No Significant Differences in Clinical and Radiographic Outcomes between PCL Retained or Sacrificed Kinematic Aligned Medial Pivot Total Knee Arthroplasty in Varus Knee
Abstract
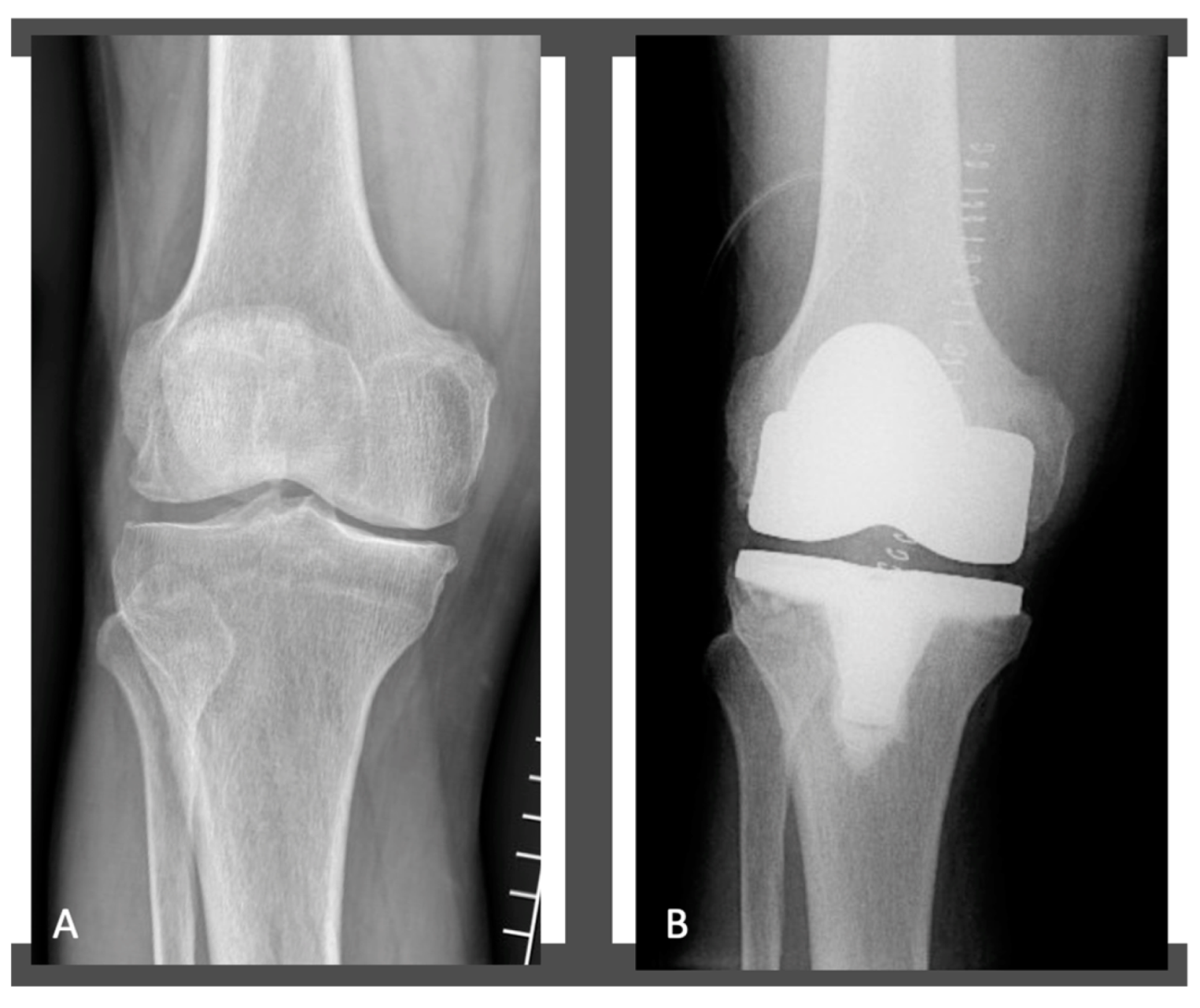
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Radiological Evaluation
2.3. Surgical Technique
2.4. Postoperative Rehabilitation Protocol
2.5. PROMs
2.6. Data Extraction
2.7. Statistical Analysis
3. Results
3.1. Preoperative Demographic and Clinical Data
3.2. Preoperative and Postoperative Radiographic Measurements
3.3. Preoperative and Postoperative Clinical Outcomes
3.4. Complications and Survivorship
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maradit Kremers, H.; Larson, D.R.; Crowson, C.S.; Kremers, W.K.; Washington, R.E.; Steiner, C.A.; Jiranek, W.A.; Berry, D.J. Prevalence of Total Hip and Knee Replacement in the United States. J. Bone Joint. Surg. Am. 2015, 97, 1386–1397. [Google Scholar] [CrossRef] [PubMed]
- Manderbacka, K.; Satokangas, M.; Arffman, M.; Reissell, E.; Keskimäki, I.; Leyland, A.H. Explaining regional variation in elective hip and knee arthroplasties in Finland 2010–2017-a register-based cohort study. BMC Health Serv. Res. 2022, 22, 891. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Cieremans, D.; Slover, J.; Schwarzkopf, R.; Meftah, M. Trends in Complications and Outcomes in Patients Aged 65 Years and Younger Undergoing Total Knee Arthroplasty: Data from the American Joint Replacement Registry. J. Am. Acad. Orthop. Surg Glob. Res. Rev. 2022, 6, e22.00116. [Google Scholar] [CrossRef] [PubMed]
- Lewis, P.L.; W-Dahl, A.; Robertsson, O.; Prentice, H.A.; Graves, S.E. Impact of patient and prosthesis characteristics on common reasons for total knee replacement revision: A registry study of 36,626 revision cases from Australia, Sweden, and USA. Acta Orthop. 2022, 93, 623–633. [Google Scholar] [CrossRef]
- Gunaratne, R.; Pratt, D.N.; Banda, J.; Fick, D.P.; Khan, R.; Robertson, B.W. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J. Arthroplast. 2017, 32, 3854–3860. [Google Scholar] [CrossRef] [PubMed]
- Shohat, N.; Heller, S.; Sudya, D.; Small, I.; Khawalde, K.; Khatib, M.; Yassin, M. Mild radiographic osteoarthritis is associated with increased pain and dissatisfaction following total knee arthroplasty when compared with severe osteoarthritis: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 965–981. [Google Scholar] [CrossRef]
- Sabatini, L.; Bosco, F.; Barberis, L.; Camazzola, D.; Bistolfi, A.; Risitano, S.; Massè, A.; Indelli, P.F. Kinetic Sensors for Ligament Balance and Kinematic Evaluation in Anatomic Bi-Cruciate Stabilized Total Knee Arthroplasty. Sensors 2021, 21, 5427. [Google Scholar] [CrossRef]
