Usefulness of Adding Maspin Staining to p53 Staining for EUS-FNA Specimens of Pancreatic Ductal Adenocarcinoma
Abstract
1. Introduction
2. Materials and Methods
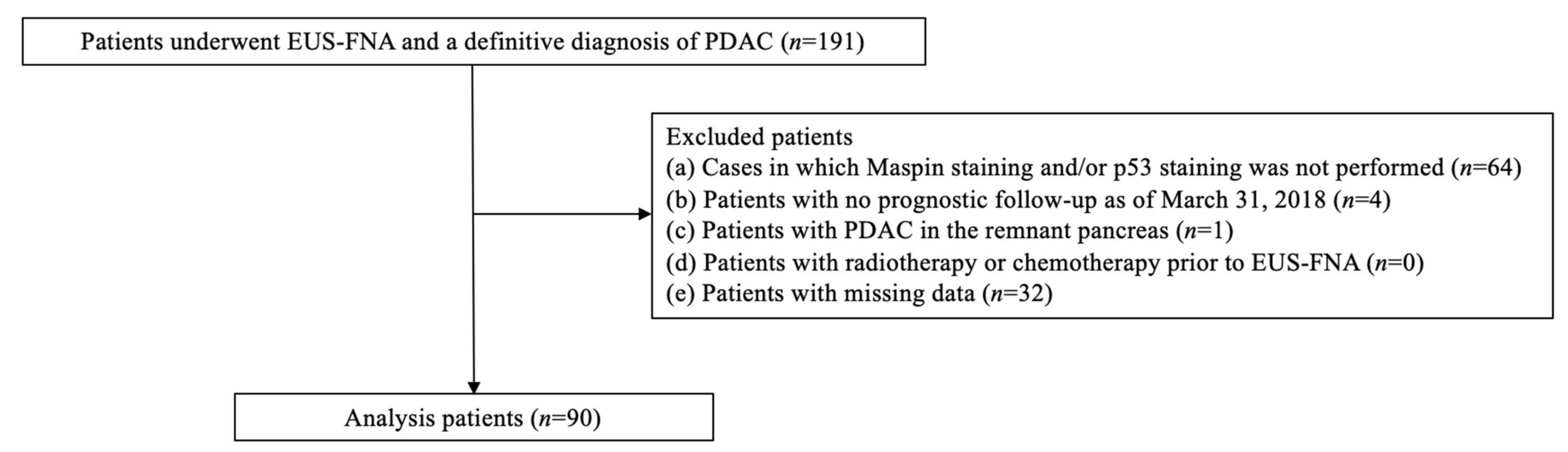
2.1. Study Design
2.2. Patients/Study Population
2.3. Procedure and Intervention
2.4. Histological Evaluation
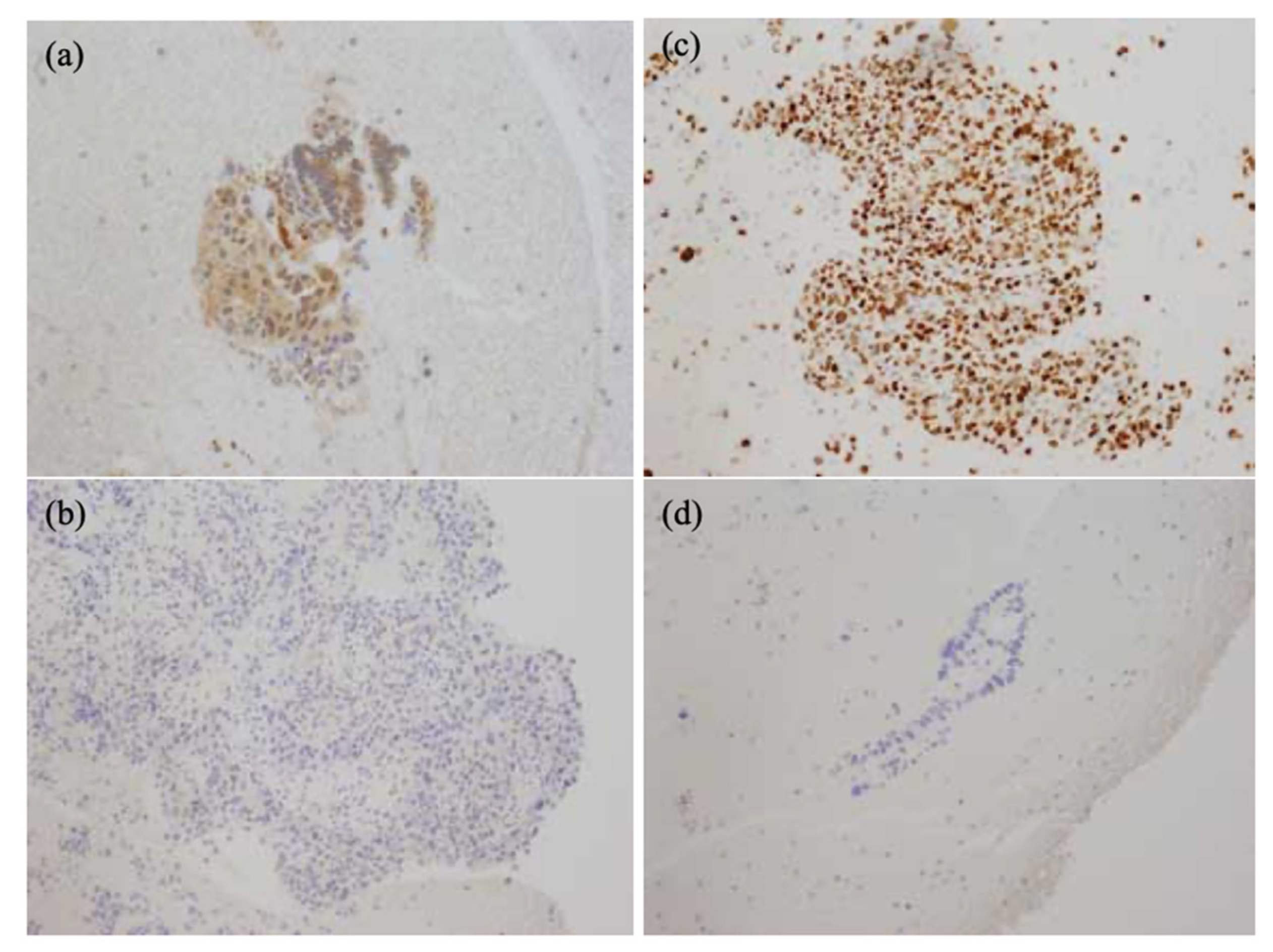
2.5. Evaluation of Immunohistochemical Staining
2.6. Investigation of the Patient Prognosis
2.7. Statistical Analysis
3. Results
3.1. Background of the Patients
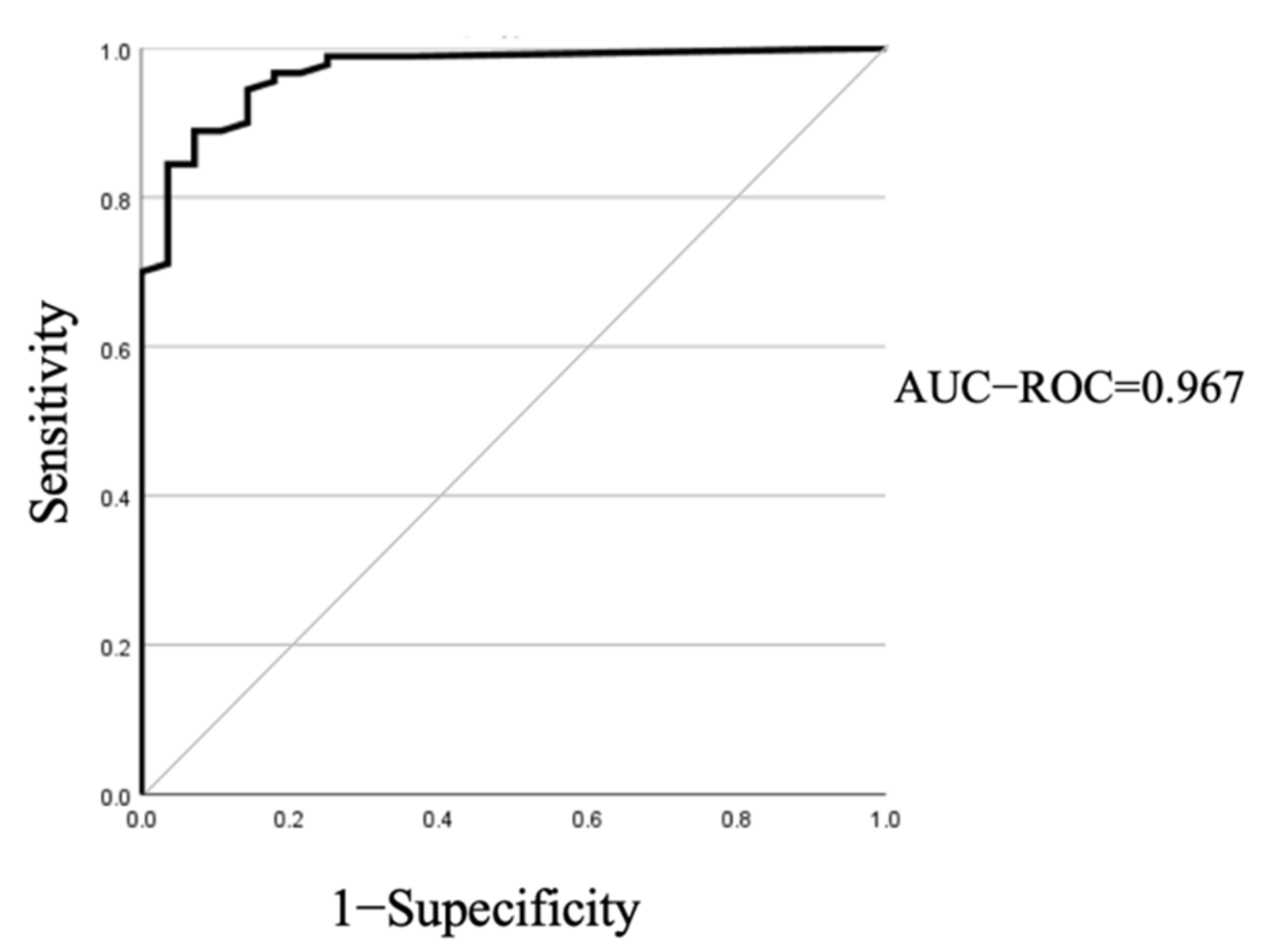
3.2. Setting the Cut-Off Value of Maspin
3.3. Examination of the Maspin Additive Effect
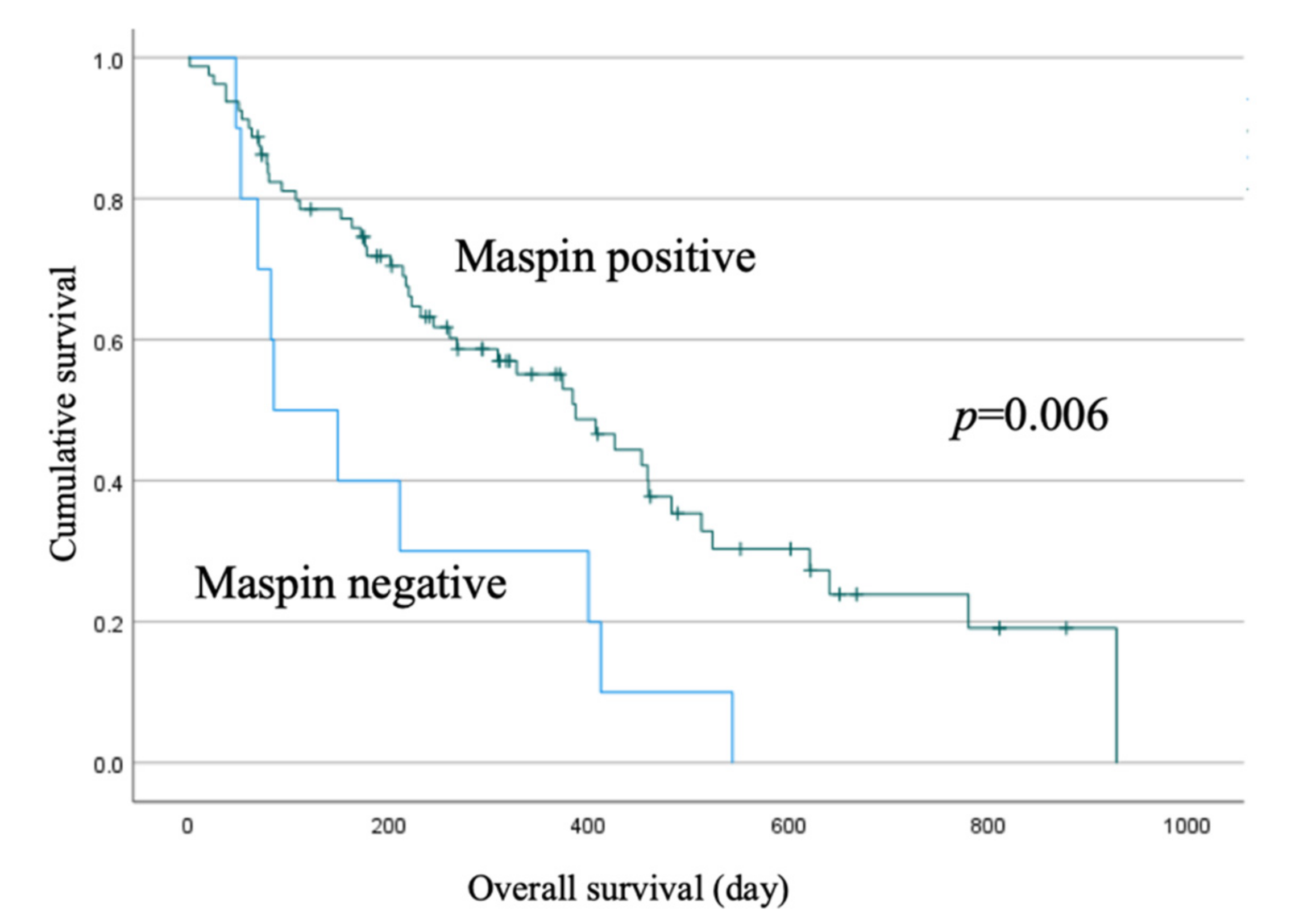
3.4. Clinicopathologic Study of Maspin-positive and Maspin-Negative Patients
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vilmann, P.; Jacobsen, G.K.; Henriksen, F.W.; Hancke, S. Endoscopic ultrasonography with guided fine needle aspiration biopsy in pancreatic disease. Gastrointest. Endosc. 1992, 38, 172–173. [Google Scholar] [CrossRef]
- Puli, S.R.; Bechtold, M.L.; Buxbaum, J.L.; Eloubeidi, M.A. How good is endoscopic ultrasound-guided fine-needle aspiration in diagnosing the correct etiology for a solid pancreatic mass? A meta-analysis and systematic review. Pancreas 2013, 42, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Haba, S.; Yamao, K.; Bhatia, V.; Mizuno, N.; Hara, K.; Hijioka, S.; Imaoka, H.; Niwa, Y.; Tajika, M.; Kondo, S.; et al. Diagnostic ability and factors affecting accuracy of endoscopic ultrasound-guided fine needle aspiration for pancreatic solid lesions: Japanese large single center experience. J. Gastroenterol. 2013, 48, 973–981. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, T.; Shirai, Y.; Nakamura, N.; Hironaka, S.; Hara, T.; Denda, T. Usefulness of brush cytology combined with pancreatic juice cytology in the diagnosis of pancreatic cancer: Significance of pancreatic juice cytology after brushing. Pancreas 2012, 41, 1225–1229. [Google Scholar] [CrossRef]
