Peripheral Nerve Block for Pain Management after Total Hip Arthroplasty: A Retrospective Study with Propensity Score Matching
Abstract
1. Introduction
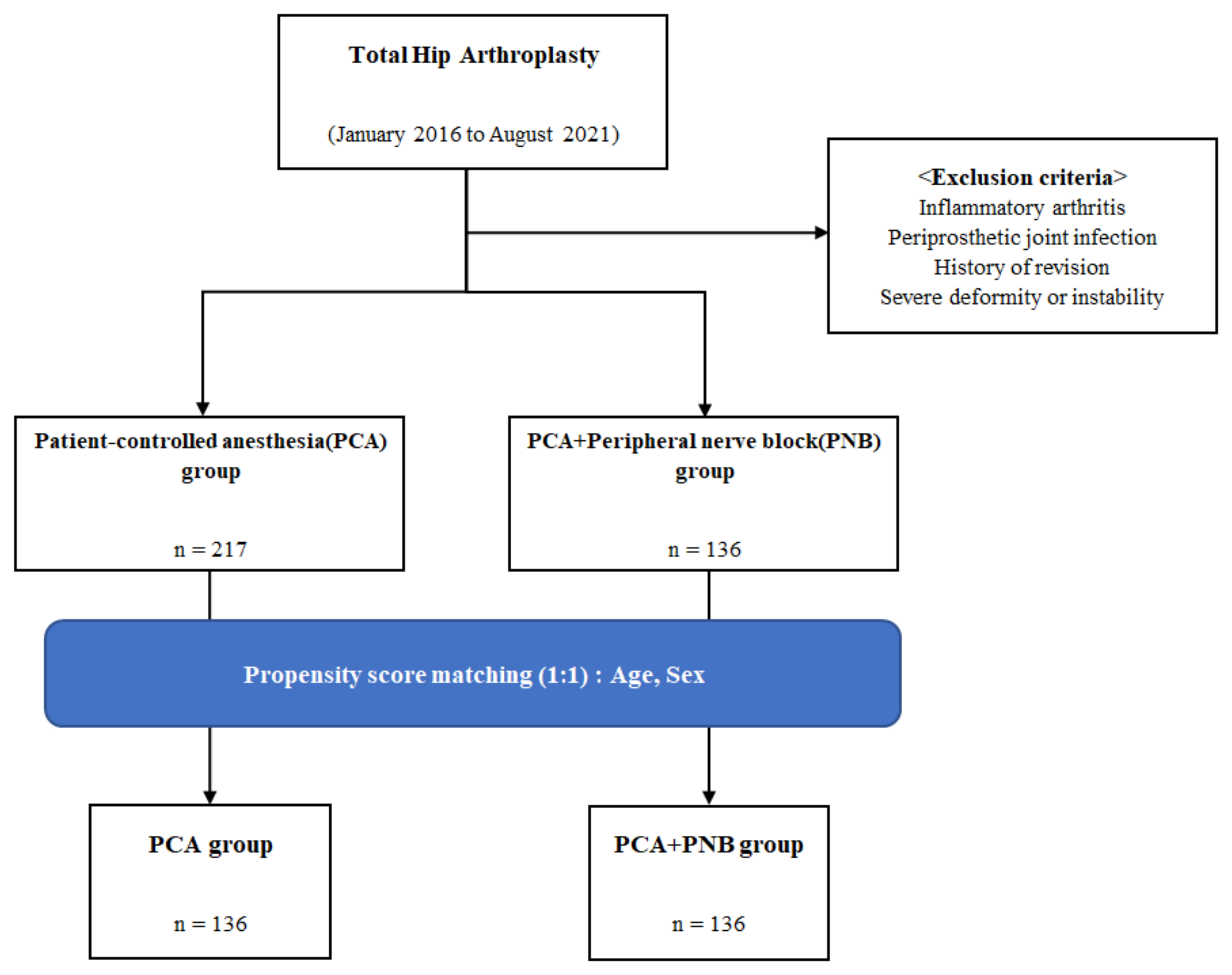
2. Materials and Methods
2.1. Data Collection
2.2. Outcome Measurements
2.3. Statistical Analysis
3. Results
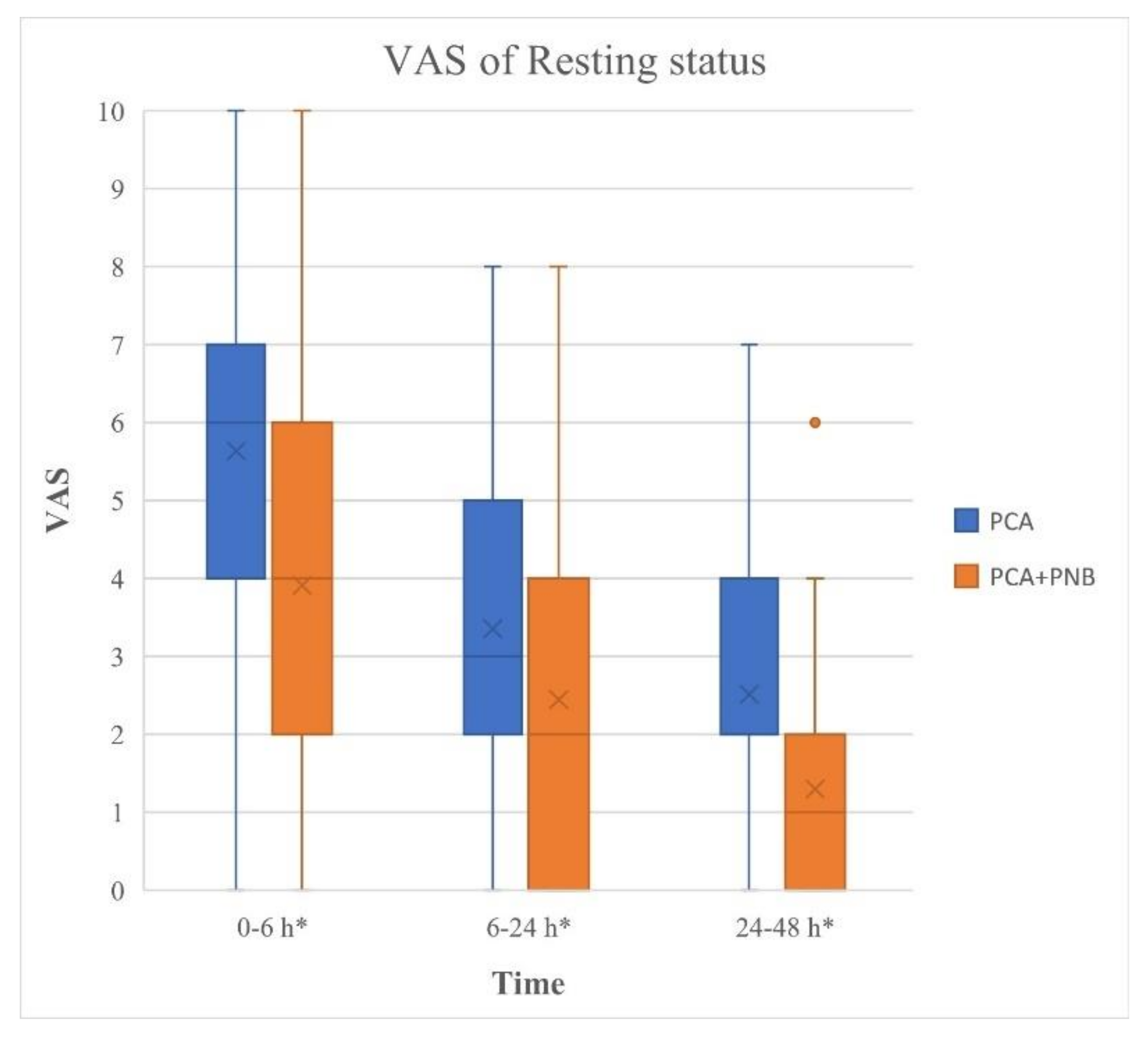
3.1. Primary Outcome
3.2. Secondary Outcome
3.3. Subgroup Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Shon, W.Y.; Park, B.Y.; Rajsankar, R.N.; Park, P.S.; Im, J.T.; Yun, H.H. Total Hip Arthroplasty: Past, Present, and Future. What Has Been Achieved? Hip Pelvis. 2019, 31, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Kurdi, O.; Tauviqirrahman, M.; Winarni, T.I.; Jamari, J. Tresca Stress Study of CoCrMo-on-CoCrMo Bearings Based on Body Mass Index Using 2D Computational Model. J. Tribol. 2022, 33, 31–38. [Google Scholar]
- Petis, S.M.; Howard, J.L.; Lanting, B.A.; Marsh, J.D.; Vasarhelyi, E.M. In-Hospital Cost Analysis of Total Hip Arthroplasty: Does Surgical Approach Matter? J. Arthroplast. 2016, 31, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Singelyn, F.J.; Deyaert, M.; Joris, D.; Pendeville, E.; Gouverneur, J.M. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth. Analg. 1998, 87, 88–92. [Google Scholar] [CrossRef]
- Choi, J.B.; Shim, Y.H.; Lee, Y.W.; Lee, J.S.; Choi, J.R.; Chang, C.H. Incidence and risk factors of postoperative nausea and vomiting in patients with fentanyl-based intravenous patient-controlled analgesia and single antiemetic prophylaxis. Yonsei Med. J. 2014, 55, 1430–1435. [Google Scholar] [CrossRef]
- Huh, J.W.; Park, M.J.; Lee, W.M.; Lee, D.H. Effectiveness of Ultrasound-guided Single-injection Triple Nerve Block before Cementless Bipolar Hip Hemiarthroplasty in Femoral Neck Fractures. Hip Pelvis. 2020, 32, 142–147. [Google Scholar] [CrossRef]
- Axelby, E.; Kurmis, A.P. Gabapentoids in knee replacement surgery: Contemporary, multi-modal, peri-operative analgesia. J. Orthop. 2019, 17, 150–154. [Google Scholar] [CrossRef]
- Kehlet, H. History and future challenges in fast-track hip and knee arthroplasty. Orthopade 2020, 49, 290–292. [Google Scholar] [CrossRef]
