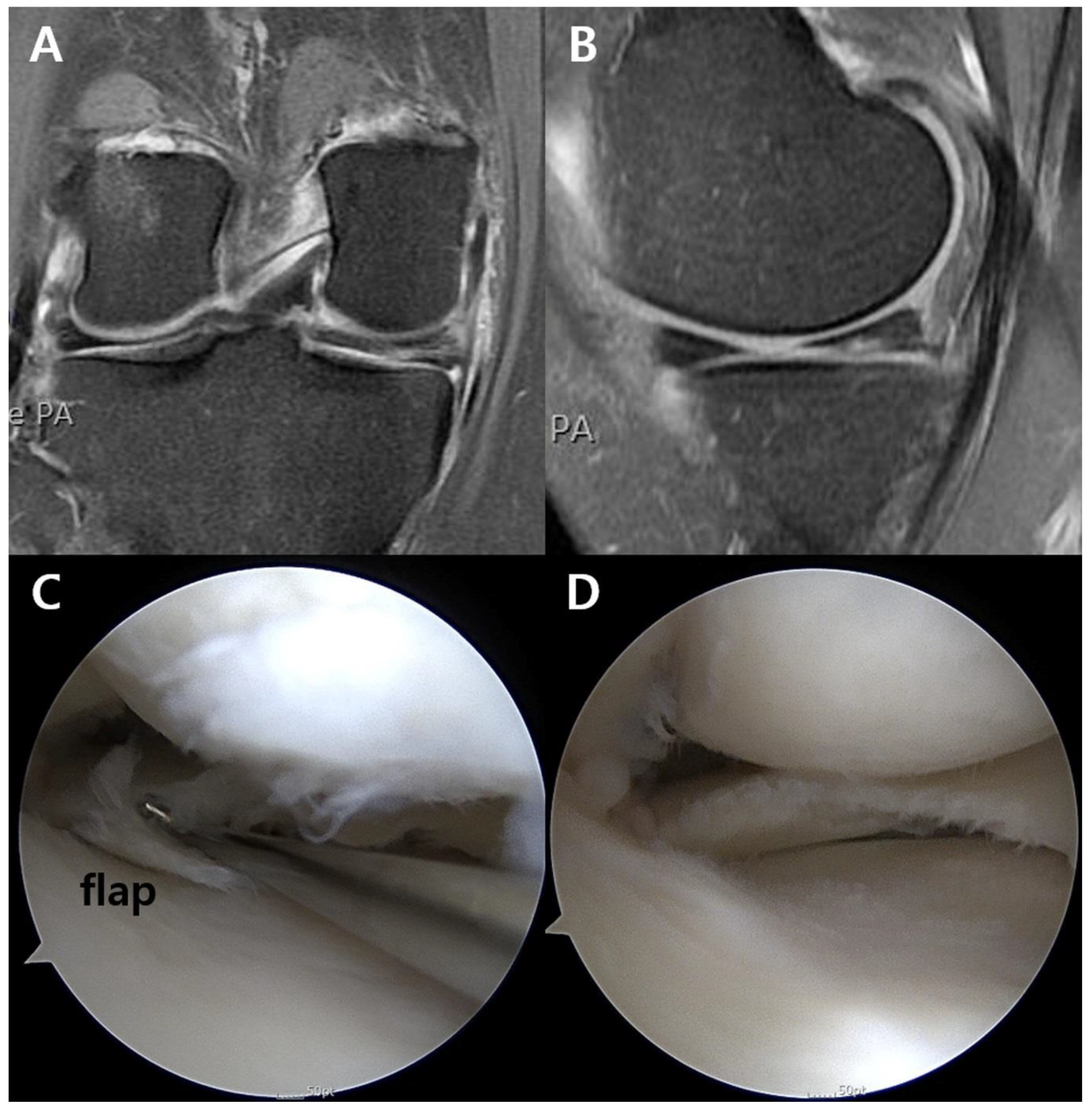
Hidden Unstable Flap Should Be Suspected in Treating Intractable Pain from Medial Meniscus Horizontal Tear
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
Logistic Regression Analyses Regarding Unstable Flap
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beaufils, P.; Pujol, N. Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol. Surg. Res. 2017, 103, S237–S244. [Google Scholar] [CrossRef] [PubMed]
- Abram, S.G.F.; Hopewell, S.; Monk, A.P.; Bayliss, L.E.; Beard, D.J.; Price, A.J. Arthroscopic partial meniscectomy for meniscal tears of the knee: A systematic review and meta-analysis. Br. J. Sports Med. 2020, 54, 652–663. [Google Scholar] [CrossRef] [PubMed]
- Herrlin, S.V.; Wange, P.O.; Lapidus, G.; Hållander, M.; Werner, S.; Weidenhielm, L. Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A five year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.N.; Brophy, R.H.; Chaisson, C.E.; de Chaves, L.; Cole, B.J.; Dahm, D.L.; Donnell-Fink, L.A.; Guermazi, A.; Haas, A.K.; Jones, M.H.; et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N. Engl. J. Med. 2013, 368, 1675–1684. [Google Scholar] [CrossRef]
- Kise, N.J.; Risberg, M.A.; Stensrud, S.; Ranstam, J.; Engebretsen, L.; Roos, E.M. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: Randomised controlled trial with two year follow-up. BMJ 2016, 354, i3740. [Google Scholar] [CrossRef]
- Yim, J.-H.; Seon, J.-K.; Song, E.-K.; Choi, J.-I.; Kim, M.-C.; Lee, K.-B.; Seo, H.-Y. A Comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am. J. Sports Med. 2013, 41, 1565–1570. [Google Scholar] [CrossRef]
- van de Graaf, V.A.; Noorduyn, J.C.A.; Willigenburg, N.W.; Butter, I.K.; de Gast, A.; Mol, B.W.; Saris, D.B.F.; Twisk, J.W.R.; Poolman, R.W.; ESCAPE Research Group. Effect of early surgery vs physical therapy on knee function among patients with nonobstructive meniscal tears: The ESCAPE randomized clinical trial. JAMA 2018, 320, 1328–1337. [Google Scholar] [CrossRef]
- Thorlund, J.B.; Juhl, C.B.; Roos, E.M.; Lohmander, L.S. Arthroscopic surgery for degenerative knee: Systematic review and meta-analysis of benefits and harms. BMJ 2015, 350, h2747. [Google Scholar] [CrossRef]
- Kim, J.G.; Lee, S.-Y.; Chay, S.; Lim, H.C.; Bae, J.-H. Arthroscopic meniscectomy for medial meniscus horizontal cleavage tears in patients under age 45. Knee Surg. Relat. Res 2016, 28, 225–232. [Google Scholar] [CrossRef]
- Noorduyn, J.C.A.; van de Graaf, V.A.; Willigenburg, N.W.; Scholten-Peeters, G.G.M.; Kret, E.J.; van Dijk, R.A.; Buchbinder, R.; Hawker, G.A.; Coppieters, M.W.; Poolman, R.W.; et al. Effect of physical therapy vs arthroscopic partial meniscectomy in people with degenerative meniscal tears: Five-year follow-up of the ESCAPE randomized clinical Trial. JAMA Netw. Open 2022, 5, e2220394. [Google Scholar] [CrossRef] [PubMed]