- Agarwal, B.; Krishna, N.B.; Labundy, J.L.; Safdar, R.; Akduman, E.I. EUS and/or EUS-guided FNA in patients with CT and/or magnetic resonance imaging findings of enlarged pancreatic head or dilated pancreatic duct with or without a dilated common bile duct. Gastrointest. Endosc. 2008, 68, 237–242. [Google Scholar] [CrossRef]
- Krishna, N.B.; LaBundy, J.L.; Saripalli, S.; Safdar, R.; Agarwal, B. Diagnostic value of EUS-FNA in patients suspected of having pancreatic cancer with a focal lesion on CT scan/MRI but without obstructive jaundice. Pancreas 2009, 38, 625–630. [Google Scholar] [CrossRef]
- Sreenarasimhaiah, J. Efficacy of endoscopic ultrasound in characterizing mass lesions in chronic pancreatitis. J. Clin. Gastroenterol. 2008, 42, 81–85. [Google Scholar] [CrossRef]
- Eloubeidi, M.A.; Jhala, D.; Chhieng, D.C.; Chen, V.K.; Eltoum, I.; Vickers, S.; Mel, W.; Jhala, N. Yield of endoscopic ultrasound-guided fine-needle aspiration biopsy in patients with suspected pancreatic carcinoma. Cancer 2003, 99, 285–292. [Google Scholar] [CrossRef]
- Ardengh, J.C.; Lopes, C.V.; de Lima, L.F.; de Oliveria, J.R.; Venco, F.; Santo, G.C.; Modena, J.L. Diagnosis of pancreatic tumors by endoscopic ultrasound-guided fine-needle aspiration. World J. Gastroenterol. 2007, 13, 3112–3116. [Google Scholar] [CrossRef]
- Yusuf, T.E.; Ho, S.; Pavey, D.A.; Michael, H.; Gress, F.G. Retrospective analysis of the utility of endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) in pancreatic masses, using a 22-gauge or 25-gauge needle system: A multicenter experience. Endoscopy 2009, 41, 445–448. [Google Scholar] [CrossRef]
- Varadarajulu, S.; Tamhane, A.; Eloubeidi, M.A. Yield of EUS-guided FNA of pancreatic masses in the presence or the absence of chronic pancreatitis. Gastrointest. Endosc. 2005, 62, 728–736. [Google Scholar] [CrossRef]
- Lin, F.; Chen, Z.E.; Wang, H.L. Utility of immunohistochemistry in the pancreatobiliary tract. Arch. Pathol. Lab. Med. 2015, 139, 24–38. [Google Scholar] [CrossRef]
- Furuhata, A.; Minamiguchi, S.; Shirahase, H.; Kodama, Y.; Adachi, S.; Sakurai, T.; Haga, H. Immunohistochemical Antibody Panel for the Differential Diagnosis of Pancreatic Ductal Carcinoma From Gastrointestinal Contamination and Benign Pancreatic Duct Epithelium in Endoscopic Ultrasound-Guided Fine-Needle Aspiration 2017, 46, 531–538. Pancreas 2017, 46, 531–538. [Google Scholar] [CrossRef]
