Orthorexia Nervosa, Eating Disorders, and Obsessive-Compulsive Disorder: A Selective Review of the Last Seven Years
Abstract
1. Introduction
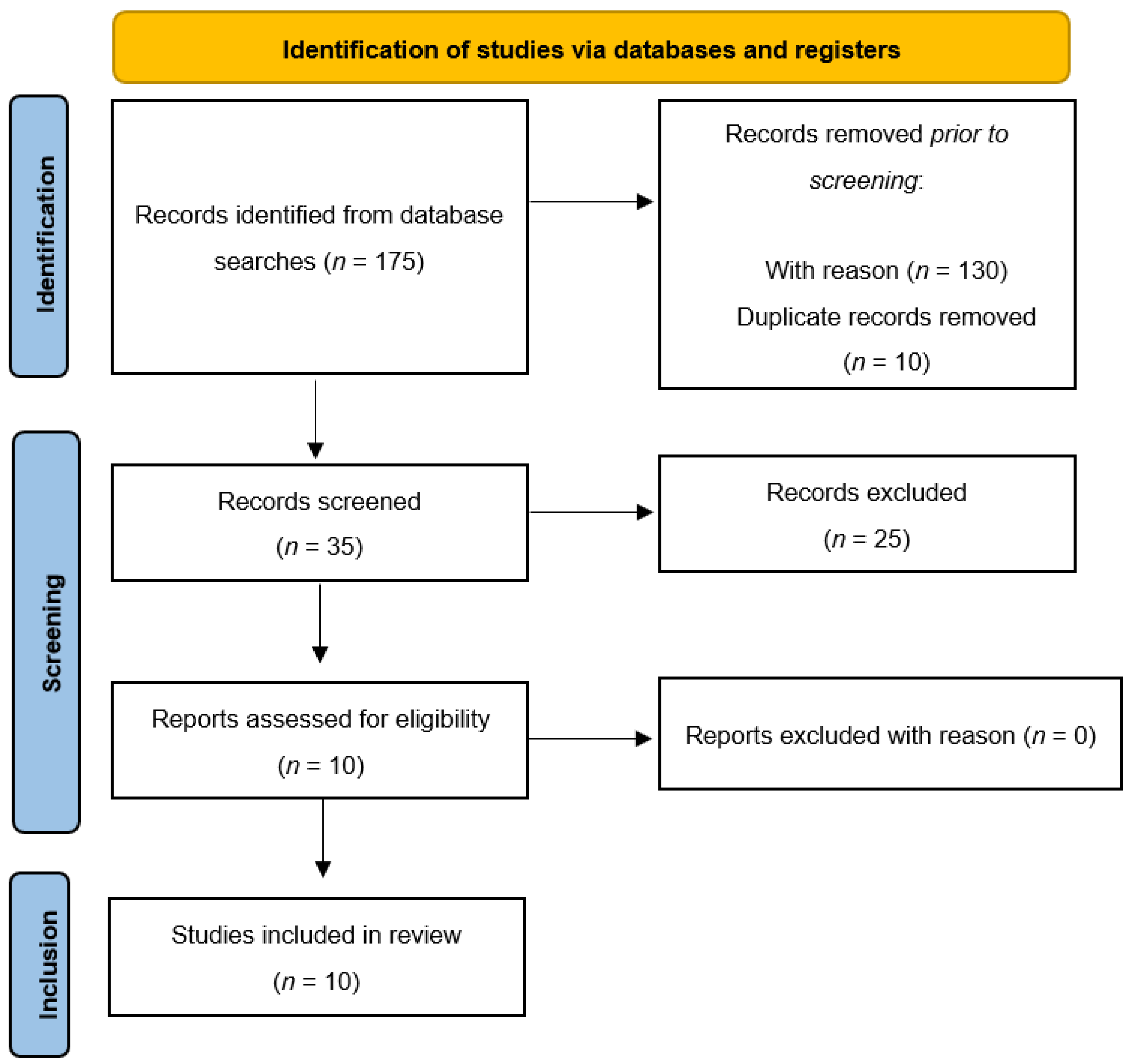
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Selection Procedure, Data Extraction, and Data Management
3. Results
3.1. Clinical significance of Orthorexia Nervosa
3.2. Orthorexia Nervosa and DSM-5 Eating Disorders
3.3. Orthorexia Nervosa and Obsessive-Compulsive Disorder
| Study | Sample | Method(s) | Measures | Results |
|---|---|---|---|---|
| Barnes and Catalbiano [50] | Sample: 220 adults (180 university psychology students, 40 recruited from Facebook; 46 male, 154 female; age range: 17–62 years [M = 23.81, SD = 8.40]) | Experimental study | ORTO-15; MPS; MBSRQ-AS; RSQ; RSES | History of an ED was the strongest predictor of ON; ORTO-15 scores were significantly correlated with perfectionism and fearful and dismissing attachment styles, but not with self-esteem |
| Novara et al. [51] | Sample: 302 university students in northern Italy. Total sample divided into two groups: “High EHQ” (n = 43; 22 male, 21 female, age range: 18–31 years [M = 20.60, SD = 2.44]) and “Low EHQ” (n = 259; 41.5% male, 58.5% female; age range: 18–49 years [M = 20.83, SD = 3.33]) | Experimental study | EHQ-21; EDI-3; OCI-R; WDQ; PSWQ; MPS; BAI; BDI-II | Association between ON and perfectionism, anxious and depressive symptoms, and ED symptoms |
| Brytek-Matera et al. [49] | Sample: 52 women diagnosed with an ED (Mage = 22.81, SD = 3.80) | Experimental study | ORTO-15; MBSRQ; EAT-26 | Lower level of eating pathology associated with more frequent orthorexic behaviors; higher level of eating pathology associated with less frequent orthorexic behaviors; ON negatively predicted by eating pathology, weight concern, health orientation, and appearance orientation |
| Barthels et al. [48] | Sample: 42 female anorexic patients with orthorexic eating behaviors (Mage = 21.17, SD = 6.88; MBMI = 15.97, SD = 1.52 kg/m2) Control group: 30 females (Mage = 22.10, SD = 7.43 years; MBMI = 21.83, SD = 2.75 kg/m2) | Experimental study | DOS; EDI-2; DKB-35; BPNS-E; MIHT | Orthorexic eating behaviors might represent coping mechanisms for patients with anorexic eating behaviors, and healthier ways of controlling food intake than focusing on low-calorie foods |
| Rania et al. [54] | Sample: 4 women with a prior psychiatric disorder (Mage = 35) | Case report | ORTO-15; SCID-5-CV | Some psychiatric conditions, across a diagnostic continuum, may lead to ON |
| Łucka et al. [47] | Sample: 864 adolescents and young adults from the general population (265 male, 599 female; age range: 13–30 years) | Experimental study | ORTO-15; EAT-26; MOCI | Significant association between EDs (EAT-26) and ON (ORTO-15); no significant relationship between the severity of obsessive-compulsive symptoms (MOCI) and orthorexia (ORTO-15) |
