Structural Features of Patients with Drusen-like Deposits and Systemic Lupus Erythematosus
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Patient Inclusion and Exclusion Criteria
2.3. Data Collection
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fortuna, G.; Brennan, M.T. Systemic Lupus Erythematosus. Epidemiology, Pathophysiology, Manifestations, and Management. Dent. Clin. N. Am. 2013, 57, 631–655. [Google Scholar] [CrossRef]
- Leffler, J.; Bengtsson, A.A.; Blom, A.M. The Complement System in Systemic Lupus Erythematosus: An Update. Ann. Rheum. Dis. 2014, 73, 1601–1606. [Google Scholar] [CrossRef]
- Invernizzi, A.; dell’Arti, L.; Leone, G.; Galimberti, D.; Garoli, E.; Moroni, G.; Santaniello, A.; Agarwal, A.; Viola, F. Drusen-like Deposits in Young Adults Diagnosed With Systemic Lupus Erythematosus. Am. J. Ophthalmol. 2017, 175, 68–76. [Google Scholar] [CrossRef][Green Version]
- Stafford-Brady, F.J.; Urowitz, M.B.; Gladman, D.D.; Easterbrook, M. Lupus Retinopathy. Patterns, Associations, and Prognosis. Arthritis Rheum. 1988, 31, 1105–1110. [Google Scholar] [CrossRef] [PubMed]
- Kemeny-Beke, A.; Szodoray, P. Ocular Manifestations of Rheumatic Diseases. Int. Ophthalmol. 2020, 40, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Altinkaynak, H.; Duru, N.; Uysal, B.S.; Erten, Ş.; Kürkcüoğlu, P.Z.; Yüksel, N.; Duru, Z.; Çağıl, N. Choroidal Thickness in Patients with Systemic Lupus Erythematosus Analyzed by Spectral-Domain Optical Coherence Tomography. Ocul. Immunol. Inflamm. 2016, 24, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Baglio, V.; Gharbiya, M.; Balacco-Gabrieli, C.; Mascaro, T.; Gangemi, C.; di Franco, M.; Pistolesi, V.; Morabito, S.; Pecci, G.; Pierucci, A. Choroidopathy in Patients with Systemic Lupus Erythematosus with or without Nephropathy. J. Nephrol. 2011, 24, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, Q.D.; Uy, H.S.; Akpek, E.K.; Harper, S.L.; Zacks, D.N.; Foster, C.S. Choroidopathy of Systemic Lupus Erythematosus. Lupus 2000, 9, 288–298. [Google Scholar] [CrossRef]
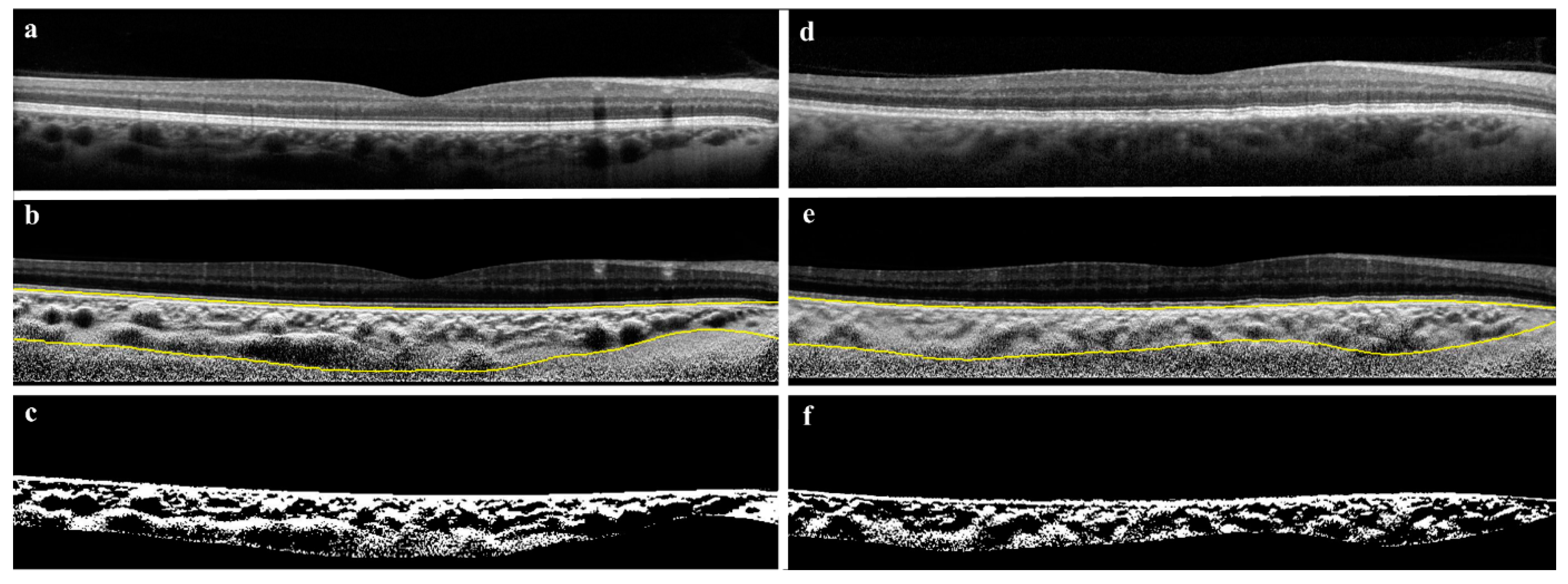
- Iovino, C.; Pellegrini, M.; Bernabei, F.; Borrelli, E.; Sacconi, R.; Govetto, A.; Vagge, A.; Di Zazzo, A.; Forlini, M.; Finocchio, L.; et al. Choroidal Vascularity Index: An in-Depth Analysis of This Novel Optical Coherence Tomography Parameter. J. Clin. Med. 2020, 9, 595. [Google Scholar] [CrossRef]
- Leys, A.; Vanrenterghem, Y.; Van Damme, B.; Snyers, B.; Pirson, Y.; Leys, M. Fundus Changes in Membranoproliferative Glomerulonephritis Type II. A Fluorescein Angiographic Study of 23 Patients. Graefe’s Arch. Clin. Exp. Ophthalmol. = Albr. von Graefes Arch. fur Klin. und Exp. Ophthalmol. 1991, 229, 406–410. [Google Scholar] [CrossRef]