- DiGiuseppe, J.A.; Hruban, R.H.; Goodman, S.N.; Polak, M.; van den Berg, F.M.; Allison, D.C.; Cameron, J.L.; Offerhaus, G.J. Overexpression of p53 protein in adenocarcinoma of the pancreas. Am. J. Clin. Pathol 1994, 101, 684–688. [Google Scholar] [CrossRef]
- Lee, C.S.; Rush, M.; Charalambous, D.; Rode, J. Immunohistochemical demonstration of the p53 tumour suppressor gene product in cancer of the pancreas and chronic pancreatitis. J. Gastroenterol. Hepatol. 1993, 8, 465–469. [Google Scholar] [CrossRef]
- Itoi, T.; Takei, K.; Sofuni, A.; Itokawa, F.; Tsuchiya, T.; Kurihara, T.; Nakamura, K.; Moriyasu, F.; Tsuchida, A.; Kasuya, K. Immunohistochemical analysis of p53 and MIB-1 in tissue specimens obtained from endoscopic ultrasonography-guided fine needle aspiration biopsy for the diagnosis of solid pancreatic masses. Oncol. Rep. 2005, 13, 229–234. [Google Scholar]
- van Heek, T.; Rader, A.E.; Offerhaus, G.J.; McCarthy, D.M.; Goggins, M.; Hruban, R.H.; Wilentz, R.E. K-ras, p53, and DPC4 (MAD4) alterations in fine-needle aspirates of the pancreas: A molecular panel correlates with and supplements cytologic diagnosis. Am. J. Clin. Pathol. 2002, 11, 755–765. [Google Scholar] [CrossRef]
- Zou, Z.; Anisowicz, A.; Hendrix, M.J.; Thor, A.; Neveu, M.; Sheng, S.; Rafidi, K.; Seftor, E.; Sager, R. Maspin, a serpin with tumor-suppressing activity in human mammary epithelial cells. Science 1994, 263, 526–529. [Google Scholar] [CrossRef]
- Maass, N.; Hojo, T.; Ueding, M.; Lüttges, J.; Klöppel, G.; Jonat, W.; Nagasaki, K. Expression of the tumor suppressor gene Maspin in human pancreatic cancers. Clin. Cancer Res. 2001, 7, 812–817. [Google Scholar]
- Fitzgerald, M.; Oshiro, M.; Holtan, N.; Krager, K.; Cullen, J.J.; Futscher, B.W.; Domann, F.E. Human pancreatic carcinoma cells activate maspin expression through loss of epigenetic control. Neoplasia 2003, 5, 427–436. [Google Scholar] [CrossRef]