| Vaccari et al. [52] | OCD group: 50 patients Control group 1: 42 patients with a diagnosed anxiety or depressive disorder Control group 2:236 subjects from the general population | Multi-center, observational, controlled study | ORTO-15; ORTO-R; OCI-R | More ON symptoms among widowers relative to subjects with a partner and separated/divorced subjects; ON symptoms more prevalent in less educated subjects and those engaging in high-frequency physical activity; ORTO-R variation associated with a positive OCI-R score |
| Yilmaz et al. [53] | Sample: 189 individuals (79 outpatients with OCD, 68 healthy controls who regularly engaged in exercise, 69 healthy controls who did not regularly engage in exercise; age range: 18–65 years) | Experimental study | SCID-5/CV Y-BOCS; EAT-40; ORTO-11; HAS | Orthorexic symptoms increased in the E + HC group as eating attitude deteriorated; orthorexic tendencies were higher in subjects with order-symmetry obsessions than in those with no such obsessions |
| Bartel et al. [12] | Sample: 512 individuals recruited through social media, an undergraduate psychology pool, and the general student body of a university in Western Canada (89 male, 423 female; Mage = 24.5 years) | Experimental study | EDE-Q; rBOT; ORTO-15; OCI-R; FMPS; FCQ | Strong correlation between ON and EDE-Q (r = 0.63); correlation between ON and OCI-R total scales (r = 0.27); controlling for EDE-Q scores, only a small or no association between ON and OC symptoms (r = 0.08) |
| Strahler et al. [46] | Sample: 713 subjects recruited through public advertisements in local shops and mailing lists from universities in the broader Giessen/Marburg area (20.2% male, 79.8% female; age range: 18–75 years [M = 25]) | Cross-sectional study | DOS; WHO-5; PSS-10; RS-13; WREQ; EDE-Q8; PHQ-9; HADS; AUDIT; Y-BOCS; GPPAQ | Strong correlation between ON and other mental disorders; ON no more prevalent than other forms of restrictive dieting and not associated with physical activity levels within a healthy lifestyle |
4. Discussion
4.1. Clinical Significance of Orthorexia Nervosa
4.2. Orthorexia Nervosa and DSM-5 Eating Disorders
4.3. Orthorexia Nervosa and Obsessive-Compulsive Disorder
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oberle, C.D.; Samaghabadi, R.O.; Hughes, E.M. Orthorexia nervosa: Assessment and correlates with gender, BMI, and personality. Appetite 2017, 108, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Fidan, T.; Ertekin, V.; Isikay, S.; Kirpinar, I. Prevalence of orthorexia among medical students in Erzurum, Turkey. Compr. Psychiatry 2010, 51, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, A.; Cooper, M.; McAdams, C.; Peebles, R.; Timko, C.A. Cultural shifts in the symptoms of anorexia nervosa: The case of orthorexia nervosa. Appetite 2022, 170, 105869. [Google Scholar] [CrossRef] [PubMed]
