Classification of Stiff-Knee Gait Kinematic Severity after Stroke Using Retrospective k-Means Clustering Algorithm
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Gait Analysis
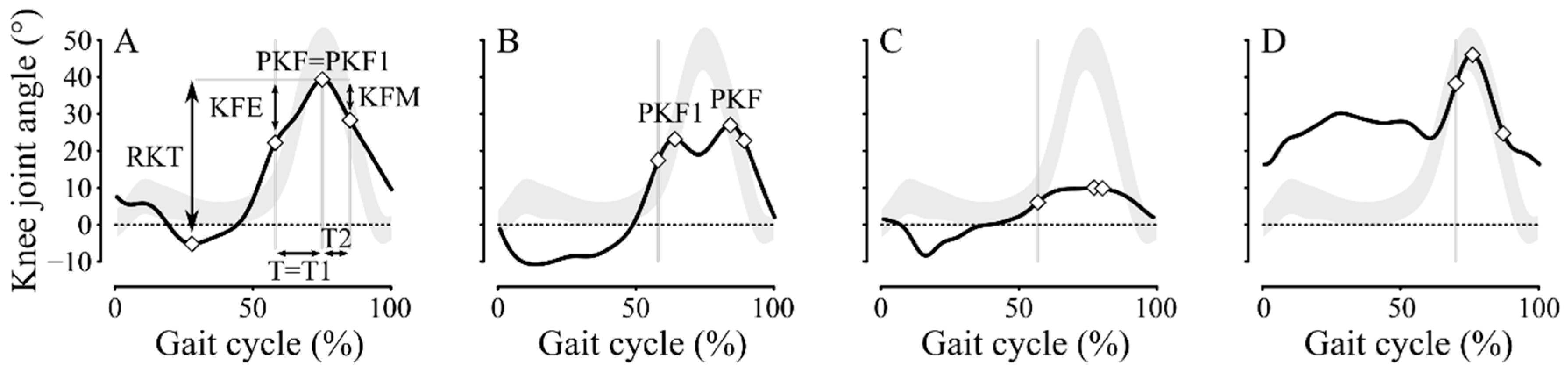
2.3. Kinematic Knee Parameters
2.4. Clustering Procedure, Construct Validity of Classification, and Statistical Analyses
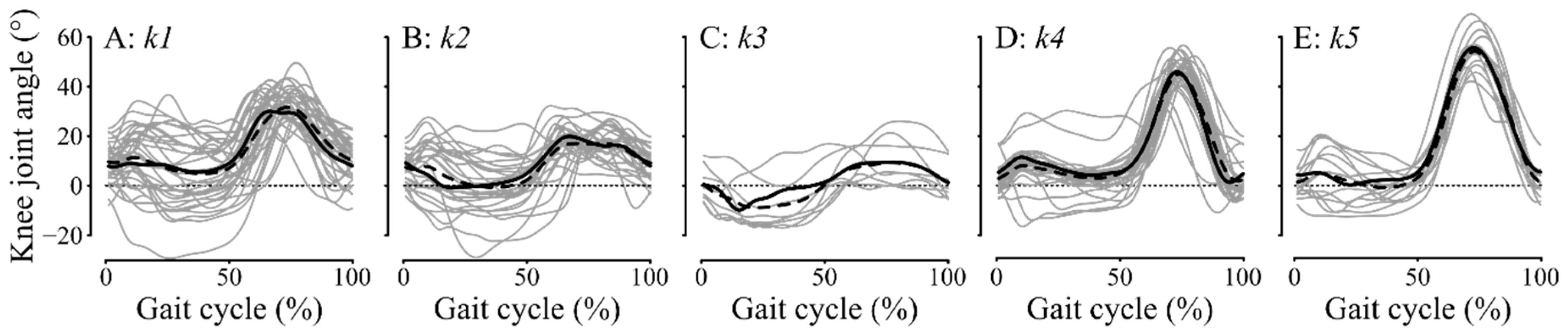
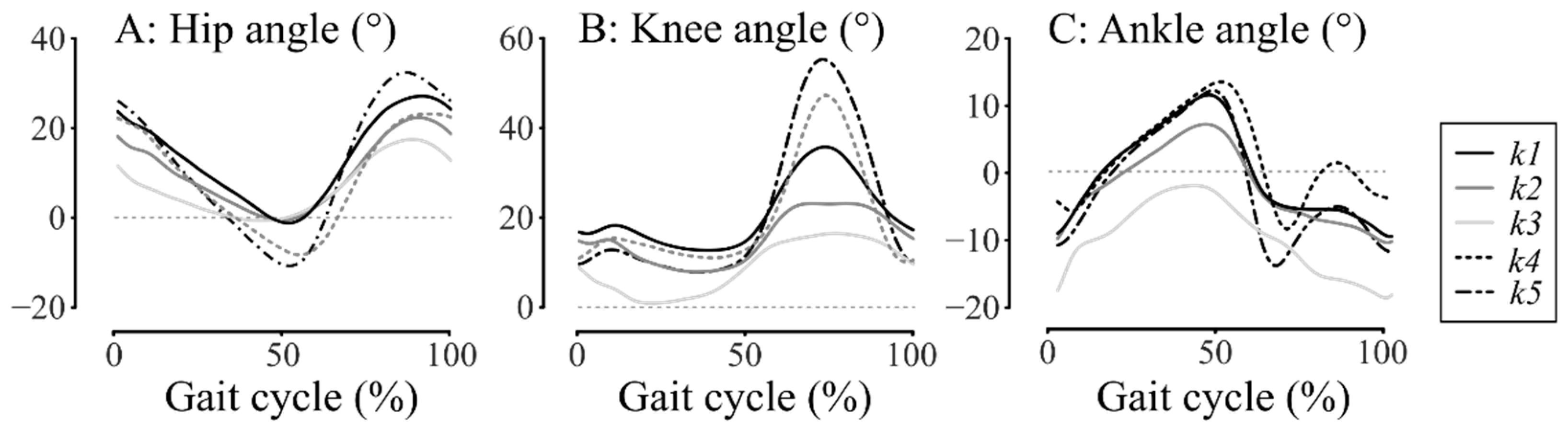
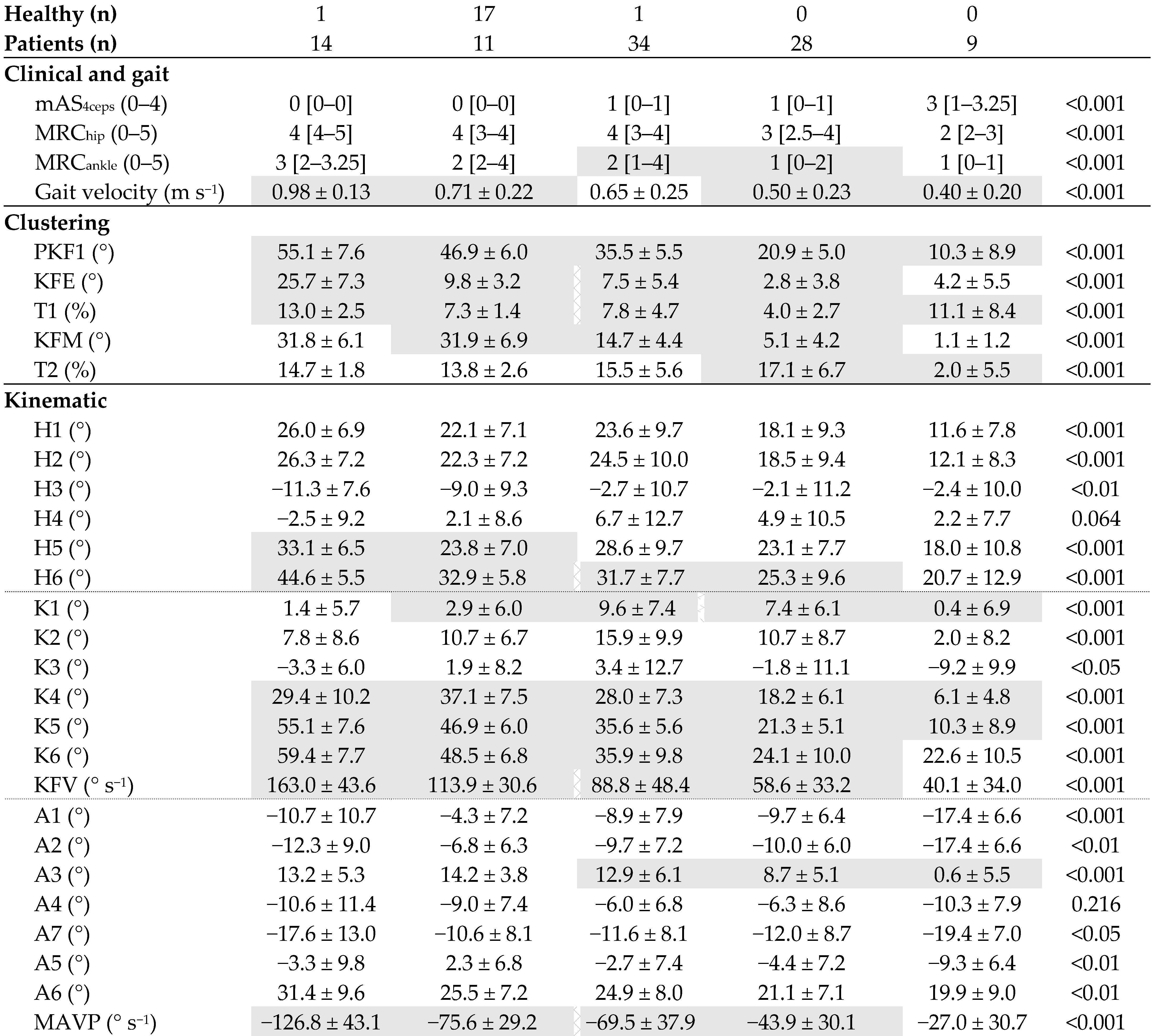
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arene, N.; Hidler, J. Understanding Motor Impairment in the Paretic Lower Limb after a Stroke: A Review of the Literature. Top. Stroke Rehabil. 2009, 16, 346–356. [Google Scholar] [CrossRef]
- Tyson, S.F.; Crow, J.L.; Connell, L.; Winward, C.; Hillier, S. Sensory Impairments of the Lower Limb after Stroke: A Pooled Analysis of Individual Patient Data. Top. Stroke Rehabil. 2013, 20, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Waters, R.L.; Garland, D.E.; Perry, J.; Habig, T.; Slabaugh, P. Stiff-Legged Gait in Hemiplegia: Surgical Correction. J. Bone Jt. Surg. Am. 1979, 61A, 927–933. [Google Scholar] [CrossRef]
- Kerrigan, D.C.; Gronley, J.; Perry, J. Stiff-Legged Gait in Spastic Paresis. Am. J. Phys. Med. Rehabil. 1991, 70, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Chantraine, F.; Detrembleur, C.; Lejeune, T.M. Effect of the Rectus Femoris Motor Branch Block on Post-Stroke Stiff-Legged Gait. Acta Neurol. Belg. 2005, 105, 171–177. [Google Scholar]
- Kerrigan, D.C.; Karvosky, M.E.; Riley, P.O. Spastic Paretic Stiff-Legged Gait: Joint Kinetics. Am. J. Phys. Med. Rehabil. 2001, 80, 244–249. [Google Scholar] [CrossRef]
- De Quervain, I.A.K.; Simon, S.R.; Leurgans, S.; Pease, W.S.; McAllister, D. Gait Pattern in the Early Recovery Period after Stroke. J. Bone Jt. Surg. Am. 1996, 78, 1506–1514. [Google Scholar] [CrossRef]
- Campanini, I.; Merlo, A.; Damiano, B. A Method to Differentiate the Causes of Stiff-Knee Gait in Stroke Patients. Gait Posture 2013, 38, 165–169. [Google Scholar] [CrossRef]
- Goldberg, S.R.; Õunpuu, S.; Arnold, A.S.; Gage, J.R.; Delp, S.L. Kinematic and Kinetic Factors That Correlate with Improved Knee Flexion Following Treatment for Stiff-Knee Gait. J. Biomech. 2006, 39, 689–698. [Google Scholar] [CrossRef]
