The Scientific Evolution of Periacetabular Osteotomy: A Global Review
Abstract
1. Introduction
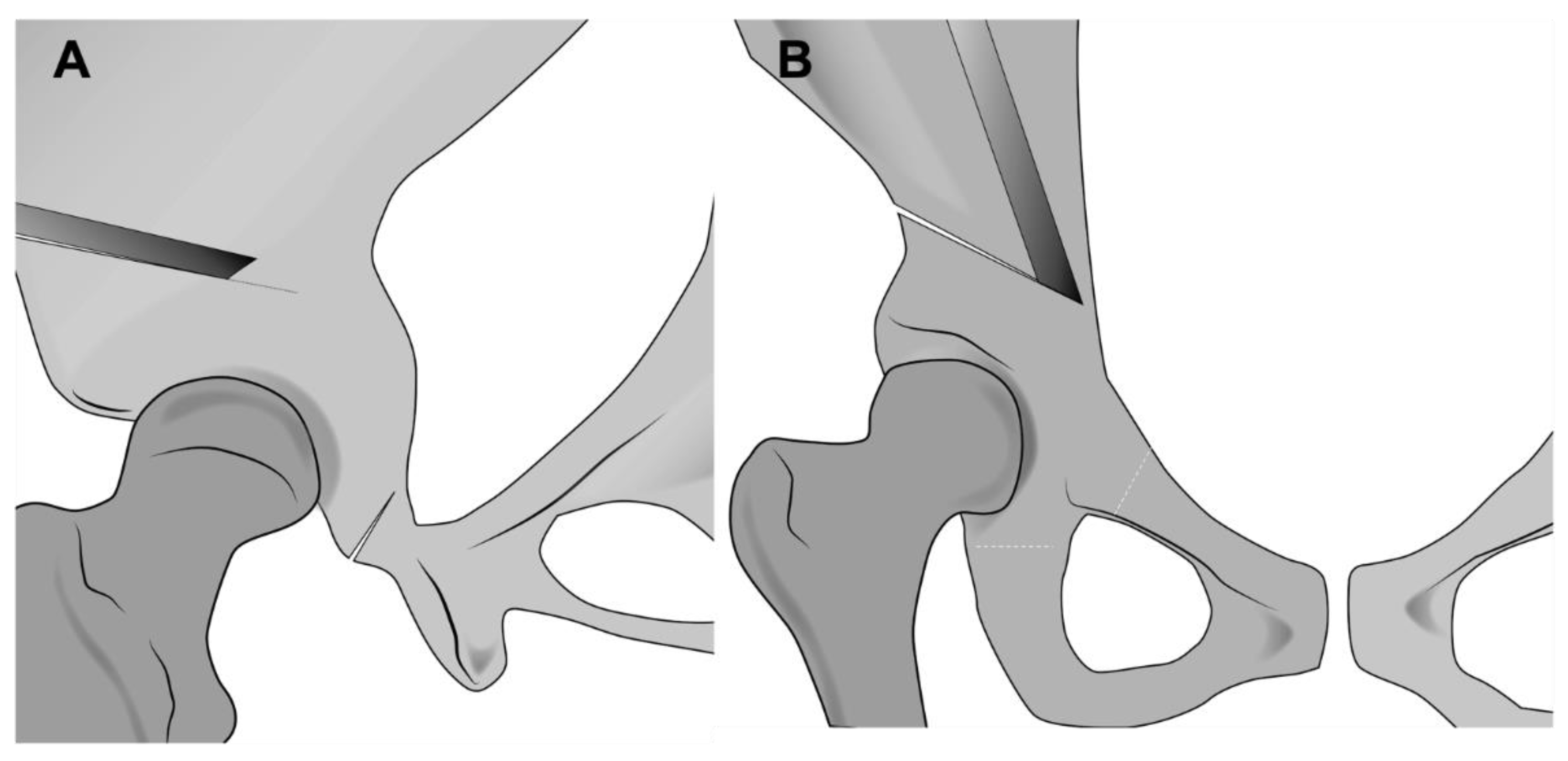
Early Description of Periacetabular Osteotomy
2. Indications for Periacetabular Osteotomy
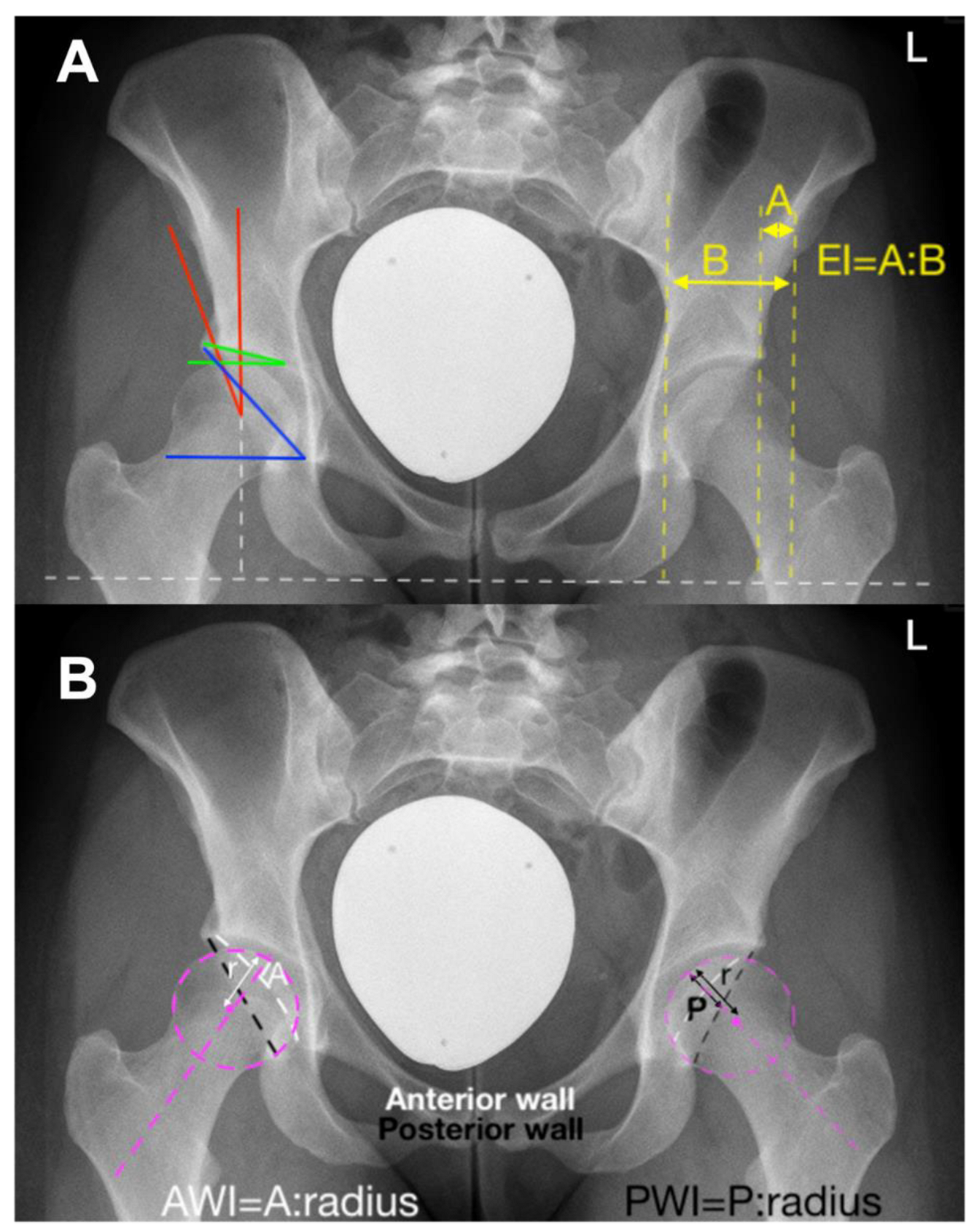
2.1. Classical Indications
- − Lateral center edge angle (LCEA): 22°
- − Acetabular index: >14°
- − Extrusion index: >27%
- − Anterior wall coverage: <14%
- − Posterior wall coverage: <35%
- − Sharp angle: >43°
2.2. Extended Indications
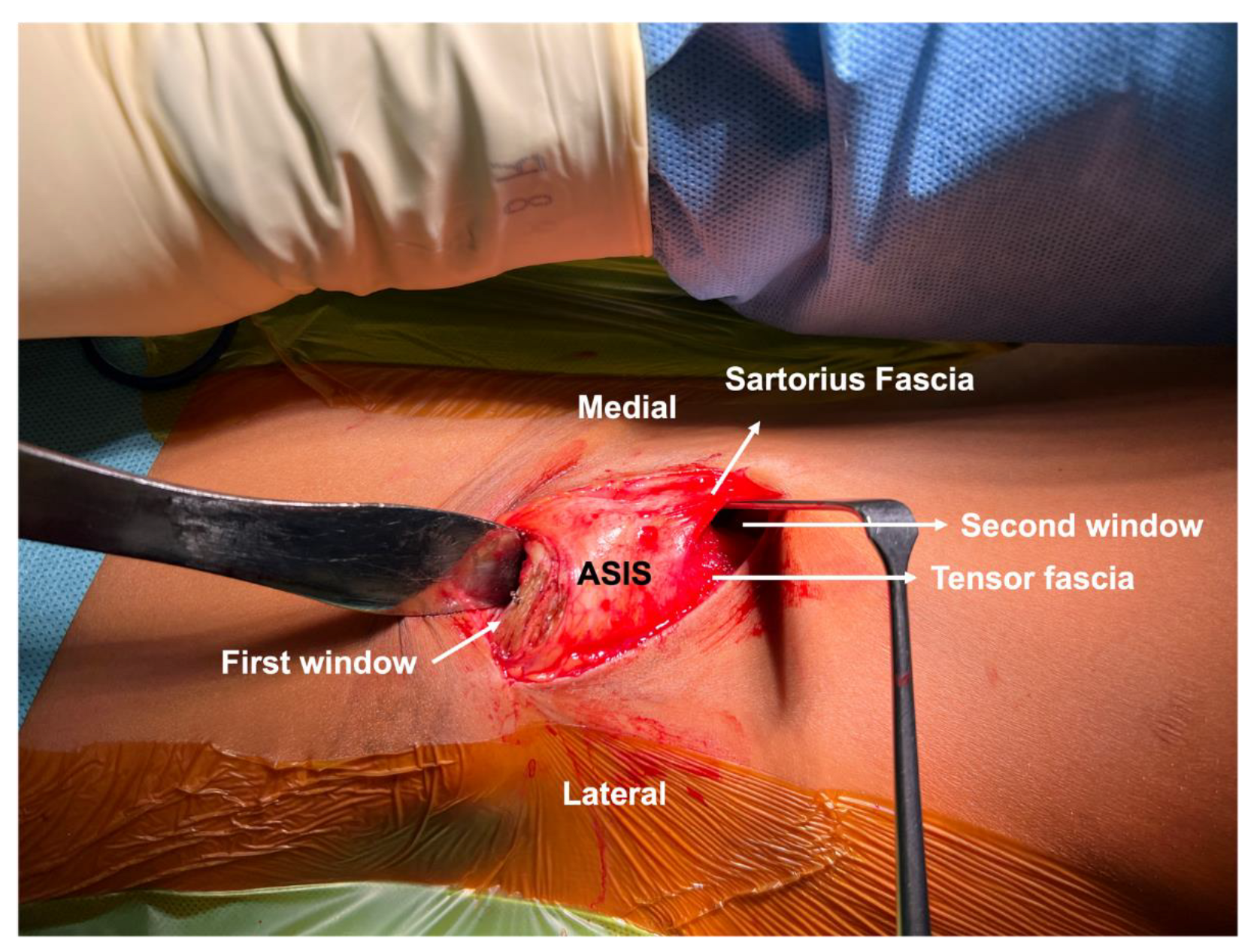
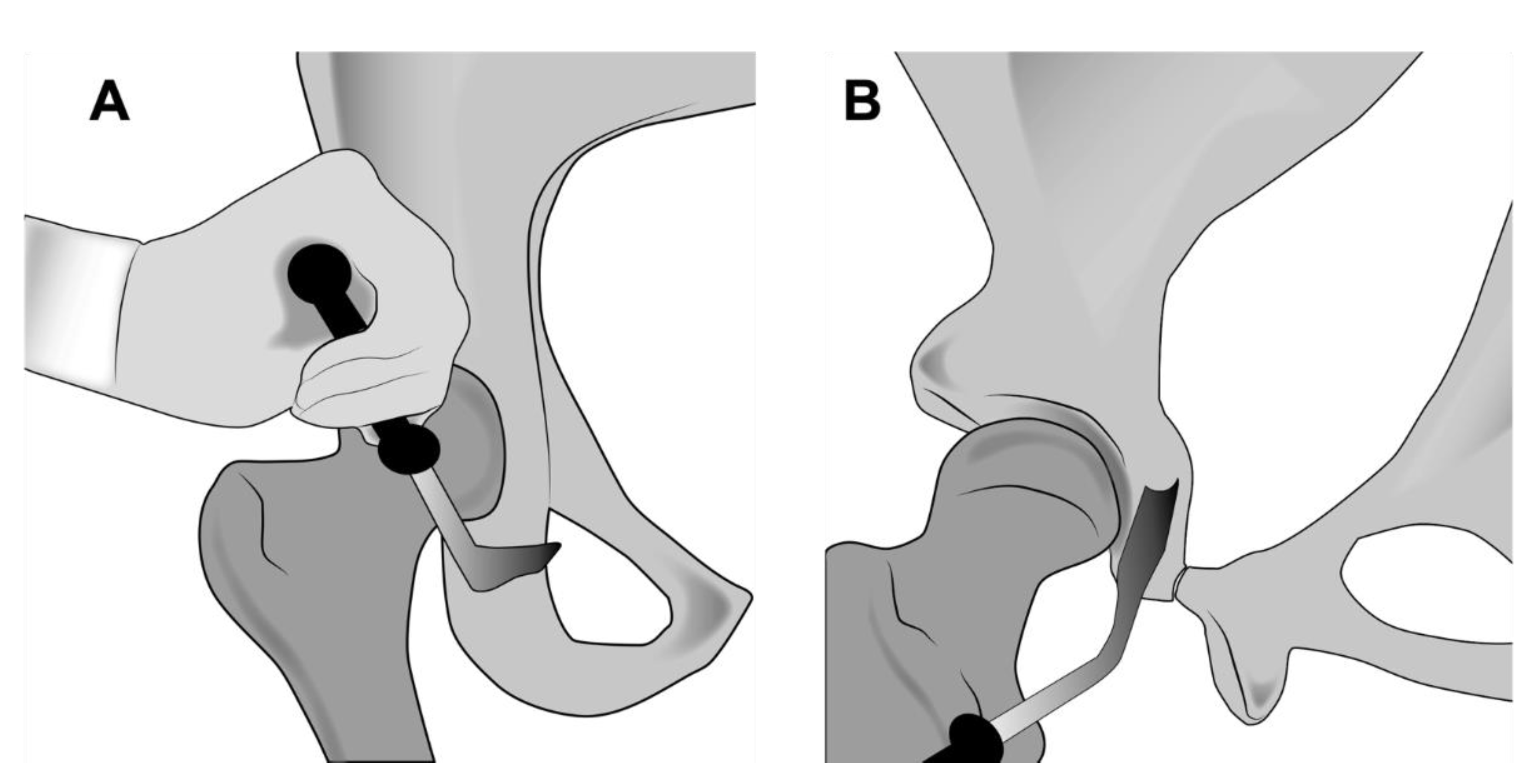
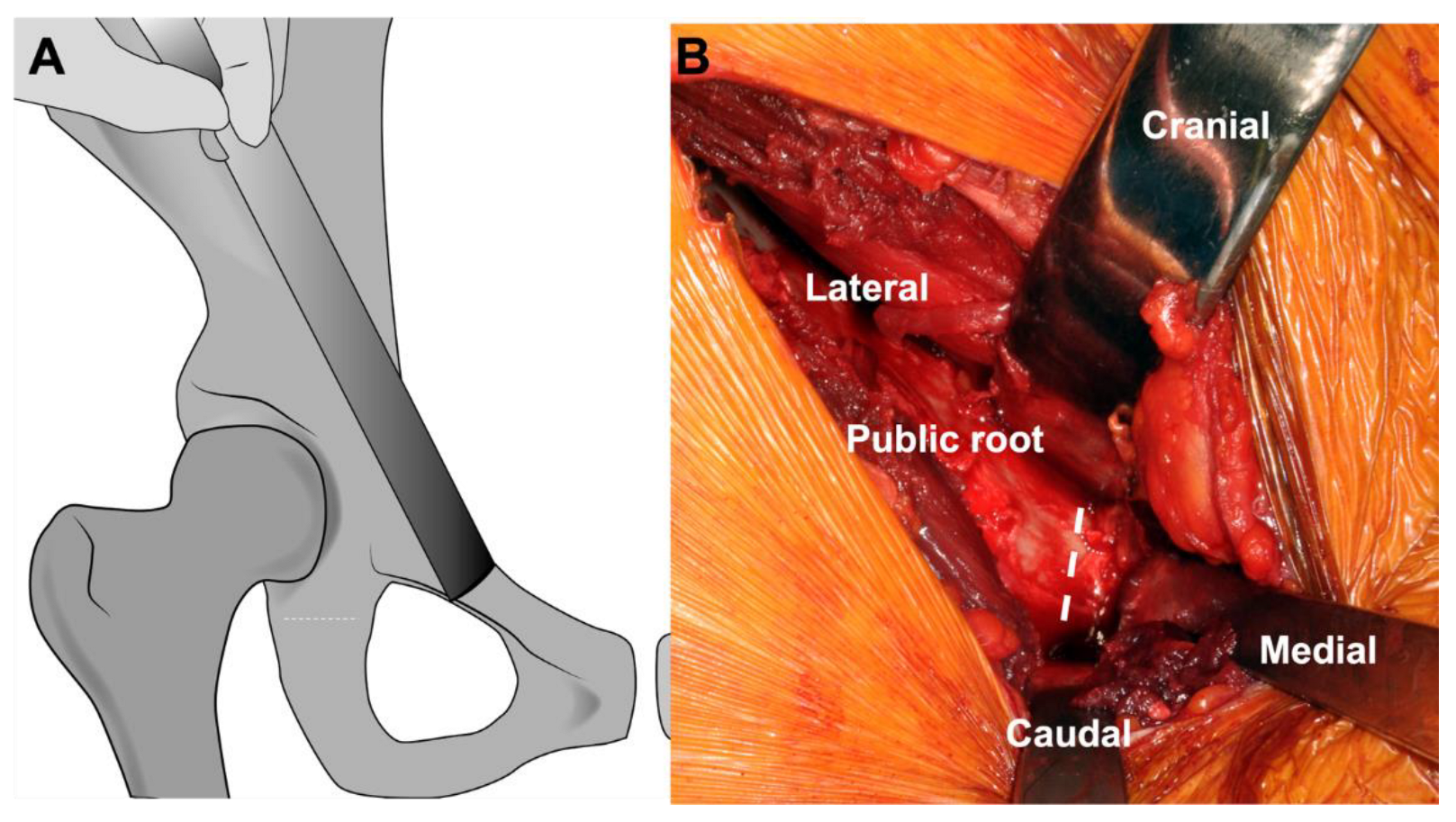
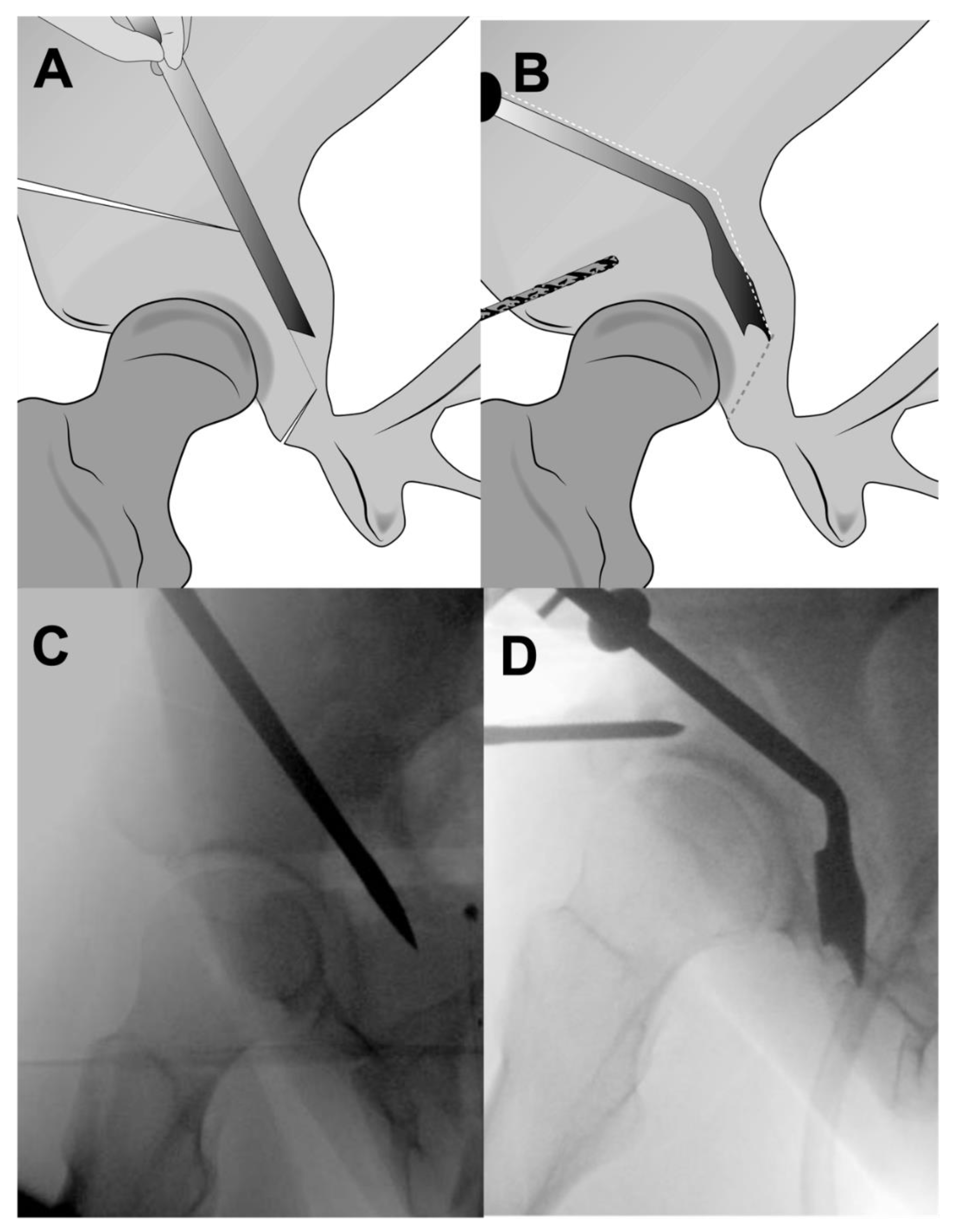
3. Surgical Technique
4. Outcome Research
4.1. Dysplasia
4.2. Acetabular Retroversion
4.3. Factors Influencing PAO Success
5. Potential Complications of the PAO Procedure
6. The PAO Learning Curve
7. Bibliometrics around PAO
8. Conclusions
9. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahmad, S.S.; Giebel, G.M.; Perka, C.; Meller, S.; Pumberger, M.; Hardt, S.; Stöckle, U.; Konrads, C. Survival of the dysplastic hip after periacetabular osteotomy: A meta-analysis. HIP Int. 2021, 11207000211048425. [Google Scholar] [CrossRef] [PubMed]
- Ganz, R.; Klaue, K.; Vinh, T.S.; Mast, J.W. A new periacetabular osteotomy for the treatment of hip dysplasias-technique and preliminary-results. Clin. Orthop. Relat. Res. 1988, 232, 26–36. [Google Scholar] [CrossRef]
- Siebenrock, K.A.; Schöll, E.; Lottenbach, M.; Ganz, R. Bernese periacetabular osteotomy. Clin. Orthop. Relat. Res. 1999, 363, 9–20. [Google Scholar] [CrossRef]