- Bistolfi, A.; Giustra, F.; Bosco, F.; Faccenda, C.; Viotto, M.; Sabatini, L.; Berchialla, P.; Sciannameo, V.; Graziano, E.; Massè, A. Comparable results between crosslinked polyethylene and conventional ultra-high molecular weight polyethylene implanted in total knee arthroplasty: Systematic review and meta-analysis of randomised clinical trials. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 3120–3130. [Google Scholar] [CrossRef]
- Bistolfi, A.; Giustra, F.; Bosco, F.; Sabatini, L.; Aprato, A.; Bracco, P.; Bellare, A. Ultra-high molecular weight polyethylene (UHMWPE) for hip and knee arthroplasty: The present and the future. J. Orthop. 2021, 25, 98–106. [Google Scholar] [CrossRef]
- Magan, A.A.; Kayani, B.; Chang, J.S.; Roussot, M.; Moriarty, P.; Haddad, F.S. Artificial intelligence and surgical innovation: Lower limb arthroplasty. Br. J. Hosp. Med. 2020, 81, 1–7. [Google Scholar] [CrossRef]
- Rivière, C.; Jackson, W.; Villet, L.; Sivaloganathan, S.; Barziv, Y.; Vendittoli, P.A. Specific case consideration for implanting TKA with the Kinematic Alignment technique. EFORT Open Rev. 2021, 6, 881–891. [Google Scholar] [CrossRef] [PubMed]
- Koh, Y.G.; Park, K.M.; Kang, K.T. Finite Element Study on the Preservation of Normal Knee Kinematics with Respect to the Prosthetic Design in Patient-Specific Medial Unicompartmental Knee Arthroplasty. Biomed. Res. Int. 2020, 2020, 1829385. [Google Scholar] [CrossRef] [PubMed]
- Pinskerova, V.; Samuelson, K.M.; Stammers, J.; Maruthainar, K.; Sosna, A.; Freeman, M.A. The knee in full flexion: An anatomical study. J. Bone Jt. Surg. Br. 2009, 91, 830–834. [Google Scholar] [CrossRef] [PubMed]
- Gray, H.A.; Guan, S.; Young, T.J.; Dowsey, M.M.; Choong, P.F.; Pandy, M.G. Comparison of posterior-stabilized, cruciate-retaining, and medial-stabilized knee implant motion during gait. J. Orthop. Res. 2020, 38, 1753–1768. [Google Scholar] [CrossRef]
- Murakami, K.; Hamai, S.; Okazaki, K.; Ikebe, S.; Nakahara, H.; Higaki, H.; Shimoto, T.; Mizu-Uchi, H.; Kuwashima, U.; Iwamoto, Y. Kinematic analysis of stair climbing in rotating platform cruciate-retaining and posterior-stabilized mobile-bearing total knee arthroplasties. Arch. Orthop. Trauma Surg. 2017, 137, 701–711. [Google Scholar] [CrossRef]
- Cacciola, G.; Mancino, F.; De Meo, F.; Di Matteo, V.; Sculco, P.K.; Cavaliere, P.; Maccauro, G.; De Martino, I. Mid-term survivorship and clinical outcomes of the medial stabilized systems in primary total knee arthroplasty: A systematic review. J. Orthop. 2021, 24, 157–164. [Google Scholar] [CrossRef]
- Cacciola, G.; De Martino, I.; De Meo, F. Does the medial pivot knee improve the clinical and radiographic outcome of total knee arthroplasty? A single centre study on two hundred and ninety seven patients. Int. Orthop. 2020, 44, 291–299. [Google Scholar] [CrossRef]
- Sabatini, L.; Risitano, S.; Parisi, G.; Tosto, F.; Indelli, P.F.; Atzori, F.; Massè, A. Medial Pivot in Total Knee Arthroplasty: Literature Review and Our First Experience. Clin. Med. Insights Arthritis Musculoskelet. Disord. 2018, 11, 1179544117751431. [Google Scholar] [CrossRef]