- Matsuda, F.; Mukaino, M.; Ohtsuka, K.; Tanikawa, H.; Tsuchiyama, K.; Teranishi, T.; Kanada, Y.; Kagaya, H.; Saitoh, E. Analysis of Strategies Used by Hemiplegic Stroke Patients to Achieve Toe Clearance. Jpn. J. Compr. Rehabil. Sci. 2016, 7, 111–118. [Google Scholar] [CrossRef]
- Perry, J. Gait Analysis: Normal and Pathological Function; SLACK: Thorofare, NJ, USA, 1992; ISBN 978-1-55642-192-1. [Google Scholar]
- Sung, D.H.; Bang, H.J. Motor Branch Block of the Rectus Femoris: Its Effectiveness in Stiff-Legged Gait in Spastic Paresis. Arch. Phys. Med. Rehabil. 2000, 81, 910–915. [Google Scholar] [CrossRef] [PubMed]
- Reinbolt, J.A.; Fox, M.D.; Arnold, A.S.; Õunpuu, S.; Delp, S.L. Importance of Preswing Rectus Femoris Activity in Stiff-Knee Gait. J. Biomech. 2008, 41, 2362–2369. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, S.R.; Anderson, F.C.; Pandy, M.G.; Delp, S.L. Muscles That Influence Knee Flexion Velocity in Double Support: Implications for Stiff-Knee Gait. J. Biomech. 2004, 37, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- Tenniglo, M.J.B.; Buurke, J.H.; Prinsen, E.C.; Kottink, A.I.R.; Nene, A.V.; Rietman, J.S. Influence of Functional Electrical Stimulation of the Hamstrings on Knee Kinematics in Stroke Survivors Walking with Stiff Knee Gait. J. Rehabil. Med. 2018, 50, 719–724. [Google Scholar] [CrossRef]
- Stoquart, G.G.; Detrembleur, C.; Palumbo, S.; Deltombe, T.; Lejeune, T.M. Effect of Botulinum Toxin Injection in the Rectus Femoris on Stiff-Knee Gait in People with Stroke: A Prospective Observational Study. Arch. Phys. Med. Rehabil. 2008, 89, 56–61. [Google Scholar] [CrossRef]
- Gross, R.; Robertson, J.; Leboeuf, F.; Hamel, O.; Brochard, S.; Perrouin-Verbe, B. Neurotomy of the Rectus Femoris Nerve: Short-Term Effectiveness for Spastic Stiff Knee Gait. Gait Posture 2017, 52, 251–257. [Google Scholar] [CrossRef]
- Merlo, A.; Campanini, I. Impact of Instrumental Analysis of Stiff Knee Gait on Treatment Appropriateness and Associated Costs in Stroke Patients. Gait Posture 2019, 72, 195–201. [Google Scholar] [CrossRef]
- Sulzer, J.S.; Gordon, K.E.; Dhaher, Y.Y.; Peshkin, M.A.; Patton, J.L. Preswing Knee Flexion Assistance Is Coupled with Hip Abduction in People with Stiff-Knee Gait after Stroke. Stroke 2010, 41, 1709–1714. [Google Scholar] [CrossRef]
