Multivessel versus Culprit-Only Percutaneous Coronary Intervention in Patients with Non-ST-Elevation Acute Coronary Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Source of Study Data
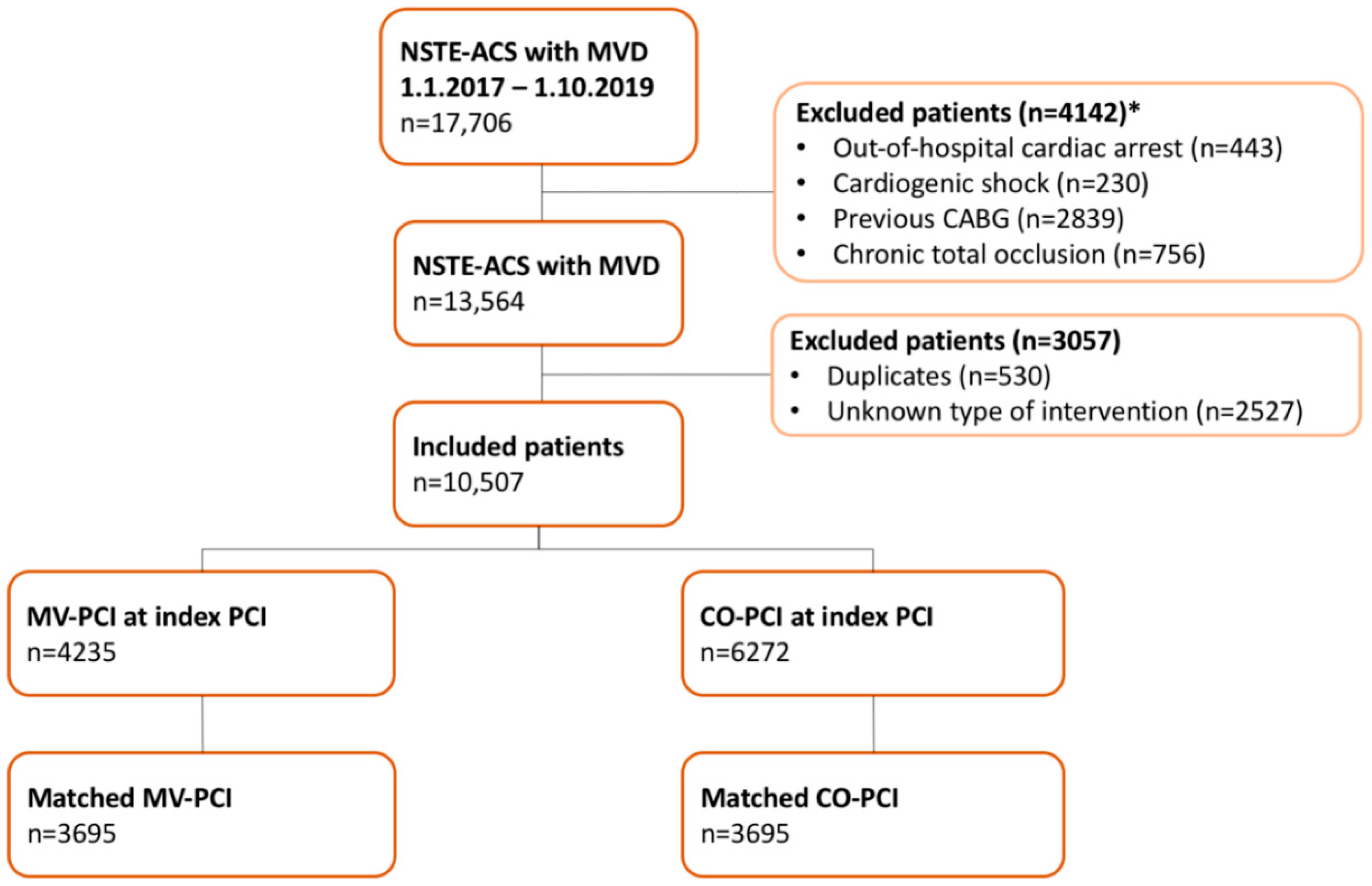
2.2. Study Population
2.3. Study Design
2.4. Outcomes
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
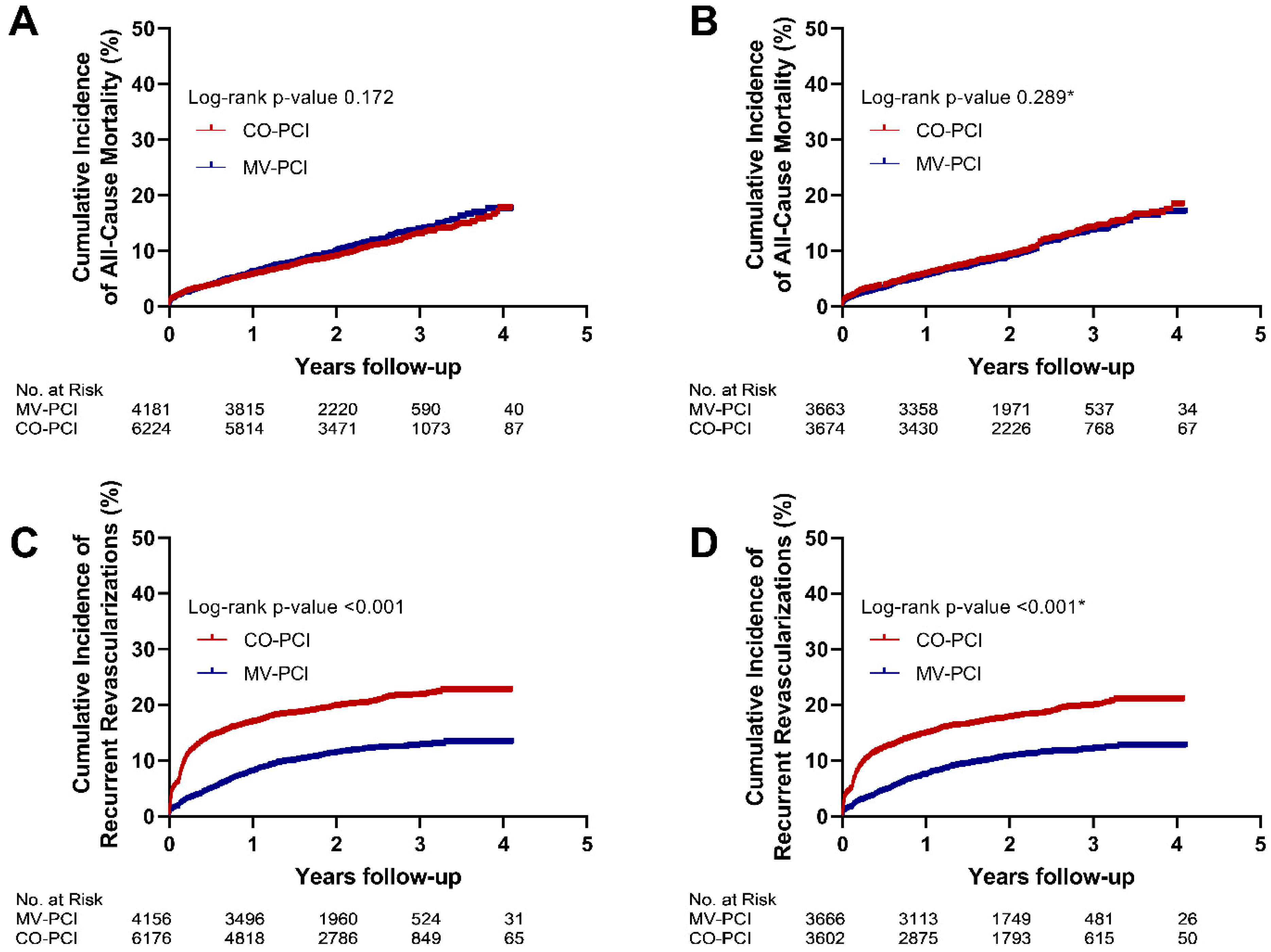
3.2. Outcome in the Overall Cohort (Crude Data)
3.3. Outcome in the Propensity Score–Matched Cohort
3.4. Predictors of All-Cause Mortality and Reinterventions
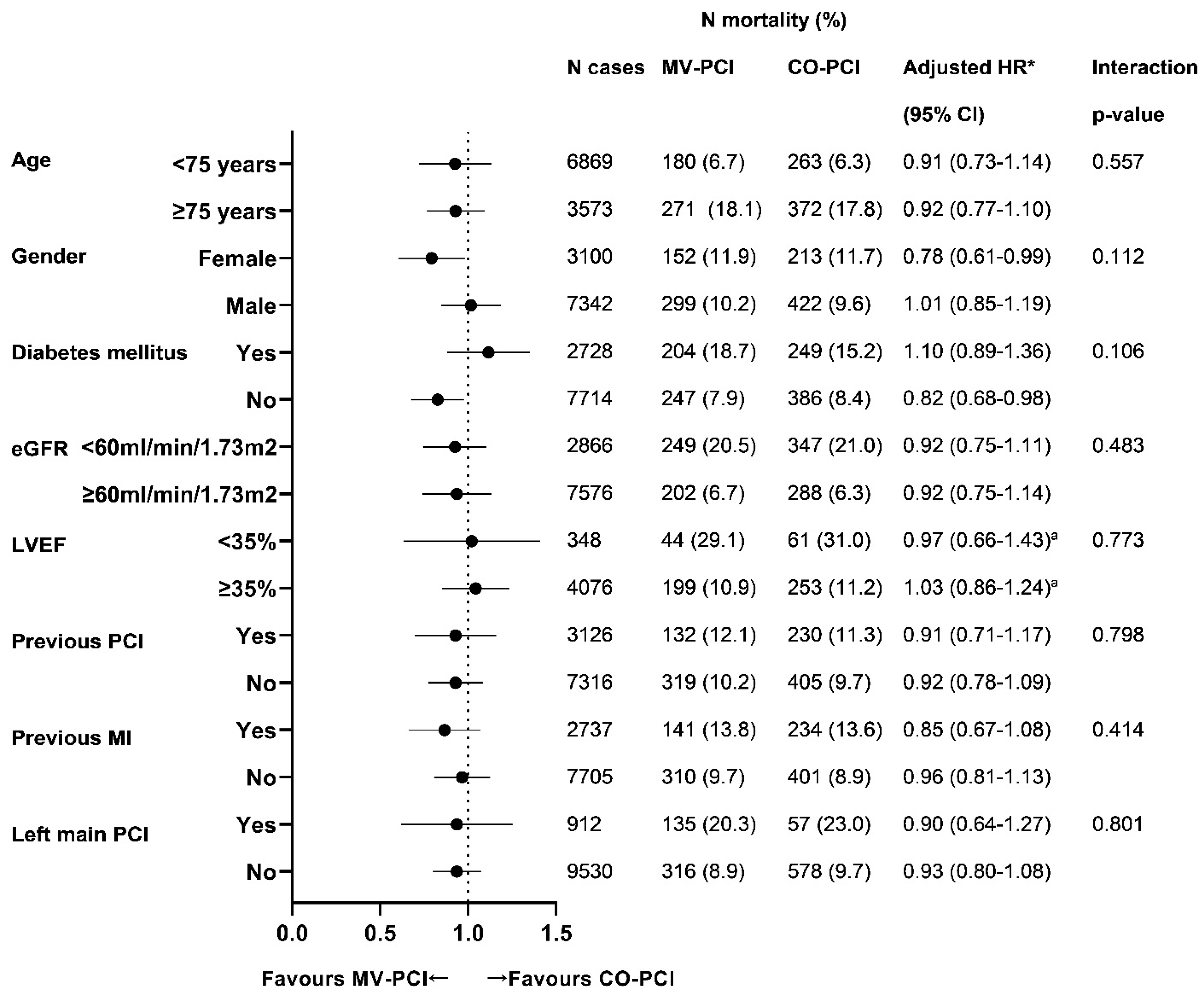
3.5. Subgroup Analysis on All-Cause Mortality and Reinterventions
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sorajja, P.; Gersh, B.J.; Cox, D.A.; McLaughlin, M.G.; Zimetbaum, P.; Costantini, C.; Stuckey, T.; Tcheng, J.E.; Mehran, R.; Lansky, A.J.; et al. Impact of multivessel disease on reperfusion success and clinical out-comes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur. Heart J. 2007, 28, 1709–1716. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef] [PubMed]
- Writing Committee Members; Lawton, J.S.; Tamis-Holland, J.E.; Bangalore, S.; Bates, E.R.; Beckie, T.M.; Bischoff, J.M.; Bittl, J.A.; Cohen, M.G.; DiMaio, J.M.; et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2022, 79, 197–215. [Google Scholar] [CrossRef]
- Wald, D.S.; Morris, J.K.; Wald, N.J.; Chase, A.J.; Edwards, R.J.; Hughes, L.O.; Berry, C.; Oldroyd, K.G.; PRAMI Investigators. Randomized Trial of Preventive Angioplasty in Myocardial Infarction. N. Engl. J. Med. 2013, 369, 1115–1123. [Google Scholar] [CrossRef]
- Kelly, D.J.; McCann, G.P.; Blackman, D.; Curzen, N.P.; Dalby, M.; Greenwood, J.P.; Fairbrother, K.; Shipley, L.; Kelion, A.; Heatherington, S.; et al. Complete Versus culprit-Lesion only PRimary PCI Trial (CVLPRIT): A multicentre trial testing management strategies when multivessel disease is detected at the time of primary PCI: Rationale and design. EuroIntervention 2013, 8, 1190–1198. [Google Scholar] [CrossRef]
- Engstrom, T.; Kelbaek, H.; Helqvist, S.; Hofsten, D.E.; Klovgaard, L.; Holmvang, L.; Jorgensen, E.; Pedersen, F.; Saunamaki, K.; Clemmensen, P.; et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANA-MI-3-PRIMULTI): An open-label, randomised controlled trial. Lancet 2015, 386, 665–671. [Google Scholar] [CrossRef]