- Hollister, A.M.; Jatana, S.; Singh, A.K.; Sullivan, W.W.; Lupichuk, A.G. The axes of rotation of the knee. Clin. Orthop. Relat. Res. 1993, 290, 259–268. [Google Scholar] [CrossRef]
- Coughlin, K.M.; Incavo, S.J.; Churchill, D.L.; Beynnon, B.D. Tibial axis and patellar position relative to the femoral epicondylar axis during squatting. J. Arthroplast. 2003, 18, 1048–1055. [Google Scholar] [CrossRef]
- Howell, S.M.; Shelton, T.J.; Hull, M.L. Implant Survival and Function Ten Years After Kinematically Aligned Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 3678–3684. [Google Scholar] [CrossRef] [PubMed]
- Risitano, S.; Cacciola, G.; Sabatini, L.; Capella, M.; Bosco, F.; Giustra, F.; Massè, A.; Vaishya, R. Restricted kinematic alignment in primary total knee arthroplasty: A systematic review of radiographic and clinical data. J. Orthop. 2022, 33, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, N.V.; Deshpande, A.N.; Panjwani, T.; Patil, R.; Jaysingani, T.; Patil, P. Robotic-assisted TKA leads to a better prosthesis alignment and a better joint line restoration as compared to conventional TKA: A prospective randomized controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 621–626. [Google Scholar] [CrossRef] [PubMed]
- Hiyama, S.; Takahashi, T.; Takeshita, K. Kinematically Aligned Total Knee Arthroplasty Did Not Show Superior Patient-Reported Outcome Measures: An Updated Meta-analysis of Randomized Controlled Trials with at Least 2-Year Follow-up. J. Knee Surg. 2022, 35, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Minoda, Y.; Sakawa, A.; Aihara, M.; Tada, K.; Kadoya, Y.; Kobayashi, A. Flexion gap preparation opens the extension gap in posterior cruciate ligament-retaining TKA. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 1321–1325. [Google Scholar] [CrossRef]
- Vermue, H.; Winnock de Grave, P.; Ryckaert, A.; Luyckx, T. Equal bony resection of distal and posterior femur will lead to flexion/extension gap inequality in robot-assisted cruciate-retaining TKA. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2617–2623. [Google Scholar] [CrossRef]
- Logterman, S.L.; Wydra, F.B.; Frank, R.M. Posterior Cruciate Ligament: Anatomy and Biomechanics. Curr. Rev. Musculoskelet. Med. 2018, 11, 510–514. [Google Scholar] [CrossRef]
- Pache, S.; Aman, Z.S.; Kennedy, M.; Nakama, G.Y.; Moatshe, G.; Ziegler, C.; LaPrade, R.F. Posterior Cruciate Ligament: Current Concepts Review. Arch. Bone Jt. Surg. 2018, 6, 8–18. [Google Scholar]
- Park, S.J.; Seon, J.K.; Park, J.K.; Song, E.K. Effect of PCL on flexion-extension gaps and femoral component decision in TKA. Orthopedics 2009, 32 (Suppl. 10), 22–25. [Google Scholar] [CrossRef]
- Kayani, B.; Konan, S.; Horriat, S.; Ibrahim, M.S.; Haddad, F.S. Posterior cruciate ligament resection in total knee arthroplasty: The effect on flexion-extension gaps, mediolateral laxity, and fixed flexion deformity. Bone Jt. J. 2019, 101-B, 1230–1237. [Google Scholar] [CrossRef]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016, 474, 1886–1893. [Google Scholar] [CrossRef] [PubMed]
