Abstract
Background: Left atrial appendage occlusion is an increasingly proposed treatment for patients with atrial fibrillation and poor tolerance to anticoagulants. All endovascular devices require antithrombotic therapy. Anatomical and clinical variables predisposing to device-related thrombosis, as well as post-procedural peri-device leaks, could mandate the continuation or reintroduction of aggressive antithrombotic treatment. Because of the absence of foreign material inside the heart, epicardial appendage closure possibly does not necessitate antithrombotic therapy, but data of large series are missing. Methods: Multidisciplinary team evaluation for standalone totally thoracoscopic epicardial appendage closure was done in 180 consecutive patients with atrial fibrillation and poor tolerance to antithrombotic therapy. One hundred and fifty-two patients consented (male 66.1%, mean age 76.1 ± 7.4, CHA2DS2VASc mean 5.3 ± 1.6, HASBLED mean 3.8 ± 1.1). Indications were cerebral hemorrhage (48%), gastro-intestinal bleeding (33.3%), and other bleeding (20.7%). No antithrombotic therapy was prescribed from the day of surgery to the latest follow up. Results: Procedural success was 98.7%. At a mean follow up of 38.2 ± 18.8 months, cardioembolic and bleeding events were 1.3% and 0.6%, respectively. Among patients with a history of blood transfusions (41.1%), none needed further transfusions or treatment post procedure. Conclusion: Epicardial appendage occlusion without any antithrombotic therapy appears to be safe and effective. This strategy could be advised when minimization of bleeding risk concomitant to stroke prevention is needed.
1. Introduction
Cerebrovascular events are the third leading cause of death in developed countries. Atrial fibrillation (AF) accounts for 15–30% of these events and requires stroke prevention treatment options with new oral anticoagulants (NOACs) as first line therapy over Vit K antagonists (OACs) as a pharmacological strategy [1]. Despite guidelines, anticoagulants are not prescribed in up to 30% of AF patients (ORBIT-GAREFIELD registry) [2]. According to the ROCKET, ARISTOTLE, and RE-LY studies, the prescription of NOACs is associated with a discontinuation rate of 23.7%, 25.3, and 20.7%; 1.7%, 1.2%, and 1.5% risk of stroke/year; and 14.9%, 18.1%, and 14.6% risk of bleeding/year, with a rate of major hemorrhage of 3.6%, 2.1%, and 2.7%, respectively [3,4]. To improve bleeding outcomes, lower dose NOACs regimens have been tested. A meta-analysis of randomized trials of patients on low dose NOACs vs. warfarin has shown similar overall reductions in cardioembolism, and a non-significant reduction in major bleeding with a significant reduction in intracranial bleeding [5]. As bleeding is a major cause of NOACs/OACs discontinuation, left atrial appendage occlusion (LAAO) has become an interventional therapeutic option [1]. PROTECT-AF, PREVAIL, and PRAGUE-17 trials have shown potential and drawbacks, mainly bleeding, of LAAO with the mandatory post procedural antithrombotic therapy [5,6,7]. The findings of the PRAGUE-17 trial with those of AVERROES support the idea that higher bleeding rates are expected in higher HASBLED risk profile cohorts on single antiplatelt therapy (SAPT) [7]. A meta-analysis of all of the major trials has demonstrated no statistically significant reduction in major bleeding of LAAO compared with (N)OAC [8]. Ewolution and Aplatzer-Amulet’s studies, reporting excellent success rates of implantation, and trend towards less aggressive post procedure antithrombotic therapy to improve bleeding outcomes, have shed further light on the potentials of interventional strategies for stroke prevention in AF [9,10]. However, bleeding remains an issue with any antithrombotic therapy according to ACTIVE and ASPREE trials [11,12]. In addition, the increasing number of procedures have brought to attention peri-device leak (PDL) and device-related thrombosis (DRT), both requiring the reintroduction of antithrombotic treatment, re-presenting the dilemma of an appropriate pharmacological regimen in patients referred to LAAO because of a poor tolerance to antithrombotic therapy [13,14,15]. Epicardial LAAO because of the absence of a foreign material inside the heart potentially does not require any antithrombotic therapy, addressing some anatomical, procedural, and clinical issues improving bleeding outcomes. Only few reports with this approach are published and all have a post procedure period of antithrombotic therapy [16,17,18,19]. Here, we describe our experience regarding the safety and efficacy of standalone totally thoracoscopic epicardial appendage clipping with immediate antithrombotic discontinuation.
2. Materials and Methods
2.1. Patients Selection
The inclusion criteria were a diagnosis of any type of atrial fibrillation, CHA2DS2VASc > 2, HAS BLED > 1, or poor tolerance to OAC/NOAC, defined as at least one of the following: life threatening hemorrhage, more than two hospital admissions for bleedings on (N)OACs requiring treatment, hemoglobin decrease > 2 g/dL, chronic underlying disease predisposing to a high risk of rebleeding if on APT. A multidisciplinary team (an electrophysiologist, a cardiac surgeon, an anesthesiologist, a neurologist, a gastroenterologist, and the referring physician) evaluated all patients. Exclusion criteria were life expectancy <1 year, ongoing DAPT for recent PTCA, contraindication to single right lung ventilation, concomitant cardiac surgery, indication to AF ablation (Table 1). All patients requiring appendage occlusion at our institution were discussed by the Heart Team and the criteria of this study were additional to the flow-chart accepted by all members of the team, which were previously published [20]. The preoperative workup included heart CT scan and echocardiogram for potential coronary artery disease/structural heart disease requiring treatment, and carotid doppler ultrasound for baseline neurologic follow up. As none of the patients had signs or symptoms of lower limb ischemia, doppler ultrasound for POVD was not routinely performed.

Table 1.
Patients characteristics.
