 648.E1–648.E15. [Google Scholar] [CrossRef]
- Damkier, P.; Broe, A. First-Trimester Pregnancy Exposure to Modafinil and Risk of Congenital Malformations. JAMA 2020, 323, 374–376. [Google Scholar] [CrossRef]
- Grosen, A.; Kelsen, J.; Hvas, C.L.; Bellaguarda, E.; Hanauer, S.B. The Influence of Methotrexate Treatment on Male Fertility and Pregnancy Outcome After Paternal Exposure. Inflamm. Bowel Dis. 2017, 23, 561–569. [Google Scholar] [CrossRef]
- Mahadevan, U. Fertility and pregnancy in the patient with inflammatory bowel disease. Gut 2006, 55, 1198–1206. [Google Scholar] [CrossRef]
- Winter, R.W.; Larsen, M.D.; Magnussen, B.; Friedman, S.; Kammerlander, H.; Nørgård, B.M. Birth outcomes after preconception paternal exposure to methotrexate: A nationwide cohort study. Reprod. Toxicol. 2017, 74, 219–223. [Google Scholar] [CrossRef]
- Broe, A.; Damkier, P.; Pottegård, A.; Hallas, J.; Bliddal, M. Congenital Malformations in Denmark: Considerations for the Use of Danish Health Care Registries. Clin. Epidemiol. 2020, 12, 1371–1380. [Google Scholar] [CrossRef]
- Boyd, P.A.; Haeusler, M.; Barisic, I.; Loane, M.; Garne, E.; Dolk, H. Paper 1: The EUROCAT network-organization and processes. Birth Defects Res. Part A Clin. Mol. Teratol. 2011, 91 (Suppl. 1), S2–S15. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Galardo, M.N.; Riera, M.F.; Pellizzari, E.H.; Chemes, H.E.; Venara, M.C.; Cigorraga, S.B.; Meroni, S.B. Regulation of expression of Sertoli cell glucose transporters 1 and 3 by FSH, IL1β, and bFGF at two different time-points in pubertal development. Cell Tissue Res. 2008, 334, 295–304. [Google Scholar] [CrossRef]
- Oliveira, P.; Alves, M.; Rato, L.; Laurentino, S.; Silva, J.; Sá, R.; Barros, A.; Sousa, M.; Carvalho, R.; Cavaco, J.; et al. Effect of insulin deprivation on metabolism and metabolism-associated gene transcript levels of in vitro cultured human Sertoli cells. Biochim. Biophys. Acta (BBA) Gen. Subj. 2012, 1820, 84–89. [Google Scholar] [CrossRef]
- Halestrap, A.P.; Price, N.T. The proton-linked monocarboxylate transporter (MCT) family: Structure, function and regulation. Biochem. J. 1999, 343 Pt 2, 281–299. [Google Scholar] [CrossRef] [PubMed]
- Bridgeman, S.C.; Ellison, G.C.; Melton, P.E.; Newsholme, P.; Mamotte, C.D.S. Epigenetic effects of metformin: From molecular mechanisms to clinical implications. Diabetes Obes. Metab. 2018, 20, 1553–1562. [Google Scholar] [CrossRef] [PubMed]