- Jahng, A.W.; Reicher, S.; Chung, D.; Varela, D.; Chhablani, R.; Dev, A.; Pham, B.; Nieto, J.; Venegas, R.J.; French, S.W.; et al. Staining for p53 and Ki-67 increases the sensitivity of EUS-FNA to detect pancreatic malignancy. World J. Gastrointest. Endosc. 2010, 2, 362–368. [Google Scholar] [CrossRef]
- Yemelyanova, A.; Vang, R.; Kshirsagar, M.; Lu, D.; Marks, M.A.; Shih, I.M.; Kurman, R.J. Immunohistochemical staining patterns of p53 can serve as a surrogate marker for TP53 mutations in ovarian carcinoma: An immunohistochemical and nucleotide sequencing analysis. Mod. Pathol. 2011, 24, 1248–1253. [Google Scholar] [CrossRef]
- Mikata, R.; Yasui, S.; Kishimoto, T.; Kouchi, Y.; Shingyoji, A.; Senoo, J.; Takahashi, K.; Nagashima, H.; Kusakabe, Y.; Ohyama, H.; et al. Diagnostic value of IMP3 and p53 immunohistochemical staining in EUS-guided fine-needle aspiration for solid pancreatic tumors. Sci. Rep. 2021, 11, 17257. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.; Shi, J.; Liu, H.; Hull, M.E.; Dupree, W.; Prichard, J.W.; Brown, R.E.; Zhang, J.; Wang, H.L.; Schuerch, C. Diagnostic utility of S100P and von Hippel—Lindau gene product (pVHL) in pancreatic adenocarcinoma-with implication of their roles in early tumorigenesis. Am. J. Surg. Pathol. 2008, 32, 78–91. [Google Scholar] [CrossRef]
- Goldstein, N.S.; Bassi, D. Cytokeratins 7, 17, and 20 reactivity in pancreatic and ampulla of vater adenocarcinomas. Percentage of positivity and distribution is affected by the cut-point threshold. Am. J. Clin. Pathol. 2001, 115, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Deng, H.; Shi, J.; Wilkerson, M.; Meschter, S.; Dupree, W.; Lin, F. Usefulness of S100P in diagnosis of adenocarcinoma of pancreas on fine-needle aspiration biopsy specimens. Am. J. Clin. Pathol. 2008, 129, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Wachter, D.L.; Schlabrakowski, A.; Hoegel, J.; Kristiansen, G.; Hartmann, A.; Riener, M.O. Diagnostic value of immunohistochemical IMP3 expression in core needle biopsies of pancreatic ductal adenocarcinoma. Am. J. Surg. Pathol. 2011, 35, 873–877. [Google Scholar] [CrossRef]