- Hempfing, A.; Leunig, M.; Nötzli, H.P.; Beck, M.; Ganz, R. Acetabular blood flow during Bernese periacetabular osteotomy: An intraoperative study using laser Doppler flowmetry. J. Orthop. Res. 2003, 21, 1145–1150. [Google Scholar] [CrossRef]
- Ahmad, S.S.; Windhagen, H.; Khanduja, V. Back to the Future with Osteotomies around the Hip. J. Clin. Med. 2022, 11, 4446. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.S.; Albers, C.E.; Buchler, L.; Kohl, S.; Ahmad, S.S.; Klenke, F.; Siebenrock, K.A.; Beck, M. The hundred most cited publications in orthopaedic hip research—A bibliometric analysis. Hip Int. 2016, 26, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Zurmühle, C.A.; Anwander, H.; Albers, C.E.; Hanke, M.S.; Steppacher, S.D.; Siebenrock, K.A.; Tannast, M. Periacetabular Osteotomy Provides Higher Survivorship Than Rim Trimming for Acetabular Retroversion. Clin. Orthop. Relat. Res. 2017, 475, 1138–1150. [Google Scholar] [CrossRef]
- Siebenrock, K.A.; Schaller, C.; Tannast, M.; Keel, M.; Büchler, L. Anteverting periacetabular osteotomy for symptomatic acetabular retroversion: Results at ten years. JBJS 2014, 96, 1785–1792. [Google Scholar] [CrossRef]
- Tannast, M.; Hanke, M.S.; Zheng, G.; Steppacher, S.D.; Siebenrock, K.A. What are the radiographic reference values for acetabular under- and overcoverage? Clin. Orthop. Relat. Res. 2015, 473, 1234–1246. [Google Scholar] [CrossRef]
- Albers, C.E.; Rogers, P.; Wambeek, N.; Ahmad, S.S.; Yates, P.J.; Prosser, G.H. Preoperative planning for redirective, periacetabular osteotomies. J. Hip Preserv. Surg. 2017, 4, 276–288. [Google Scholar] [CrossRef]
