The Challenge of High Coronary Thrombotic Events in Patients with ST-Segment Elevation Myocardial Infarction and COVID-19
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Population
2.2. Data Collection and Definitions
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Paraclinical Characteristics
3.2.1. Laboratory Findings
3.2.2. Echocardiographic and Procedural Characteristics
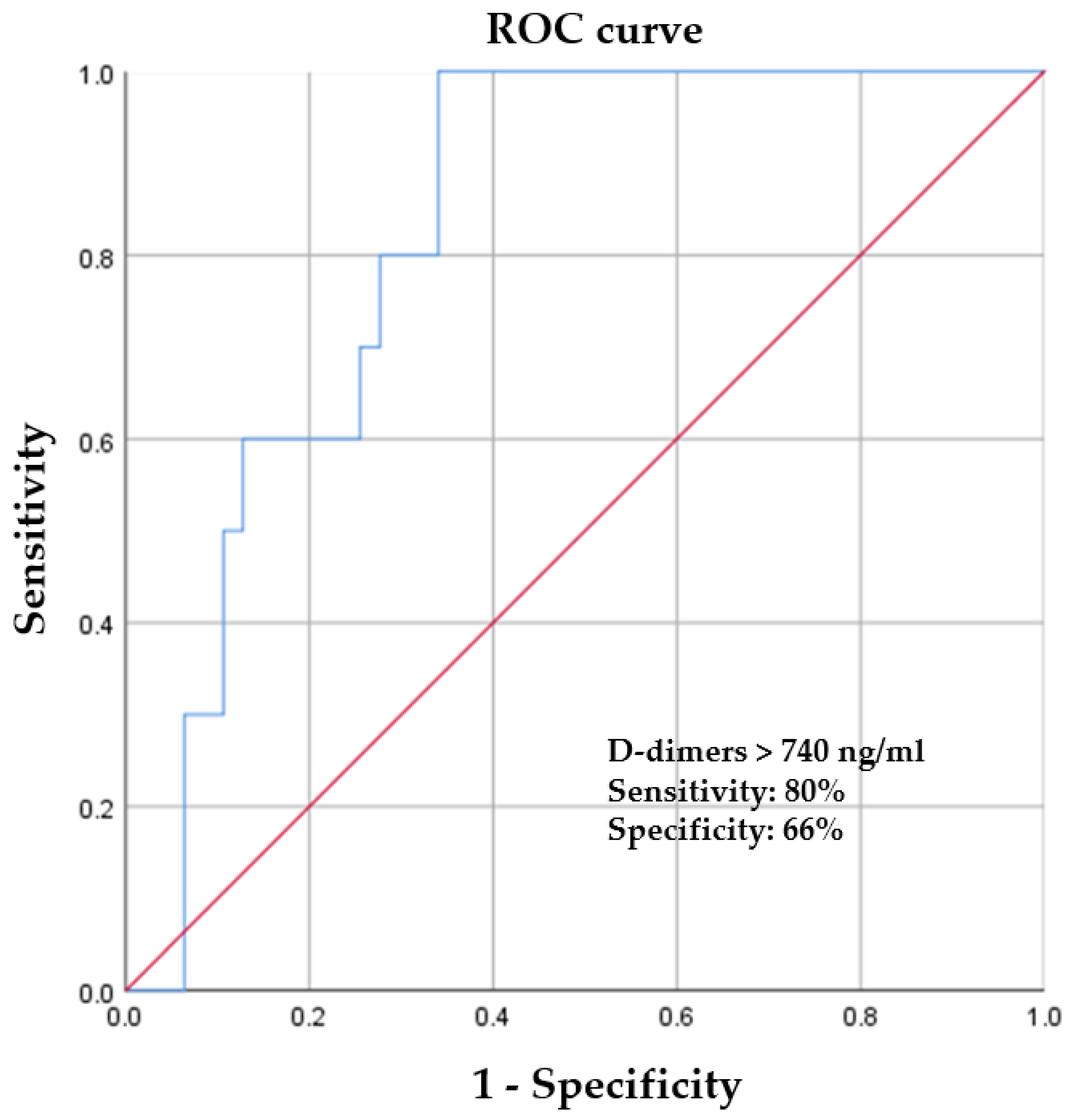
3.3. Correlations between Biological Markers and the Presence of Coronary Thrombosis in COVID-19-Positive Patients
3.4. In-Hospital Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Toscano, O.; Cosentino, N.; Campodonico, J.; Bartorelli, A.L.; Marenzi, G. Acute myocardial infarction during the COVID-19 pandemic: An update on clinical characteristics and outcomes. Front. Cardiovasc. Med. 2021, 8, 648290. [Google Scholar] [CrossRef]
- Choudry, F.A.; Hamshere, S.M.; Rathod, K.S.; Akhtar, M.M.; Archbold, R.A.; Guttman, O.P.; Woldman, S.; Jain, A.K.; Knight, J.C.; Baumbach, A.; et al. High thrombus burden in patients with Covid-19 presenting with ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 2020, 76, 1168–1176. [Google Scholar] [CrossRef]
- Levi, M.; Thachil, J.; Iba, T.; Levy, J.H. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020, 7, e438–e440. [Google Scholar] [CrossRef]
- Writing Committee Gluckman, T.J.; Bhave, N.M.; Allen, L.A.; Chung, E.H.; Spatz, E.S.; Ammirati, E.; Baggish, A.L.; Bozkurt, B.; Cornwell, W.K., III; Harmon, K.G. 2022 ACC Expert Consensus decision pathway on cardiovascular sequelae of COVID-19 in adults: Myocarditis and other myocardial involvement, post-acute sequelae of SARS-CoV-2 infection, and return to play. J. Am. Coll. Cardiol. 2022, 79, 1717–1756. [Google Scholar] [CrossRef] [PubMed]
- Thakker, R.A.; Elbadawi, A.; Chatila, K.F.; Goel, S.S.; Reynoso, D.; Berbarie, R.F.; Gilani, S.; Rangasetty, U.; Khalife, W. Comparison of coronary artery involvement and mortality in STEMI patients with and without SARS-CoV-2 during the COVID-19 pandemic: A systematic review and meta-analysis. Curr. Probl. Cardiol. 2022, 47, 101032. [Google Scholar] [CrossRef]
- Schiavone, M.; Gobbi, C.; Biondi-Zoccai, G.; D’Ascenzo, F.; Palazzuoli, A.; Gasperetti, A.; Mittacchione, G.; Viecca, M.; Galli, M.; Fedele, F.; et al. Acute coronary syndromes and Covid-19: Exploring the uncertainties. J. Clin. Med. 2020, 9, 1683. [Google Scholar] [CrossRef]
