Airway Ultrasound for Anesthesia and in Intensive Care Patients—A Narrative Review of the Literature
Abstract
1. Introduction
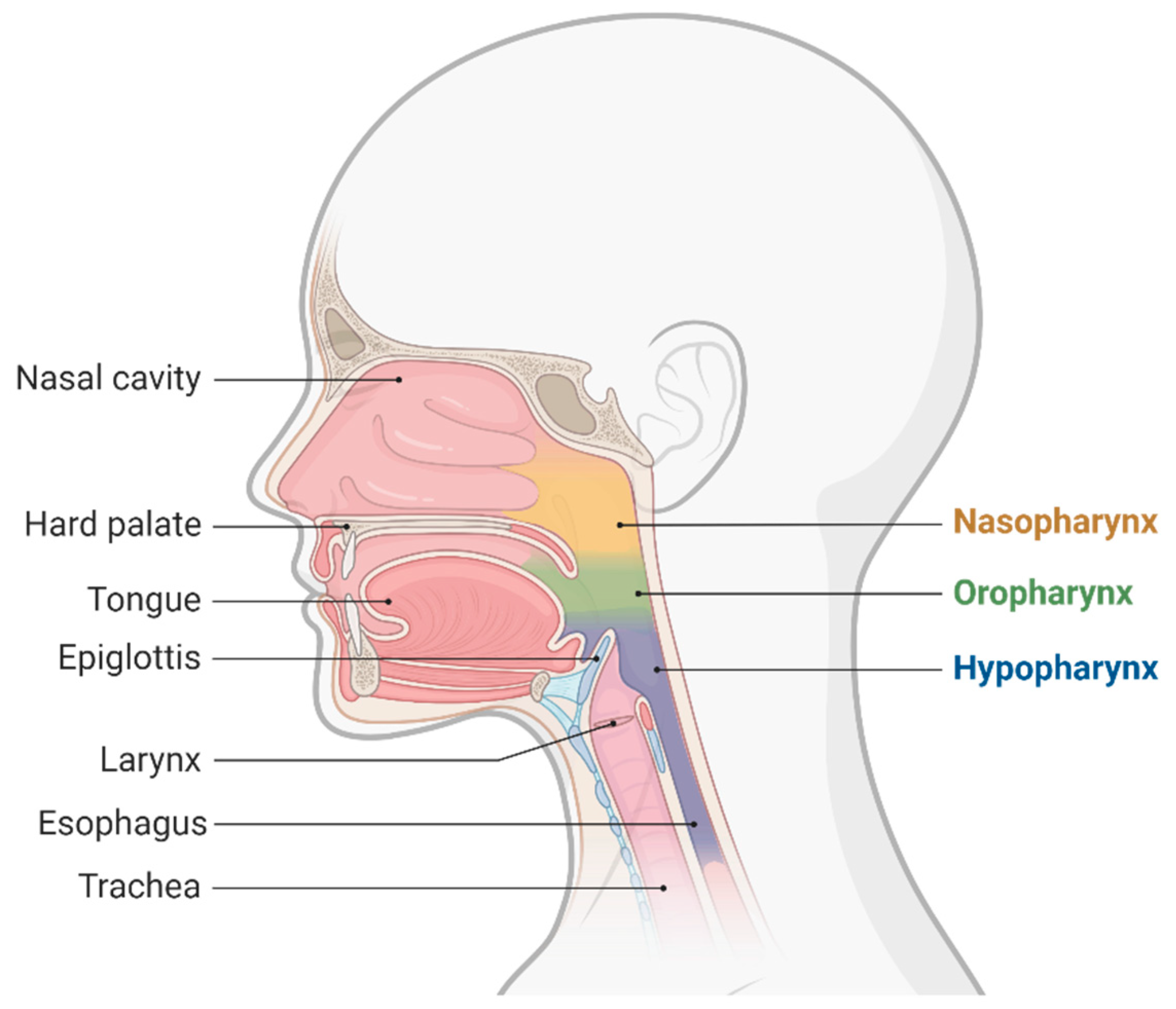
2. Perioperative Ultrasound Airway Evaluation Utility
3. Technical Aspects of an Airway Ultrasound