- Mazzoli, D.; Giannotti, E.; Manca, M.; Longhi, M.; Prati, P.; Cosma, M.; Ferraresi, G.; Morelli, M.; Zerbinati, P.; Masiero, S.; et al. Electromyographic Activity of the Vastus Intermedius Muscle in Patients with Stiff-Knee Gait after Stroke. A Retrospective Observational Study. Gait Posture 2018, 60, 273–278. [Google Scholar] [CrossRef]
- Robertson, J.V.G.; Pradon, D.; Bensmail, D.; Fermanian, C.; Bussel, B.; Roche, N. Relevance of Botulinum Toxin Injection and Nerve Block of Rectus Femoris to Kinematic and Functional Parameters of Stiff Knee Gait in Hemiplegic Adults. Gait Posture 2009, 29, 108–112. [Google Scholar] [CrossRef]
- Fujita, K.; Kobayashi, Y.; Miaki, H.; Hori, H.; Tsushima, Y.; Sakai, R.; Nomura, T.; Ogawa, T.; Kinoshita, H.; Nishida, T.; et al. Pedaling Improves Gait Ability of Hemiparetic Patients with Stiff-Knee Gait: Fall Prevention during Gait. J. Stroke Cerebrovasc. Dis. 2020, 29, 105035. [Google Scholar] [CrossRef] [PubMed]
- Tenniglo, M.J.; Nederhand, M.J.; Prinsen, E.C.; Nene, A.V.; Rietman, J.S.; Buurke, J.H. Effect of Chemodenervation of the Rectus Femoris Muscle in Adults with a Stiff Knee Gait Due to Spastic Paresis: A Systematic Review with a Meta-Analysis in Patients with Stroke. Arch. Phys. Med. Rehabil. 2014, 95, 576–587. [Google Scholar] [CrossRef]
- Xu, G.; Zhang, Y.; Begg, R. Mining Gait Pattern for Clinical Locomotion Diagnosis Based on Clustering Techniques. In Advanced Data Mining and Applications; Li, X., Zaïane, O.R., Li, Z., Eds.; Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2006; Volume 4093, pp. 296–307. ISBN 978-3-540-37025-3. [Google Scholar]
- Rozumalski, A.; Schwartz, M.H. Crouch Gait Patterns Defined Using K-Means Cluster Analysis Are Related to Underlying Clinical Pathology. Gait Posture 2009, 30, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, L.; Rojhani-Shirazi, Z.; Razeghi, M.; Raeisi-Shahraki, H. Kinematic Cluster Analysis of the Crouch Gait Pattern in Children with Spastic Diplegic Cerebral Palsy Using Sparse K-Means Method. Clin. Biomech. 2021, 81, 105248. [Google Scholar] [CrossRef] [PubMed]
- Kuntze, G.; Nettel-Aguirre, A.; Ursulak, G.; Robu, I.; Bowal, N.; Goldstein, S.; Emery, C.A. Multi-Joint Gait Clustering for Children and Youth with Diplegic Cerebral Palsy. PLoS ONE 2018, 13, e0205174. [Google Scholar] [CrossRef]