2.2. LAAO-T Procedure
The procedure was performed as described previously [21]. Briefly, three ports in a “hockey stick” configuration were introduced in the left hemithorax between the anterior and mid-axillary line in the III, V, and VII intercostal space. After CO2 insufflation, the pericardium was opened, the LAA was measured, and the AtriClipPro2 (AtriCure Inc., Mason, OH, USA) was deployed at its base under direct view and TOE guidance.
2.3. Post Procedure Pharmacological Therapy
No antithrombotic therapy was prescribed from the day of surgery to the latest follow up, except in four patients requiring SAPT for atherosclerotic disease.
Of these four patients, two had a previous stroke, and the others, despite the degree of carotid artery stenosis, received no antiplatelet therapy, because in presence of asymptomatic carotid stenosis, antiplatelet therapy is not mandatory according to the guidelines of the European Society of Vascular Surgery (class of indication IIa level of evidence C), and in the US version no recommendation is given [22,23]. In all cases with carotid stenosis >50% the decision by the Heart Team regarding the appropriate antiplatelet regimen was always discussed with the patient.
2.4. Follow up
All patients underwent outpatient clinic visit with physical examination, ECG, laboratory tests, and completion of the Questionnaire for Verifying Stroke Free Status (QVSFS) at 1, 2, 6, and 12 months and annually thereafter. This questionnaire, validated by the European Society of Neurology, was chosen as it has been shown to be effective at identifying stroke free individuals with accuracy, also in a population with a large proportion of patients with previous stroke or TIA. In the case of at least one positive answer, a CT scan was planned [24]. For appendage closure assessment, TOE and CT scans at 1–3 months were scheduled. Criteria of success was considered a stump less than 1 cm [25]. Although arbitrary, this value is widely accepted and has been shown to be a risk factor for DRT for endovascular devices [26].
2.5. Statistical Analysis
Categorical variables are expressed in numbers (n/N) and percentages (%). Continuous variables with a normal distribution using a Shapiro–Wilk test are expressed as mean ± standard deviation (SD), median, and interquartile range (Q1–Q3) when meaningful. The individual patient annual risk for stroke and bleeding was calculated in accordance with CHA2DS2VASc and HASBLED, and then calculated for the population (expected risk rate) and compared with the corresponding observed risk rate [27,28]. The relative risk reduction (RR) was then calculated as (observed risk − expected risk)/expected risk × 100. To analyze event rates at the latest follow up for cardiovascular death, cardioembolism, and hemorrhage, the Kaplan–Meier survival analysis was calculated. A Log rank test was performed for comparison.
3. Results
3.1. Patients
One-hundred and eighty consecutive patients underwent a multidisciplinary team evaluation: 152 (age 76.9 ± 6.7, male 65.8%, CHA2DS2VASc 5.4 ± 1.6, HASBLED 3.8 ± 1.1, cerebral hemorrhage 55.0%, previous cardioembolism 14.1%, GI bleeding 31.3%, non-cerebral/GI bleeding 15.3%, and anatomy unsuitable for percutaneous procedure 5.5%) underwent LAAOT. The patients with an unsuitable anatomy for the percutaneous procedure were not referred for ablation as this would have required at least three months of oral anticoagulation and this period was considered by the Heart Team as being at too high risk for bleeding for each of the patients. Twenty-eight patients (age 71.5 ± 9.4, male 83.3%, CHA2DS2Vasc 4.3 ± 1.1, HASBLED 3.7 ± 1.3, cerebral hemorrhage 40%, previous stroke 28%, GI bleeding 52%, and non-cerebral/GI bleeding 4%) denied consent (nLAAOT).
3.2. Procedural Outcomes
All but 2 of the 152 patients underwent LAAOT. Operative data and outcomes are shown in Table 2.

Table 2.
Intra-post operative data, pharmacological therapy.
No deaths or conversion to thoracotomy or device-related complications were reported. Eighteen patients had their appendage successfully closed despite pericardial adhesions. For this reason, two were referred to percutaneous closure. The only complication reported was pericarditis in 7 of the first 50 patients, and none were reported after the introduction of prophylactic colchicine at 0.5 mg bid or indomethacin 50 mg bid. TOE and CT scans showed satisfactory device deployment in all patients, with a mean stump of 2.4 ± 2.3 mm and absence of stump in 81% of cases (Figure 1 and Figure 2).
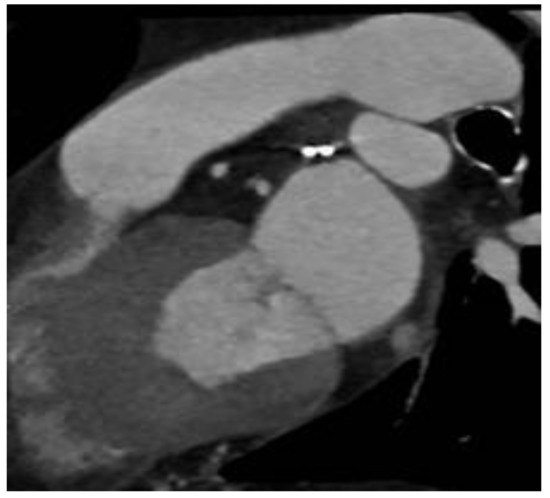
Figure 1.
Clip short axis.

Figure 2.
Clip long axis.