- Varga, M.; Dukay-Szabó, S.; Túry, F.; Van Furth, E.F.; Van Furth, E.F. Evidence and gaps in the literature on orthorexia nervosa. Eat. Weight Disord. 2013, 18, 103–111. [Google Scholar] [CrossRef]
- Bratman, S.; Knight, D. Health food junkies. In Orthorexia Nervosa: Overcoming the Obsession with Healthful Eating, 1st ed.; Brodways Books: New York, NY, USA, 2000; p. 256. [Google Scholar]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Cannella, C. Orthorexia nervosa: A preliminary study with a proposal for diagnosis and an attempt to measure the dimension of the phenomenon. Eat. Weight Disord. 2004, 9, 151–157. [Google Scholar] [CrossRef]
- Koven, N.S.; Abry, A.W. The clinical basis of orthorexia nervosa: Emerging perspectives. Neuropsychiatr. Dis. Treat. 2015, 11, 385–394. [Google Scholar] [CrossRef]
- Grammatikopoulou, M.G.; Gkiouras, K.; Polychronidou, G.; Kaparounaki, C.; Gkouskou, K.K.; Magkos, F.; Donini, L.M.; Eliopoulos, A.G.; Goulis, D.G. Obsessed with Healthy Eating: A Systematic Review of Observational Studies Assessing Orthorexia Nervosa in Patients with Diabetes Mellitus. Nutrients 2021, 13, 3823. [Google Scholar] [CrossRef]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Cannella, C. Orthorexia nervosa: Validation of a diagnosis questionnaire. Eat. Weight Disord. 2005, 10, e28–e32. [Google Scholar] [CrossRef]
- Barthels, F.; Meyer, F.; Pietrowsky, R. Orthorexic eating behavior: A new type of disordered eating. Ernahr. Umsch. 2015, 62, 156–161. [Google Scholar] [CrossRef]
- Haeberle-Savard, A.C. Motivation and the Relationship between Orthorexia Nervosa and Depressive Symptoms. Ph.D. Thesis, Concordia University, Montreal, QC, Canada, 2015. [Google Scholar]
- Bartel, S.J.; Sherry, S.B.; Farthing, G.R.; Stewart, S.H. Classification of orthorexia nervosa: Further evidence for placement within the eating disorders spectrum. Eat. Behav. 2020, 38, 101406. [Google Scholar] [CrossRef]
- Biswajit, C.; Sangita, P.; Bandyopadhyay, A. Exploring scientific legitimacy of orthorexia nervosa: A newly emerging eating disorder. J. Hum. Sport Exerc. 2013, 8, 1045–1053. [Google Scholar]
- Mathieu, J. What is orthorexia? J. Am. Diet. Assoc. 2005, 105, 1510–1512. [Google Scholar] [CrossRef]
- Scarff, J.R. Orthorexia Nervosa: An Obsession with Healthy Eating. Fed. Pract. 2017, 34, 36–39. [Google Scholar]
- Dell’Osso, L.; Carpita, B.; Muti, D.; Cremone, I.M.; Massimetti, G.; Diadema, E.; Gesi, C.; Carmassi, C. Prevalence and characteristics of orthorexia nervosa in a sample of university students in Italy. Eat. Weight Disord. 2018, 23, 55–65. [Google Scholar] [CrossRef]
- Stice, E.; Gau, J.M.; Rohde, P.; Shaw, H. Risk factors that predict future onset of each DSM-5 eating disorder: Predictive specificity in high-risk adolescent females. J. Abnorm. Psychol. 2017, 126, 38–51. [Google Scholar] [CrossRef]
- Oberle, C.D.; Klare, D.L.; Patyk, K.C. Health beliefs, behaviors, and symptoms associated with orthorexia nervosa. Eat. Weight Disord. 2019, 24, 495–506. [Google Scholar] [CrossRef]