- Böhm, H.; Oestreich, C.; Rethwilm, R.; Federolf, P.; Döderlein, L.; Fujak, A.; Dussa, C.U. Cluster Analysis to Identify Foot Motion Patterns in Children with Flexible Flatfeet Using Gait Analysis. A Statistical Approach to Detect Decompensated Pathology? Gait Posture 2019, 71, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Sawacha, Z.; Guarneri, G.; Avogaro, A.; Cobelli, C. A New Classification of Diabetic Gait Pattern Based on Cluster Analysis of Biomechanical Data. J. Diabetes Sci. Technol. 2010, 4, 1127–1138. [Google Scholar] [CrossRef]
- Van Drongelen, S.; Stetter, B.J.; Böhm, H.; Stief, F.; Stein, T.; Meurer, A. Identification of Patients with Similar Gait Compensating Strategies Due to Unilateral Hip Osteoarthritis and the Effect of Total Hip Replacement: A Secondary Analysis. J. Clin. Med. 2021, 10, 2167. [Google Scholar] [CrossRef]
- Alashwal, H.; El Halaby, M.; Crouse, J.J.; Abdalla, A.; Moustafa, A.A. The Application of Unsupervised Clustering Methods to Alzheimer’s Disease. Front. Comput. Neurosci. 2019, 13, 31. [Google Scholar] [CrossRef]
- Kinsella, S.; Moran, K. Gait Pattern Categorization of Stroke Participants with Equinus Deformity of the Foot. Gait Posture 2008, 27, 144–151. [Google Scholar] [CrossRef]
- Kaczmarczyk, K.; Wit, A.; Krawczyk, M.; Zaborski, J. Gait Classification in Post-Stroke Patients Using Artificial Neural Networks. Gait Posture 2009, 30, 207–210. [Google Scholar] [CrossRef] [PubMed]
- Mulroy, S.; Gronley, J.; Weiss, W.; Newsam, C.; Perry, J. Use of Cluster Analysis for Gait Pattern Classification of Patients in the Early and Late Recovery Phases Following Stroke. Gait Posture 2003, 18, 114–125. [Google Scholar] [CrossRef]
- Manca, M.; Ferraresi, G.; Cosma, M.; Cavazzuti, L.; Morelli, M.; Benedetti, M.G. Gait Patterns in Hemiplegic Patients with Equinus Foot Deformity. BioMed. Res. Int 2014, 2014, 939316. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, C.; Moissenet, F. A Multimodal Dataset of Human Gait at Different Walking Speeds Established on Injury-Free Adult Participants. Sci. Data 2019, 6, 111. [Google Scholar] [CrossRef]