- Leys, A.; Michielsen, B.; Leys, M.; Vanrenterghem, Y.; Missotten, L.; Van Damme, B. Subretinal Neovascular Membranes Associated with Chronic Membranoproliferative Glomerulonephritis Type II. Graefe’s Arch. Clin. Exp. Ophthalmol. = Albr. von Graefes Arch. fur Klin. und Exp. Ophthalmol. 1990, 228, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Goud, A.; Singh, S.R.; Sahoo, N.K.; Rasheed, M.A.; Vupparaboina, K.K.; Ankireddy, S.; Lupidi, M.; Chhablani, J. New Insights on Choroidal Vascularity: A Comprehensive Topographic Approach. Investig. Ophthalmol. Vis. Sci. 2019, 60, 3563–3569. [Google Scholar] [CrossRef] [PubMed]
- Vupparaboina, K.K.; Dansingani, K.K.; Goud, A.; Rasheed, M.A.; Jawed, F.; Jana, S.; Richhariya, A.; Freund, K.B.; Chhablani, J. Quantitative Shadow Compensated Optical Coherence Tomography of Choroidal Vasculature. Sci. Rep. 2018, 8, 6461. [Google Scholar] [CrossRef] [PubMed]
- Al-Sheikh, M.; Falavarjani, K.G.; Akil, H.; Sadda, S.R. Impact of Image Quality on OCT Angiography Based Quantitative Measurements. Int. J. Retin. Vitr. 2017, 3, 4–9. [Google Scholar] [CrossRef]
- Ağın, A.; Kadayıfçılar, S.; Sönmez, H.E.; Baytaroğlu, A.; Demir, S.; Sağ, E.; Özen, S.; Eldem, B. Evaluation of Choroidal Thickness, Choroidal Vascularity Index and Peripapillary Retinal Nerve Fiber Layer in Patients with Juvenile Systemic Lupus Erythematosus. Lupus 2019, 28, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, A.; Yokoyama, T.; Kodera, S.; Zhang, D.; Hirose, S.; Shirai, T.; Kanai, A. Ocular Fundus Lesions in Systemic Lupus Erythematosus Model Mice. Jpn. J. Ophthalmol. 1998, 42, 345–351. [Google Scholar] [CrossRef]
- Dias-Santos, A.; Tavares Ferreira, J.; Pinheiro, S.; Cunha, J.P.; Alves, M.; Papoila, A.L.; Moraes-Fontes, M.F.; Proença, R. Neurodegeneration in Systemic Lupus Erythematosus: Layer by Layer Retinal Study Using Optical Coherence Tomography. Int. J. Retin. Vitr. 2020, 6, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Dias-Santos, A.; Tavares Ferreira, J.; Pinheiro, S.; Paulo Cunha, J.; Alves, M.; Papoila, A.; Moraes-Fontes, M.F.; Proença, R. Choroidal Thickness Changes in Systemic Lupus Erythematosus Patients. Clin. Ophthalmol. 2019, 13, 1567–1578. [Google Scholar] [CrossRef]
- Işık, M.U.; Akmaz, B.; Akay, F.; Güven, Y.Z.; Solmaz, D.; Gercik, Ö.; Kabadayı, G.; Kurut, İ.; Akar, S. Evaluation of Subclinical Retinopathy and Angiopathy with OCT and OCTA in Patients with Systemic Lupus Erythematosus. Int. Ophthalmol. 2021, 41, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.Y.; Utset, T.O.; Bernard, J.T. Retinal Nerve Fiber Layer and Macular Thinning in Systemic Lupus Erythematosus: An Optical Coherence Tomography Study Comparing SLE and Neuropsychiatric SLE. Lupus 2015, 24, 1169–1176. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.W.; Pfeiffer, R.L.; Ferrell, W.D.; Watt, C.B.; Marmor, M.; Marc, R.E. Retinal Remodeling in Human Retinitis Pigmentosa. Exp. Eye Res. 2016, 150, 149–165. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Bishop, R.J.; Forooghian, F.; Cho, Y.; Fariss, R.N.; Chan, C.-C. Autoimmune Retinopathy in Systemic Lupus Erythematosus: Histopathologic Features. Open Ophthalmol. J. 2009, 3, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.N.; Mahroo, O.A.; Khan, R.S.; Mohamed, M.D.; McKibbin, M.; Bird, A.; Michaelides, M.; Tufail, A.; Moore, A.T. Differentiating Drusen: Drusen and Drusen-like Appearances Associated with Ageing, Age-Related Macular Degeneration, Inherited Eye Disease and Other Pathological Processes. Prog. Retin. Eye Res. 2016, 53, 70–106. [Google Scholar] [CrossRef] [PubMed]
- Cheung, L.K.; Eaton, A. Age-Related Macular Degeneration. Pharmacotherapy 2013, 33, 838–855. [Google Scholar] [CrossRef]
- Lally, D.R.; Baumal, C. Subretinal Drusenoid Deposits Associated with Complement-Mediated IgA Nephropathy. JAMA Ophthalmol. 2014, 132, 775–777. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Duvall-Young, J.; MacDonald, M.K.; McKechnie, N.M. Fundus Changes in (Type II) Mesangiocapillary Glomerulonephritis Simulating Drusen: A Histopathological Report. Br. J. Ophthalmol. 1989, 73, 297–302. [Google Scholar] [CrossRef]
- Ishizaki, J.; Saito, K.; Nawata, M.; Mizuno, Y.; Tokunaga, M.; Sawamukai, N.; Tamura, M.; Hirata, S.; Yamaoka, K.; Hasegawa, H.; et al. Low Complements and High Titre of Anti-Sm Antibody as Predictors of Histopathologically Proven Silent Lupus Nephritis without Abnormal Urinalysis in Patients with Systemic Lupus Erythematosus. Rheumatology 2015, 54, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Bao, L.; Zhou, R.; Wu, Y.; Wang, J.; Shen, M.; Lu, F.; Wang, H.; Chen, Q. Unique Changes in the Retinal Microvasculature Reveal Subclinical Retinal Impairment in Patients with Systemic Lupus Erythematosus. Microvasc. Res. 2020, 129, 103957. [Google Scholar] [CrossRef]
- Arfeen, S.A.; Bahgat, N.; Adel, N.; Eissa, M.; Khafagy, M.M. Assessment of Superficial and Deep Retinal Vessel Density in Systemic Lupus Erythematosus Patients Using Optical Coherence Tomography Angiography. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
- Ermurat, S.; Koyuncu, K. Evaluation of Subclinical Retinal Microvascular Changes in Systemic Lupus Erythematosus Patients Using Optical Coherence Tomography Angiography and Its Relationship with Disease Activity. Lupus 2022, 31, 541–554. [Google Scholar] [CrossRef] [PubMed]
- Pichi, F.; Woodstock, E.; Hay, S.; Neri, P. Optical Coherence Tomography Angiography Findings in Systemic Lupus Erythematosus Patients with No Ocular Disease. Int. Ophthalmol. 2020, 40, 2111–2118. [Google Scholar] [CrossRef] [PubMed]