- Rasoul, S.; Van Ommen, V.; Vainer, J.; Ilhan, M.; Veenstra, L.; Erdem, R.; Ruiters, L.; Theunissen, R.; Hoorntje, J. Multivessel revascularisation versus infarct-related artery only revascularisation during the index primary PCI in STEMI patients with multivessel disease: A meta-analysis. Neth. Heart J. 2015, 23, 224–231. [Google Scholar] [CrossRef]
- Smits, P.C.; Abdel-Wahab, M.; Neumann, F.-J.; Klerk, B.M.B.-D.; Lunde, K.; Schotborgh, C.E.; Piroth, Z.; Horak, D.; Wlodarczak, A.; Ong, P.J.; et al. Fractional Flow Reserve–Guided Multivessel Angioplasty in Myocardial Infarction. N. Engl. J. Med. 2017, 376, 1234–1244. [Google Scholar] [CrossRef]
- Mehta, S.R.; Wood, D.A.; Storey, R.F.; Mehran, R.; Bainey, K.R.; Nguyen, H.; Meeks, B.; Di Pasquale, G.; Lopez-Sendon, J.; Faxon, D.P.; et al. Complete Revascularization with Multivessel PCI for Myocardial Infarction. N. Engl. J. Med. 2019, 381, 1411–1421. [Google Scholar] [CrossRef]
- Brener, S.J.; Murphy, S.A.; Gibson, C.M.; DiBattiste, P.M.; Demopoulos, L.A.; Cannon, C.P.; TACTICS-TIMI 18 Investigators. Treat Angina with Aggrastat and Determine Cost of Therapy with an Invasive or Conservative Strat-egy-Thrombosis in Myocardial Infarction. Efficacy and safety of multivessel percutaneous revascularization and tirofiban therapy in patients with acute coronary syndromes. Am. J. Cardiol. 2002, 90, 631–633. [Google Scholar] [CrossRef]
- Wang, T.Y.; McCoy, L.A.; Bhatt, D.L.; Rao, S.V.; Roe, M.T.; Resnic, F.S.; Cavender, M.A.; Messenger, J.C.; Peterson, E.D. Multivessel vs culprit-only percutaneous coronary intervention among patients 65 years or older with acute myocardial infarction. Am. Heart J. 2015, 172, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Mariani, G.; De Servi, S.; Dellavalle, A.; Repetto, S.; Chierchia, S.; D’Urbano, M.; Repetto, A.; Klersy, C.; ROSAI Study Group. Complete or incomplete percutaneous coronary revascularization in patients with unstable angina in stent era: Are early and one-year results different? Catheter. Cardiovasc. Interv. 2001, 54, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Mariani, J.; Macchia, A.; De Abreu, M.; Gonzalez Villa Monte, G.; Tajer, C. Multivessel versus Single Vessel An-gioplasty in Non-ST Elevation Acute Coronary Syndromes: A Systematic Review and Metaanalysis. PLoS ONE 2016, 11, e0148756. [Google Scholar] [CrossRef] [PubMed]