3.1. Ultrasound Approaches Which Are Practical for the Airway
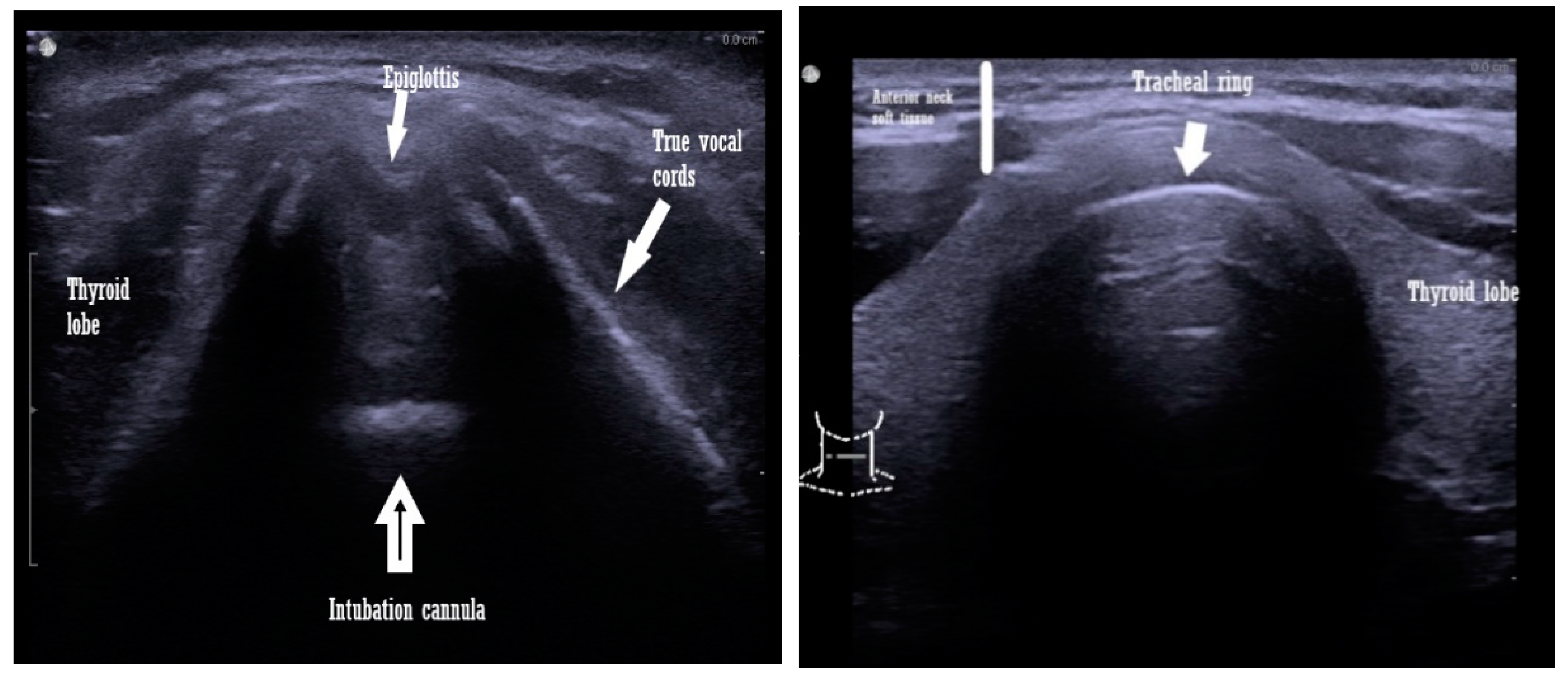
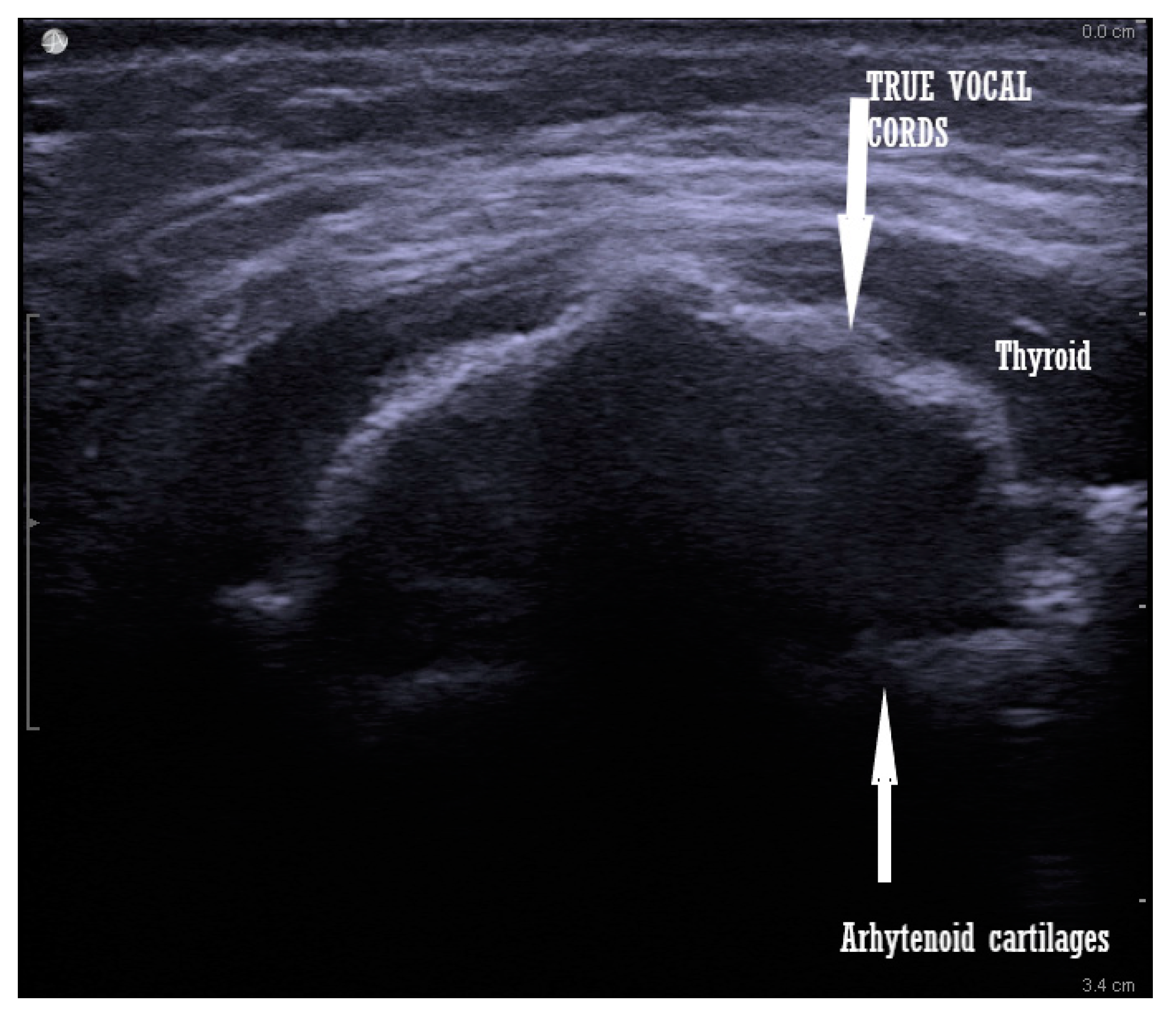
3.2. Airway Measurements Performed by Ultrasound
- Tongue thickness and anterior neck soft tissue, at the level of the hyoid bone, are measured from the skin on the short axis [17].
- Thyrohyoid membrane: from the hyoid bone to the thyroid membrane [17].
- Transverse tracheal air shadow diameter in the subglottic area of the front of the neck: from the mid-front part of the neck, at the level of true vocal cords [18].