| Children Fathered by Men Treated with Insulin (ATC A10A) N = 5527 | Children Fathered by Men Treated with Non-Insulin Anti-Hyperglycemic Agents (ATC A10B) N = 2121 | Children Fathered by Men Not Treated with Insulin or Antidiabetics N = 1,311,036 | |
|---|---|---|---|
| Paternal age at child birth, years (n, %) | |||
| −30 | 1585 (28.7) | 103 (4.9) | 400,628 (30.6) |
| 31–40 | 3277 (59.3) | 859 (40.5) | 762,768 (58.2) |
| 41– | 665 (12.0) | 1159 (54.6) | 147,640 (11.3) |
| Paternal Charlson’s comorbidity index (n, %) | |||
| 0 | 5042 (91.2) | 1756 (82.8) | 1,230,252 (93.8) |
| >=1 | 485 (8.8) | 365 (17.2) | 80,784 (6.2) |
| Maternal use of antidiabetics (n, %) | |||
| No | 5437 (98.4) | 2029 (95.7) | 1,296,172 (98.9) |
| Yes | 90 (1.6) | 92 (4.3) | 14,864 (1.1) |
| Maternal age at child birth, years (n, %) | |||
| −30 | 2604 (47.1) | 512 (24.1) | 612,733 (46.7) |
| 31–40 | 2760 (49.9) | 1328 (62.6) | 662,754 (50.6) |
| 41– | 163 (2.9) | 281 (13.2) | 35,549 (2.7) |
| Maternal Charlson’s comorbidity (n, %) | |||
| 0 | 5130 (92.8) | 1963 (92.6) | 1,227,353 (93.6) |
| >=1 | 397 (7.2) | 158 (7.4) | 83,683 (6.4) |
| Maternal smoking (n, %) | |||
| No | 4288 (77.6) | 1778 (83.8) | 1,002,296 (76.5) |
| Yes | 831 (15.0) | 239 (11.3) | 180,175 (13.7) |
| Missing | 408 (7.4) | 104 (4.9) | 128,565 (9.8) |
| Maternal BMI a (n, %) | |||
| <18.5 | 155 (2.8) | 48 (2.3) | 37,420 (2.9) |
| 18.5–24.9 | 2144 (38.8) | 621 (29.3) | 513,929 (39.2) |
| >=25 | 1367 (24.7) | 1028 (48.5) | 276,856 (21.1) |
| Missing | 1861 (33.7) | 424 (20.0) | 482,831 (36.8) |
| Parity (n, %) | |||
| First child | 2433 (44.0) | 582 (27.4) | 570,606 (43.5) |
| Second or more | 3028 (54.8) | 1524 (71.9) | 705,333 (53.8) |
| Missing | 66 (1.2) | 15 (0.7) | 35,097 (2.7) |
| Child sex (n, %) | |||
| Girl | 2682 (48.5) | 1032 (48.7) | 638,060 (48.7) |
| Boy | 2845 (51.5) | 1089 (51.3) | 672,976 (51.3) |
| Calendar year of birth (n, %) | |||
| 1997–2002 | 1512 (27.4) | 300 (14.1) | 377,636 (28.8) |
| 2003–2008 | 1594 (28.8) | 507 (23.9) | 367,847 (28.1) |
| 2009–2014 | 1469 (26.6) | 726 (34.2) | 336,183 (25.6) |
| 2015–2018 | 952 (17.2) | 588 (27.7) | 229,370 (17.5) |
| Type of non-insulin anti-hyperglycemic agents b (n, %) | |||
| Metformin | 1617 (76.2) | ||
| Sulfonylureas | 664 (31.3) | ||
| Others | 327 (15.4) | ||
| Father’s use of methotrexate prior to conception (n, %) | 2 (0.0) | 1 (0.0) | 241 (0.0) |