- Lyman, S.; Oh, L.S.; Reinhardt, K.R.; Mandl, L.A.; Katz, J.N.; Levy, B.A.; Marx, R.G. Surgical decision making for arthroscopic partial meniscectomy in patients aged over 40 years. Arthroscopy 2012, 28, 492–501.e1. [Google Scholar] [CrossRef] [PubMed]
- Jevsevar, D.S.; Yates, A.J.; Sanders, J.O. Arthroscopic partial meniscectomy for degenerative meniscal tear. N. Engl. J. Med. 2014, 370, 1260. [Google Scholar] [CrossRef] [PubMed]
- Krych, A.J.; Carey, J.L.; Marx, R.G.; Dahm, D.L.; Sennett, B.J.; Stuart, M.J.; Levy, B.A. Does arthroscopic knee surgery work? Arthroscopy 2014, 30, 544–545. [Google Scholar] [CrossRef] [PubMed]
- Lefevre, N.; Klouche, S.; Sezer, H.B.; Gerometta, A.; Bohu, Y.; Lefevre, E. The “sleeper’s sign” is valid and suggestive of a medial sub-meniscal flap tear. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 51–58. [Google Scholar] [CrossRef]
- Herschmiller, T.A.; Anderson, J.A.; Garrett, W.E.; Taylor, D.C. The trapped medial meniscus tear: An examination maneuver helps predict arthroscopic findings. Orthop. J. Sports Med. 2015, 3, 2325967115583954. [Google Scholar] [CrossRef]
- Becker, R.; Bernard, M.; Scheffler, S.; Kopf, S. Treatment of degenerative meniscal lesions: From eminence to evidence-based medicine. Orthopade 2017, 46, 808–821. [Google Scholar] [CrossRef]
- Vande Berg, B.C.; Malghem, J.; Poilvache, P.; Maldague, B.; Lecouvet, F.E. Meniscal Tears with fragments displaced in notch and recesses of knee: MR imaging with arthroscopic comparison. Radiology 2005, 234, 842–850. [Google Scholar] [CrossRef]
- Lance, V.; Heilmeier, U.R.; Joseph, G.B.; Steinbach, L.; Ma, B.; Link, T.M. MR imaging characteristics and clinical symptoms related to displaced meniscal flap tears. Skeletal Radiol. 2015, 44, 375–384. [Google Scholar] [CrossRef]
- Davis, K.W.; Rosas, H.G.; Graf, B.K. Magnetic resonance imaging and arthroscopic appearance of the menisci of the knee. Clin. Sports Med. 2013, 32, 449–475. [Google Scholar] [CrossRef]
- Lecas, L.K.; Helms, C.A.; Kosarek, F.J.; Garret, W.E. Inferiorly displaced flap tears of the medial meniscus: MR appearance and clinical significance. AJR Am. J. Roentgenol. 2000, 174, 161–164. [Google Scholar] [CrossRef]
- Pihl, K.; Ensor, J.; Peat, G.; Englund, M.; Lohmander, S.; Jørgensen, U.; Nissen, N.; Fristed, J.V.; Thorlund, J.B. Wild goose chase—No predictable patient subgroups benefit from meniscal surgery: Patient-reported outcomes of 641 patients 1 year after surgery. Br. J. Sports Med. 2020, 54, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Noorduyn, J.C.A.; van de Graaf, V.A.; Willigenburg, N.W.; Scholten-Peeters, G.G.M.; Mol, B.W.; Heymans, M.W.; Coppieters, M.W.; Poolman, R.W.; ESCAPE Research Group. An individualized decision between physical therapy or surgery for patients with degenerative meniscal tears cannot be based on continuous treatment selection markers: A marker-by-treatment analysis of the ESCAPE study. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1937–1948. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Li, X.; Lu, Z.; Koh, J.L.; Wang, C.; Wang, P.; Shao, X.; Wang, J. Arthroscopic repair of degenerative medial meniscus tears in patients aged over 45 years resulted in favorable clinical outcomes and low clinical failure rates at a minimum 2-year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2022. preprint. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, H.; Matsumoto, K.; Sengoku, M.; Yoshioka, H.; Akiyama, H. Arthroscopic repair of horizontal cleavage meniscus tears provides good clinical outcomes in spite of poor meniscus healing. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3474–3480. [Google Scholar] [CrossRef]
- Wadhwa, V.; Omar, H.; Coyner, K.; Khazzam, M.; Robertson, W.; Chhabra, A. ISAKOS classification of meniscal tears-illustration on 2D and 3D isotropic spin echo MR imaging. Eur. J. Radiol. 2016, 85, 15–24. [Google Scholar] [CrossRef]
- Yulish, B.S.; Montanez, J.; Goodfellow, D.B.; Bryan, P.J.; Mulopulos, G.P.; Modic, M.T. Chondromalacia patellae: Assessment with MR imaging. Radiology 1987, 164, 763–766. [Google Scholar] [CrossRef]
- Song, J.-H.; Bin, S.-I.; Kim, J.-M.; Lee, B.-S. Cartilage status, rather than chronologic age, determines the outcomes of open wedge high tibial osteotomy: A cartilage status-matched cohort study. Arthroscopy 2021, 37, 2915–2922. [Google Scholar] [CrossRef]
- Peterfy, C.G.; Guermazi, A.; Zaim, S.; Tirman, P.F.J.; Miaux, Y.; White, D.; Kothari, M.; Lu, Y.; Fye, K.; Zhao, S.; et al. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthr. Cartil. 2004, 12, 177–190. [Google Scholar] [CrossRef]
- Beaufils, P.; Becker, R.; Kopf, S.; Englund, M.; Verdonk, R.; Ollivier, M.; Seil, R. Surgical management of degenerative meniscus lesions: The 2016 ESSKA meniscus consensus. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 335–346. [Google Scholar] [CrossRef]
- Christoforakis, J.; Pradhan, R.; Sanchez-Ballester, J.; Hunt, N.; Strachan, R.K. Is there an association between articular cartilage changes and degenerative meniscus tears? Arthroscopy 2005, 21, 1366–1369. [Google Scholar] [CrossRef]
- Englund, M. Meniscal tear—A feature of osteoarthritis. Acta Orthop. Scand. Suppl. 2004, 75, 1–45. [Google Scholar] [PubMed]
- Beamer, B.S.; Walley, K.C.; Okajima, S.; Manoukian, O.S.; Perez-Viloria, M.; DeAngelis, J.P.; Ramappa, A.J.; Nazarian, A. Changes in contact area in meniscus horizontal cleavage tears subjected to repair and resection. Arthroscopy 2017, 33, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, T.; Gale, D.; Dewire, P.; Totterman, S.; Gale, M.E.; McLaughlin, S.; Einhorn, T.A.; Felson, D.T. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J. Bone Joint Surg. Am. 2003, 85, 4–9. [Google Scholar] [CrossRef]