- Canzano, P.; Brambilla, M.; Porro, B.; Cosentino, N.; Tortorici, E.; Vicini, S.; Poggio, P.; Cascella, A.; Pengo, M.F.; Veglia, F.; et al. Platelet and endothelial activation as potential mechanism behind the thrombotic complications of COVID-19 patients. JACC Basic Transl. Sci. 2021, 6, 202–218. [Google Scholar] [CrossRef]
- Quagliariello, V.; Bonelli, A.; Caronna, A.; Conforti, G.; Iovine, M.; Carbone, A.; Berretta, M.; Botti, G.; Maurea, N. SARS-CoV-2 Infection and Cardioncology: From Cardiometabolic Risk Factors to Outcomes in Cancer Patients. Cancers 2020, 12, 3316. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, D.; Kawakami, R.; Guagliumi, G.; Sakamato, A.; Kawai, K.; Gianatii, A.; Nasr, A.; Kutys, R.; Guo, L.; Cornelissen, A.; et al. Microthrombi as a major cause of cardiac injury in COVID-19. Circulation 2021, 143, 1031–1042. [Google Scholar] [CrossRef]
- Garcia, S.; Dehghani, P.; Grines, C.; Davidson, L.; Nayak, K.R.; Saw, J.; Waksman, R.; Blair, J.; Akshay, B.; Garberich, R.; et al. Initial findings from The North American COVID-19 Myocardial Infarction Registry. J. Am. Coll. Cardiol. 2021, 77, 1994–2003. [Google Scholar] [CrossRef]
- Tokarek, T.; Dziewierz, A.; Malinowski, K.P.; Rakowski, T.; Bartuś, S.; Dudek, D.; Siudak, Z. Treatment delay and clinical outcomes in patients with ST-Segment Elevation Myocardial Infarction during the COVID-19 pandemic. J. Clin. Med. 2021, 10, 3920. [Google Scholar] [CrossRef] [PubMed]
- Budrys, P.; Lizaitis, M.; Cerlinskaite-Bajore, K.; Bajoras, V.; Rodevic, G.; Martinonyte, A.; Dieckus, L.; Badaras, I.; Serpytis, P.; Gurevicius, R.; et al. Increase of myocardial ischemia time and short-term prognosis of patients with acute myocardial infarction during the first COVID-19 pandemic wave. Medicina 2021, 57, 1296. [Google Scholar] [CrossRef] [PubMed]
- Ayad, S.; Shenouda, R.; Henein, M. The impact of COVID-19 on in-hospital outcomes of ST-Segment Elevation Myocardial Infarction Patients. J. Clin. Med. 2021, 10, 278. [Google Scholar] [CrossRef] [PubMed]
- Gluckman, T.J.; Wilson, M.A.; Chiu, S.T.; Penny, B.W.; Chepuri, V.B.; Waggoner, J.W.; Spinelli, K.J. Case rates, treatment approaches, and outcomes in acute myocardial infarction during Coronavirus disease 2019 pandemic. JAMA Cardiol. 2020, 5, 1419–1424. [Google Scholar] [CrossRef] [PubMed]
- Mesnier, J.; Cottin, Y.; Coste, P.; Ferrari, E.; Schiele, F.; Lemesle, G.; Thuaire, C.; Angoulvant, D.; Cayla, G.; Bouleti, C.; et al. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: A registry study. Lancet Public Health 2020, 5, e536–e542. [Google Scholar] [CrossRef]