- He, Z.; Tang, X.; Yang, X.; Guo, Y.; George, T.J.; Charness, N.; Hem, K.B.Q.; Hogan, W.; Bian, J. Clinical Trial Generalizability Assessment in the Big Data Era: A Review. Clin. Transl. Sci. 2020, 13, 675–684. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Smith, M.B. Interrater Reliability of a Modified Ashworth Scale of Muscle Spasticity. Phys. Ther. 1987, 67, 206–207. [Google Scholar] [CrossRef]
- Medical Research Council. Aids to the Investigation of the Peripheral Nervous System, Memorandum No. 45; Pendragon House: London, UK, 1976; ISBN 0-11-450033-9. [Google Scholar]
- Van Sint Jan, S. Color Atlas of Skeletal Landmark Definitions; Churchill Livingstone/Elsevier: Amsterdam, The Netherlands, 2007; ISBN 0-443-10315-1. [Google Scholar]
- Dumas, R.; Wojtusch, J. Estimation of the Body Segment Inertial Parameters for the Rigid Body Biomechanical Models Used in Motion Analysis. In Handbook of Human Motion; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; pp. 1–31. [Google Scholar]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB Recommendation on Definitions of Joint Coordinate System of Various Joints for the Reporting of Human Joint Motion—Part I: Ankle, Hip, and Spine. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef]
- Forgy, E.W. Cluster Analysis of Multivariate Data: Efficiency versus Interpretability of Classifications. Biometrics 1965, 21, 768–769. [Google Scholar]
- Lloyd, S. Least Squares Quantization in PCM. IEEE Trans. Inf. Theory 1982, 28, 129–137. [Google Scholar] [CrossRef]
- Selim, S.Z.; Ismail, M.A. K-Means-Type Algorithms: A Generalized Convergence Theorem and Characterization of Local Optimality. IEEE Trans. Pattern Anal. Mach. Intell. 1984, PAMI-6, 81–87. [Google Scholar] [CrossRef]
- Tibshirani, R.; Walther, G.; Hastie, T. Estimating the Number of Clusters in a Data Set via the Gap Statistic. J. R. Stat. Soc. Ser. B Stat. Methodol. 2001, 63, 411–423. [Google Scholar] [CrossRef]
- Chantraine, F.; Filipetti, P.; Schreiber, C.; Remacle, A.; Kolanowski, E.; Moissenet, F. Proposition of a Classification of Adult Patients with Hemiparesis in Chronic Phase. PLoS ONE 2016, 11, e0156726. [Google Scholar] [CrossRef] [PubMed]