- Swarup, I.; Zaltz, I.; Robustelli, S.; Sink, E. Outcomes of periacetabular osteotomy for borderline hip dysplasia in adolescent patients. J. Hip Preserv. Surg. 2020, 7, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Leunig, M.; Siebenrock, K.A.; Ganz, R. Rationale of Periacetabular Osteotomy and Background Work. JBJS 2001, 83, 438. [Google Scholar] [CrossRef]
- Lerch, T.D.; Meier, M.K.; Boschung, A.; Steppacher, S.D.; Siebenrock, K.A.; Tannast, M.; Schmaranzer, F. Diagnosis of acetabular retroversion: Three signs positive and increased retroversion index have higher specificity and higher diagnostic accuracy compared to isolated positive cross over sign. Eur. J. Radiol. Open 2022, 9, 100407. [Google Scholar] [CrossRef] [PubMed]
- Steppacher, S.D.; Tannast, M.; Ganz, R.; Siebenrock, K.A. Mean 20-year followup of Bernese periacetabular osteotomy. Clin. Orthop. Relat. Res. 2008, 466, 1633–1644. [Google Scholar] [CrossRef]
- Siebenrock, K.A.; Steppacher, S.D.; Tannast, M.; Büchler, L. Anteverting Periacetabular Osteotomy for Acetabular Retroversion. JBJS Essent. Surg. Tech. 2015, 5, e1. [Google Scholar] [CrossRef]
- Tan, S.H.S.; Tan, J.H.I.; Lim, A.K.S.; Hui, J.H. Periacetabular osteotomy for acetabular retroversion: A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 2021, 107, 103078. [Google Scholar] [CrossRef]
- McClincy, M.P.; Wylie, J.D.; Kim, Y.J.; Millis, M.B.; Novais, E.N. Periacetabular Osteotomy Improves Pain and Function in Patients With Lateral Center-edge Angle Between 18° and 25°, but Are These Hips Really Borderline Dysplastic? Clin. Orthop. Relat. Res. 2019, 477, 1145–1153. [Google Scholar] [CrossRef]