- Hambraeus, K.; Jensevik, K.; Lagerqvist, B.; Lindahl, B.; Carlsson, R.; Farzaneh-Far, R.; Kellerth, T.; Omerovic, E.; Stone, G.; Varenhorst, C.; et al. Long-Term Outcome of Incomplete Revascularization After Percutaneous Coro-nary Intervention in SCAAR (Swedish Coronary Angiography and Angioplasty Registry). JACC Cardiovasc. Interv. 2016, 9, 207–215. [Google Scholar] [CrossRef]
- Rathod, K.S.; Koganti, S.; Jain, A.K.; Astroulakis, Z.; Lim, P.; Rakhit, R.; Kalra, S.S.; Dalby, M.C.; O’Mahony, C.; Malik, I.S.; et al. Complete Versus Culprit-Only Lesion Intervention in Patients with Acute Coronary Syndromes. J. Am. Coll. Cardiol. 2018, 72, 1989–1999. [Google Scholar] [CrossRef]
- Timmermans, M.J.C.; Houterman, S.; Daeter, E.D.; Danse, P.W.; Li, W.W.; Lipsic, E.; Roefs, M.M.; van Veghel, D.; PCI Registration Committee of The Netherlands Heart Registration and the Cardiothoracic Surgery Registration Committee of The Netherlands Heart Registration. Using real-world data to monitor and improve quality of care in coronary artery disease: Results from The Netherlands Heart Registration. Neth. Heart J. 2022. [Google Scholar] [CrossRef]
- Kim, M.C.; Jeong, M.H.; Ahn, Y.; Kim, J.H.; Chae, S.C.; Kim, Y.J.; Hur, S.H.; Seong, I.W.; Hong, T.J.; Choi, D.H.; et al. What is optimal revascularization strategy in patients with multivessel coronary artery disease in non-ST-elevation myocardial infarction? Multivessel or culprit-only revascularization. Int. J. Cardiol. 2010, 153, 148–153. [Google Scholar] [CrossRef]
- Shishehbor, M.H.; Lauer, M.S.; Singh, I.M.; Chew, D.P.; Karha, J.; Brener, S.J.; Moliterno, D.J.; Ellis, S.G.; Topol, E.J.; Bhatt, D.L. In unstable angina or non-ST-segment acute coronary syndrome, should patients with multivessel coro-nary artery disease undergo multivessel or culprit-only stenting? J. Am. Coll. Cardiol. 2007, 49, 849–854. [Google Scholar] [CrossRef]