- Lesko, C.R.; Buchanan, A.L.; Westreich, D.; Edwards, J.K.; Hudgens, M.G.; Cole, S.R. Generalizing Study Results: A Potential Outcomes Perspective. Epidemiology 2017, 28, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Cahan, A.; Cahan, S.; Cimino, J.J. Computer-Aided Assessment of the Generalizability of Clinical Trial Results. Int. J. Med. Inform. 2017, 99, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Caty, G.D.; Detrembleur, C.; Bleyenheuft, C.; Deltombe, T.; Lejeune, T.M. Effect of Simultaneous Botulinum Toxin Injections into Several Muscles on Impairment, Activity, Participation, and Quality of Life among Stroke Patients Presenting with a Stiff Knee Gait. Stroke 2008, 39, 2803–2808. [Google Scholar] [CrossRef]
- Boudarham, J.; Roche, N.; Pradon, D.; Delouf, E.; Bensmail, D.; Zory, R. Effects of Quadriceps Muscle Fatigue on Stiff-Knee Gait in Patients with Hemiparesis. PLoS ONE 2014, 9, e94138. [Google Scholar] [CrossRef]
- Tenniglo, M.J.B.; Nederhand, M.J.; Fleuren, J.F.; Rietman, J.S.; Buurke, J.H.; Prinsen, E.C. Does the Duncan-Ely Test Predict Abnormal Activity of the Rectus Femoris in Stroke Survivors with a Stiff Knee Gait? J. Rehabil. Med. 2021, 54, 637. [Google Scholar] [CrossRef]
- Roche, N.; Boudarham, J.; Hardy, A.; Bonnyaud, C.; Bensmail, B. Use of Gait Parameters to Predict the Effectiveness of Botulinum Toxin Injection in the Spastic Rectus Femoris Muscle of Stroke Patients with Stiff Knee Gait. Eur. J. Phys. Rehabil. Med. 2015, 51, 10. [Google Scholar]
- Guzik, A.; Drużbicki, M.; Wolan-Nieroda, A.; Turolla, A.; Kiper, P. Estimating Minimal Clinically Important Differences for Knee Range of Motion after Stroke. J. Clin. Med. 2020, 9, 3305. [Google Scholar] [CrossRef]
- Lamontagne, A.; Malouin, F.; Richards, C.L.; Dumas, F. Mechanisms of Disturbed Motor Control in Ankle Weakness during Gait after Stroke. Gait Posture 2002, 15, 244–255. [Google Scholar] [CrossRef]
- Akalan, N.E.; Kuchimov, S.; Apti, A.; Temelli, Y.; Nene, A. Weakening Iliopsoas Muscle in Healthy Adults May Induce Stiff Knee Pattern. Acta Orthop. Traumatol. Turc. 2016, 50, 642–648. [Google Scholar] [CrossRef] [PubMed]
- Souissi, H.; Zory, R.; Bredin, J.; Roche, N.; Gerus, P. Co-Contraction around the Knee and the Ankle Joints during Post-Stroke Gait. Eur. J. Phys. Rehabil. Med. 2018, 54, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Horst, F.; Lapuschkin, S.; Samek, W.; Müller, K.-R.; Schöllhorn, W.I. Explaining the Unique Nature of Individual Gait Patterns with Deep Learning. Sci. Rep. 2019, 9, 2391. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | All Patients (n = 96) | Healthy (n = 19) |