- Soft tissue depth at the vocal cords and the suprasternal notch of the distance from the skin to the anterior part of the trachea, determined at three levels: vocal cords, thyroid isthmus, and suprasternal notch. The amount of soft tissue in each zone is considered the average of the amounts of soft tissue obtained in the central axis of the neck and ≈1.5 mm to the left and right of the central axis [19].
- The distance from the epiglottis to the midpoint of the distance between the vocal folds (E-VC) [20].
- Submandibular ultrasound of the hyomental distance ratio: the hyomental distance measured in neutral and in the hyperextended position of the neck [23].
- Tongue volume is the result of the multiplication of the mid-sagittal cross-sectional area, by its width, in a transverse ultrasonogram [23].
- Visibility of the hyoid bone [21].
- Anterior commissure: the shortest distance from the skin to the anterior commissure [24].
- Tongue thickness and the ratio to thyromental distance: measured in the medial sagittal plane, after asking the patient to rest the tip of the tongue on their lower incisors, since the tongue is a dynamic muscle [25].
4. Prediction of a Difficult Airway and Identification of Some Airway Pathologies, with the Aid of Ultrasound
4.1. Determination of the Trachea Size or the Tracheal Potential Abnormalities
4.2. Cuff Pressure and the Trachea Wall Pressure Determination
4.3. Epiglottitis Diagnosis
4.4. Determination of Thyroid Cancer or the Goiter Influence upon the Airway
4.5. Vocal Cord Functionality
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Terkawi, A.; Karakitsos, D.; Elbarbary, M.; Blaivas, M.; Durieux, M.E. Ultrasound for the Anesthesiologists: Present and Future. Sci. World J. 2013, 2013, 683685. [Google Scholar] [CrossRef]
- Lau, B.C.; Motamedi, D.; Luke, A. Use of Pocket-Sized Ultrasound Device in the Diagnosis of Shoulder Pathology. Clin. J. Sport Med. 2018, 30, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Sole, M.L.; Su, X.; Talbert, S.; Penoyer, D.A.; Kalita, S.; Jimenez, E.; Ludy, J.E.; Bennett, M. Evaluation of an Intervention to Maintain Endotracheal Tube Cuff Pressure Within Therapeutic Range. Am. J. Crit. Care 2011, 20, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.S.; Teoh, W.H. Ultrasound identification of the cricothyroid membrane: The new standard in preparing for front-of-neck airway access. Br. J. Anaesth. 2020, 126, 22–27. [Google Scholar] [CrossRef]
- Cook, T.M.; MacDougall-Davis, S.R. Complications and failure of airway management. Br. J. Anaesth. 2012, 109, i68–i85. [Google Scholar] [CrossRef]
- Law, J.A.; Canadian Airway Focus Group; Broemling, N.; Cooper, R.M.; Drolet, P.; Duggan, L.V.; Griesdale, D.E.; Hung, O.R.; Jones, P.M.; Kovacs, G.; et al. The difficult airway with recommendations for management—Part 2—The anticipated difficult airway. Can. J. Anaesth. 2013, 60, 1119–1138. [Google Scholar] [CrossRef] [PubMed]
- Yentis, S.M. Predicting difficult intubation—Worthwhile exercise or pointless ritual? Anaesthesia 2002, 57, 105–109. [Google Scholar] [PubMed]
- Lundstrøm, L.H.; Vester-Andersen, M.; Møller, A.M.; Charuluxananan, S.; L’Hermite, J.; Wetterslev, J. Poor prognostic value of the modified Mallampati score: A meta-analysis involving 177,088 patients. Br. J. Anaesth. 2011, 107, 659–667. [Google Scholar] [CrossRef]