- Segura-Garcia, C.; Ramacciotti, C.; Rania, M.; Aloi, M.; Caroleo, M.; Bruni, A.; Gazzarrini, D.; Sinopoli, F.; De Fazio, P. The prevalence of orthorexia nervosa among eating disorder patients after treatment. Eat. Weight Disord. 2015, 20, 161–166. [Google Scholar] [CrossRef]
- Brytek-Matera, A. Orthorexia nervosa—An eating disorder, obsessive-compulsive disorder or disturbed eating habit? Arch. Psychiatry Psychother. 2012, 1, 55–60. [Google Scholar]
- Atchison, A.E.; Zickgraf, H.F. Orthorexia nervosa and eating disorder behaviors: A systematic review of the literature. Appetite 2022, 177, 106134. [Google Scholar] [CrossRef]
- Brytek-Matera, A. Vegetarian diet and orthorexia nervosa: A review of the literature. Eat. Weight Disord. 2021, 26, 1–11. [Google Scholar] [CrossRef]
- Costa, C.B.; Hardan-Khalil, K.; Gibbs, K. Orthorexia nervosa: A review of the literature. Issues Ment. Health Nurs. 2017, 38, 980–988. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Abelli, M.; Carpita, B.; Pini, S.; Castellini, G.; Carmassi, C.; Ricca, V. Historical evolution of the concept of anorexia nervosa and relationships with orthorexia nervosa, autism, and obsessive-compulsive spectrum. Neuropsychiatr. Dis. Treat. 2016, 12, 1651–1660. [Google Scholar] [CrossRef]
- Dukay-Szabó, S.; Varga, M.; Túry, F. Az evészavarok és a terhesség összefüggései—Irodalmi áttekintés [Eating disorders and pregnancy—A review of literature]. Szle. Ideggyógyászati 2016, 69, 299–305. [Google Scholar] [CrossRef]
- Dunn, T.M.; Bratman, S. On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eat Behav. 2016, 21, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Gortat, M.; Samardakiewicz, M.; Perzyński, A. Orthorexia nervosa—A distorted approach to healthy eating. Psychiatr. Pol. 2021, 55, 421–433, (In English, Polish). [Google Scholar] [CrossRef]
- Goutaudier, N.; Rousseau, A. L’orthorexie: Une nouvelle forme de trouble des conduites alimentaires? [Othorexia: A new type of eating disorder?]. Presse Médicale 2019, 48, 1065–1071. [Google Scholar] [CrossRef]
- Håman, L.; Barker-Ruchti, N.; Patriksson, G.; Lindgren, E.C. Orthorexia nervosa: An integrative literature review of a lifestyle syndrome. Int. J. Qual. Stud. Health Well-Being 2015, 10, 26799. [Google Scholar] [CrossRef]
- Hyrnik, J.; Zasada, I.; Wilczyński, K.M.; Jelonek, I.; Janas-Kozik, M. Orthorexia—Current approach. A review. Psychiatr. Pol. 2021, 55, 405–420. [Google Scholar] [CrossRef] [PubMed]
- Kalra, S.; Kapoor, N.; Jacob, J. Orthorexia nervosa. J. Pak. Med. Assoc. 2020, 70, 1282–1284. [Google Scholar] [PubMed]
- McComb, S.E.; Mills, J.S. Orthorexia nervosa: A review of psychosocial risk factors. Appetite 2019, 140, 50–75. [Google Scholar] [CrossRef] [PubMed]
- Michalska, A.; Szejko, N.; Jakubczyk, A.; Wojnar, M. Nonspecific eating disorders—A subjective review. Psychiatr. Pol. 2016, 50, 497–507. [Google Scholar] [CrossRef]