|---|---|---|
| Demographic | ||
| Sex (w/m) Age (years) Weight (kg) Height (m) | 41/55 53 ± 12 79 ± 17 1.69 ± 0.08 | 10/9 54 ± 7 73 ± 14 1.74 ± 0.07 |
| Clinical | ||
| Hemiparetic side (l/r) Time since stroke (months) mAS4ceps (0–4) MRChip (0–5) MRCankle (0–5) | 49/47 49 ± 69 0 [0–1] 4 [3–4] 2 [1–3] | NA NA NA NA NA |
| Gait | ||
| Velocity (m s−1) | 0.64 ± 0.28 | 0.59 ± 0.07 |
| K5 (°) | 26 ± 9 | 23 ± 7 |
| Joints | Abbreviation | Description | Units | References |
|---|---|---|---|---|
| Hip | ||||
| H1 | Hip joint angle at initial contact | ° | [32,47] | |
| H2 | Maximum hip flexion during loading phase | ° | [32,47] | |
| H3 | Maximum hip extension in stance phase | ° | [32,47] | |
| H4 | Hip joint angle at toe-off | ° | [32,47] | |
| H5 | Maximum hip flexion in swing phase | ° | [32,47] | |
| H6 | Total hip excursion in sagittal plane | ° | [32,47] | |
| Knee | ||||
| K1 | Knee joint angle at initial contact | ° | [32,47] | |
| K2 | Maximum knee flexion during loading phase | ° | [32,47] | |
| K3 | Maximum knee extension in stance phase | ° | [32,47] | |
| K4 | Knee joint angle at toe-off | ° | [32,47] | |
| K5 | Maximum knee flexion in swing phase | ° | [32,47] | |
| K6 | Total knee excursion in sagittal plane | ° | [32,47] | |
| KFV | Mean knee flexion velocity in preswing phase | ° s−1 | [8] | |
| Ankle | ||||
| A1 | Ankle joint angle at initial contact | ° | [32,47] | |
| A2 | Maximum ankle plantarflexion during loading phase | ° | [32,47] | |
| A3 | Maximum ankle dorsiflexion in stance phase | ° | [32,47] | |
| A4 | Ankle joint angle at toe-off | ° | [32,47] | |
| A5 | Maximum ankle dorsiflexion in swing phase | ° | [32,47] | |
| A6 | Total ankle excursion in sagittal plane | ° | [32,47] | |
| A7 | Maximum ankle plantarflexion in swing phase | ° | [32,47] | |
| MAVP | Mean ankle plantarflexion velocity in preswing phase | ° s−1 | - |
| k1 | k2 | k3 | k4 | k5 | Error/Total (%) | |
|---|---|---|---|---|---|---|
| UKG (Mild) | BKG (Moderate) | FLG (Severe) | Healthy | Non-SKG | ||
| Goldberg index | 30/115 (26.1) | |||||
| 0 | 1 | 0 | 0 | 17 | 1 | |
| 1 | 9 | 0 | 0 | 7 | 14 | |
| 2 | 13 | 5 | 2 | 4 | 0 | |
| 3 | 11 | 12 | 5 | 0 | 0 | |
| 4 | 1 | 11 | 2 | 0 | 0 | |
| CHGC | 7/115 (6.1) | |||||
| G0 | 1 | 0 | 0 | 17 | 1 | |