- Kehlet, H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br. J. Anaesth. 1997, 78, 606–617. [Google Scholar] [CrossRef]
- Li, K.; Liu, Y.W.; Feng, J.H.; Zhang, W. Clinical Study of Enhanced Recovery after Surgery in Peri-operative Management of Total Hip Arthroplasty. Sichuan Da Xue Xue Bao Yi Xue Ban 2019, 50, 604–608. [Google Scholar]
- Spruce, L. Enhanced Recovery After Surgery for Patients Undergoing Total Hip or Total Knee Arthroplasty. AORN J. 2020, 111, 550–557. [Google Scholar] [CrossRef]
- Horlocker, T.T.; Kopp, S.L.; Pagnano, M.W.; Hebl, J.R. Analgesia for total hip and knee arthroplasty: A multimodal pathway featuring peripheral nerve block. J. Am. Acad. Orthop. Surg. 2006, 14, 126–135. [Google Scholar] [CrossRef]
- Liu, S.S.; Bae, J.J.; Bieltz, M.; Wukovits, B.; Ma, Y. A prospective survey of patient-controlled epidural analgesia with bupivacaine and clonidine after total hip replacement: A pre- and postchange comparison with bupivacaine and hydromorphone in 1000 patients. Anesth Analg. 2011, 113, 1213–1217. [Google Scholar] [CrossRef]
- Sun, C.; Zhang, X.; Song, F.; Zhao, Z.; Du, R.; Wu, S.; Ma, Q.; Cai, X. Is continuous catheter adductor canal block better than single-shot canal adductor canal block in primary total knee arthroplasty?: A GRADE analysis of the evidence through a systematic review and meta-analysis. Medicine 2020, 99, e20320. [Google Scholar] [CrossRef]
- Kacmaz, M.; Turhan, Z.Y. The Effect of Femoral Nerve Block and Adductor Canal Block Methods on Patient Satisfaction in Unilateral Knee Arthroplasty: Randomized Non-Inferiority Trial. Geriatr. Orthop. Surg. Rehabil. 2021, 12, 2151459321996632. [Google Scholar] [CrossRef]
- Halawi, M.J.; Grant, S.A.; Bolognesi, M.P. Multimodal Analgesia for Total Joint Arthroplasty. Orthopedics 2015, 38, e616–e625. [Google Scholar] [CrossRef]
- Remily, E.A.; Hochstein, S.R.; Wilkie, W.A.; Mohamed, N.S.; Thompson, J.V.; Kluk, M.W.; Nace, J.; Delanois, R.E. The pericapsular nerve group block: A step towards outpatient total hip arthroplasty? Hip Int. 2022, 32, 318–325. [Google Scholar] [CrossRef]