- Solomon, M.D.; McNulty, E.J.; Rana, J.S.; Leong, T.K.; Lee, C.; Sung, S.H.; Ambrosy, A.P.; Sidney, S.; Go, A.S. The Covid-19 pandemic and the incidence of acute myocardial infarction. N. Engl. J. Med. 2020, 383, 691–693. [Google Scholar] [CrossRef]
- Primessnig, U.; Pieske, B.M.; Sherif, M. Increased mortality and worse cardiac outcome of acute myocardial infarction during the early COVID-19 pandemic: Insights from a regional public service healthcare hub. Circ. Cardiovasc. Interv. 2020, 13, e009413. [Google Scholar]
- Mohammad, M.A.; Koul, S.; Olivecrona, G.K.; Götberg, M.; Tydén, P.; Rydberg, E. Incidence and outcome of myocardial infarction treated with percutaneous coronary intervention during COVID-19 pandemic. Heart 2020, 106, 1812–1818. [Google Scholar] [CrossRef]
- Mafham, M.M.; Spata, E.; Goldacre, R.; Gair, D.; Curnow, P.; Bray, M. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 2020, 396, 381–389. [Google Scholar] [CrossRef]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabro, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef]
- Carugo, S.; Ferlini, M.; Castini, D.; Andreassi, A.; Guagliumi, G.; Metra, M.; Lombardi, C.; Cuccia, C.; Savonitto, S.; Piatti, L.; et al. Management of acute coronary syndromes during the COVID-19 outbreak in Lombardy: The “macro-hub” experience. Int. J. Cardiol. Heart Vasc. 2020, 31, 100662. [Google Scholar] [CrossRef] [PubMed]
- Cosentino, N.; Marenzi, G.; Bartorelli, A.L. Time to treatment still matters in ST-elevation myocardial infarction: A call to maintain treatment effectiveness during the COVID-19 pandemic. Eur. Heart J. Cardiovasc. Pharmacother. 2020, 6, 408–409. [Google Scholar] [CrossRef] [PubMed]
- Nallamothu, B.K.; Bradley, E.H.; Krumholz, H.M. Time to treatment in primary percutaneous coronary intervention. N. Engl. J. Med. 2007, 357, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Popovic, B.; Varlot, J.; Metzdorf, P.A.; Jeulin, H.; Goehringer, F.; Camenzind, E. Changes in characteristics and management among patients with ST-elevation myocardial infarction due to COVID-19 infection. Catheter. Cardiovasc. Interv. 2021, 97, E319–E326. [Google Scholar] [CrossRef]
- Chew, N.W.; Ow, Z.G.W.; Teo, V.X.Y.; Heng, R.R.Y.; Ng, C.H.; Lee, C.H.; Low, A.F.; Chan, M.Y.; Yeo, T.C.; Tan, H.C.; et al. The global impact of the COVID-19 pandemic on STEMI care: A systematic review and meta-analysis. Can. J. Cardiol. 2021, 37, 1450–1459. [Google Scholar] [CrossRef]