- Das, P.K.; Bellapukonda, S.; Nayak, B.M.; Mallick, M. Can intubate but cannot ventilate! An unexpected event in a child with stridor after accidental aspiration of the potassium permanganate solution. Saudi J. Anaesth. 2020, 14, 272–273. [Google Scholar] [CrossRef]
- Shiga, T.; Wajima, Z.I.; Inoue, T.; Sakamoto, A. Predicting difficult intubation in apparently normal patients: A meta-analysis of bedside screening test performance. J. Am. Soc. Anesthesiol. 2005, 103, 429–437. [Google Scholar] [CrossRef]
- Jain, K.; Yadav, M.; Gupta, N.; Thulkar, S.; Bhatnagar, S. Ultrasonographic assessment of airway. J. Anaesthesiol. Clin. Pharmacol. 2020, 36, 5. [Google Scholar] [PubMed]
- Kristensen, S. Ultrasonography in the management of the airway. Acta Anaesthesiol. Scand. 2011, 55, 1155–1173. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Spychalski, P.; Aszkiełowicz, A.; Mikaszewski, B.; Kobiela, J. Transcutaneous Laryngeal Ultrasound for Vocal Cord Paralysis Assessment in Patients Undergoing Thyroid and Parathyroid Surgery—A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5393. [Google Scholar] [CrossRef] [PubMed]
- Beaudoin, E.L.; Chee, A.; Stather, D.R. Interventional pulmonology: An update for internal medicine physicians. Minerva Med. 2014, 105, 197–209. [Google Scholar] [PubMed]
- Tsui, B.C.; Hui, C.M. Challenges in sublingual airway ultrasound interpretation. Can. J. Anesth. J. Can. D’anesthésie 2009, 56, 393–394. [Google Scholar] [CrossRef] [PubMed]
- Fulkerson, J.S.; Moore, H.M.; Anderson, T.S.; Lowe, R.F. Ultrasonography in the preoperative difficult airway assessment. Int. J. Clin. Monit. Comput. 2016, 31, 513–530. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, S.; Zeger, W.; Schmier, C.; Crum, T.; Craven, A.; Frrokaj, I.; Pang, H.; Shostrom, V. Pilot Study to Determine the Utility of Point-of-care Ultrasound in the Assessment of Difficult Laryngoscopy. Acad. Emerg. Med. 2011, 18, 754–758. [Google Scholar] [CrossRef] [PubMed]
- Aydogmus, M.T.; Erkalp, K.; Sinikoglu, S.N.; Usta, T.A.; Ulger, G.O.; Alagol, A. Is ultrasonic investigation of transverse tracheal air shadow diameter reasonable for evaluation of difficult airway in pregnant women: A prospective comparative study. Pak. J. Med. Sci. 2014, 30, 91. [Google Scholar]
- Ezri, T.; Gewürtz, G.; Sessler, D.I.; Medalion, B.; Szmuk, P.; Hagberg, C.; Susmallian, S. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue*. Anaesthesia 2003, 58, 1111–1114. [Google Scholar] [CrossRef] [PubMed]
- Carsetti, A.; Sorbello, M.; Adrario, E.; Donati, A.; Falcetta, S. Airway Ultrasound as Predictor of Difficult Direct Laryngoscopy: A Systematic Review and Meta-analysis. Anesth. Analg. 2022, 134, 740. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Srirajakalidindi, A.; Ittiara, B.; Apple, L.; Toshniwal, G.; Haber, H. Ultrasonographic modification of Cormack Lehane classification for pre-anesthetic airway assessment. Middle East J. Anaesthesiol. 2012, 21, 835–842. [Google Scholar] [PubMed]
- Pinto, J.; Cordeiro, L.; Pereira, C.; Gama, R.; Fernandes, H.L.; Assunção, J. Predicting difficult laryngoscopy using ultrasound measurement of distance from skin to epiglottis. J. Crit. Care 2016, 33, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Wojtczak, J.A. Submandibular sonography: Assessment of hyomental distances and ratio, tongue size, and floor of the mouth musculature using portable sonography. J. Ultrasound Med. 2012, 31, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Dong, J.; Ding, Y.; Zheng, J. Role of anterior neck soft tissue quantifications by ultrasound in predicting difficult laryngoscopy. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2014, 20, 2343. [Google Scholar]