- Marques Luís, N.; Varatojo, R. Radiological assessment of lower limb alignment. EFORT Open Rev. 2021, 6, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Meneghini, R.M.; Mont, M.A.; Backstein, D.B.; Bourne, R.B.; Dennis, D.A.; Scuderi, G.R. Development of a Modern Knee Society Radiographic Evaluation System and Methodology for Total Knee Arthroplasty. J. Arthroplast. 2015, 30, 2311–2314. [Google Scholar] [CrossRef] [PubMed]
- Bravi, M.; Santacaterina, F.; Bressi, F.; Papalia, R.; Campi, S.; Sterzi, S.; Miccinilli, S. Does Posterior Cruciate Ligament Retention or Sacrifice in Total Knee Replacement Affect Proprioception? A Systematic Review. J. Clin. Med. 2021, 10, 3470. [Google Scholar] [CrossRef] [PubMed]
- Nedopil, A.J.; Howell, S.M.; Hull, M.L. More passive internal tibial rotation with posterior cruciate ligament retention than with excision in a medial pivot TKA implanted with unrestricted caliper verified kinematic alignment. Knee Surg. Sports Traumatol. Arthrosc. 2021. [Google Scholar] [CrossRef]
- Howell, S.M.; Shelton, T.J.; Gill, M.; Hull, M.L. A cruciate-retaining implant can treat both knees of most windswept deformities when performed with calipered kinematically aligned TKA. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 437–445. [Google Scholar] [CrossRef]
- Shelton, T.J.; Gill, M.; Athwal, G.; Howell, S.M.; Hull, M.L. Outcomes in Patients with a Calipered Kinematically Aligned TKA That Already Had a Contralateral Mechanically Aligned TKA. J. Knee Surg. 2021, 34, 87–93. [Google Scholar] [CrossRef]
- Howell, S.M. Calipered Kinematically Aligned Total Knee Arthroplasty: An Accurate Technique That Improves Patient Outcomes and Implant Survival. Orthopedics 2019, 42, 126–135. [Google Scholar] [CrossRef]
- Nedopil, A.J.; Delman, C.; Howell, S.M.; Hull, M.L. Restoring the Patient’s Pre-Arthritic Posterior Slope Is the Correct Target for Maximizing Internal Tibial Rotation When Implanting a PCL Retaining TKA with Calipered Kinematic Alignment. J. Pers. Med. 2021, 11, 516. [Google Scholar] [CrossRef]
- Scuderi, G.R.; Bourne, R.B.; Noble, P.C.; Benjamin, J.B.; Lonner, J.H.; Scott, W.N. The new Knee Society Knee Scoring System. Clin. Orthop. Relat. Res. 2012, 470, 3–19. [Google Scholar] [CrossRef]
- Lee, Q.J.; Chang, W.; Wong, Y.C. Forgotten Joint Score for early outcome assessment after total knee arthroplasty: Is it really useful? Knee Surg. Relat. Res. 2020, 32, 37. [Google Scholar] [CrossRef] [PubMed]
- Delgado, D.A.; Lambert, B.S.; Boutris, N.; McCulloch, P.C.; Robbins, A.B.; Moreno, M.R.; Harris, J.D. Validation of Digital Visual Analog Scale Pain Scoring with a Traditional Paper-based Visual Analog Scale in Adults. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e088. [Google Scholar] [CrossRef] [PubMed]