3.3. Follow up
Clinical and imaging follow up for the appendage was complete for all 180 patients (mean 38.2 ± 18.8 months, range 65–6 months), resulting in 377.9 patient/year for stroke and 378.8 patient/year for hemorrhage. In the LAAO-T group, no hospital re-admissions were documented for cardiovascular events related to the procedure. All patients completed the QVSFS. There was one minor stroke and one TIA (10 and 5 months, respectively) in the absence of a significant LAA stump at CT scan. On the QVSFS, no suspicion of neurological events was raised in all other patients. The actual ischemic rate was 1.3% compared with the expected adjusted mean stroke rate of 6.8%/year. None of the patients (46.6%) in the LAAOT group with a history of repetitive blood transfusions were readmitted for blood requirement. With one cerebral hemorrhage (cerebral artero–venous malformation), the rate of bleeding was 0.6%, which compared favorably with the expected 6.9% predicted bleeds/years, but the effective reduction was higher, considering that 7.9% of patients had HASBLED > 5, and for this value, the effective bleeding risk/year is not available in literature (Figure 3) [27].
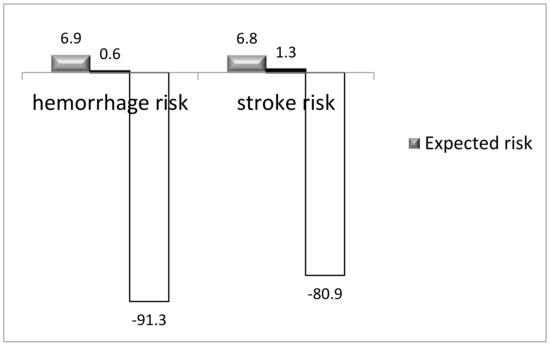
Figure 3.
RR reduction for hemorrhage and stroke.
In the LAAOT patients, there were four deaths at 50 days, 6 months, 1.5 year, and 1.9 years for the recurrence of cerebral hemorrhage, multi-organ failure, pneumonia, and SARS-CoV-2 infection, respectively. Of the 28 patients who denied consent (nLAAOT) (12 on LMWH and 16 on APT), 6 died (3 cerebral hemorrhage, 2 strokes, and 1 GI re bleeding), 4 experienced repetitive transfusion/treatment during follow up (total re bleeding event 28.5%), and 1 cardioembolic event (total cardioembolic event 10.7%), and the remainder experienced no adverse events (Figure 4 and Figure 5).
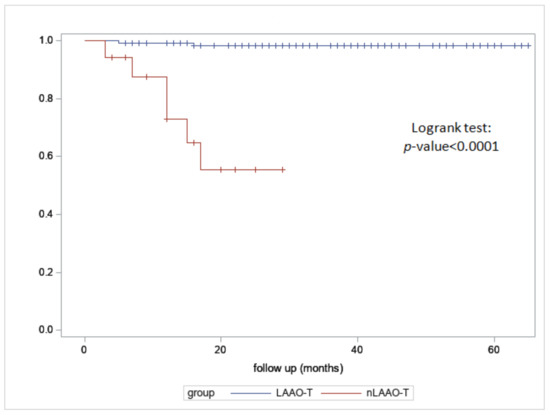
Figure 4.
Kaplan–Meier for stroke for LAAO-T and nLAAOT.
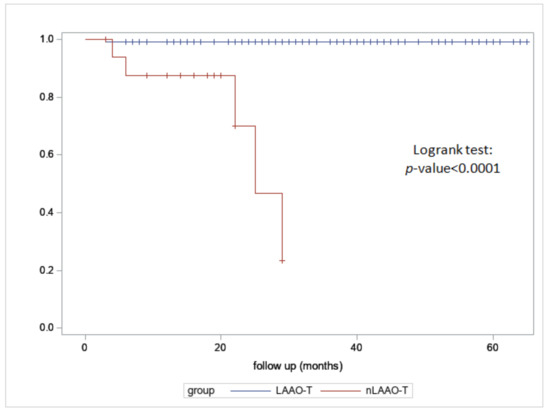
Figure 5.
Kaplan–Meier for hemorrhage for LAAOT and nLAAOT.
4. Discussion
Up to date, this is the first study on the safety and efficacy for haemorrhage and stroke prevention of an epicardial approach to LAAO in the absence of any antithrombotic therapy from the immediate postoperative day. Cardioembolism and hemorrhage are the two faces of the same coin when deciding upon optimal antithrombotic therapy in AF [1]. (N)OACs are first line therapy, but bleeding is a major cause of discontinuation [2,3,5]. Antiplatelet therapy may only partially address cardioembolic issues, and bleeding remains a problem, as shown by the ACTIVE and ASPREE trials [11,12]. In the case of major bleeding complications, the decision when to resume or discontinue antithrombotic therapy in the long-term is still the subject of debates [26,27,28,29,30,31]. In a report of Redfors on patients off (N)OACs for at least one year due to contraindication, incidences of ischemic and hemorrhagic stroke were 12 and 20.3%, respectively, and both were strongly correlated [32]. According to the TREAT-AF study, resumption of antithrombotic therapy at 90 days following major bleeding is associated with significant increased risk of non-intracranial bleeding and a trend to a lower risk of stroke, suggesting that stroke prevention strategies after major bleeding events could be beneficial if bleeding risk is minimized [33]. As the majority of thrombi in patients with AF are thought to come from the LAA [34], different devices for LAAO have been designed. The annual ischemic strokes rates with NOACs are 1–2%, and with percutaneous devices they range from 0 to 2.2% [8,9,10,35]. Meta-analysis of RCTs have shown a similar rate of ischemic stroke for percutaneous LAAO compared with N(OACs), and reductions in hemorrhagic strokes, but no statistically significant reduction in major bleeding [8]. Another meta-analysis of RCTs and 27 observational studies comparing major bleeding events in percutaneous LAAO vs. NOAC showed 2.2 events per 100 patient-year events vs. 2.5 events per 100 patient-year event, respectively [36].
