Outcomes of Transcatheter Edge-to-Edge Repair in Degenerative vs. Functional Mitral Regurgitation
Abstract
1. Introduction
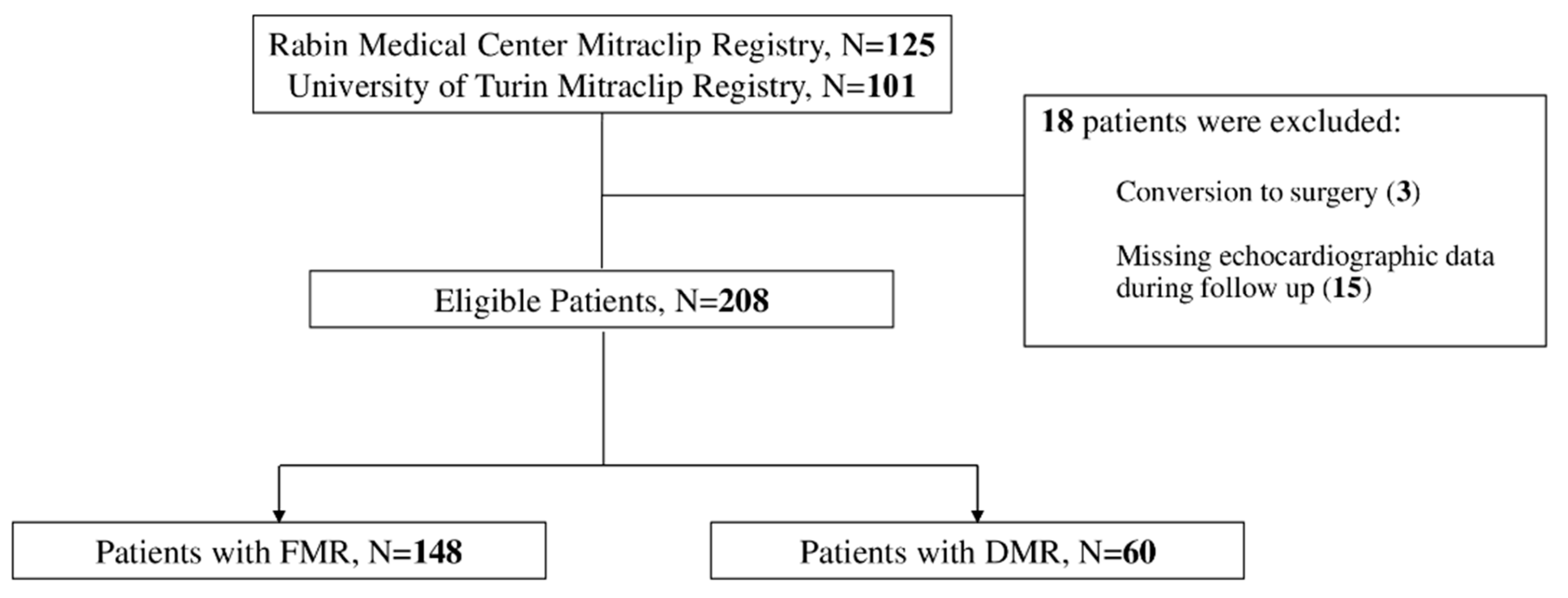
2. Methods
2.1. Patients and Data Collection
2.2. Endpoints
2.3. Statistical Analysis
3. Results
3.1. Patient and Echocardiographic Characteristics
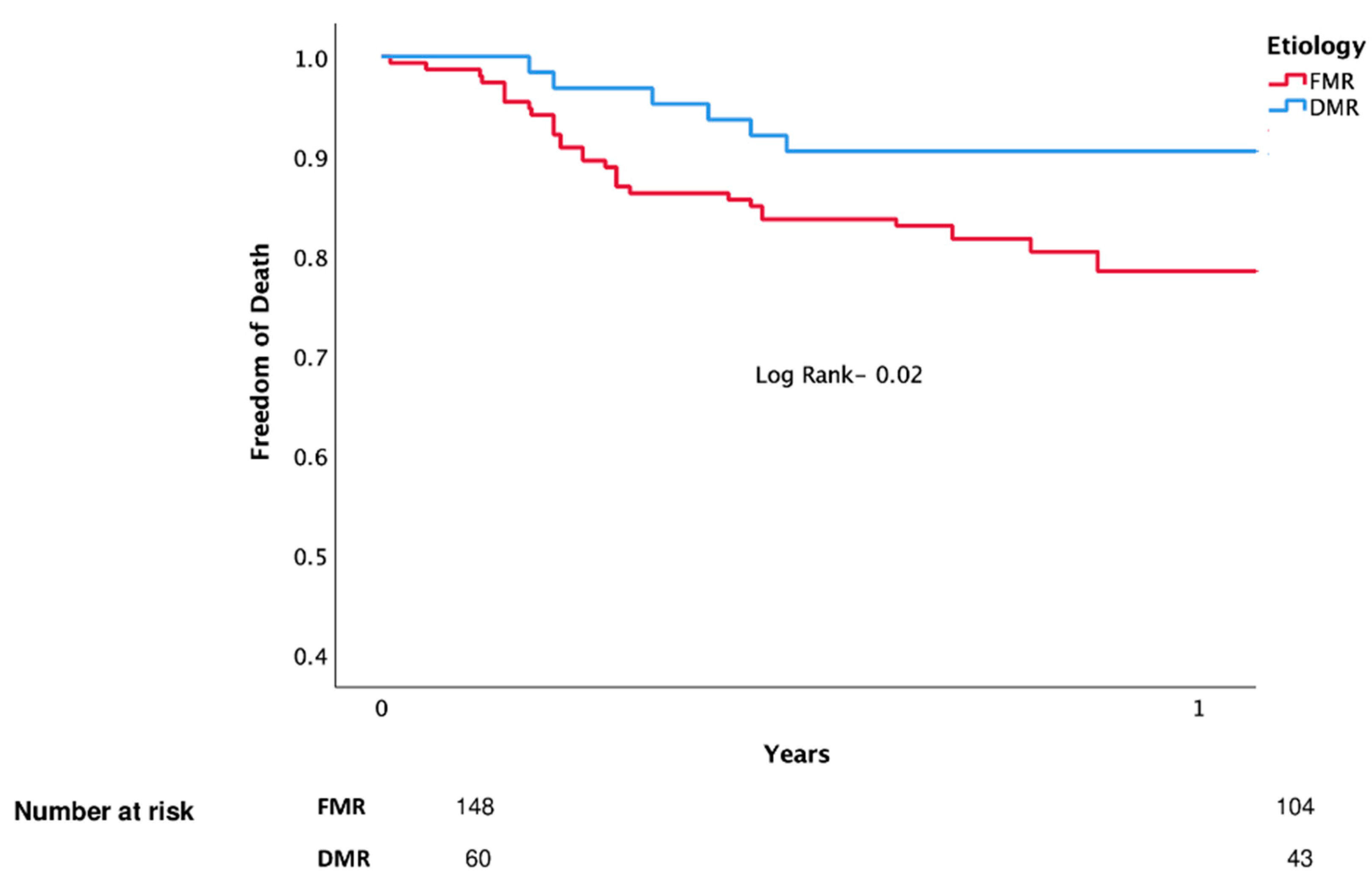
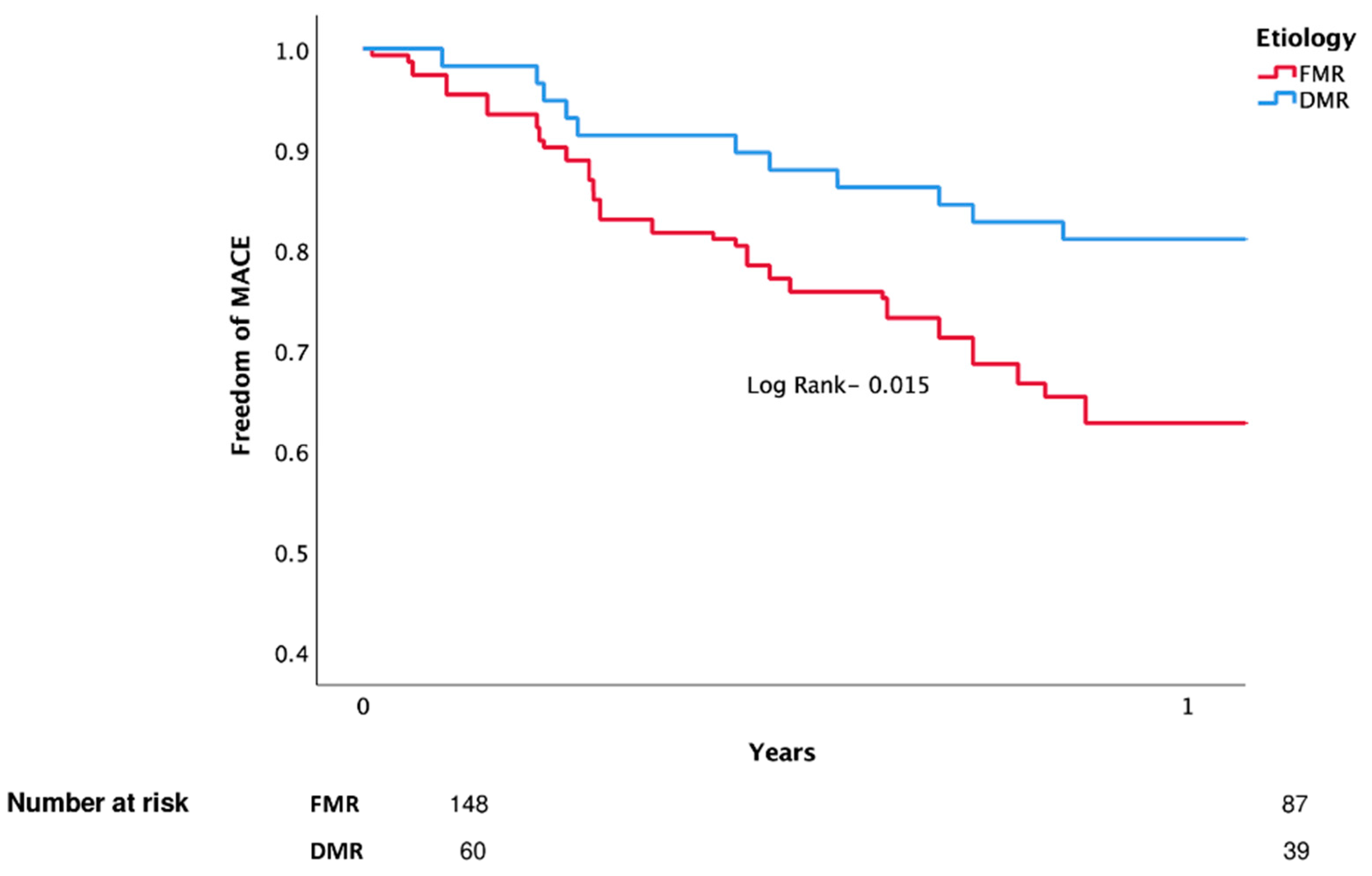
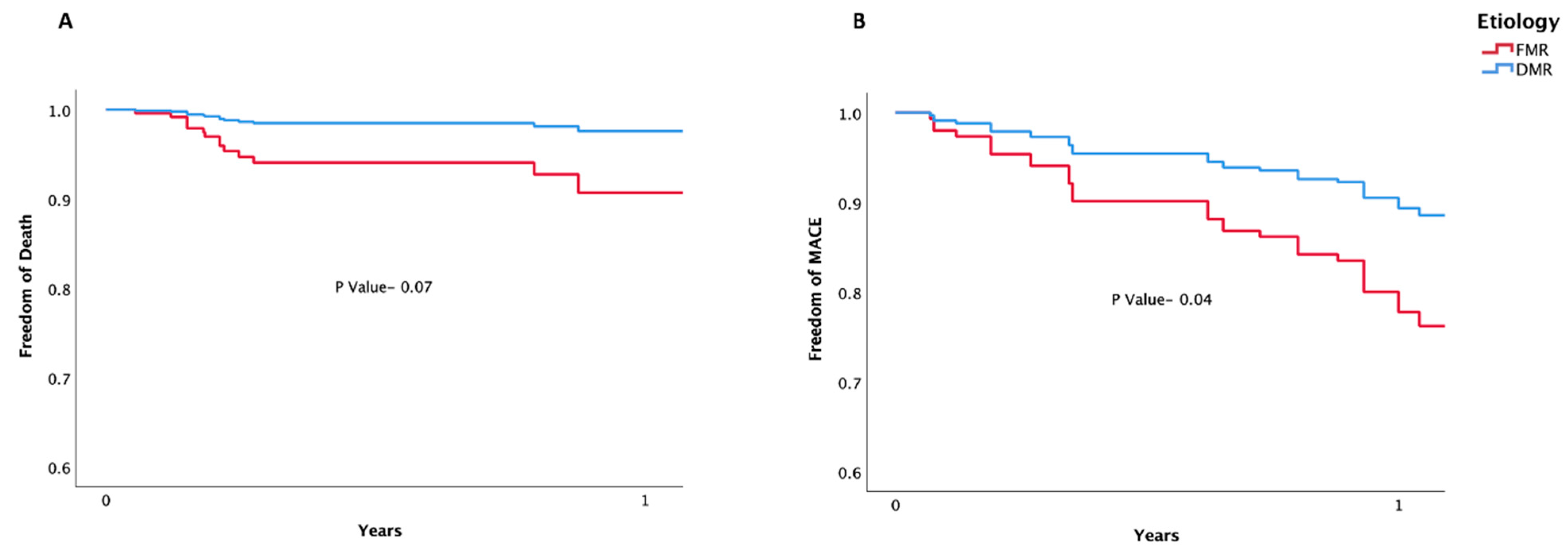
3.2. Clinical Outcomes
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of valvular heart diseases: A population-based study. Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef]
- Dziadzko, V.; Clavel, M.-A.; Dziadzko, M.; Medina-Inojosa, J.R.; Michelena, H.; Maalouf, J.; Nkomo, V.; Thapa, P.; Enriquez-Sarano, M. Outcome and undertreatment of mitral regurgitation: A community cohort study. Lancet 2018, 391, 960–969. [Google Scholar] [CrossRef]
- Zipes, D.P. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine, 12th ed.; Mitral Regurgitation, Chapter 76; Elsevier: Amsterdam, The Netherlands, 2022; pp. 1458–1467. [Google Scholar]