- Thippanna, R.K.; Mahesh, P.; Kumar, M.N. PCL-retaining versus PCL-substituting TKR-Outcome assessment based on the “forgotten joint score”. J. Clin. Orthop. Trauma. 2015, 6, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Bieganowski, T.; Fiedler, B.; Singh, V.; Karlin, E.; Anil, U.; Rozell, J.C.; Schwarzkopf, R. Does Retention of the Posterior Cruciate Ligament Lead to a More “Forgotten Joint” Following Total Knee Arthroplasty? Surg. Technol. Int. 2022, 40, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Stronach, B.M.; Adams, J.C.; Jones, L.C.; Farrell, S.M.; Hydrick, J.M. The Effect of Sacrificing the Posterior Cruciate Ligament in Total Knee Arthroplasties That Use a Highly Congruent Polyethylene Component. J. Arthroplast. 2019, 34, 286–289. [Google Scholar] [CrossRef] [PubMed]


| Parameters | Total Knees | PCL Preservation Group | PCL Sacrifice Group | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N° (%) | Mean | SD | N° (%) | Mean | SD | N° (%) | Mean | SD | ||
| Total patients | 64 (100%) | 35 (54.7%) | 29 (45.3%) | |||||||
| Women | 37 (57.8%) | 21 (56.8%) | 16 (43.2%) | 0.697 | ||||||
| Age (years) | 73.4 | 8.2 | 72.8 | 9.1 | 74.1 | 7.9 | 0.787 | |||
| BMI (Kg/m2) | 26.4 | 4.4 | 25.9 | 3.9 | 26.7 | 4.6 | 0.656 | |||
| KSS knee Score | 40.3 | 11,2 | 41.1 | 10.8 | 39.9 | 11.4 | 0.766 | |||
| KSS function Score | 38.5 | 9.9 | 39.9 | 10.4 | 37.5 | 9.2 | 0.645 | |||
| Measurements | Preoperative | Postoperative | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Knees | PCL Preservation Group | PCL Sacrifice Group | p Value | Total Knees | PCL Preservation Group | PCL Sacrifice Group | p Value | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| HKA | 174.4° | 4.4° | 173.9° | 3.9° | 174.7° | 4.5° | 0.565 | 176.2° | 3.9° | 175.9° | 3.8° | 177° | 3.4° | 0.772 |
| MPTA | 86.6° | 3.6° | 86.8° | 3.7° | 85.8° | 3.9° | 0.772 | 86.3° | 3.4° | 85.8° | 3.2° | 86.6° | 3.6° | 0.564 |
| LDFA | 88.4° | 3.3° | 88.2° | 3.6° | 88.7° | 3.5° | 0.688 | 87.3° | 2.2° | 87.1° | 2.5° | 87.5° | 2.1° | 0.423 |
| PTS | 7.7° | 4.9° | 7.3° | 4.7° | 7.9° | 5.1° | 0.881 | 5.4° | 4.1° | 5.2° | 3.8° | 5.7° | 4.2° | 0.776 |
| PROMs | Preoperative | Postoperative | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Knees | PCL Preservation Group | PCL Sacrifice Group | p Value | Total Knees | PCL Preservation Group | PCL Sacrifice Group | p Value | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| KSS knee score | 48.4 | 6.2 | 47.2 | 5.8 | 48.7 | 6.4 | 0.778 | 94.5 | 7.7 | 96.7 | 8.1 | 93.1 | 5.9 | 0.343 |
| KSS function score | 45.2 | 5.8 | 46.1 | 6.1 | 44.8 | 5.7 | 0.664 | 91.4 | 7.4 | 93.2 | 7.9 | 89.8 | 7.7 | 0.289 |
| FJS | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 60.3 | 18.4 | 63.3 | 19.8 | 59.7 | 18.1 | 0.051 |
| Active ROM | 114.5° | 11.3° | 113.8° | 10.8° | 115.2° | 11.5° | 0.667 | 118.7° | 11.7° | 116.4 | 11.8° | 125.4° | 12.1° | 0.074 |