- Hassan, R.; Laszik, Z.G.; Lerner, M.; Raffeld, M.; Postier, R.; Brackett, D. Mesothelin is overexpressed in pancreaticobiliary adenocarcinomas but not in normal pancreas and chronic pancreatitis. Am. J. Clin. Pathol. 2005, 124, 838–845. [Google Scholar] [CrossRef]
- Nash, J.W.; Bhardwaj, A.; Wen, P.; Frankel, W.L. Maspin is useful in the distinction of pancreatic adenocarcinoma from chronic pancreatitis: A tissue microarray based study. Appl. Immunohistochem. Mol. Morphol. 2007, 15, 59–63. [Google Scholar] [CrossRef]
- Oh, Y.L.; Song, S.Y.; Ahn, G. Expression of maspin in pancreatic neoplasms: Application of maspin immunohistochemistry to the differential diagnosis. Appl. Immunohistochem. Mol. Morphol. 2002, 10, 62–66. [Google Scholar] [CrossRef]
- Mamdouh, M.M.; Okasha, H.; Shaaban, H.A.M.; Hafez, N.H.; El-Gemeie, E.H. Role of Maspin, CK17 and Ki-67 Immunophenotyping in Diagnosing of Pancreatic Ductal Adenocarcinoma in Endoscopic Ultrasound-Guided Fine Needle Aspiration Cytology. Asian Pac. J. Cancer Prev. 2021, 22, 3299–3307. [Google Scholar] [CrossRef]
- Aksoy-Altinboga, A.; Baglan, T.; Umudum, H.; Ceyhan, K. Diagnostic Value of S100p, IMP3, Maspin, and pVHL in the Differantial Diagnosis of Pancreatic Ductal Adenocarcinoma and Normal/chronic Pancreatitis in Fine Needle Aspiration Biopsy. J. Cytol. 2018, 35, 247–251. [Google Scholar] [CrossRef]
- Liu, H.; Shi, J.; Anandan, V.; Wang, H.L.; Diehl, D.; Blansfield, J.; Gerhard, G.; Lin, F. Reevaluation and identification of the best immunohistochemical panel (pVHL, Maspin, S100P, IMP-3) for ductal adenocarcinoma of the pancreas. Arch. Pathol. Lab. Med. 2012, 136, 601–609. [Google Scholar] [CrossRef]
- Maass, N.; Nagasaki, K.; Ziebart, M.; Mundhenke, C.; Jonat, W. Expression and regulation of tumor suppressor gene maspin in breast cancer. Clin. Breast Cancer 2002, 3, 281–287. [Google Scholar] [CrossRef]
- Sheng, S.; Carey, J.; Seftor, E.A.; Dias, L.; Hendrix, M.J.; Sager, R. Maspin acts at the cell membrane to inhibit invasion and motility of mammary and prostatic cancer cells. Proc. Natl. Acad. Sci. USA 1996, 93, 11669–11674. [Google Scholar] [CrossRef]