| Mother’s exposure to known teratogens c (n, %) | 39 (0.7) | 14 (0.7) | 4053 (0.3) |
| Children Fathered by Men Treated with Insulin within Three Months before Conception | Children Fathered by Men Not Treated with Insulin or Non-Insulin Anti-Hyperglycemic Agents within Three Months before Conception | ||||||
|---|---|---|---|---|---|---|---|
| Events (%) | N | Events (%) | N | Crude OR (95% CI) | Adjusted OR a (95% CI) | Adjusted OR b (95% CI) | |
| BIRTH OUTCOMES | |||||||
| Preterm birth | 299 (5.4) | 5527 | 65,050 (5.0) | 1,311,036 | 1.10 (0.97–1.23) | 1.06 (0.94–1.19) | 1.10 (0.95–1.27) |
| SGA | 164 (3.0) | 5512 | 47,770 (3.7) | 1,287,707 | 0.80 (0.68–0.93) | 0.83 (0.71–0.97) | 0.96 (0.78–1.18) |
| Events/total time at risk (years) | N | Events/total time at risk (years) | N | Crude HR (95% CI) | Adjusted HR a (95% CI) | Adjusted HR b (95% CI) | |
| EARLY CHILD OUTCOMES (FIRST YEAR OF LIFE) | |||||||
| Major congenital malformations | 189/5316 | 5486 | 46,692/ 1,261,546 | 1,306,743 | 0.96 (0.83–1.11) | 0.94 (0.81–1.09) | 0.97 (0.82–1.15) |
| Infections | |||||||
| Overall infections | 767/5132 | 5527 | 179,618/ 1,214,168 | 1,311,036 | 1.01 (0.94–1.08) | 1.00 (0.93–1.07) | 0.99 (0.91–1.08) |
| Respiratory | 443/5301 | 5527 | 96,765/ 1,256,729 | 1,311,036 | 1.09 (0.99–1.19) | 1.07 (0.97–1.17) | 1.05 (0.94–1.17) |
| Gastrointestinal | 125/5462 | 5527 | 32,017/ 1,290,404 | 1,311,036 | 0.92 (0.77–1.10) | 0.91 (0.76–1.09) | 0.94 (0.77–1.15) |
| Urological/gynecological | 29/5497 | 5527 | 6644/ 1,300,267 | 1,311,036 | 1.03 (0.72–1.49) | 1.03 (0.72–1.48) | 1.02 (0.67–1.55) |
| Skin/subcutaneous tissue | 0/5514 | 5527 | 121/ 1,304,014 | 1,311,036 | |||
| Bacteremia | 11/5504 | 5527 | 2372/ 1,302,387 | 1,311,036 | 1.10 (0.61–1.99) | 1.09 (0.60–1.98) | 1.32 (0.71–2.46) |
| Other infections | 305/5370 | 5527 | 74,234/ 1,268,781 | 1,311,036 | 0.97 (0.87–1.09) | 0.96 (0.86–1.08) | 0.93 (0.81–1.06) |
| Children Fathered by Men Treated with Non-Insulin Anti-Hyperglycemic Agents within Three Months before Conception | Children Fathered by Men Not Treated with Insulin or Non-Insulin Anti-Hyperglycemic Agents within Three Months before Conception | ||||||
|---|---|---|---|---|---|---|---|
| Events (%) | N | Events (%) | N | Crude OR (95% CI) | Adjusted OR a (95% CI) | Adjusted OR b (95% CI) | |
| BIRTH OUTCOMES | |||||||
| Preterm birth | |||||||
| Metformin | 97 (6.0) | 1617 | 65,080 (5.0) | 1,311,540 | 1.22 (1.00–1.50) | 1.08 (0.86–1.35) | 1.07 (0.84–1.37) |