Endocardial devices share four scenarios: immediate antithrombotic therapy, DRT, PDL, and a favorable LAA anatomy [35]. The PROTECT, PRAVAIL, and PRAGUE-17 trials, and EWOLUTION and AMPLATZER-AMULET studies have reported the potentials and drawbacks of endocardial devices [6,7,9,10]. In the EWOLUTION study, good implantation rates have been reported with 2.2% of patients excluded for suboptimal anatomy. The incidence of DRT was 4.1%, and 4.6% had major bleeding with 27% of patients on OAC/NOAC, 60% on DAPT, 8% (off label implant) without APT, and 7% on SAPT at discharge. At 2 years, 8% were still on OAC/NOAC, 7% on DAPT, 71% on SAPT, and 14% were without any antithrombotic therapy [9]. The AMPLATZER-AMULET study reported comparable procedural success, with incidence of DRT of 1.69%, with 57.7% of patients discharged on DAPT, 22.4% on SAPT, 11.2% on OAC, with an annual ischemic stroke rate of 2.2%/year, annual TIAs of 1.0%/year, and annual rate of major bleeding of 7.2%, ranging from 10.1%/year at 1 year and 4%/year thereafter. At 2 years, 15.7% of patients were still on OAC/DAPT, 62.8% on SAPT, and 21.5% were without any APT [10]. The detection of DRT and PDL requires the reintroduction of aggressive antithrombotic therapy [14,23] as they are potentially associated with a higher risk of death and cardioembolism [14,26,35,37].
DAPT with clopidrogel + aspirin, the most frequently used combination, increases the risk of major bleeding by up to 30% compared with SAPT alone [29]. In addition, this mandatory post procedure therapy may be not ideal for patients with high HASBLED or comorbidity with persistent high risk of bleeding on APT (i.e., degenerative amyloid angiopathy, Rendu Osler Weber syndrome, intracranial hemorrhages requiring prolonged follow up, some hematologic diseases, and GI angiodysplasia). To improve bleeding outcomes, a shortened post procedure period of NOAC/OAC/APT, despite a lack of large trials, has been suggested [9,10]. All of the above suggest a clinical need to further optimize bleeding outcomes in frail patients. The 2020 ESC guidelines state that for patients who do not tolerate any antiplatelet therapy, either an epicardial catheter approach (e.g., Lariat system) or thoracoscopic clipping of the LAA may be considered. Based on this evidence, we designed a study whose peculiarities are as follows: a high CHA2DS2VASc and HASBLED score, based on the Heart Team assessment and on immediate antithrombotic therapy discontinuation post implantation.
In our experience, LAAO thoracoscopically was successfully performed in 98.7% of cases. This is in line with other papers on epicardial and endocardial devices for LAAO [9,10,16,17,18,19]. However, with percutaneous devices, 15–17% of successfully implanted patients are still on (N)OAC/DAPT after 2 years [9,10]. Therefore, although LAAO may be occasionally voluntarily associated with NOACs prescription, the procedural success does not always reflect treatment success. This is further affected by the incidence of DRT and PDL requiring the reintroduction of antithrombotic therapy [13,14,15,29]. In our experience, a successful procedure equals treatment success, as no patient received any antithrombotic therapy from surgery to the latest follow up. This compares favorably to all up to date published reports on epicardial devices all including a period of APT and with the largest up to date paper on LAAO with Lariat with 98% effective complete closure [15,16,17,18].
The clipping device used has been specifically designed for LAAO in contrast with endostaplers, which have a lower success outcome, as reported by Lee et al. [37]. Delivering the clip with a simplified and standardized thoracoscopic technique requiring only basic thoracoscopic skills may be interesting for centers with larger volumes of LAAO procedures, as an epicardial approach could be the solution for those technically ineligible for a percutaneous procedure [7,8,9,10,13,15,18,19].
Pericarditis was the only complication reported and the introduction of colchicine dramatically reduced the incidence of tissue inflammation, contributing to no further events. This is in accordance with Gunda et al. [38] and compares favorably to other epicardial procedures with 8.3−14% incidence of pericarditis [18,19,35].
No anatomically ineligible appendages were found and all patients ineligible for the percutaneous device were successfully treated thoracoscopically. The absence of stump was reported in 81% of our series, in line with Caliskan et al. with 72% of no stump in the open chest surgery, and suggests that a thoracoscopic approach may provide results comparable to open chest surgery [39]. Therefore, data on the efficacy of this device can probably be mutually extrapolated from both accesses. The lariat is the only other available epicardial device specifically designed for LAAO, and in all reports published, adhesions have been described as a contraindication in all cases [40,41]. The success of implantation in our experience in the case of adhesions led us to the conclusion that adhesions should not be considered a contraindication, but detailed discussion with patients is mandatory to clarify the potential risks of the thoracoscopic procedure. For those eligible patients who denied consent to the procedure, self-perception of their frailty was the leading reason for refusal. The incidence of cardioembolism (1.3 vs. 10.7%) and hemorrhage (0.6 vs. 28.5%) of LAAOT vs. n-LAAOT patients is in line with the only up to date published paper of Parikh et al. [19], with comparable HASBLED to ours, reporting on 108 lariat patients vs. 45 patients excluded from LAAO (cardioembolism 1.9% vs. 24%, hemorrhage 9.2 vs. 24.4%), suggesting that in patients with high HASBLED, epicardial LAAO seems to have a better prognosis than the resumption of subtherapeutic antithrombotic therapy [19,32,33].
In terms of cardioembolism prevention with a mean CHA2DS2VASc of 5.3 ± 1.6 for this study, a 80.9% relative risk reduction for stroke in the absence of any antithrombotic therapy at more than 3 years is in line with the reported 63−86% of percutaneous studies, all with a lower mean CHA2DS2VASc [9,10] and with the results reported in a multicenter study on epicardial appendage clipping [17].