- Yao, W.; Wang, B. Can tongue thickness measured by ultrasonography predict difficult tracheal intubation? BJA Br. J. Anaesth. 2017, 118, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Feng, Y.K.; Hong, L.; Xie, W.L.; Chen, S.Q.; Yin, P.; Wu, Q.P. Ultrasound for diagnosing new difficult laryngoscopy indicator: A prospective, self-controlled, assessor blinded, observational study. Chin. Med. J. 2019, 132, 2066–2072. [Google Scholar] [CrossRef] [PubMed]
- Koundal, V.; Rana, S.; Thakur, R.; Chauhan, V.; Ekke, S.; Kumar, M. The usefulness of point of care ultrasound (POCUS) in preanaesthetic airway assessment. Indian J. Anaesth. 2019, 63, 1022. [Google Scholar] [PubMed]
- Shih, J.Y.; Lee, L.N.; Wu, H.D.; Yu, C.J.; Wang, H.C.; Chang, Y.L.; Yang, P.C. Sonographic imaging of the trachea. J. Ultrasound Med. 1997, 16, 783–790. [Google Scholar] [CrossRef]
- Kameda, T.; Fujita, M. Point-of-care ultrasound detection of tracheal wall thickening caused by smoke inhalation. Crit. Ultrasound J. 2014, 6, 11. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ye, R.; Cai, F.; Guo, C.; Zhang, X.; Yan, D.; Chen, C.; Bin Chen, B. Assessing the accuracy of ultrasound measurements of tracheal diameter: An in vitro experimental study. BMC Anesthesiol. 2021, 21, 177. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, S.; Farsi, D.; Zare, M.A.; Hajimohammadi, M.; Rezai, M.; Hafezimoghadam, P. Direct ultrasound methods: A confirmatory technique for proper endotracheal intubation in the emergency department. Eur. J. Emerg. Med. 2015, 22, 10–16. [Google Scholar] [CrossRef]
- Shibasaki, M.; Nakajima, Y.; Ishii, S.; Shimizu, F.; Shime, N.; Sessler, D.I. Prediction of pediatric endotracheal tube size by ultrasonography. J. Am. Soc. Anesthesiol. 2010, 113, 819–824. [Google Scholar] [CrossRef]
- Šustić, A.; Miletić, D.; Protić, A.; Ivančić, A.; Cicvarić, T. Can ultrasound be useful for predicting the size of a left double-lumen bronchial tube? Tracheal width as measured by ultrasonography versus computed tomography. J. Clin. Anesth. 2008, 20, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Tessaro, M.O.; Salant, E.P.; Arroyo, A.C.; Haines, L.E.; Dickman, E. Tracheal rapid ultrasound saline test (TRUST) for confirming correct endotracheal tube depth in children. Resuscitation 2015, 89, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Ramsingh, D.; Frank, E.; Haughton, R.; Schilling, J.; Gimenez, K.M.; Banh, E.; Cannesson, M. Auscultation versus point-of-care ultrasound to determine endotracheal versus bronchial intubation: A diagnostic accuracy study. Anesthesiology 2016, 124, 1012–1020. [Google Scholar] [CrossRef] [PubMed]
- Seegobin, R.D.; Van Hasselt, G.L. Endotracheal cuff pressure and tracheal mucosal blood flow: Endoscopic study of effects of four large volume cuffs. BMJ 1984, 288, 965–968. [Google Scholar] [CrossRef] [PubMed]
- Horisberger, T.; Gerber, S.; Bernet, V.; Weiss, M. Measurement of tracheal wall pressure: A comparison of three different in vitro techniques. Anaesthesia 2008, 63, 418–422. [Google Scholar] [CrossRef]