| Sulfonylureas | 43 (6.5) | 664 | 65,134 (5.0) | 1,312,493 | 1.33 (0.97–1.81) | 1.21 (0.87–1.67) | 1.20 (0.79–1.83) |
| Other | 19 (5.8) | 327 | 65,158 (5.0) | 1,312,830 | 1.18 (0.74–1.88) | 1.01 (0.61–1.65) | 1.10 (0.65–1.85) |
| SGA | |||||||
| Metformin | 71 (4.4) | 1613 | 47,794 (3.7) | 1,288,208 | 1.20 (0.94–1.52) | 1.17 (0.90–1.52) | 1.36 (0.99–1.86) |
| Sulfonylureas | 38 (5.8) | 660 | 47,827 (3.7) | 1,289,161 | 1.59 (1.14–2.20) | 1.52 (1.06–2.18) | 1.80 (1.11–2.93) |
| Other | 14 (4.3) | 326 | 47,851 (3.7) | 1,289,495 | 1.16 (0.68–1.99) | 1.05 (0.60–1.83) | 0.91 (0.45–1.83) |
| Events/total time at risk (years) | N | Events/total time at risk (years) | N | Crude HR (95% CI) | Adjusted HR a (95% CI) | Adjusted HR b (95% CI) | |
| EARLY CHILD OUTCOMES (FIRST YEAR OF LIFE) | |||||||
| Major congenital malformations | |||||||
| Metformin | 92/1517 | 1603 | 46,704/1,262,036 | 1,307,246 | 1.62 (1.32–1.99) | 1.55 (1.25–1.92) | 1.40 (1.11–1.76) |
| Sulfonylureas | 30/632 | 663 | 46,766/1,262,921 | 1,308,186 | 1.27 (0.89–1.82) | 0.99 (0.68–1.43) | 1.24 (0.81–1.90) |
| Other | 14/310 | 325 | 46,782/1,263,243 | 1,308,524 | 1.21 (0.72–2.05) | 0.90 (0.53–1.52) | 0.98 (0.58–1.65) |
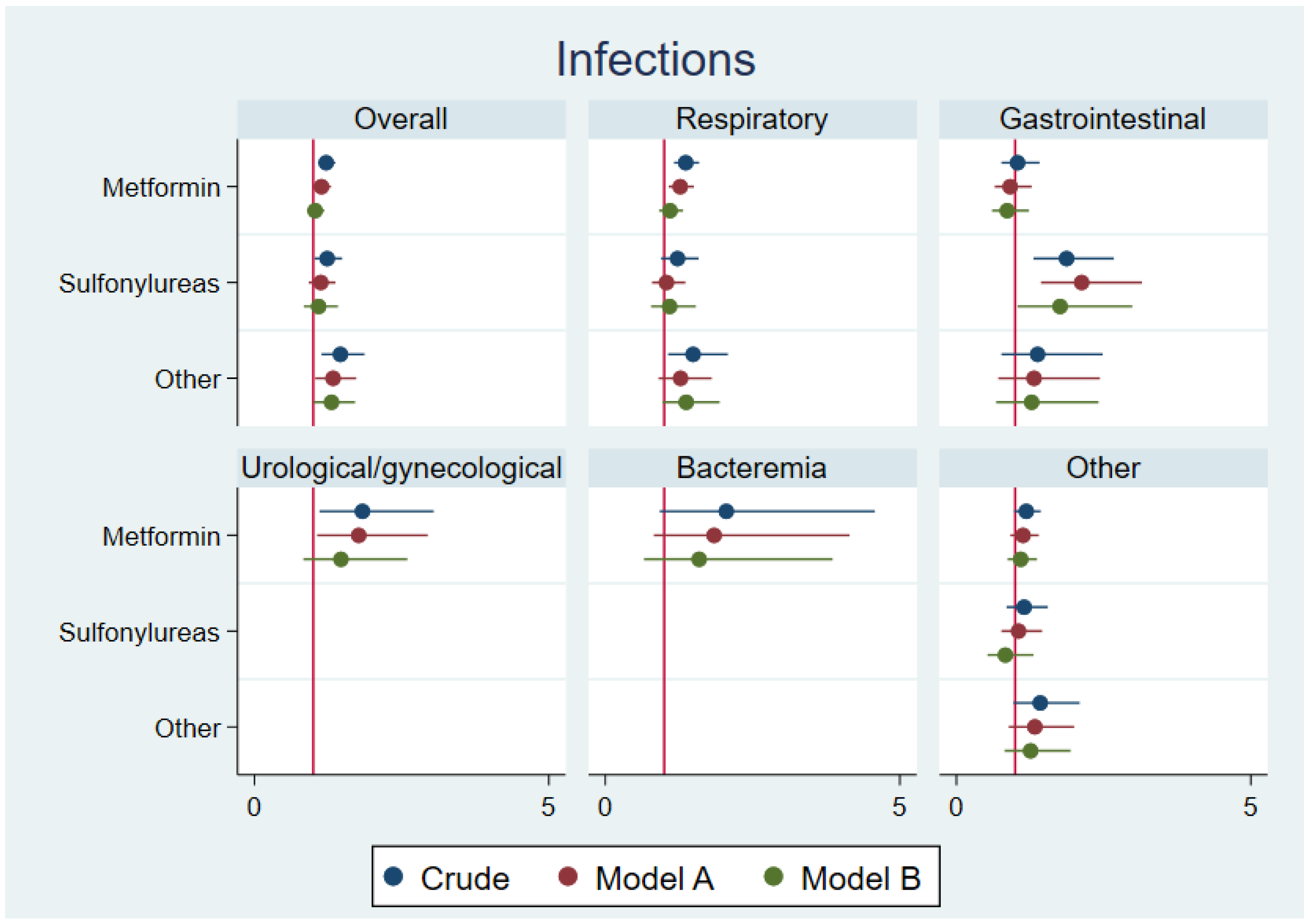
| Infections | |||||||
| Overall infections | |||||||
| Metformin | 264/1465 | 1617 | 179,703/1,214,628 | 1,311,540 | 1.22 (1.08–1.38) | 1.14 (1.00–1.30) | 1.03 (0.89–1.19) |
| Sulfonylureas | 110/602 | 664 | 179,857/1,215,491 | 1,312,493 | 1.24 (1.02–1.49) | 1.13 (0.92–1.38) | 1.09 (0.84–1.42) |
| Other | 63/291 | 327 | 179,904/1,215,801 | 1,312,830 | 1.46 (1.14–1.87) | 1.34 (1.03–1.73) | 1.31 (1.00–1.71) |
| Respiratory | |||||||
| Metformin | 160/1525 | 1617 | 96,805/1,257,209 | 1,311,540 | 1.36 (1.17–1.59) | 1.27 (1.07–1.50) | 1.10 (0.91–1.32) |
| Sulfonylureas | 59/626 | 664 | 96,906/1,258,109 | 1,312,493 | 1.22 (0.95–1.58) | 1.04 (0.79–1.36) | 1.09 (0.78–1.54) |
| Other | 35/305 | 327 | 96,930/1,258,429 | 1,312,830 | 1.49 (1.07–2.08) | 1.28 (0.90–1.81) | 1.37 (0.97–1.94) |
| Gastrointestinal | |||||||
| Metformin | 41/1590 | 1617 | 32,040/1,290,897 | 1,311,540 | 1.04 (0.76–1.41) | 0.91 (0.65–1.28) | 0.86 (0.60–1.23) |
| Sulfonylureas | 30/647 | 664 | 32,051/1,291,839 | 1,312,493 | 1.87 (1.31–2.67) | 2.13 (1.44–3.15) | 1.76 (1.04–2.99) |
| Other | 11/322 | 327 | 32,070/1,292,165 | 1,312,830 | 1.38 (0.76–2.48) | 1.32 (0.71–2.44) | 1.28 (0.68–2.42) |