- Cao, D.; Zhang, Q.; Wu, L.S.; Salaria, S.N.; Winter, J.W.; Hruban, R.H.; Goggins, M.S.; Abbruzzese, J.L.; Maitra, A.; Ho, L. Prognostic significance of maspin in pancreatic ductal adenocarcinoma: Tissue microarray analysis of 223 surgically resected cases. Mod. Pathol. 2007, 20, 570–578. [Google Scholar] [CrossRef]
- Sato, N.; Fukushima, N.; Matsubayashi, H.; Goggins, M. Identification of maspin and S100P as novel hypomethylation targets in pancreatic cancer using global gene expression profiling. Oncogene 2004, 23, 1531–1538. [Google Scholar] [CrossRef]
- Guerra, C.; Schuhmacher, A.J.; Cañamero, M.; Grippo, P.J.; Verdaguer, L.; Pérez-Gallego, L.; Dubus, P.; Sandgren, E.P.; Barbacid, M. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell 2007, 11, 291–302. [Google Scholar] [CrossRef]
- Jones, S.; Zhang, X.; Parsons, D.W.; Lin, J.C.; Leary, R.J.; Angenendt, P.; Mankoo, P.; Carter, H.; Kamiyama, H.; Jimeno, A.; et al. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science 2008, 321, 1801–1806. [Google Scholar] [CrossRef]
- Kanda, M.; Matthaei, H.; Wu, J.; Hong, S.M.; Yu, J.; Borges, M.; Hruban, R.H.; Maitra, A.; Kinzler, K.; Vogelstein, B.; et al. Presence of somatic mutations in most early-stage pancreatic intraepithelial neoplasia. Gastroenterology 2012, 142, 730–733. [Google Scholar] [CrossRef]
- Murphy, S.J.; Hart, S.N.; Lima, J.F.; Kipp, B.R.; Klebig, M.; Winters, J.L.; Szabo, C.; Zhang, L.; Eckloff, B.W.; Petersen, G.M.; et al. Genetic alterations associated with progression from pancreatic intraepithelial neoplasia to invasive pancreatic tumor. Gastroenterology 2013, 145, 1098–1109. [Google Scholar] [CrossRef]
- Uchinaka, E.I.; Sakabe, T.; Hanaki, T.; Tokuyasu, N.; Sakamoto, T.; Honjo, S.; Fujiwara, Y.; Umekita, Y. Cytoplasmic-only Expression of Maspin Predicts Unfavorable Prognosis in Patients With Pancreatic Ductal Adenocarcinoma. Anticancer Res. 2021, 41, 2543–2552. [Google Scholar] [CrossRef]