However, in this latter multicenter study, the stroke preventive effect of the post procedure antithrombotic therapy at discharge ((N)OAC 10%, 3% LMWH, 41% on SAPT, and 2% on DAPT) and during follow up not objectively specified might have influenced the results in the median follow up of 12.5 months [17]. The results by Litwinowicz et al. are promising [41] for long term outcomes with the Lariat, with a mean follow up of 4.2 years, documenting 81% risk reduction for stroke and 78% risk reduction of bleeding, but the post procedural antithrombotic therapy (58% on anticoagulants) again might have had an impact on the event rate calculations. These findings seem to be confirmed by the long term clinical outcomes for lariat reported by Parikh et al., with a systemic thromboembolic event rate of 1.9% at a follow up of 6.5 ± 0.8 years, 15.7% without any antiplatelet therapy from the third month [19], and in the largest up to date European experience with Lariat by Tilz et al., with 1.8% incidence of cardioembolic events at a mean follow up of 181 ± 72 days with post procedure antiplatelet therapy [42,43].
Although promising, all these data do not allow for drawing definitive conclusions on the effective added value of an epicardial closure whose peculiarity is the absence of the required post procedure APT. This might only help the up to date report of epicardial LAAO with the shortest period of anticoagulation and no further antithrombotic therapy by Ohtsuka et al. documenting two cardioembolic events and no bleedings on 201 patients at a mean follow up period of 48 months [18].
In terms of bleeding outcomes, considering the mean HASBLED and the distribution of our population, a 88.9% relative risk reduction compared favorably with all of the up to date published data on endovascular devices, all of which included the overall lower predicted risk of bleeding, and suggest that the overall 46% relative risk reduction of major bleeding reported by Boersma et al. and the 7.2% risk of hemorrhage by Hildick-Smith might be improved by the absence of antithrombotic therapy [9,10,11,31].
Patients with specific diseases with intrinsic high re-bleeding risk on antithrombotic therapy should preferably be treated with a solution that allows for immediate antithrombotic therapy discontinuation. In our series, except for one case of cerebral hemorrhage, no recurrence of bleeding was reported. Among the enrolled patients with repetitive bleeding requiring treatment, 33.3% had previous GI bleeding. After LAAOT, no further hospitalizations for transfusions were documented. This finding compares favorably with the only up to date report on a sub-category of 151 patients with previous GI bleeding who had undergone endocardial LAAO and subsequent antithrombotic therapy. In this report, 4% vs. 0.8% of major periprocedural bleeding were calculated among patients with previous GI bleeding and non-GI, respectively, with overall 4.6% vs. 1.5% major bleeding events at a follow up of 1.3 years and a 20.1% relative reduction according to the expected rate based on the HASBLED for GI group [44]. The comparison was also favorable with Hildick-Smith et al., reporting on 1088 patients implanted with Amplatzer Amulet: incidence of bleeding was 10.2%, mainly GI and prescription of a less aggressive antithrombotic therapy showed no significant difference between DAPT and SAPT (41.8% vs. 34.4%) (10), as GI bleedings’ indication to LAAO are often associated with a high bleeding recurrence on APT [45,46]. We expect our result to be confirmed over time due to the stable closure rate of the device documented after 5 years [47].
From the first trials on LAAO, there has been a trend towards a higher degree of frailty for eligible patients and, to improve outcomes, as in other cardiovascular diseases, a multidisciplinary approach has been advocated for, along with studies on endocardial vs. epicardial devices [48,49]. In a report comparing Watchman vs. Lariat, incidence of leaks was 21% vs. 14%, of thrombus 3.7% vs. 1.4%, and of stroke was 1.3% vs. 1.1%. In a preliminary report comparing transcatheter and thoracoscopic approaches, both strategies seemed to be safe and effective [20].
In the case of poor tolerance to (N)OACS, the optimal therapeutic option is the subject of active debate, especially in frail patients and the selection of the appropriate treatment option for pharmacologic, endovascular, or epicardial should probably be based on absolute risk of stroke and bleeding recurrence for a given patient in a multidisciplinary approach.
5. Conclusions
Epicardial appendage closure without antithrombotic therapy appears to be safe and effective for hemorrhage and stroke prevention at the midterm. In the presence of anatomical and clinical aspects predisposing to suboptimal implantation or the recurrence of bleeding on APT, an epicardial approach should be considered. Further studies comparing epicardial vs. endocardial devices, preferably randomized, are needed with the main aim of improving patient selection, as specific categories of patients might benefit from a specific treatment option.
6. Limitations
The number of patients, length of follow up, and being a single center study are major limitations. Although totally thoracoscopic cardiac surgery is not widely diffused, this procedure requires only basic thoracoscopic skills and is thus easily accessible for those centers willing to offer an epicardial option when endovascular LAAO is not feasible. The definition used to define the success of implantation is arbitrary and requires further evaluation for clinically relevant implications. HAS BLED is a useful scoring tool, but it is imperfect. A cerebral MRI to assess microembolization might help to detect subclinical strokes, but this would require comparison with a control group to be meaningful; it is of note that this data are missing in the largest studies on percutaneous devices. The absence of a control group is also a limitation, but as data on the safety and efficacy of stand alone epicardial LAAO are few, the present study was designed as potentially preliminary to a RCT that will require a control group.
Author Contributions
Conceptualization: S.B., F.G., M.M. and M.L.M.; methodology, S.B., M.L.M., and M.M.; software, G.D. and G.C.; validation, M.L.M., S.B., M.M., M.F. and C.S.; formal analysis S.B., M.M., F.G., G.C. and D.C.; investigation, S.B., M.L.M., E.M. and M.F.; data curation, S.B., F.G., L.A. and G.C.; writing—original draft preparation, S.B. and M.L.M.; writing—review and editing, S.B. and M.L.M.; visualization, S.B., F.G. and D.C.; supervision, M.L.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and was approved by the Institutional Review Board (Santa Chiara Hospital Ethics Committee) of Santa Chiara Hospital (protocol code A378 last renewal 2021).
Informed Consent Statement
Informed consent was obtained from all of the subjects involved in the study.