| Q: Are You Aware of You Artificial Joint When? | PCL Preservation Group | PCL Sacrifice Group | p Value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| 1. In a bed at night | 2.48 | 2.55 | 0.331 |
| 2. Sitting in a chair > 1 h | 2.89 | 2.61 | 0.087 |
| 3. Walking for > 15 min | 2.65 | 2.78 | 0.303 |
| 4. Taking a bath/shower | 1.78 | 1.9 | 0.432 |
| 5. Travelling in a car | 2.44 | 2.71 | 0.087 |
| 6. Climbing stairs | 2.78 | 3.1 | 0.323 |
| 7. Walking on uneven ground | 2.5 | 3.1 | 0.045 |
| 8. Standing from low sitting position | 2.48 | 3.12 | 0.041 |
| 9. Standing for a long period of time | 2.88 | 2.92 | 0.512 |
| 10. Doing housework/gardening | 3.01 | 2.99 | 0.445 |
| 11. Taking a walk/hike | 2.77 | 3.02 | 0.061 |
| 12. Doing your favorite sport | 2.98 | 3.11 | 0.322 |
| Total Score | 59.5 ± 21.1 | 55.7 ± 19.3 | 0.064 |
| Patients with Complications | Age (Years) | Sex | PCL Preservation (Y/N) | Postoperative KSS Knee Score | Postoperative KSS Function Score | Postoperative FJS | Active ROM | Complications | Need to TKA Revision or Reoperation (Y/N) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 73 | F | Y | 88.2 | 86.4 | 58.1 | 93° | Extension deficit | N |
| 2 | 68 | M | Y | 89.5 | 87.1 | 55.4 | 94° | Flexion deficit | N |
| 3 | 76 | M | N | 92.1 | 89.8 | 59.4 | 96° | Extension deficit | N |
| 4 | 74 | F | N | 85.2 | 81.4 | 60.1 | 87° | Extension deficit | N |
| 5 | 77 | F | y | 79.1 | 76.4 | 55.1 | 91° | Flexion deficit | N |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giustra, F.; Bosco, F.; Cacciola, G.; Risitano, S.; Capella, M.; Bistolfi, A.; Massè, A.; Sabatini, L. No Significant Differences in Clinical and Radiographic Outcomes between PCL Retained or Sacrificed Kinematic Aligned Medial Pivot Total Knee Arthroplasty in Varus Knee. J. Clin. Med. 2022, 11, 6569. https://doi.org/10.3390/jcm11216569
Giustra F, Bosco F, Cacciola G, Risitano S, Capella M, Bistolfi A, Massè A, Sabatini L. No Significant Differences in Clinical and Radiographic Outcomes between PCL Retained or Sacrificed Kinematic Aligned Medial Pivot Total Knee Arthroplasty in Varus Knee. Journal of Clinical Medicine. 2022; 11(21):6569. https://doi.org/10.3390/jcm11216569
Chicago/Turabian StyleGiustra, Fortunato, Francesco Bosco, Giorgio Cacciola, Salvatore Risitano, Marcello Capella, Alessandro Bistolfi, Alessandro Massè, and Luigi Sabatini. 2022. "No Significant Differences in Clinical and Radiographic Outcomes between PCL Retained or Sacrificed Kinematic Aligned Medial Pivot Total Knee Arthroplasty in Varus Knee" Journal of Clinical Medicine 11, no. 21: 6569. https://doi.org/10.3390/jcm11216569
APA StyleGiustra, F., Bosco, F., Cacciola, G., Risitano, S., Capella, M., Bistolfi, A., Massè, A., & Sabatini, L. (2022). No Significant Differences in Clinical and Radiographic Outcomes between PCL Retained or Sacrificed Kinematic Aligned Medial Pivot Total Knee Arthroplasty in Varus Knee. Journal of Clinical Medicine, 11(21), 6569. https://doi.org/10.3390/jcm11216569