- Deferm, S.; Bertrand, P.B.; Verbrugge, F.H.; Verhaert, D.; Rega, F.; Thomas, J.D.; Vandervoort, P.M. Atrial Functional Mitral Regurgitation. J. Am. Coll. Cardiol. 2019, 73, 2465–2476. [Google Scholar] [CrossRef] [PubMed]
- Bonow, R.; Carabello, B.; de Leon, A.; Edmunds, L.H.; Fedderly, B.; Freed, M.; Gaasch, W.; McKay, C.; Nishimura, R.; O’Gara, P.; et al. ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease. J. Am. Coll. Cardiol. 2021, 77, e25–e197. [Google Scholar] [CrossRef]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2021, 43, ehab395. [Google Scholar] [CrossRef]
- Stone, G.W.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Mishell, J.M.; Whisenant, B.; Grayburn, P.A.; Rinaldi, M.; Kapadia, S.R.; et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N. Engl. J. Med. 2018, 379, 2307–2318. [Google Scholar] [CrossRef] [PubMed]
- Obadia, J.-F.; Messika-Zeitoun, D.; Leurent, G.; Iung, B.; Bonnet, G.; Piriou, N.; Lefèvre, T.; Piot, C.; Rouleau, F.; Carrié, D.; et al. Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation. N. Engl. J. Med. 2018, 379, 2297–2306. [Google Scholar] [CrossRef]