- Rattka, M.; Dreyhaupt, J.; Winsauer, C.; Stuhler, L.; Baumhardt, M.; Thiessen, K.; Rottbauer, W.; Imhof, A. Effect of the COVID-19 pandemic on mortality of patients with STEMI: A systematic review and meta-analysis. Heart 2020, 107, 482–487. [Google Scholar] [CrossRef]
- Tokarek, T.; Dziewierz, A.; Plens, K.; Rakowski, T.; Jaroszyńska, A.; Bartuś, S.; Siudak, Z. Percutaneous coronary intervention during on- and off-hours in patients with ST-segment elevation myocardial infarction. Hell. J. Cardiol. 2021, 62, 212–218. [Google Scholar] [CrossRef]
- Rangé, G.; Hakim, R.; Beygui, F.; Angoulvant, D.; Marcollet, P.; Godin, M.; Deballon, R.; Bonnet, P.; Fichaux, O.; Barbey, C.; et al. Incidence, delays, and outcomes of STEMI during COVID-19 outbreak: Analysis from the France PCI registry. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1168–1176. [Google Scholar] [CrossRef]
- Bruoha, S.; Yosefy, C.; Gallego-Colon, E.; Rieck, J.; Orlov, Y.; Osherov, A.; Jihad, A.H.; Sherer, Y.; Viki, N.; Jafari, J. Impact in total ischemic time and ST-segment elevation myocardial infarction admissions during COVID-19. Am. J. Emerg. Med. 2021, 45, 7–10. [Google Scholar] [CrossRef]
- Rodriguez-Leor, O.; Cid Alvarez, A.B.; de Prado, P.A.; Rossello, X.; Ojeda, S.; Serrador, A.; López-Palop, R.; Martin-Moreiras, J.; Rumoroso, J.R.; Cequier, A.; et al. In-hospital outcomes of COVID-19 ST-elevation myocardial infarction patients. EuroIntervention 2021, 16, 1426–1433. [Google Scholar] [CrossRef]
- Koutsoukis, A.; Kanakakis, I. Challenges and unanswered questions in STEMI management. Hell. J. Cardiol. 2019, 60, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Feng, X.; Zhang, D.; Jiang, C.; Mei, H.; Wang, J.; Zhang, C.; Li, H.; Xia, X.; Kong, S.; et al. Deep vein thrombosis in hospitalized patients with COVID-19 in Wuhan, China: Prevalence, risk factors, and outcome. Circulation 2020, 142, 114–128. [Google Scholar] [CrossRef] [PubMed]
- Poissy, J.; Goutay, J.; Caplan, M.; Parmentier, E.; Duburcq, T.; Lassalle, F.; Jeanpierre, E.; Rauch, A.; Labreuche, J.; Susen, S. Lille ICU Haemostasis COVID-19 Group. Pulmonary embolism in patients with COVID-19: Awareness of an increased prevalence. Circulation 2020, 142, 184–186. [Google Scholar] [CrossRef]
- Lodigiani, C.; Iapichino, G.; Carenzo, L.; Cecconi, M.; Ferrazzi, P.; Sebastian, T.; Kucher, N.; Studt, J.D.; Sacco, C.; Bertuzzi, A.; et al. Humanitas COVID-19 Task Force. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb. Res. 2020, 191, 9–14. [Google Scholar] [CrossRef]