Data Availability Statement
All of the data are available upon written request to the corresponding author.
Acknowledgments
The authors would like to thank Riccardo Pertile for the statistical analysis.
Conflicts of Interest
M.L.M. is consultant for Atricure Inc., all other authors declare no conflict of interest.
References
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.; Blomstrom-Lunqvist, C.; Borian, G.; Castella, M.; Dan, G.; Dilaveris, P.; et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, B.A.; Gao, H.; Shrader, P.; Pieper, K.; Thomas, L.; Camm, A.; Ezekowitz, M.; Fonarow, G.; Gersh, B.; Goldhaber, S.; et al. International trends in clinical characteristics and oral anticoagulation treatment for patients with atrial fibrillation: Results from the GAREFIELD-AF, ORBIT-AF I, anf ORBIT AF II registries. Am. Heart J. 2017, 194, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Ruff, C.; Giuliano, P.; Braunwald, E.; Hoffman, E.; Deenadayau, N.; Ezekowitz, M.; Camm, A.; Weitz, J.; Lewis, B.; Parkhomenko, A.; et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomized trials. Lancet 2014, 383, 3955–3962. [Google Scholar] [CrossRef]
- Hankey, G.; Norrving, B.; Hacke, W.; Steiner, T. Management of acute stroke in patients taking novel oral anticoagulants. Lancet 2014, 9, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Holmes, D.; Kar, S.; Price, M.; Whisenant, B.; Sievert, H.; Doshi, S.; Huber, K.; Reddy, V. Prospective randomized evaluation of the watchman left atrial appendage closure device in patients with atrial fibrillation versus long term warfarin therapy. J. Am. Coll. Cardiol. 2014, 8, 1–12. [Google Scholar] [CrossRef]
- Reddy, V.Y.; Sievert, H.; Halperin, J.; Doshi, S.; Buchbinder, M.; Neuzil, P.; Huber, K.; Whisenat, P.; Kar, S.; Swarup, V.; et al. PROTECT AF steering committee and Investigators. Percutaneous left atrial appendage closure vs warfarin for atrial fibrillation: A randomized clinical trial. JAMA 2014, 312, 1988–1998. [Google Scholar] [CrossRef]
- Osmancik, P.; Herman, D.; Neuzil, P.; Hala, P.; Taborsky, M.; Kala, P.; Poloczek, M.; Stasek, J.; Haman, L.; Branny, M.; et al. Left atrial appendage closure versus direct oral anticoagulants in high risk patients with atrial fibrillation. J. Am. Coll. Cardiol. 2020, 25, 3122–3135. [Google Scholar] [CrossRef]
- Turagam, M.; Osmancik, P.; Neuzil, P.; Dukkipati, S.; Reddy, V. Left atrial appendage closure versus oral anticoagulants in atrial fibrillation, A meta-analysis of randomized trials. J. Am. Coll. Cardiol. 2020, 76, 2795–2797. [Google Scholar] [CrossRef]
- Boersma, L.; Ince, H.; Kische, S.; Pokushalov, E.; Scmitz, T.; Schmidt, B.; Gori, T.; Meincke, F.; Protopopov, A.; Betts, T.; et al. Evaluating real world clinical outcomes in atrial fibrillation patients receiving the WATCHMAN left atrial appendage closure technology. Circ. Arrhythm. Electrophysiol. 2019, 12, e006841. [Google Scholar] [CrossRef]
- Hildick-Smith, D.; Landmesser, U.; Camm, J.; Diener, H.; Paul, V.; Scmidt, B.; Settergren, M.; Teiger, N.; Nielsen-Kudsk, J.; Tondo, C. Left atrial appendage occlusion with the Amplatezer Amulet device: Full results of the prospective global observational study. Eur. Heart J. 2020, 41, 2894–2901. [Google Scholar] [CrossRef]
- The ACTIVE Investigators. Effect of clopidogrel added to aspirin in patient with atrial fibrillation. N. Engl. J. Med. 2009, 360, 2066–2078. [Google Scholar] [CrossRef]
- Mc Neil, J.J.; Woods, R.; Nelson, M.; Reid, C.M.; Kirpach, B.; Wolfe, R.; Storey, E.; Shah, R.C.; Lockery, J.E.; Tonkin, A.M.; et al. Effect of Aspirin on Disability-free Survival in the Healthy Elderly. N. Engl. J. Med. 2018, 379, 1499–1508. [Google Scholar] [CrossRef]
- Asmarats, L.; Rodes-Cabau, J. Percutaneous left atrial appendage closure: Current devices and clinical outcomes. Circ. Cardiovasc. Interv. 2017, 10, e005359. [Google Scholar] [CrossRef]
- Granier, M.; Laugaudin, G.; Massin, F.; Stephane, C.; Pierre, F.W.; Cornelia, F.; Pasquie, J.-L. Occurrence of incomplete endothelization causing residual permeability after left atrial appendage closure. J. Invasive Cardiol. 2018, 30, 245–250. [Google Scholar]
- Lempereur, M.; Aminian, A.; Freixa, X.; Gafoor, S.; Kefer, J.; Tzikas, A.; Legrand, V.; Saw, J. Device-associated thrombus formation after left atrial appendage occlusion: A systematic review of events reported with the Watchman, the Amplatzer Cardiac plug and the Amulet. Catheter. Cardiovasc. Interv. 2018, 92, e216–e217. [Google Scholar] [CrossRef]
- Lakkireddy, D.; Afzal, M.R.; Lee, R.J.; Nagaraj, H.; Tschopp, D.; Gidney, B.; Ellis, C.; Altman, E.; Lee, B.; Kar, S.; et al. Short and long term outcomes of percutaneous left atrial appendage suture ligation: Results from US multicenter evaluation. Heart Rhythm. 2016, 13, 1030–1036. [Google Scholar] [CrossRef]