- Niedzielski, A.; Kaźmierczak-Wojtaś, N. Prevalence of orthorexia nervosa and its diagnostic tools—A literature review. Int. J. Environ. Res. Public Health 2021, 18, 5488. [Google Scholar] [CrossRef]
- Opitz, M.C.; Newman, E.; Mellado, A.S.A.V.; Robertson, M.D.A.; Sharpe, H. The psychometric properties of orthorexia nervosa assessment scales: A systematic review and reliability generalization. Appetite 2020, 155, 104797. [Google Scholar] [CrossRef]
- Strahler, J. Sex differences in orthorexic eating behaviors: A systematic review and meta-analytical integration. Nutrition 2019, 67–68, 10534. [Google Scholar] [CrossRef]
- Strahler, J.; Wachten, H.; Mueller-Alcazar, A. Obsessive healthy eating and orthorexic eating tendencies in sport and exercise contexts: A systematic review and meta-analysis. J. Behav. Addict. 2021, 10, 456–470. [Google Scholar] [CrossRef]
- Valente, M.; Syurina, E.V.; Donini, L.M. Shedding light upon various tools to assess orthorexia nervosa: A critical literature review with a systematic search. Eat. Weight Disord. 2019, 24, 671–682. [Google Scholar] [CrossRef]
- Zagaria, A.; Vacca, M.; Cerolini, S.; Ballesio, A.; Lombardo, C. Associations between orthorexia, disordered eating, and obsessive-compulsive symptoms: A systematic review and meta-analysis. Int. J. Eat Disord. 2022, 55, 295–312. [Google Scholar] [CrossRef]
- Babilonia, M.B.; Donovan, K.A.; di Ciccone, B.B.L.; Rajasekhara, S. When orthorexia nervosa meets cancer—A case review. Psychooncology 2020, 29, 1507–1509. [Google Scholar] [CrossRef]
- Bóna, E.; Szél, Z.; Kiss, D.; Gyarmathy, V.A. An unhealthy health behavior: Analysis of orthorexic tendencies among Hungarian gym attendees. Eat. Weight Disord. 2019, 24, 13–20. [Google Scholar] [CrossRef]
- Domingues, R.B.; Carmo, C. Orthorexia nervosa in yoga practitioners: Relationship with personality, attitudes about appearance, and yoga engagement. Eat. Weight Disord. 2021, 26, 789–795. [Google Scholar] [CrossRef]
- Kinzl, J.F.; Hauer, K.; Traweger, C.; Kiefer, I. Orthorexia nervosa in dieticians. Psychother. Psychosom. 2006, 75, 395–396. [Google Scholar] [CrossRef]
- Ouyaba, A.T.; Öztürk, P.Ç. The effect of the information-motivation-behavioral skills (IMB) model variables on orthorexia nervosa behaviors of pregnant women. Eat. Weight Disord. 2022, 27, 361–372. [Google Scholar] [CrossRef]
- Tremelling, K.; Sandon, L.; Vega, G.L.; McAdams, C.J. Orthorexia nervosa and eating disorder symptoms in registered dietitian nutritionists in the United States. J. Acad. Nutr. Diet. 2017, 117, 1612–1617. [Google Scholar] [CrossRef]
- Strahler, J.; Hermann, A.; Walter, B.; Stark, R. Orthorexia nervosa: A behavioral complex or a psychological condition? J. Behav. Addict. 2018, 4, 1143–1156. [Google Scholar] [CrossRef]