- Quagliariello, V.; Paccone, A.; Iovine, M.; Cavalcanti, E.; Berretta, M.; Maurea, C.; Canale, M.L.; Maurea, N. Interleukin-1 blocking agents as promising strategy for prevention of anticancer drug-induced cardiotoxicities: Possible implications in cancer patients with COVID-19. Eur. Rev. Med. Pharm. Sci. 2021, 25, 6797–6812. [Google Scholar]
- Carvelli, J.; Demaria, O.; Vély, F.; Batista, L.; Chouaki Benmansour, N.; Fares, J.; Carpentier, S.; Thibult, M.L.; Morel, A.; Remark, R.; et al. Association of COVID-19 inflammation with activation of the C5a-C5aR1 axis. Nature 2020, 588, 146–150. [Google Scholar] [CrossRef]
- Bois, M.C.; Boire, N.A.; Layman, A.J.; Aubry, M.C.; Alexander, M.P.; Roden, A.C.; Hagen, C.E.; Quinton, R.A.; Larsen, C.; Erben, Y.; et al. COVID-19-associated nonocclusive fibrin microthrombi in the heart. Circulation 2021, 143, 230–243. [Google Scholar] [CrossRef]
- Bangalore, S.; Sharma, A.; Slotwiner, A.; Yatskar, L.; Harari, R.; Shah, B.; Ibrahim, H.; Friedman, G.H.; Thompson, C.; Alviar, C.L.; et al. ST-segment elevation in patients with Covid-19—A case series. N. Engl. J. Med. 2020, 382, 2478–2480. [Google Scholar] [CrossRef]
- Rashid, M.; Timmis, A.; Kinnaird, T.; Curzen, N.; Zaman, A.; Shoaib, A.; Mohamed, M.O.; De Belder, M.A.; Deanfield, J.; Martin, G.P.; et al. Racial differences in management and outcomes of acute myocardial infarction during COVID-19 pandemic. Heart 2021, 107, 734–740. [Google Scholar] [CrossRef]
| Variable | COVID + Patients (n = 57 Patients) | Control Patients (n = 74 Patients) | p Value |
|---|---|---|---|
| Baseline characteristics | |||
| Age (years) | 64 (40–89) | 64 (41–88) | 0.860 |
| Male | 49 (85.96%) | 64 (86.48%) | 0.564 |
| Urban area | 34 (59.64%) | 44 (59.45%) | 0.563 |
| Admission complaints | |||
| Chest pain | 43 (75.43%) | 57 (77.02%) | 0.496 |
| Dyspnea | 47 (82.43%) | 46 (61.41%) | 0.048 |
| Medical history | |||
| Prior MI | 9 (15.78%) | 25 (33.78%) | 0.016 |
| Prior PCI | 6 (10.52%) | 11 (14.86%) | 0.595 |
| Prior CABG | 2 (3.51%) | 3 (4.05%) | 0.622 |
| Risk factors | |||
| Diabetes mellitus | 30 (52.70%) | 33 (44.59%) | 0.567 |
| Hypertension | 32 (56.14%) | 44 (59.45%) | 0.419 |
| Obesity | 29 (50.87%) | 34 (45.94%) | 0.289 |
| BMI (kg/m2) | |||
| <18 | 6 (10.52%) | 7 (9.45%) | |
| 18–30 | 22 (38.59%) | 33 (44.59%) | |
| 30–40 | 25 (43.85%) | 31 (41.80%) | |