- Cartledge, R.; Suwalski, G.; Witkowska, A.; Gottlieb, G.; Cioci, A.; Chidiac, G.; Ilsin, B.; Merrill, B.; Suwalsky, P. Standalone epicardial left atrial appendage exclusion for thromboembolism prevention in atrial fibrillation. Interact. Cardiovasc. Thor. Surg. 2021, 34, 548–555. [Google Scholar] [CrossRef]
- Ohtsuka, T.; Nonaka, T.; Hisagi, M.; Ninomiya, N.; Masukawa, A.; Ota, T. Thoracoscopic stapler-and-loop technique for left atrial appendage closure in nonvalvular atrial fibrillation: Mid-term outcomes in 201 patients. Heart Rhythm. 2018, 15, 1314–1320. [Google Scholar] [CrossRef]
- Parikh, V.; Bartus, K.; Litwinowicz, R.; Turagam, M.; Sadowsky, J.; Kapelak, B.; Bartus, M.; Podolec, J.; Brzezinsky, M.; Musat, D.; et al. Long Term clinical outcomes from real world experience of left atrial appendage exclusion with LARIAT device. J. Cardiovasc. Electrophysiol. 2019, 30, 2849–2857. [Google Scholar] [CrossRef]
- Branzoli, S.; Guarracini, F.; Marini, M.; D’ognhia, G.; Penzo, D.; Piffer, S.; Peterlana, D.; Graffigna, A.; Gulizia, M.M.; Gelsomino, S.; et al. Heart Team for Left atrial appendage occlusion: A patient tailored approach. J. Clin. Med. 2022, 11, 176. [Google Scholar] [CrossRef]
- Branzoli, S.; Marini, M.; Guarracini, F.; Pederzolli, C.; D’onghia, G.; Centonze, M.; Pomarolli, C.; La Graffigna, A. Standalone totally thoracoscopi;55:3-81c left appendage clipping: Safe, Simple, Standardized. Ann. Thor. Surg. 2021, 111, 61–63. [Google Scholar] [CrossRef]
- Naylor, A.; Ricco, J.; de Borst, G.; Debus, S.; de Haro, J.; Halliday, A.; Hamilton, G.; Kakisis, J.; Kakkos, S.; Lepidi, S.; et al. Mangement of carotid and vertebral Artery disease. Gidelines of European society of vascular surgery. Eur. J. Vascual Endovasc. Surg. 2018, 55, 3–81. [Google Scholar] [CrossRef]
- Hackam, D.G. Optimal medical management of asymptomatic carotid stenosis. Stroke 2021, 52, 2191–2198. [Google Scholar] [CrossRef]
- Jones, W.; Williams, L.; Meschia, J. Validating the Questionnaire for Verifying stroke free status QSVS by Neurological history and examination. Stroke 2001, 32, 2232–2236. [Google Scholar] [CrossRef]
- Emmert, M.; Puippe, G.; Baumuller, S.; Alkadhi, H.; Landmesser, U.; Plass, A.; Bettex, D.; Scherman, J.; Grunenfelder, J.; Genoni, M.; et al. Safe, effective and durable epicardial left atrial appendage clip occlusion in patients with atrial fibrillation undergoing cardiac surgery: First long term results from a prospective device trial. Eur. J. Cardiothorac. Surg. 2014, 45, 126–131. [Google Scholar] [CrossRef]
- Sinard, T.; Jung, R.; Lehenbauer, K.; Piayda, K.; Pracon, R.; Jackson, G.; Flors-Umanzor, E.; Faroux, L.; Korsholm, K.; Chun, J. Predictors of device related thrombus following percutaneous left atrial appendage occlusion. J. Am. Coll. Cardiol. 2021, 78, 297–313. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.; Frison, L.; Halperin, J.L.; Lane, D.A. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: The HASBLED (Hypertension, Abnormal renal/liver function, Stroke, Bleeding History or predisposition, labile INR, elderly, drugs/alcohol concomitantly. J. Am. Coll. Cardiol. 2011, 2, 173–180. [Google Scholar]
- Friberg, L.; Rosenqvist, M.; Lip, G.Y. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182678 patients with atrial fibrillation:the Swedish atrial fibrillation cohort study. Eur. Heart J. 2012, 33, 1500–1510. [Google Scholar] [CrossRef] [PubMed]
- Elmariah, S.; Doros, G.; Benavente, O.R.; Bhatt, D.; Connolly, S.; Yusuf, S.; Steinhubl, S.; Liu, Y.; Hsieh, W.; Yeh, R. Impact of clopidrogel therapy on mortality and cancer in patients with cardiovascular and cerebrovascular disease: A patient-level meta-analysis. Circ. Cardiovasc. Interv. 2018, 11, e005795. [Google Scholar] [CrossRef]
- Xu, Y.; Shoamenesh, A.; Sculman, S.; Dowlatshahi, D.; Salman, R.A.S.; Moldovan, I.; Wells, P.; Alkheraif, F. Oral anticoagulant re-initiation following intracerebral hemorrhage in non valvular atrial fibrillation: Global survey of the practices of neurologists, neurosurgeons and thrombosis expert. PLoS ONE 2018, 13, e0191137. [Google Scholar]
- Saperas, E.; Videla, S.; Dot, J.; Bayarri, C.; Lobo, B.; Abu-Subho, M.; Malagelada, J. Risk factors for recurrence of acute gastrointestinal bleeding form angiodysplasia. Eur. J. Gastroenterol. Hepatol. 2009, 21, 1333–1339. [Google Scholar] [CrossRef]
- Armengol, J. Anticoagulant treatment due to increased bleeding risk are common and have a high risk of stroke. J. Am. Coll. Cardiol. 2017, 12, 1369–1376. [Google Scholar]