- Conigliaro, P.; Cesareo, M.; Chimenti, M.S.; Triggianese, P.; Canofari, C.; Aloe, G.; Nucci, C.; Perricone, R. Evaluation of Retinal Microvascular Density in Patients Affected by Systemic Lupus Erythematosus: An Optical Coherence Tomography Angiography Study. Ann. Rheum. Dis. 2019, 78, 287–288. [Google Scholar] [CrossRef] [PubMed]


| Eyes with DLD (n = 16) | Eyes without DLD (n = 16) | Healthy Control Group (n = 51) | |
|---|---|---|---|
| Age, years, mean (SD) | |||
| First Exam | 41.2 (12.3) | 40.6 (12.3) | 57.7 (18.3) |
| Sex, n (%) | |||
| Male | 4 (33.3) | 5 (31.3) | 24 (47.1) |
| Female | 12 (66.7) | 11 (68.8) | 27 (52.9) |
| Ethnicity, n (%) | |||
| Caucasian | 13 (81.3) | 10 (62.5) | |
| Asian | 3 (18.8) | 5 (31.3) | |
| Other | 0 (0.0) | 1 (6.3) | |
| Smoking Status, n (%) | |||
| Yes | 5 (38.5) | 8 (50.0) | |
| No | 4 (30.8) | 5 (31.3) | |
| Quit | 1 (7.7) | 1 (6.3) | |
| Unknown | 3 (23.1) | 2 (12.6) |
| Eyes with DLD (n = 16) | Eyes without DLD (n = 16) | p-Value | |
|---|---|---|---|
| HCQ Treatment | |||
| Daily Dose, mg (range) | 200 (200–200) | 200 (200–400) | 0.260 |
| Cumulative Dose, g (range) | 567.6 (450.5–899.8) | 486.6 (322.4–1026.5) | 0.429 |
| Dosage, mg/kg (range) | 3.8 (2.8–5.1) | 4.3 (2.7–5.3) | 0.612 |
| Treatment Duration, years (range) | 7.4 (4.7–12.3) | 5.3 (2.5–8.3) | 0.188 |
| Comorbidity, n (%) | |||
| Cardiovascular Disease | 10 (62.5) | 3 (18.8) | 0.036 |
| Renal Involvement | 3 (18.8) | 2 (12.5) | 0.678 |
| GFR 1, mean (SD) | 88.1 (33.7) | 101.4 (18.0) | 0.321 |
| GFR 2, mean (SD) | 90.6 (32.7) | 96.4 (31.4) | 0.856 |
| Eyes with DLD (n = 16) | Eyes without DLD (n = 16) | Healthy Control Group (n = 51) | ||
|---|---|---|---|---|
| Bright Region Volume WSR, mm3, mean (range) | OD | 0.62 (0.54–0.76) | 0.49 (0.35–1.06) | 0.77 (0.48–0.90) |
| OS | 0.57 (0.46–0.72) | 0.49 (0.39–1.18) | 0.57 (0.49–0.81) | |
| Dark Region Volume, mm3, mean (range) | OD | 0.26 (0.24–0.32) | 0.22 (0.15–0.42) | 0.31 (0.21–0.36) |
| OS | 0.25 (0.21–0.31) | 0.20 (0.16–0.50) | 0.24 (0.19–0.32) | |
| CVI WSR Proposed, mean (range) | OD | 0.35 (0.28–0.43) | 0.26 (0.20–0.63) | 0.44 (0.29–0.52) |
| OS | 0.32 (0.25–0.40) | 0.28 (0.21–0.67) | 0.34 (0.26–0.48) | |
| Bright Region Volume WSR, mm3, mean (range) | OD | 0.56 (0.54–0.59) | 0.57 (0.52–0.58) | 0.58 (0.57–0.59) |
| OS | 0.56 (0.54–0.58) | 0.56 (0.55–0.58) | 0.58 (0.57–0.60) | |
| Eyes with DLD | Eyes without DLD | ||||
|---|---|---|---|---|---|
| OD | OS | OD | OS | ||
| Retina, µm | Center Min ± SD | 222.6 ± 20.2 | 224.3 ± 14.0 | 205.1 ± 59.4 | 217.3 ± 25.4 |
| Center Max ± SD | 318.4 ± 24.9 | 321.8 ± 17.7 | 291.2 ± 82.5 | 313.8 ± 27.1 | |