- Marland, J.D.; Wylie, J.D. Periacetabular Osteotomy for Mild or Borderline Acetabular Dysplasia. Oper. Tech. Orthop. 2020, 30, 100782. [Google Scholar] [CrossRef]
- Freiman, S.M.; Schwabe, M.T.; Fowler, L.; Clohisy, J.C.; Nepple, J.J. Prevalence of Borderline Acetabular Dysplasia in Symptomatic and Asymptomatic Populations: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2022, 10, 23259671211040455. [Google Scholar] [CrossRef]
- Murata, Y.; Fukase, N.; Martin, M.; Soares, R.; Pierpoint, L.; Dornan, G.J.; Uchida, S.; Philippon, M.J. Comparison Between Hip Arthroscopic Surgery and Periacetabular Osteotomy for the Treatment of Patients With Borderline Developmental Dysplasia of the Hip: A Systematic Review. Orthop. J. Sports Med. 2021, 9, 23259671211007401. [Google Scholar] [CrossRef]
- Wassilew, G.I.; Hofer, A.; Rakow, A.; Gebhardt, S.; Hoffmann, M.; Janz, V.; Zimmerer, A. [Minimally invasive periacetabular osteotomy for adult hip dysplasia]. Oper. Orthopädie Traumatol. 2022, 34, 275–294. [Google Scholar] [CrossRef] [PubMed]
- Lara, J.; Garín, A.; Herrera, C.; Abara, S.; Besomi, J.; Villegas, D.; Neumann, H.; Tobar, C. Bernese periacetabular osteotomy: Functional outcomes in patients with untreated intra-articular lesions. J. Hip Preserv. Surg. 2020, 7, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Larsen, J.B.; Mechlenburg, I.; Jakobsen, S.S.; Thilleman, T.M.; Søballe, K. 14-year hip survivorship after periacetabular osteotomy: A follow-up study on 1,385 hips. Acta Orthop. 2020, 91, 299–305. [Google Scholar] [CrossRef]