- Ohike, N.; Maass, N.; Mundhenke, C.; Biallek, M.; Zhang, M.; Jonat, W.; Lüttges, J.; Morohoshi, T.; Klöppel, G.; Nagasaki, K. Clinicopathological significance and molecular regulation of maspin expression in ductal adenocarcinoma of the pancreas. Cancer Lett. 2003, 199, 193–200. [Google Scholar] [CrossRef]
| Male/Female (n = 90) | 66/34 |
|---|---|
| Age [median (range)] | 71 (42–90) |
| Tumor size (mm) [median (range)] | 29.9 (10–64) |
| Location of pancreatic lesion (Uncinate process/head/body/tail) | 11/42/26/11 |
| Tumor marker [median (range)] | |
| CA19-9 (U/mL) | 526.5 (2–12,000) |
| CEA (ng/mL) | 4.1 (0.6–750) |
| DUPAN2 (U/mL) | 370 (25–280,000) |
| SPAN1 (U/mL) | 100 (5–90,000) |
| TNM-Staging | |
| T1/T2/T3/T4 | 11/13/42/24 |
| N0/N1 | 52/38 |
| M0/M1 | 46/44 |
| Stage | |
| I/II/III/IV | 11/21/14/44 |
| PDAC (n = 90) | Benign (n = 28) | |
|---|---|---|
| p53 | 44 (48.9%) | 0 (0%) |
| Maspin | 80 (88.9%) | 3 (10.7%) |
| p53+maspin | 85 (94.4%) | 3 (10.7%) |
| Marker | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Youden | Cohen’s Kappa (κ) Coefficient (95%CI) | p-Value † | PABAK (95%CI) |
|---|---|---|---|---|---|---|---|---|
| H&E | 97.8 | 100 | 100 | 93.3 | 0.978 | 0.954 (0.774–1.135) | <0.001 | 0.966 (0.880–0.996) |
| p53 | 48.9 | 100 | 100 | 62.1 | 0.489 | 0.312 (0.181–0.443) | <0.001 | 0.220 (0.032–0.397) |
| Maspin | 88.9 | 92.9 | 97.5 | 72.2 | 0.818 | 0.720 (0.541–0.898) | <0.001 | 0.780 (0.638–0.880) |
| Maspin + p53 | 94.4 | 92.9 | 97.7 | 83.9 | 0.873 | 0.817 (0.637–0.997) | <0.001 | 0.864 (0.742–0.941) |
| H&E +p53 | 97.8 | 100 | 100 | 93.3 | 0.978 | 0.954 (0.774–1.135) | <0.001 | 0.966 (0.880–0.996) |
| H&E + Maspin | 100 | 100 | 100 | 100 | 1.000 | 1.000 (0.820–1.180) | <0.001 | 1.000 (0.938–1.00) |
| H&E + Maspin +p53 | 100 | 100 | 100 | 100 | 1.000 | 1.000 (0.820–1.180) | <0.001 | 1.000 (0.938–1.00) |
| Clinicopathological Factors | Maspin Status | p-Value † | |
|---|---|---|---|
| Maspin Positive (n = 80) | Maspin Negative (n = 10) | ||
| Sex (M:F) | 50 | 6 | 1.00 |
| Age [median (range)] | 70 | 69.6 | 0.912 |
| Tumor size (mm) [median (range)] | 28.9 | 37.7 | 0.008 |
| Location of pancreatic lesion | 0.027 | ||
| Uncinate process | 10 | 1 | |
| Head | 40 | 2 | |
| Body | 20 | 6 | |