- Zapata, G.O.; Lasave, L.I.; Kozak, F.; Damonte, A.; Meiriño, A.; Rossi, M.; Carbó, S.; Pollice, A.; Paolasso, E.; Picabea, E. Culprit-Only or Multivessel Percutaneous Coronary Stenting in Patients with Non-ST-Segment Elevation Acute Coronary Syndromes: One-Year Follow-Up. J. Interv. Cardiol. 2009, 22, 329–335. [Google Scholar] [CrossRef]
- Qiao, Y.; Salim, M.; Mohamed, S.; Nie, S.; Du, X.; Zhang, Y.; Jia, C.; Wang, X.; Liu, X.; Ma, C. A comparison of multivessel and culprit vessel percutaneous coronary intervention in non-ST-segment elevation acute coronary syndrome patients with multivessel disease: A meta-analysis. EuroIntervention 2015, 11, 525–532. [Google Scholar] [CrossRef]
- Jang, J.S.; Jin, H.Y.; Seo, J.S.; Yang, T.H.; Kim, D.K.; Kim, D.S.; Cho, K.I.; Kim, B.H.; Park, Y.H.; Je, H.G. Meta-analysis of mul-tivessel versus culprit-only percutaneous coronary intervention in patients with non-ST-segment elevation acute coronary syndrome and multivessel coronary disease. Am. J. Cardiol. 2015, 115, 1027–1032. [Google Scholar] [CrossRef] [PubMed]
- Onuma, Y.; Muramatsu, T.; Girasis, C.; Kukreja, N.; Garcia-Garcia, H.M.; Daemen, J.; Gonzalo, N.; Piazza, N.; Einthoven, J.; Van Domburg, R.; et al. Single-vessel or multivessel PCI in patients with multivessel disease presenting with non-ST-elevation acute coronary syndromes. EuroIntervention 2013, 9, 916–922. [Google Scholar] [CrossRef]
- Gershlick, A.H.; Khan, J.N.; Kelly, D.J.; Greenwood, J.P.; Sasikaran, T.; Curzen, N.; Blackman, D.J.; Dalby, M.; Fairbrother, K.L.; Banya, W.; et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing pri-mary percutaneous coronary intervention for STEMI and multivessel disease: The CvLPRIT trial. J. Am. Coll. Cardiol. 2015, 65, 963–972. [Google Scholar] [CrossRef] [PubMed]
- Cannon, C.P.; Weintraub, W.S.; Demopoulos, L.A.; Vicari, R.; Frey, M.J.; Lakkis, N.; Neumann, F.J.; Robertson, D.H.; DeLucca, P.T.; DiBattiste, P.M.; et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syn-dromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N. Engl. J. Med. 2001, 344, 1879–1887. [Google Scholar] [CrossRef]