| >40 | 4 (7.14%) | 3 (4.05%) | |
| Dyslipidemia | 19 (33.33%) | 25 (33.78%) | 0.476 |
| Chronic kidney disease | 2 (3.50%) (≥G3a) | 2 (2.70%) (≥G3a) | 0.129 |
| Active smoker | 16 (28.07%) | 20 (27.02%) | 0.872 |
| Admission hemodynamics | |||
| SBP (mmHg) | 132 (88–145) | 145 (120–174) | NA |
| HR (bpm) | 67 (35–87) | 78 (56–112) | NA |
| Oxygen saturation aa (%) | 92% (81–100) | 97% (92–100) | 0.018 |
| Total ischemia time | |||
| <6 h | 5 (8.77%) | 13 (17.56%) | 0.016 |
| 6–12 h | 41 (71.94%) | 54 (72.98%) | 0.563 |
| >12 h | 11 (19.29%) | 7 (9.46%) | 0.024 |
| Killip Class | |||
| I | 46 (80.71%) | 66 (89.19%) | 0.187 |
| II | 3 (5.26%) | 4 (5.40%) | 0.406 |
| III | 2 (3.51%) | 1 (1.36%) | 0.281 |
| IV | 6 (10.52%) | 3 (4.05%) | 0.012 |
| Variable | COVID + Patients (n = 57 Patients) | Control Patients (n = 74 Patients) | p Value |
|---|---|---|---|
| Hemoglobin (g/dL) | 13.5 (12.5–14.6) | 13.8 (12.8–14.8) | 0.565 |
| Hematocrit (%) | 41.8 (39.5–44.8) | 42.3 (38.8–44.6) | 0.239 |
| Platelets (mm3) | 270,000 (210,000–450,000) | 265,000 (190,000–345,000) | 0.805 |
| White blood cells (mm3) | 12,500 (8800–14,500) | 10,600 (9000–11,500) | 0.001 |
| LDL cholesterol (mg/dL) | 105 (78–180) | 111 (88–130) | 0.227 |
| Creatinine (mg/dL) | 1.06 (0.9–1.78) | 1.04 (0.8–1.98) | 0.636 |
| Uric acid (mg/dL) | 7.6 (7.3–8.0) | 7.2 (6.8–7.9) | 0.185 |
| ALAT (U/L) | 84 (45–110) | 82 (38–138) | 0.846 |
| ASAT (U/L) | 122 (100–168) | 117 (98–156) | 0.688 |
| CK-MB (U/L) | 156 (55–168) | 118 (88–256) | 0.061 |
| LDH (U/L) | 1215 (868–2300) | 872 (456–1300) | 0.016 |
| hs-cTnI (ng/L) | 2470 (1800–3400) | 1218 (654–1560) | 0.001 |
| CRP (mg/L) | 93 (40–128) | 65 (48–82) | 0.002 |
| ESR (mm/1h) | 58 (42–88) | 33 (22–55) | 0.001 |
| Fibrinogen (mg/dL) | 640 (560–780) | 450 (390–520) | 0.023 |
| Ferritin (ng/mL) | 480 (390–620) | 350 (290–410) | 0.025 |
| D-dimer (ng/mL) | 1450 (1100–1780) | 490 (380–580) | 0.007 |
| Variable | COVID + Patients (n = 57 Patients) | Control Patients (n = 74 Patients) | p Value |
|---|---|---|---|
| Echocardiographic characteristics | |||
| Mean LVEF (%) | 39 (32–56) | 33 (30–48) | 0.044 |
| Number of coronary lesions | |||
| Without atherosclerotic lesions | 9 (15.78%) | 1 (1.35%) | 0.020 |
| Unicoronary lesion | 31 (54.38%) | 39 (52.70%) | 0.423 |
| Bicoronary lesions | 8 (14.03%) | 18 (24.32%) | 0.068 |
| Tricoronary lesions | 9 (15.78%) | 16 (21.62%) | 0.085 |
| Primary PCI | |||
| LAD | 23 (40.35%) | 34 (45.94%) | 0.134 |