| Tail | 10 | 1 | |
| Histological type | 0.033 | ||
| Well | 29 | 1 | |
| Moderate | 33 | 3 | |
| Poor | 18 | 6 | |
| Tumor marker [median (range)] | |||
| CA19-9 (U/mL) | 601.5 (2–12,000) | 238 (7–6710) | 0.634 |
| CEA (ng/mL) | 4.6 (0.6–750) | 3.3 (2–10.7) | 0.351 |
| DUPAN2 | 365 (25–280,000) | 470 (25–4800) | 0.57 |
| SPAN1 | 94 (16–90,000) | 150 (5–1950) | 0.493 |
| T (T1/T2/T3/T4) | 10/11/39/20 | 1/2/3/4 | 0.636 |
| N (N0/N1) | 48/32 | 4/6 | 0.312 |
| M (M0/M1) | 44/36 | 2/8 | 0.047 |
| Stage (Ⅰ/Ⅱ/Ⅲ/Ⅳ) | 10/21/13/36 | 1/0/1/8 | 0.163 |
| Treatment | 0.327 | ||
| Operation | 23 | 3 | |
| Chemotherapy | 25 | 1 | |
| Best supportive care | 32 | 6 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukushi, K.; Yamamiya, A.; Tominaga, K.; Abe, Y.; Hoshi, K.; Nagashima, K.; Kashima, K.; Kunogi, Y.; Sakuma, F.; Yamagishi, H.; et al. Usefulness of Adding Maspin Staining to p53 Staining for EUS-FNA Specimens of Pancreatic Ductal Adenocarcinoma. J. Clin. Med. 2022, 11, 6097. https://doi.org/10.3390/jcm11206097
Fukushi K, Yamamiya A, Tominaga K, Abe Y, Hoshi K, Nagashima K, Kashima K, Kunogi Y, Sakuma F, Yamagishi H, et al. Usefulness of Adding Maspin Staining to p53 Staining for EUS-FNA Specimens of Pancreatic Ductal Adenocarcinoma. Journal of Clinical Medicine. 2022; 11(20):6097. https://doi.org/10.3390/jcm11206097
Chicago/Turabian StyleFukushi, Koh, Akira Yamamiya, Keiichi Tominaga, Yoko Abe, Koki Hoshi, Kazunori Nagashima, Ken Kashima, Yasuhito Kunogi, Fumi Sakuma, Hidetsugu Yamagishi, and et al. 2022. "Usefulness of Adding Maspin Staining to p53 Staining for EUS-FNA Specimens of Pancreatic Ductal Adenocarcinoma" Journal of Clinical Medicine 11, no. 20: 6097. https://doi.org/10.3390/jcm11206097
APA StyleFukushi, K., Yamamiya, A., Tominaga, K., Abe, Y., Hoshi, K., Nagashima, K., Kashima, K., Kunogi, Y., Sakuma, F., Yamagishi, H., Ishida, K., Haruyama, Y., & Irisawa, A. (2022). Usefulness of Adding Maspin Staining to p53 Staining for EUS-FNA Specimens of Pancreatic Ductal Adenocarcinoma. Journal of Clinical Medicine, 11(20), 6097. https://doi.org/10.3390/jcm11206097