- Poole-Wilson, P.A.; Pocock, S.J.; Fox, K.A.; Henderson, R.A.; Wheatley, D.J.; Chamberlain, D.A.; Shaw, T.R.; Clayton, T.C.; Randomised Intervention Trial of unstable Angina Investigators. Interventional versus conservative treatment in acute non-ST elevation coronary syndrome: Time course of patient management and disease events over one year in the RITA 3 trial. Heart 2006, 92, 1473–1479. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wallentin, L.; Lindhagen, L.; Ärnström, E.; Husted, S.; Janzon, M.; Johnsen, S.P.; Kontny, F.; Kempf, T.; Levin, L.Å.; Lindahl, B.; et al. Early invasive versus non-invasive treatment in patients with non-ST-elevation acute coronary syndrome (FRISC-II): 15 year follow-up of a prospective, randomised, multicentre study. Lancet 2016, 388, 1903–1911. [Google Scholar] [CrossRef]
- Goldstein, J.A.; Demetriou, D.; Grines, C.L.; Pica, M.; Shoukfeh, M.; O’Neill, W.W. Multiple complex coronary plaques in patients with acute myocardial infarction. N. Engl. J. Med. 2000, 343, 915–922. [Google Scholar] [CrossRef]
- Sardella, G.; Lucisano, L.; Garbo, R.; Pennacchi, M.; Cavallo, E.; Stio, R.E.; Calcagno, S.; Ugo, F.; Boccuzzi, G.; Fedele, F.; et al. Single-Staged Compared with Multi-Staged PCI in Multivessel NSTEMI Patients: The SMILE Trial. J. Am. Coll. Cardiol. 2016, 67, 264–272. [Google Scholar] [CrossRef]
- Pustjens, T.F.S.; Streukens, B.; Vainer, J.; Gho, B.; Ruiters, A.W.; Stein, M.; Ilhan, M.; Veenstra, L.; Theunissen, R.; Bekkers, S.C.A.M.; et al. Design and rationale of ischaemia-driven complete revascularisation versus usual care in patients with non-ST-elevation myocardial infarction and multivessel coronary disease: The South Limburg Myocardial Infarction (SLIM) trial. Neth. Heart J. 2020, 28, 75–80. [Google Scholar] [CrossRef]
- den Dekker, W.K.; Van Mieghem, N.M.; Bennett, J.; Sabate, M.; Esposito, G.; van Bommel, R.J.; Daemen, J.; Vrolix, M.; Cummins, P.A.; Lenzen, M.J.; et al. Percutaneous com-plete revascularization strategies using sirolimus-eluting biodegradable polymer-coated stents in patients pre-senting with acute coronary syndrome and multivessel disease: Rationale and design of the BIOVASC trial. Am. Heart J. 2020, 227, 111–117. [Google Scholar] [CrossRef]