- Łucka, I.; Janikowska-Hołoweńko, D.; Domarecki, P.; Plenikowska-Ślusarz, T.; Domarecka, M. Orthorexia nervosa—A separate clinical entity, a part of eating disorder spectrum or another manifestation of obsessive-compulsive disorder? Psychiatr. Pol. 2019, 53, 371–382. [Google Scholar] [CrossRef]
- Barthels, F.; Meyer, F.; Huber, T.; Pietrowsky, R. Orthorexic eating behaviour as a coping strategy in patients with anorexia nervosa. Eat. Weight Disord. 2017, 22, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Brytek-Matera, A.; Rogoza, R.; Gramaglia, C.; Zeppegno, P. Predictors of orthorexic behaviours in patients with eating disorders: A preliminary study. BMC Psychiatry 2015, 15, 252. [Google Scholar] [CrossRef] [PubMed]
- Barnes, M.A.; Caltabiano, M.L. The interrelationship between orthorexia nervosa, perfectionism, body image and attachment style. Eat. Weight Disord. 2016, 22, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Novara, C.; Pardini, S.; Maggio, E.; Mattioli, S.; Piasentin, S. Orthorexia nervosa: Over concern or obsession about healthy food? Eat. Weight Disord. 2021, 26, 2577–2588. [Google Scholar] [CrossRef] [PubMed]
- Vaccari, G.; Cutino, A.; Luisi, F.; Giambalvo, N.; Daneshmand, S.N.; Pinelli, M.; Maina, G.; Galeazzi, G.M.; Kaleci, S.; Albert, U.; et al. Is orthorexia nervosa a feature of obsessive-compulsive disorder? A multicentric, controlled study. Eat. Weight Disord. 2021, 26, 2531–2544. [Google Scholar] [CrossRef]
- Yılmaz, H.; Karakuş, G.; Tamam, L.; Demirkol, M.E.; Namlı, Z.; Yeşiloğlu, C. Association of orthorexic tendencies with obsessive-compulsive symptoms, eating attitudes and exercise. Neuropsychiatr. Dis. Treat. 2020, 16, 3035–3044. [Google Scholar] [CrossRef]
- Rania, M.; De Filippis, R.; Caroleo, M.; Carbone, E.; Aloi, M.; Bratman, S.; Segura-Garcia, C. Pathways to orthorexia nervosa: A case series discussion. Eat. Weight Disord. 2020, 26, 1675–1683. [Google Scholar] [CrossRef] [PubMed]
- Dunn, T.M.; Gibbs, J.; Whitney, N.; Starosta, A. Prevalence of orthorexia nervosa is less than 1%: Data from a US sample. Eat. Weight 2017, 22, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.J.; Parman, K.M.; Rudat, D.A.; Craighead, L.W. Disordered eating, perfectionism, and food rules. Eat. Behav. 2012, 13, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Bardone-Cone, A.M.; Wonderlich, S.A.; Frost, R.O.; Bulik, C.M.; Mitchell, J.E.; Uppala, S.; Simonich, H. Perfectionism and eating disorders: Current status and future directions. Clin. Psychol. Rev. 2007, 27, 384–405. [Google Scholar] [CrossRef]
- Hrabosky, J.I.; Cash, T.F.; Veale, D.; Neziroglu, F.; Soll, E.A.; Garner, D.M.; Strachan-Kinser, M.; Bakke, B.; Clauss, L.J.; Phillips, K.A. Multidimensional body image comparisons among patients with eating disorders, body dysmorphic disorder, and clinical controls: A multisite study. Body Image 2009, 6, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Shafran, R.; Cooper, Z. A cognitive behavioural theory of anorexia nervosa. A Behav. Res. 1999, 37, 1–13. [Google Scholar] [CrossRef]