- Perino, A.; Kaiser, D.; Lee, R.; Fan, J.; Askari, M.; Schmitt, S.; Turakia, M. Incidence and outcomes of patients with atrial fibrillation and major bleeding complications: From the TREART-AF study. J. Card. Electrophysiol. 2021, 62, 133–142. [Google Scholar] [CrossRef]
- Blackshear, J.L.; Odell, J.A. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann. Thorac. Surg. 1996, 61, 755–759. [Google Scholar] [CrossRef]
- Wunderlich, N.; Beigel, R.; Swaans, M.; Ho, S.; Siegel, R. Percutaneous Interventions for left atrial appendage exclusion: Options, assessment, and imaging using 2D and 3D Echocardiography. JACC Cardivasc. Imaging 2015, 8, 472–488. [Google Scholar] [CrossRef]
- Li, X.; Wen, S.N.; Li, S.N.; Bai, R.; Liu, N.; Feng, L.; Ruan, Y.; Du, X.; Dong, J.; Ma, C. Over 1 year efficacy and safety of left atrial appendage occlusion versus novel oral anticoagulants for stroke prevention in atrial fibrillation: A systematic review and meta-analysis of randomized controlled trials and observational studies. Heart Rhythm 2016, 13, 1203–1214. [Google Scholar] [CrossRef]
- Lee, R.; Vassallo, P.; Kruse, J.; Malaisrie, S.; Rigolin, V.; Andrei, A.; McCarthy, P. A randomized, prospective pilot comparison of 3 atrial appendage elimination techniques:internal ligation, stapled excision, and surgical excision. J. Thorac. Cardiovasc. Surg. 2016, 152, 1075–1080. [Google Scholar] [CrossRef]
- Gunda, S.; Reddy, M.; Nath, J.; Nagarj, H.; Atoui, M.; Rasek, A.; Ellis, C.; Badhwar, N.; Lee, R.; Dibiase, L.; et al. Impact of periprocedural management in patients undergoing a left atrial appendage ligation using lariat. J. Cardiovasc. Electrophysiol. 2016, 1, 60–64. [Google Scholar] [CrossRef]
- Caliskan, E.; Eberhard, M.; Alkadhi, V.F.H.; Emmert, M. Incidence and characteristics of left atrial appendage stumps after device-enabled epicardial closure. Interact. Cardiovasc. Thorac. Surg. 2019, 29, 663–669. [Google Scholar] [CrossRef]
- Litwinowicz, R.; Bartus, M.; Burysz, M.; Brzezinky, M.; Swalsky, P.; Kapelak, B.; Vuddanda, V.; Lakkireddy, D.; Lee, R.; Trabka, R.; et al. Long term outcomes after left atrial appendage closure with LARIAT device-Stroke risk reduction over five years follow up. PLoS ONE 2018, 13, e0208710. [Google Scholar] [CrossRef]
- Tilz, R.; Fink, T.; Bartus, K.; Wong, T.; Volger, J.; Netwich, K.; Panniker, S.; Fang, Q.; Piorkowsky, C.; Liosis, S.; et al. A collective European experience with left atrial appendage suture ligation using the lariat device. Europace 2020, 22, 924–931. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, M.C.; See, V.Y.; Dawood, M.Y.; Price, M. A review of the LARIAT device: Insight from the cumulative experience. Spingerplus 2015, 4, 522. [Google Scholar] [CrossRef]
- Lempereur, M.; Aminian, A.; Freixa, X.; Gafoor, S.; Shakir, S.; Omran, H.; Beri, S.; Santoro, G.; Kefer, J.; Landmesser, U.; et al. Left atrial appendage occlusion in patients with atrial fibrillation and previous major gastrointestinal bleeding (from the Amplatzer cardiac plug multicenter registry). Am. J. Cardiol. 2017, 120, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Hallas, J.; Dall, M.; Andries, A.; Andersen, B.; Aalikke, C.; Hansen, J.; Andersen, M.; Lassen, A. Use of single and combined antithrombotic therapy and risk of serious upper gastrointestinal bleeding: Population based case control study. BMJ 2006, 33, 726. [Google Scholar] [CrossRef] [PubMed]
- Nikura, R.; Nagata, N.; Yamada, A.; Akiyama, J.; Shimbo, T.; Uemura, N. Recurrence of colonic diverticular bleeding and associated risk factors. Colorectal. Dis. 2021, 14, 302–305. [Google Scholar] [CrossRef]
- Caliskan, E.; Sahin, A.; Yilmaz, M.; Seifert, B.; Hinzpeter, R.; Alkadhi, K.; Cox, J.; Holubec, T.; Reser, D.; Falk, V.; et al. Epicardial left atrial appendage Atriclip occlusion reduces the incidence of stroke in patients with atrial fibrillation undergoing cardiac surgery. Europace 2017, 104, 127–132. [Google Scholar] [CrossRef]
- Salzberg, S.; Grunenfelder, J.; Emmert, M. Left atrial appendage closure to prevent stroke in patients with atrial fibrillation: A call for the heart team approach. Europace 2015, 17, 1880–1881. [Google Scholar] [CrossRef][Green Version]
- Kany, S.; Metzner, A.; Lubos, E.; Kirchof, P. The atrial fibrillation heart team guiding therapy in left atrial appendage occlusion with increasingly complex patients and little evidence. Eur. Heart J. 2021, 43, 1691–1692. [Google Scholar] [CrossRef]
- Pillarisetti, J.; Reddy, Y.; Gunda, S.; Swarup, V.; Lee, R.; Rasekh, H.; Horton, R.; Massumi, A.; Cheng, J.; Barus, K.; et al. Endocardial (watchman) vs epicardial (lariat) left atrial appendage exclusion devices: Understanding the differences in the location and type of leaks and their clinical implications. Heart Rhythm 2015, 12, 1501–1507. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).