- Biscaglia, S.; Guiducci, V.; Santarelli, A.; Amat Santos, I.; Fernandez-Aviles, F.; Lanzilotti, V.; Varbella, F.; Fileti, L.; Moreno, R.; Giannini, F.; et al. Physiology-guided revascularization versus optimal medical therapy of non-culprit lesions in elderly patients with myocardial infarction: Rationale and design of the FIRE trial. Am. Heart J. 2020, 229, 100–109. [Google Scholar] [CrossRef] [PubMed]
| Overall Cohort | Propensity Score Matched Cohort | |||||||
|---|---|---|---|---|---|---|---|---|
| MV-PCI n = 4235 | CO-PCI n = 6272 | OR (95%-CI) | p-Value | MV-PCI n = 3695 | CO-PCI n = 3695 | OR (95%-CI) | p-Value | |
| Age | 69.1 ± 11.6 | 68.4 ± 11.4 | NA | 0.004 | 68.6 ± 11.6 | 68.5 ± 11.6 | NA | 0.839 |
| Gender, female | 1286 (30.4) | 1824 (29.1) | 1.06 (0.98–1.16) | 0.157 | 1105 (29.9) | 1087 (29.4) | 1.02 (0.92–1.14) | 0.661 |
| eGFR < 60 mL/min/1.73 m2 | 1136 (28.3) | 1579 (26.0) | 0.89 (0.82–0.98) | 0.012 | 1007 (27.2) | 1010 (27.3) | 1.00 (0.90–1.13) | 0.940 |
| Diabetes mellitus | 1086 (25.9) | 1634 (26.3) | 0.98 (0.90–1.07) | 0.701 | 937 (25.4) | 963 (26.1) | 0.96 (0.85–1.09) | 0.545 |
| LVEF < 35% | 151 (7.6) | 198 (8.0) | 1.06 (0.85–1.33) | 0.588 | 129 (7.4) | 127 (8.5) | 1.16 (0.90–1.52) | 0.252 |
| Dialysis | 37 (1.0) | 51 (0.9) | 1.09 (0.71–1.67) | 0.683 | 29 (0.9) | 29 (0.9) | 0.94 (0.54–1.64) | 0.837 |
| Previous MI | 1008 (24.1) | 1702 (27.5) | 0.84 (0.77–0.92) | <0.001 | 882 (23.9) | 889 (24.1) | 0.99 (0.89–111) | 0.867 |
| Previous PCI | 1084 (25.8) | 2015 (32.7) | 0.72 (0.66–0.78) | <0.001 | 934 (25.3) | 919 (24.9) | 1.02 (0.92–1.14) | 0.687 |
| Radial approach | 3410 (85.5) | 5027 (86.6) | 0.91 (0.81–1.02) | 0.117 | 3140 (85.0) | 3060 (82.8) | 1.15 (0.75–1.77) | 0.456 |
| Left main PCI | 666 (15.7) | 252 (4.0) | 4.46 (3.83–5.18) | <0.001 | 252 (6.8) | 251 (6.8) | 1.01 (0.83–1.22) | 0.962 |
| Treated vessels | -* | -* | -* | -* | ||||
| LAD | 2537 (40.4) | 2282 (61.8) | ||||||
| LCX | 1562 (24.9) | 896 (24.2) | ||||||
| RCA | 1904 (30.4) | 265 (7.2) | ||||||
| LAD + LCX | 2081 (49.1) | 1693 (45.6) | ||||||
| LAD + RCA | 1106 (26.1) | 1074 (29.1) | ||||||
| LCX + RCA | 630 (14.9) | 607 (16.4) | ||||||
| LAD + LCX + RCA | 416 (9.8) | 319 (8.6) | ||||||