- Isaksen, K.F.; Roscher, E.K.; Iversen, K.S.; Eitzen, I.; Clarke-Jenssen, J.; Nordsletten, L.; Madsen, J.E. Preoperative incipient osteoarthritis predicts failure after periacetabular osteotomy: 69 hips operated through the anterior intrapelvic approach. Hip Int. 2019, 29, 516–526. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.; Schoenecker, P.; Duncan, S.; Goss, C.W.; Thomason, K.; Clohisy, J.C. Intermediate-Term Hip Survivorship and Patient-Reported Outcomes of Periacetabular Osteotomy: The Washington University Experience. JBJS 2018, 100, 218–225. [Google Scholar] [CrossRef]
- Grammatopoulos, G.; Wales, J.; Kothari, A.; Gill, H.S.; Wainwright, A.; Theologis, T. What Is the Early/Mid-term Survivorship and Functional Outcome After Bernese Periacetabular Osteotomy in a Pediatric Surgeon Practice? Clin. Orthop. Relat. Res. 2016, 474, 1216–1223. [Google Scholar] [CrossRef]
- Vahedi, H.; Aalirezaie, A.; Schlitt, P.K.; Parvizi, J. Acetabular Retroversion Is a Risk Factor for Less Optimal Outcome After Femoroacetabular Impingement Surgery. J. Arthroplast. 2019, 34, 1342–1346. [Google Scholar] [CrossRef]
- Matheney, T.; Kim, Y.-J.; Zurakowski, D.; Matero, C.; Millis, M. Intermediate to Long-Term Results Following the Bernese Periacetabular Osteotomy and Predictors of Clinical Outcome. JBJS 2009, 91, 2113–2123. [Google Scholar] [CrossRef]
- Lerch, T.D.; Steppacher, S.D.; Liechti, E.F.; Tannast, M.; Siebenrock, K.A. One-third of Hips After Periacetabular Osteotomy Survive 30 Years With Good Clinical Results, No Progression of Arthritis, or Conversion to THA. Clin. Orthop. Relat. Res. 2017, 475, 1154–1168. [Google Scholar] [CrossRef]