| Urological/gynecological | |||||||
| Metformin | 15/1601 | 1617 | 6644/1,300,768 | 1,311,540 | 1.83 (1.11–3.04) | 1.77 (1.06–2.95) | 1.47 (0.83–2.60) |
| Sulfonylureas c | 2/657 | 664 | 6657/1,301,712 | 1,312,493 | |||
| Other c | 1/325 | 327 | 6658/1,302,044 | 1,312,830 | |||
| Skin/subcutaneous tissue | |||||||
| Metformin c | 1/1609 | 1617 | 121/1,304,515 | 1,311,540 | |||
| Sulfonylureas c | 0/659 | 664 | 122/1,305,466 | 1,312,493 | |||
| Other c | 0/325 | 327 | 122/1,305,799 | 1,312,830 | |||
| Bacteremia | |||||||
| Metformin | 6/1604 | 1617 | 2374/1,302,888 | 1,311,540 | 2.05 (0.92–4.58) | 1.85 (0.82–4.15) | 1.59 (0.66–3.86) |
| Sulfonylureas c | 2/658 | 664 | 2378/1,303,834 | 1,312,493 | |||
| Other c | 1/325 | 327 | 2379/1,304,166 | 1,312,830 | |||
| Other infections | |||||||
| Metformin | 108/1555 | 1617 | 74,272/1,269,264 | 1,311,540 | 1.19 (0.98–1.43) | 1.13 (0.91–1.40) | 1.09 (0.87–1.37) |
| Sulfonylureas | 43/639 | 664 | 74,337/1,270,180 | 1,312,493 | 1.15 (0.85–1.55) | 1.06 (0.76–1.46) | 0.83 (0.53–1.31) |
| Other | 26/312 | 327 | 74,354/1,270,507 | 1,312,830 | 1.42 (0.97–2.09) | 1.33 (0.89–2.00) | 1.26 (0.82–1.94) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nørgård, B.M.; Fedder, J.; Jølving, L.R.; Damkier, P.; Nielsen, J. Adverse Birth and Child Outcomes in Children Fathered by Men Treated with Antidiabetics Prior to Conception: A Nationwide Cohort Study. J. Clin. Med. 2022, 11, 6595. https://doi.org/10.3390/jcm11216595
Nørgård BM, Fedder J, Jølving LR, Damkier P, Nielsen J. Adverse Birth and Child Outcomes in Children Fathered by Men Treated with Antidiabetics Prior to Conception: A Nationwide Cohort Study. Journal of Clinical Medicine. 2022; 11(21):6595. https://doi.org/10.3390/jcm11216595
Chicago/Turabian StyleNørgård, Bente Mertz, Jens Fedder, Line Riis Jølving, Per Damkier, and Jan Nielsen. 2022. "Adverse Birth and Child Outcomes in Children Fathered by Men Treated with Antidiabetics Prior to Conception: A Nationwide Cohort Study" Journal of Clinical Medicine 11, no. 21: 6595. https://doi.org/10.3390/jcm11216595
APA StyleNørgård, B. M., Fedder, J., Jølving, L. R., Damkier, P., & Nielsen, J. (2022). Adverse Birth and Child Outcomes in Children Fathered by Men Treated with Antidiabetics Prior to Conception: A Nationwide Cohort Study. Journal of Clinical Medicine, 11(21), 6595. https://doi.org/10.3390/jcm11216595