| Lesions treated | 2 (2–3) | 1 (1–1) | NA | <0.001 | 2 (2–3) | 1 (1–2) | NA | <0.001 |
| Stent treatment | 4.72 (3.74–5.95) | <0.001 | 1.06 (0.78–1.44) | 0.712 | ||||
| DES | 3501 (84.4) | 5083 (88.9) | 3037 (84.1) | 2978 (82.5) | ||||
| BMS | 6 (0.1) | 19 (0.3) | 4 (0.1) | 19 (0.5) | ||||
| BRS | 0 (-) | 6 (0.1) | 0 (-) | 0 (-) | ||||
| Unknown | 643 (15.5) | 611 (10.7) | 571 (15.8) | 611 (16.9) | ||||
| Balloon dilatation | 365 (8.6) | 525 (8.4) | 1.03 (0.90–1.19) | 0.654 | 230 (6.2) | 232 (6.3) | 0.90 (0.82–1.20) | 0.989 |
| Other treatment | 174 (4.1) | 203 (3.2) | 1.28 (1.04–1.58) | 0.019 | 80 (2.1) | 84 (2.3) | 0.94 (0.58–1.52) | 0.789 |
| Overall Cohort | Propensity Score–Matched Cohort | |||||||
|---|---|---|---|---|---|---|---|---|
| MV-PCI n = 4235 | CO-PCI n = 6272 | OR or HR (95%-CI) | p-Value | MV-PCI n = 3696 | CO-PCI n = 3696 | OR or HR (95%-CI) | p-Value | |
| Urgent CABG (<1 day) | 3 (0.1) | 26 (0.4) | 0.17 (0.052–0.56) | 0.004 | 3 (0.1) | 9 (0.2) | 0.33 (0.088–1.27) | 0.107 |
| MI ≤ 30 days | 24 (0.8) | 44 (0.9) | 0.85 (0.51–1.40) | 0.513 | 21 (0.8) | 28 (1.0) | 0.77 (0.43–1.39) | 0.388 |
| TVR at 1 year | 199 (5.2) | 404 (6.7) | 0.77 (0.65–0.92) | 0.003 | 151 (4.6) | 189 (5.4) | 0.86 (0.69–1.06) | 0.156 |
| Mortality at 1 year | 253 (6.0) | 351 (5.6) | 1.08 (0.92–1.27) | 0.351 | 197 (5.4) | 216 (5.9) | 0.92 (0.76–1.13) | 0.439 |
| Mortality at long-term follow-up | 451 (10.7) | 635 (10.2) | 1.09 (0.96–1.23) | 0.173 | 358 (9.7) | 404 (11.0) | 0.92 (0.80–1.07) | 0.289 |
| Reinterventions at long-term follow-up | 470 (11.1) | 1254 (20.0) | 0.53 (0.47–0.59) | <0.001 | 389 (10.5) | 668 (18.1) | 0.57 (0.50–0.64) | <0.001 |
| PCI | 409 (87.0) | 1035 (82.5) | 340 (87.4) | 585 (87.6) | ||||
| CABG | 61 (13.0) | 219 (17.5) | 49 (12.6) | 83 (12.4) | ||||
| Univariable | Multivariable * | |
|---|---|---|
| Age | 1.07 (1.06–1.07) | 1.05 (1.04–1.06) |
| Gender, female | 1.21 (1.07–1.37) | 0.85 (0.74–0.98) |
| eGFR < 60 mL/min/1.73 m2 | 3.55 (3.15–4.00) | 2.00 (1.72–2.31) |
| Diabetes mellitus | 2.08 (1.84–2.34) | 1.73 (1.51–1.97) |
| LVEF | 3.13 (2.53–3.87) | NA |
| Dialysis | 7.29 (5.45–9.75) | 3.18 (2.33–4.33) |