- Liu, X.-H.; Shi, J.-Y.; Feng, X.-J.; Feng, D.-C.; Wang, L.; Pang, H.-Y.; Xie, H.-Z.; Wang, F.-F.; Hsu, J.; Jia, F.-W.; et al. Short-term and 1-year outcomes after MitraClip therapy in functional versus degenerative mitral regurgitation patients: A systematic review and meta-analysis. J. Thorac. Dis. 2018, 10, 4156–4168. [Google Scholar] [CrossRef] [PubMed]
- Chiarito, M.; Pagnesi, M.; Martino, E.A.; Pighi, M.; Scotti, A.; Biondi-Zoccai, G.; Latib, A.; Landoni, G.; Di Mario, C.; Margonato, A.; et al. Outcome after percutaneous edge-to-edge mitral repair for functional and degenerative mitral regurgitation: A systematic review and meta-analysis. Heart 2018, 104, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Sugiura, A.; Kavsur, R.; Spieker, M.; Iliadis, C.; Goto, T.; Öztürk, C.; Weber, M.; Tabata, N.; Zimmer, S.; Sinning, J.-M.; et al. Recurrent Mitral Regurgitation After MitraClip: Predictive Factors, Morphology, and Clinical Implication. Circ. Cardiovasc. Interv. 2022, 15, e010895. [Google Scholar] [CrossRef]