- Wang, X.; Sun, Y.; Wang, L.; Hao, X. Femoral nerve block versus fascia iliaca block for pain control in total knee and hip arthroplasty: A meta-analysis from randomized controlled trials. Medicine 2017, 96, e7382. [Google Scholar] [CrossRef]
- Singh, S. Total hip arthroplasty under continuous pericapsular nerve group block (cPENG) in a high risk patient. J. Clin. Anesth. 2021, 68, 110096. [Google Scholar] [CrossRef]
- Li, J.; Dai, F.; Ona Ayala, K.E.; Zhou, B.; Schonberger, R.B.; Sharma, A. Transmuscular Quadratus Lumborum and Lateral Femoral Cutaneous Nerve Block in Total Hip Arthroplasty. Clin. J. Pain. 2021, 37, 366–371. [Google Scholar] [CrossRef]
- Harold, R.E.; Butler, B.A.; Delagrammaticas, D.; Sullivan, R.; Stover, M.; Manning, D.W. Patient-Reported Outcomes Measurement Information System Correlates with Modified Harris Hip Score in Total Hip Arthroplasty. Orthopedics 2021, 44, e19–e25. [Google Scholar] [CrossRef]
- Rahman, W.A.; Greidanus, N.V.; Siegmeth, A.; Masri, B.A.; Duncan, C.P.; Garbuz, D.S. Patients report improvement in quality of life and satisfaction after hip resurfacing arthroplasty. Clin. Orthop. Relat. Res. 2013, 471, 444–453. [Google Scholar] [CrossRef][Green Version]
- Nielsen, S.; Degenhardt, L.; Hoban, B.; Gisev, N. A synthesis of oral morphine equivalents (OME) for opioid utilisation studies. Pharmacoepidemiol. Drug Saf. 2016, 25, 733–737. [Google Scholar]
- Auinger, D.; Sandner-Kiesling, A.; Striessnig, A.; Lindenmann, J.; Smolle, J.; Friedl, H.; Smolle-Jüttner, F.-M. Is There an Impact of Sex on Acute Postthoracotomy Pain? A Retrospective Analysis. Ann. Thorac. Surg. 2020, 109, 1104–1111. [Google Scholar] [CrossRef]
- Choi, Y.S.; Park, K.K.; Lee, B.; Nam, W.S.; Kim, D.H. Pericapsular Nerve Group (PENG) Block versus Supra-Inguinal Fascia Iliaca Compartment Block for Total Hip Arthroplasty: A Randomized Clinical Trial. J. Pers. Med. 2022, 12, 408. [Google Scholar] [CrossRef]
- Hebl, J.R.; Dilger, J.A.; Byer, D.E.; Kopp, S.L.; Stevens, S.R.; Pagnano, M.W.; Hanssen, A.D.; Horlocker, T.T. A pre-emptive multimodal pathway featuring peripheral nerve block improves perioperative outcomes after major orthopedic surgery. Reg. Anesth. Pain. Med. 2008, 33, 510–517. [Google Scholar] [CrossRef]