| Ganglion Cell Layer, µm | Center Min ± SD | 1.4 ± 1.5 | 0.8 ± 1.5 | 1.1 ± 1.2 | 1.3 ± 1.2 |
| Center Max ± SD | 36.9 ± 9.2 | 37.9 ± 11.0 | 28.6 ± 12.3 | 32.5 ± 10.5 | |
| Outer Nuclear Layer, µm | Center Min ± SD | 55.3 ± 14.9 | 50.7 ± 13.9 | 51.6 ± 19.3 | 54.5 ± 17.1 |
| Center Max ± SD | 117.8 ± 12.4 | 117.1 ± 14.7 | 102.4 ± 32.3 | 108.5 ± 17.1 | |
| Retinal Pigment Epithelium, µm | Center Min ± SD | 11.4 ± 1.9 | 11.4 ± 2.6 | 11.6 ± 3.5 | 12.5 ± 2.2 |
| Center Max ± SD | 28.1 ± 6.9 | 36.1 ± 23.1 | 23.6 ± 6.7 | 25.6 ± 4.2 | |
| Outer Retinal Layers, µm | Center Min ± SD | 81.0 ± 5.5 | 81.5 ± 5.3 | 79.8 ± 21.9 | 84.4 ± 5.7 |
| Center Max ± SD | 98.4 ± 7.8 | 104.6 ± 18.4 | 95.9 ± 26.5 | 101.7 ± 8.6 | |
| Photoreceptor Cell Layer, µm | Center Min ± SD | 69.7 ± 5.8 | 69.5 ± 4.5 | 72.7 ± 5.5 | 71.9 ± 5.3 |
| Center Max ± SD | 68.8 ± 7.7 | 66.5 ± 10.5 | 77.1 ± 7.3 | 76.1 ± 6.3 | |
| Eyes with DLD | Eyes without DLD | p-Value | ||
|---|---|---|---|---|
| 3 × 3 Mean Inner Ring, mm/mm2, mean (SD) | Vessel Density Superficial | 16.4 (2.4) | 17.6 (1.1) | 0.248 |
| Vessel Density Deep | 12.7 (3.3) | 13.1 (1.6) | 0.847 | |
| Perfusion Density Superficial | 0.37 (0.05) | 0.39 (0.02) | 0.501 | |
| Perfusion Density Deep | 0.27 (0.07) | 0.28 (0.04) | 0.773 | |
| Choriocapillaris Area | 1.6 (0.0) | 1.6 (0.0) | 1.000 | |
| Choriocapillaris % Area | 18.1 (5.1) | 18.1 (4.3) | 0.700 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kukan, M.; Driban, M.; Vupparaboina, K.K.; Schwarz, S.; Kitay, A.M.; Rasheed, M.A.; Busch, C.; Barthelmes, D.; Chhablani, J.; Al-Sheikh, M. Structural Features of Patients with Drusen-like Deposits and Systemic Lupus Erythematosus. J. Clin. Med. 2022, 11, 6012. https://doi.org/10.3390/jcm11206012
Kukan M, Driban M, Vupparaboina KK, Schwarz S, Kitay AM, Rasheed MA, Busch C, Barthelmes D, Chhablani J, Al-Sheikh M. Structural Features of Patients with Drusen-like Deposits and Systemic Lupus Erythematosus. Journal of Clinical Medicine. 2022; 11(20):6012. https://doi.org/10.3390/jcm11206012
Chicago/Turabian StyleKukan, Marc, Matthew Driban, Kiran K. Vupparaboina, Swen Schwarz, Alice M. Kitay, Mohammed A. Rasheed, Catharina Busch, Daniel Barthelmes, Jay Chhablani, and Mayss Al-Sheikh. 2022. "Structural Features of Patients with Drusen-like Deposits and Systemic Lupus Erythematosus" Journal of Clinical Medicine 11, no. 20: 6012. https://doi.org/10.3390/jcm11206012
APA StyleKukan, M., Driban, M., Vupparaboina, K. K., Schwarz, S., Kitay, A. M., Rasheed, M. A., Busch, C., Barthelmes, D., Chhablani, J., & Al-Sheikh, M. (2022). Structural Features of Patients with Drusen-like Deposits and Systemic Lupus Erythematosus. Journal of Clinical Medicine, 11(20), 6012. https://doi.org/10.3390/jcm11206012