- Brimacombe, J.; Keller, C.; Giampalmo, M.; Sparr, H.J.; Berry, A. Direct measurement of mucosal pressures exerted by cuff and non-cuff portions of tracheal tubes with different cuff volumes and head and neck positions. Br. J. Anaesth. 1999, 82, 708–711. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hung, T.Y.; Li, S.; Chen, P.S.; Wu, L.T.; Yang, Y.J.; Tseng, L.M.; Wang, T.L. Bedside ultrasonography as a safe and effective tool to diagnose acute epiglottitis. Am. J. Emerg. Med. 2011, 29, 359-e1. [Google Scholar] [CrossRef] [PubMed]
- Ko, D.R.; Chung, Y.E.; Park, I.; Lee, H.J.; Park, J.W.; You, J.S.; Kim, S. Use of bedside sonography for diagnosing acute epiglottitis in the emergency department: A preliminary study. J. Ultrasound Med. 2012, 31, 19–22. [Google Scholar] [CrossRef] [PubMed]
- Yamamura, N.; Fukushima, S.; Nakao, K.; Nakahara, M.; Kurozumi, K.; Imabun, S.; Tsujimoto, M. Relation between ultrasonographic and histologic findings of tracheal invasion by differentiated thyroid cancer. World J. Surg. 2002, 26, 1071–1073. [Google Scholar] [CrossRef] [PubMed]
- Chang, D.B.; Yang, P.C.; Kuo, S.H. Diagnosis of intrathoracic goiter based on sonographic findings. AJR. Am. J. Roentgenol. 1992, 159, 671–672. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Sinha, C.; Kumar, A.; Singh, A.K.; Vardhan, H.; Bhavana, K.; Bhar, D. Assessment of functionality of vocal cords using ultrasound before and after thyroid surgery: An observational study. Indian J. Anaesth. 2018, 62, 599. [Google Scholar] [PubMed]
- Shah, M.K.; Ghai, B.; Bhatia, N.; Verma, R.K.; Panda, N.K. ☆ Comparison of transcutaneous laryngeal ultrasound with video laryngoscope for assessing the vocal cord mobility in patients undergoing thyroid surgery. Auris Nasus Larynx 2019, 46, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Ruan, Z.; Ren, R.; Dong, W.; Ma, J.; Xu, Z.; Mao, Y.; Jiang, L. Assessment of vocal cord movement by ultrasound in the ICU. Intensiv. Care Med. 2018, 44, 2145–2152. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.-P.; Lang, B.; Lam, S.; Au, K.-P.; Chan, D.T.-Y.; Kotewall, N.C. Determining the Learning Curve of Transcutaneous Laryngeal Ultrasound in Vocal Cord Assessment by CUSUM Analysis of Eight Surgical Residents: When to Abandon Laryngoscopy. World J. Surg. 2015, 40, 659–664. [Google Scholar] [CrossRef] [PubMed]
- Votruba, J.; Zemanová, P.; Lambert, L.; Vesela, M.M. The role of airway and endobronchial ultrasound in perioperative medicine. BioMed Res. Int. 2015, 2015, 754626. [Google Scholar] [CrossRef] [PubMed]
- Blehar, D.J.; Barton, B.; Gaspari, R.J. Learning Curves in Emergency Ultrasound Education. Acad. Emerg. Med. 2015, 22, 574–582. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lazar, A.E.; Gherghinescu, M.C. Airway Ultrasound for Anesthesia and in Intensive Care Patients—A Narrative Review of the Literature. J. Clin. Med. 2022, 11, 6327. https://doi.org/10.3390/jcm11216327
Lazar AE, Gherghinescu MC. Airway Ultrasound for Anesthesia and in Intensive Care Patients—A Narrative Review of the Literature. Journal of Clinical Medicine. 2022; 11(21):6327. https://doi.org/10.3390/jcm11216327
Chicago/Turabian StyleLazar, Alexandra Elena, and Mircea Constantin Gherghinescu. 2022. "Airway Ultrasound for Anesthesia and in Intensive Care Patients—A Narrative Review of the Literature" Journal of Clinical Medicine 11, no. 21: 6327. https://doi.org/10.3390/jcm11216327
APA StyleLazar, A. E., & Gherghinescu, M. C. (2022). Airway Ultrasound for Anesthesia and in Intensive Care Patients—A Narrative Review of the Literature. Journal of Clinical Medicine, 11(21), 6327. https://doi.org/10.3390/jcm11216327