| RCA | 7 (12.28%) | 8 (10.81%) | 0.204 |
| LCX | 14 (24.56%) | 24 (32.43%) | 0.098 |
| Thromboaspiration (no need for primary PCI) | 10 (17.54%) | 2 (2.70%) | <0.001 |
| Risk Factor | Pearson r Correlation Coefficient | p Value |
|---|---|---|
| Diabetes mellitus | 0.656 | 0.035 |
| Hypertension | 0.111 | 0.211 |
| Obesity | 0.133 | 0.130 |
| Dyslipidemia | 0.565 | 0.048 |
| Chronic kidney disease | 0.162 | 0.065 |
| Active smoker | 0.856 | 0.008 |
| Alcohol consumption | 0.056 | 0.524 |
| Inflammatory Marker | Pearson r Correlation Coefficient | p Value |
|---|---|---|
| CRP (mg/L) | 0.703 | 0.005 |
| ESR (mm/1h) | 0.686 | 0.018 |
| Fibrinogen (mg/dL) | 0.756 | 0.001 |
| WBC (mm3) | 0.173 | 0.199 |
| Ferritin (ng/mL) | 0.099 | 0.465 |
| Variable | COVID + Patients (n = 57 Patients) | Control Patients (n = 74 Patients) | p Value |
|---|---|---|---|
| Ventricular tachycardia/fibrillation | 3 (5.26%) | 2 (2.70%) | 0.044 |
| Atrial fibrillation | 3 (5.26%) | 8 (10.81%) | 0.012 |
| Mean length of hospital stay (days) | 4 (1–8) | 6 (3–9) | 0.029 |
| In-hospital mortality | 9 (15.78%) | 1 (1.35%) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anghel, L.; Tudurachi, B.-S.; Leonte, A.; Sascău, R.A.; Zota, I.M.; Bazyani, A.; Tinică, G.; Stătescu, C. The Challenge of High Coronary Thrombotic Events in Patients with ST-Segment Elevation Myocardial Infarction and COVID-19. J. Clin. Med. 2022, 11, 6542. https://doi.org/10.3390/jcm11216542
Anghel L, Tudurachi B-S, Leonte A, Sascău RA, Zota IM, Bazyani A, Tinică G, Stătescu C. The Challenge of High Coronary Thrombotic Events in Patients with ST-Segment Elevation Myocardial Infarction and COVID-19. Journal of Clinical Medicine. 2022; 11(21):6542. https://doi.org/10.3390/jcm11216542
Chicago/Turabian StyleAnghel, Larisa, Bogdan-Sorin Tudurachi, Andreea Leonte, Radu Andy Sascău, Ioana Mădălina Zota, Amin Bazyani, Grigore Tinică, and Cristian Stătescu. 2022. "The Challenge of High Coronary Thrombotic Events in Patients with ST-Segment Elevation Myocardial Infarction and COVID-19" Journal of Clinical Medicine 11, no. 21: 6542. https://doi.org/10.3390/jcm11216542
APA StyleAnghel, L., Tudurachi, B.-S., Leonte, A., Sascău, R. A., Zota, I. M., Bazyani, A., Tinică, G., & Stătescu, C. (2022). The Challenge of High Coronary Thrombotic Events in Patients with ST-Segment Elevation Myocardial Infarction and COVID-19. Journal of Clinical Medicine, 11(21), 6542. https://doi.org/10.3390/jcm11216542