- Albers, C.E.; Steppacher, S.D.; Ganz, R.; Tannast, M.; Siebenrock, K.A. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin. Orthop. Relat. Res. 2013, 471, 1602–1614. [Google Scholar] [CrossRef]
- Troelsen, A.; Elmengaard, B.; Søballe, K. Medium-Term Outcome of Periacetabular Osteotomy and Predictors of Conversion to Total Hip Replacement. JBJS 2009, 91, 2169–2179. [Google Scholar] [CrossRef] [PubMed]
- Stetzelberger, V.M.; Leibold, C.S.; Steppacher, S.D.; Schwab, J.M.; Siebenrock, K.A.; Tannast, M. The Acetabular Wall Index Is Associated with Long-term Conversion to THA after PAO. Clin. Orthop. Relat. Res. 2021, 479, 1052–1065. [Google Scholar] [CrossRef] [PubMed]
- Novais, E.N.; Carry, P.M.; Kestel, L.A.; Ketterman, B.; Brusalis, C.M.; Sankar, W.N. Does Surgeon Experience Impact the Risk of Complications After Bernese Periacetabular Osteotomy? Clin. Orthop. Relat. Res. 2017, 475, 1110–1117. [Google Scholar] [CrossRef] [PubMed]
- Zaltz, I.; Baca, G.; Kim, Y.-J.; Schoenecker, P.; Trousdale, R.; Sierra, R.; Sucato, D.; Sink, E.; Beaulé, P.; Millis, M.B.; et al. Complications Associated with the Periacetabular Osteotomy: A Prospective Multicenter Study. JBJS 2014, 96, 1967–1974. [Google Scholar] [CrossRef]
- Cates, R.A.; Boon, A.J.; Trousdale, R.T.; Douge, A.; Sierra, R.J. Prospective evaluation of lateral femoral cutaneous nerve injuries during periacetabular osteotomy. J. Hip Preserv. Surg. 2019, 6, 77–85. [Google Scholar] [CrossRef]
- Peters, C.L.; Erickson, J.A.; Hines, J.L. Early Results of the Bernese Periacetabular Osteotomy: The Learning Curve at an Academic Medical Center. JBJS 2006, 88, 1920–1926. [Google Scholar] [CrossRef]