- Indelli, P.F.; Grant, S.A.; Nielsen, K.; Vail, T.P. Regional anesthesia in hip surgery. Clin. Orthop. Relat. Res. 2005, 441, 250–255. [Google Scholar] [CrossRef]
- Gaffney, C.J.; Pelt, C.E.; Gililland, J.M.; Peters, C.L. Perioperative Pain Management in Hip and Knee Arthroplasty. Orthop. Clin. N. Am. 2017, 48, 407–419. [Google Scholar] [CrossRef]
- Fowler, S.J.; Christelis, N. High volume local infiltration analgesia compared to peripheral nerve block for hip and knee arthroplasty-what is the evidence? Anaesth. Intensive Care 2013, 41, 458–462. [Google Scholar] [CrossRef]
- Rashiq, S.; Vandermeer, B.; Abou-Setta, A.M.; Beaupre, L.A.; Jones, C.A.; Dryden, D.M. Efficacy of supplemental peripheral nerve blockade for hip fracture surgery: Multiple treatment comparison. Can. J. Anaesth. 2013, 60, 230–243. [Google Scholar] [CrossRef]
- Lin, D.Y.; Morrison, C.; Brown, B.; Saies, A.A.; Pawar, R.; Vermeulen, M.; Anderson, S.R.; Lee, T.S.; Doornberg, J.; Kroon, H.M.; et al. Pericapsular nerve group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: A single-center double-blinded randomized comparative trial. Reg. Anesth. Pain Med. 2021, 46, 398–403. [Google Scholar] [CrossRef] [PubMed]

| Total Hip Arthroplasty | |||
|---|---|---|---|
| PCA Group (n = 136) | PCA + PNB Group (n = 136) | p-Value | |
| Age (years) | 51.7 ± 11.4 | 59.1 ± 13.0 | 0.000 * |
| Sex | |||
| Male No. (%) | 49 (36.0) | 59 (43.4) | |
| Female No. (%) | 87 (64.0) | 77 (56.6) | |
| BMI | 24.2 ± 3.4 | 25.0 ± 3.8 | 0.043 * |
| ASA (%) | 0.199 | ||
| 1 | 21 (15.4) | 8 (6.0) | |
| 2 | 64 (47.1) | 73 (53.7) | |
| 3 | 49 (36.0) | 54 (39.6) | |
| 4 | 2 (1.5) | 1 (0.7) | |
| PNB method | |||
| FNB | 66 | ||
| FICB | 36 | ||
| PENG | 29 | ||
| Others | 5 | ||
| PCA | |||
| IV PCA | 136 | NA | |
| IV PCA + PNB | NA | 136 | |
| Total Hip Arthroplasty | |||
|---|---|---|---|
| PCA Group (n = 136) | PCA + PNB Group (n = 136) | p-Value | |
| WOMAC | |||
| Pre-operative | 50.2 ± 21.1 | 51.7 ± 20.1 | 0.562 |
| Post-operative 3 months | 14.0 ± 12.7 | 25.0 ± 21.3 | 0.009 * |
| HHS | |||