- van de Graaf, V.A.; Bloembergen, C.H.; Willigenburg, N.W.; Noorduyn, J.C.A.; Saris, D.B.; Harris, I.A.; Poolman, R.W.; ESCAPE Research Group. Can even experienced orthopaedic surgeons predict who will benefit from surgery when patients present with degenerative meniscal tears? A survey of 194 orthopaedic surgeons who made 3880 predictions. Br. J. Sports Med. 2020, 54, 354–359. [Google Scholar] [CrossRef] [PubMed]

| Overall | Flap Group (n = 45) | Non-Flap Group (n = 20) | p Value | |
|---|---|---|---|---|
| Age, yr a | 52.2 ± 12.6 | 49.6 ± 12.8 | 57.7 ± 11.7 | 0.036 |
| Male/Female, n | 29/36 | 21/24 | 8/12 | 0.788 |
| BMI, kg/m2 a | 24.8 ± 6.1 | 24.4 ± 3.9 | 25.8 ± 9.6 | 0.394 |
| Lower limb alignment, deg a, b | 2.7 ± 2.7 | 2.3 ± 2.8 | 3.6 ± 2.4 | 0.116 |
| Trauma history, n | 29 | 22 | 7 | 0.418 |
| Mechanical symptom, n | 50 | 34 | 16 | 0.761 |
| Symptom duration, month a | 13.0 ± 5.8 | 9.3 ± 4.4 | 20.9 ± 11.3 | 0.017 |
| VAS score a | 5.9 ± 2.4 | 6.0 ± 2.5 | 5.8 ± 2.4 | 0.793 |
| Lysholm score a | 67.7 ± 17.6 | 65.9 ± 19.5 | 71.6 ± 11.9 | 0.284 |
| High-grade cartilage wear c | ||||
| Medial femoral condyle | 8 | 2 | 6 | 0.008 |
| Medial tibial plateau | 5 | 1 | 4 | 0.028 |
| Subchondral BML | 7 | 2 | 5 | 0.025 |
| p Value | Exp(β) Coefficient (95% CI) | |||
|---|---|---|---|---|
| Univariate | Multivariate | Univariate | Multivariate | |
| Age | 0.046 | 0.258 | 0.94 (0.89–0.99) | 0.96 (0.90–1.03) |
| Sex | 0.618 | 1.31 (0.45–3.82) | ||
| BMI | 0.409 | 0.97 (0.89–1.05) | ||
| Lower limb alignment | 0.119 | 0.83 (0.65–1.05) | ||
| Trauma history | 0.301 | 1.78 (0.60–5.28) | ||
| Mechanical symptom | 0.695 | 0.77 (0.21–2.81) | ||
| Symptom duration | 0.028 | 0.026 | 0.99 (0.98–0.99) | 0.99 (0.98–0.99) |
| VAS score | 0.788 | 1.04 (0.81–1.33) | ||
| Lysholm score | 0.281 | 0.98 (0.94–1.02) | ||
| High-grade cartilage wear a | ||||
| Medial femoral condyle | 0.011 | 0.017 | 0.11 (0.02–0.60) | 0.06 (0.01–0.61) |
| Medial tibial plateau | 0.038 | 0.95 | 0.09 (0.01–0.88) | 1.00 (0.99–1.00) |
| Subchondral BML | 0.027 | 0.187 | 0.14 (0.02–0.80) | 0.25 (0.03–1.98) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.M.; Joo, Y.B.; An, B.K.; Song, J.-H. Hidden Unstable Flap Should Be Suspected in Treating Intractable Pain from Medial Meniscus Horizontal Tear. J. Clin. Med. 2022, 11, 6245. https://doi.org/10.3390/jcm11216245
Kim YM, Joo YB, An BK, Song J-H. Hidden Unstable Flap Should Be Suspected in Treating Intractable Pain from Medial Meniscus Horizontal Tear. Journal of Clinical Medicine. 2022; 11(21):6245. https://doi.org/10.3390/jcm11216245
Chicago/Turabian StyleKim, Young Mo, Yong Bum Joo, Byung Kuk An, and Ju-Ho Song. 2022. "Hidden Unstable Flap Should Be Suspected in Treating Intractable Pain from Medial Meniscus Horizontal Tear" Journal of Clinical Medicine 11, no. 21: 6245. https://doi.org/10.3390/jcm11216245
APA StyleKim, Y. M., Joo, Y. B., An, B. K., & Song, J.-H. (2022). Hidden Unstable Flap Should Be Suspected in Treating Intractable Pain from Medial Meniscus Horizontal Tear. Journal of Clinical Medicine, 11(21), 6245. https://doi.org/10.3390/jcm11216245