- Howie, D.W.; Beck, M.; Costi, K.; Pannach, S.M.; Ganz, R. Mentoring in complex surgery: Minimising the learning curve complications from peri-acetabular osteotomy. Int. Orthop. 2012, 36, 921–925. [Google Scholar] [CrossRef]
- Davey, J.P.; Santore, R.F. Complications of periacetabular osteotomy. Clin. Orthop. Relat. Res. 1999, 363, 33–37. [Google Scholar] [CrossRef]
- Trousdale, R.; Cabanela, M. Lessons learned after more than 250 periacetabular osteotomies. Acta Orthop. Scand. 2003, 74, 119–126. [Google Scholar] [CrossRef]
- Smith, G.W.; Lightfoot, N.J.; Munro, J.T.; Boyle, M.J. Does hip preservation fellowship training flatten the learning curve associated with periacetabular osteotomy? J. Hip Preserv. Surg. 2020, 7, 563–569. [Google Scholar] [CrossRef]
- Kiarostami, P.; Dennler, C.; Roner, S.; Sutter, R.; Fürnstahl, P.; Farshad, M.; Rahm, S.; Zingg, P.O. Augmented reality-guided periacetabular osteotomy—proof of concept. J. Orthop. Surg. Res. 2020, 15, 540. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.; Picard-Aitken, M.; Côté, G.; Caruso, J.; Valentim, R.; Edmonds, S.; Williams, G.T.; Macaluso, B.; Robitaille, J.-P.; Bastien, N.; et al. Bibliometrics as a performance measurement tool for research evaluation: The case of research funded by the National Cancer Institute of Canada. Am. J. Eval. 2010, 31, 66–83. [Google Scholar] [CrossRef]
- Markhardt, B.K.; Beilfuss, M.A.; Hetzel, S.J.; Goodspeed, D.C.; Spiker, A.M. 3D-printed models for periacetabular osteotomy surgical planning. J. Hip Preserv. Surg. 2021, 7, 748–754. [Google Scholar] [CrossRef] [PubMed]