| Pre-operative | 50.7 ± 19.5 | 48.1 ± 20.2 | 0.278 |
| Post-operative 3 months | 71.7 ± 34.1 | 76.4 ± 18.0 | 0.210 |
| Rescue Medication | |||
|---|---|---|---|
| PCA Group (n = 136) | PCA + PNB Group (n = 136) | p-Value | |
| Total count | 2.05 ± 2.3 | 1.79 ± 2.4 | 0.091 |
| Morphine equivalent (mg) | 23.4 | 21.1 | 0.069 |
| FNB (n = 66) | FICB (n = 36) | PENG (n = 29) | p-Value | |
|---|---|---|---|---|
| 0–6 h Rest | 5 (1, 6) | 5 (2, 6) | 3 (2, 5) | 0.818 |
| 0–6 h Activity | 7 (5.5, 8) | 7 (6, 8) | 7 (6, 8) | 0.684 |
| 6–24 h Rest | 3 (1, 4) | 3 (0, 5) | 2 (0, 3) | 0.161 |
| 6–24 h Activity | 5 (5, 6.5) | 6 (5.5, 7) | 5 (4, 6) | 0.052 |
| 24–48 h Rest | 2 (0, 2) | 0.5 (0, 2) | 0.5 (0, 1.3) | 0.179 |
| 24–48 h Activity | 4 (2, 5) | 5 (4, 6) | 5 (3, 5) | 0.014 * |
| PNB Subgroup | p-Value | p-Value (Adjusted) |
|---|---|---|
| FNB-PENG | 0.338 | 1.000 |
| FNB-FICB | 0.004 * | 0.021 * |
| PENG-FICB | 0.129 | 0.775 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, H.J.; Park, K.K.; Park, J.Y.; Lee, B.; Choi, Y.S.; Kwon, H.M. Peripheral Nerve Block for Pain Management after Total Hip Arthroplasty: A Retrospective Study with Propensity Score Matching. J. Clin. Med. 2022, 11, 5456. https://doi.org/10.3390/jcm11185456
Park HJ, Park KK, Park JY, Lee B, Choi YS, Kwon HM. Peripheral Nerve Block for Pain Management after Total Hip Arthroplasty: A Retrospective Study with Propensity Score Matching. Journal of Clinical Medicine. 2022; 11(18):5456. https://doi.org/10.3390/jcm11185456
Chicago/Turabian StylePark, Heon Jung, Kwan Kyu Park, Jun Young Park, Bora Lee, Yong Seon Choi, and Hyuck Min Kwon. 2022. "Peripheral Nerve Block for Pain Management after Total Hip Arthroplasty: A Retrospective Study with Propensity Score Matching" Journal of Clinical Medicine 11, no. 18: 5456. https://doi.org/10.3390/jcm11185456
APA StylePark, H. J., Park, K. K., Park, J. Y., Lee, B., Choi, Y. S., & Kwon, H. M. (2022). Peripheral Nerve Block for Pain Management after Total Hip Arthroplasty: A Retrospective Study with Propensity Score Matching. Journal of Clinical Medicine, 11(18), 5456. https://doi.org/10.3390/jcm11185456