- Cena, H.; Barthels, F.; Cuzzolaro, M.; Bratman, S.; Brytek-Matera, A.; Dunn, T.; Varga, M.; Missbach, B.; Donini, L.M. Definition and diagnostic criteria for orthorexia nervosa: A narrative review of the literature. Eat. Weight Disord. 2019, 24, 209–246. [Google Scholar] [CrossRef]
- Bratman, S.; Knight, D. Health food junkie. Yoga J. 1997, 136, 42–50. [Google Scholar]
- Koven, N.S.; Senbonmatsu, R. A neuropsychological evaluation of orthorexia nervosa. Open J. Psychiatry 2013, 3, 214–222. [Google Scholar] [CrossRef]
| Reason for Exclusion | Study Name |
|---|---|
| Article format (e.g., review) | Bhattacharya, A. et al. [3]; |
| Brytek-Matera, A. [22]; | |
| Costa, C.B. et al. [23]; | |
| Dell’Osso et al. [24]; | |
| Dukay-Szabó, S. et al. [25]; | |
| Dunn, T.M. et al. [26]; | |
| Gortat, M. et al. [27]; | |
| Goutaudier, N. et al. [28]; | |
| Håman, L. et al. [29]; | |
| Hyrnik, J. et al. [30]; | |
| Kalra, S. et al. [31]; | |
| McComb, S.E. et al. [32]; | |
| Michalska, A. et al. [33]; | |
| Niedzielski, A. et al. [34]; | |
| Opitz, M.C. et al. [35]; | |
| Strahler, J. [36]; | |
| Strahler, J. et al. [37]; | |
| Valente, M. et al. [38]; | |
| Zagaria, A. et al. [39] | |
| Sample characteristics: only specific population included | Bobonis Babilonia, M. et al. [40]; |
| Bóna, E. et al. [41]; | |
| Domingues, R.B. et al. [42]; | |
| Kinzl, J.F. et al. [43]; | |
| Taştekin Ouyaba, A. et al. [44]; | |
| Tremeling et al. [45] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pontillo, M.; Zanna, V.; Demaria, F.; Averna, R.; Di Vincenzo, C.; De Biase, M.; Di Luzio, M.; Foti, B.; Tata, M.C.; Vicari, S. Orthorexia Nervosa, Eating Disorders, and Obsessive-Compulsive Disorder: A Selective Review of the Last Seven Years. J. Clin. Med. 2022, 11, 6134. https://doi.org/10.3390/jcm11206134
Pontillo M, Zanna V, Demaria F, Averna R, Di Vincenzo C, De Biase M, Di Luzio M, Foti B, Tata MC, Vicari S. Orthorexia Nervosa, Eating Disorders, and Obsessive-Compulsive Disorder: A Selective Review of the Last Seven Years. Journal of Clinical Medicine. 2022; 11(20):6134. https://doi.org/10.3390/jcm11206134
Chicago/Turabian StylePontillo, Maria, Valeria Zanna, Francesco Demaria, Roberto Averna, Cristina Di Vincenzo, Margherita De Biase, Michelangelo Di Luzio, Benedetta Foti, Maria Cristina Tata, and Stefano Vicari. 2022. "Orthorexia Nervosa, Eating Disorders, and Obsessive-Compulsive Disorder: A Selective Review of the Last Seven Years" Journal of Clinical Medicine 11, no. 20: 6134. https://doi.org/10.3390/jcm11206134
APA StylePontillo, M., Zanna, V., Demaria, F., Averna, R., Di Vincenzo, C., De Biase, M., Di Luzio, M., Foti, B., Tata, M. C., & Vicari, S. (2022). Orthorexia Nervosa, Eating Disorders, and Obsessive-Compulsive Disorder: A Selective Review of the Last Seven Years. Journal of Clinical Medicine, 11(20), 6134. https://doi.org/10.3390/jcm11206134