- Matthews, J.H.; Shields, J.S. The Clinical Application of Augmented Reality in Orthopaedics: Where Do We Stand? Curr. Rev. Musculoskelet. Med. 2021, 14, 316–319. [Google Scholar] [CrossRef]
- Löchel, J.; Janz, V.; Leopold, V.J.; Krämer, M.; Wassilew, G.I. Transversus abdominis Plane Block for Improved Early Postoperative Pain Management after Periacetabular Osteotomy: A Randomized Clinical Trial. J. Clin. Med. 2021, 10, 394. [Google Scholar] [CrossRef]
- Hajewski, C.; Anthony, C.A.; Rojas, E.O.; Westermann, R.; Willey, M. Detailing postoperative pain and opioid utilization after periacetabular osteotomy with automated mobile messaging. J. Hip Preserv. Surg. 2019, 6, 370–376. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmad, S.S.; Haertlé, M.; Konrads, C.; Derksen, A.; Windhagen, H.; Wirries, N. The Scientific Evolution of Periacetabular Osteotomy: A Global Review. J. Clin. Med. 2022, 11, 6099. https://doi.org/10.3390/jcm11206099
Ahmad SS, Haertlé M, Konrads C, Derksen A, Windhagen H, Wirries N. The Scientific Evolution of Periacetabular Osteotomy: A Global Review. Journal of Clinical Medicine. 2022; 11(20):6099. https://doi.org/10.3390/jcm11206099
Chicago/Turabian StyleAhmad, Sufian S., Marco Haertlé, Christian Konrads, Alexander Derksen, Henning Windhagen, and Nils Wirries. 2022. "The Scientific Evolution of Periacetabular Osteotomy: A Global Review" Journal of Clinical Medicine 11, no. 20: 6099. https://doi.org/10.3390/jcm11206099
APA StyleAhmad, S. S., Haertlé, M., Konrads, C., Derksen, A., Windhagen, H., & Wirries, N. (2022). The Scientific Evolution of Periacetabular Osteotomy: A Global Review. Journal of Clinical Medicine, 11(20), 6099. https://doi.org/10.3390/jcm11206099