| Previous MI | 1.57 (1.39–1.76) | 1.37 (1.17–1.60) |
| Previous PCI | 1.21 (1.06–1.37) | 0.90 (0.77–1.05) |
| Radial approach | 0.62 (0.39–0.76) | 0.67 (0.57–0.78) |
| Left main PCI | 2.48 (2.12–2.90) | 1.54 (1.28–1.84) |
| Vessel treatment | ||
| Stent treatment | 0.81 (0.65–1.01) | NA |
| Balloon dilatation | 1.30 (1.07–1.57) | NA |
| Other treatment | 1.61 (1.24–2.10) | 1.47 (1.10–1.95) |
| Multivessel PCI | 1.09 (0.96–1.23) | 0.91 (0.80–1.05) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pustjens, T.F.S.; Timmermans, M.J.C.; Rasoul, S.; van ‘t Hof, A.W.J.; on behalf of the PCI Registration Committee; the Cardiothoracic Surgery Registration Committee of The Netherlands Heart Registration. Multivessel versus Culprit-Only Percutaneous Coronary Intervention in Patients with Non-ST-Elevation Acute Coronary Syndrome. J. Clin. Med. 2022, 11, 6144. https://doi.org/10.3390/jcm11206144
Pustjens TFS, Timmermans MJC, Rasoul S, van ‘t Hof AWJ, on behalf of the PCI Registration Committee, the Cardiothoracic Surgery Registration Committee of The Netherlands Heart Registration. Multivessel versus Culprit-Only Percutaneous Coronary Intervention in Patients with Non-ST-Elevation Acute Coronary Syndrome. Journal of Clinical Medicine. 2022; 11(20):6144. https://doi.org/10.3390/jcm11206144
Chicago/Turabian StylePustjens, Tobias F. S., Marijke J. C. Timmermans, Saman Rasoul, Arnoud W. J. van ‘t Hof, on behalf of the PCI Registration Committee, and the Cardiothoracic Surgery Registration Committee of The Netherlands Heart Registration. 2022. "Multivessel versus Culprit-Only Percutaneous Coronary Intervention in Patients with Non-ST-Elevation Acute Coronary Syndrome" Journal of Clinical Medicine 11, no. 20: 6144. https://doi.org/10.3390/jcm11206144
APA StylePustjens, T. F. S., Timmermans, M. J. C., Rasoul, S., van ‘t Hof, A. W. J., on behalf of the PCI Registration Committee, & the Cardiothoracic Surgery Registration Committee of The Netherlands Heart Registration. (2022). Multivessel versus Culprit-Only Percutaneous Coronary Intervention in Patients with Non-ST-Elevation Acute Coronary Syndrome. Journal of Clinical Medicine, 11(20), 6144. https://doi.org/10.3390/jcm11206144