| GIa | 1 | 0 | 0 | 4 | 4 | |
| GIb | 0 | 0 | 0 | 3 | 9 | |
| GIIa | 16 | 9 | 0 | 1 | 1 | |
| GIIb | 15 | 13 | 4 | 2 | 0 | |
| GIIIa | 1 | 2 | 1 | 0 | 0 | |
| GIIIb | 1 | 4 | 4 | 1 | 0 |
| k5 | k4 | k1 | k2 | k3 | p | |
|---|---|---|---|---|---|---|
| Non-SKG | Healthy | UKG (Mild) | BKG (Moderate) | FLG (Severe) | ||
 | ||||||
| Present SKG Sample | Target Sample(s) [Reference] | Sscore | Gscore | |
|---|---|---|---|---|
| Demographic | 90 | |||
| Sex (% women) | 39 | 45 [18] 30 [52] | 87 77 | |
| Age (years) | 55 ± 11 | 55 ± 14 [18] 57 ± 13 [52] | 100 96 | |
| Weight (kg) | 80 ± 16 | 74 ± 12 [18] 67 ± 11/73 ± 8 [22] | 93 84/91 | |
| Clinical | 72 | |||
| Hemiparetic side (% left) | 45 | 31 [18] 48 [52] | 69 94 | |
| Time since stroke (months) | 54 ± 75 | 83 ± 71 [52] 53 ± 49 [20] | 65 98 | |
| mAS4ceps | 1 [1] | 2 [1]/2 [2,22] 1 [1]/2.5 [1,50] | 50 100/40 | |
| MRChip | 3 [1] | 3 [3,17] | 100 | |
| MRCankle | 1 [2] | 3 [2,51] | 33 | |
| Gait | 95 | |||
| Velocity (m s−1) | 0.56 ± 0.25 | 0.58 ± 0.25 [53] 0.57 ± 0.20/0.54 ± 0.18 [22] | 97 98/96 | |
| K5 (°) | 25 ± 10 | 25 ± 9 [8] 30 ± 12 [18] | 100 83 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chantraine, F.; Schreiber, C.; Pereira, J.A.C.; Kaps, J.; Dierick, F. Classification of Stiff-Knee Gait Kinematic Severity after Stroke Using Retrospective k-Means Clustering Algorithm. J. Clin. Med. 2022, 11, 6270. https://doi.org/10.3390/jcm11216270
Chantraine F, Schreiber C, Pereira JAC, Kaps J, Dierick F. Classification of Stiff-Knee Gait Kinematic Severity after Stroke Using Retrospective k-Means Clustering Algorithm. Journal of Clinical Medicine. 2022; 11(21):6270. https://doi.org/10.3390/jcm11216270
Chicago/Turabian StyleChantraine, Frédéric, Céline Schreiber, José Alexandre Carvalho Pereira, Jérôme Kaps, and Frédéric Dierick. 2022. "Classification of Stiff-Knee Gait Kinematic Severity after Stroke Using Retrospective k-Means Clustering Algorithm" Journal of Clinical Medicine 11, no. 21: 6270. https://doi.org/10.3390/jcm11216270
APA StyleChantraine, F., Schreiber, C., Pereira, J. A. C., Kaps, J., & Dierick, F. (2022). Classification of Stiff-Knee Gait Kinematic Severity after Stroke Using Retrospective k-Means Clustering Algorithm. Journal of Clinical Medicine, 11(21), 6270. https://doi.org/10.3390/jcm11216270