- Hassan, A.; Eleid, M.F. Recurrent Mitral Regurgitation after MitraClip: Defining Success and Predicting Outcomes. Circ. Cardiovasc. Interv. 2022, 15, e011837. [Google Scholar] [CrossRef] [PubMed]
- Buzzatti, N.; De Bonis, M.; Denti, P.; Barili, F.; Schiavi, D.; Di Giannuario, G.; La Canna, G.; Alfieri, O. What is a “good” result after transcatheter mitral repair? Impact of 2+ residual mitral regurgitation. J. Thorac. Cardiovasc. Surg. 2016, 151, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Sorajja, P.; Vemulapalli, S.; Feldman, T.; Mack, M.; Holmes, D.R.; Stebbins, A.; Kar, S.; Thourani, V.; Ailawadi, G. Outcomes with Transcatheter Mitral Valve Repair in the United States. J. Am. Coll. Cardiol. 2017, 70, 2315–2327. [Google Scholar] [CrossRef] [PubMed]
- Kar, S.; Feldman, T.; Qasim, A.; Trento, A.; Kapadia, S.; Pedersen, W.; Lim, D.S.; Kipperman, R.; Smalling, R.W.; Bajwa, T.; et al. Five-year outcomes of transcatheter reduction of significant mitral regurgitation in high-surgical-risk patients. Heart 2019, 105, 1622–1628. [Google Scholar] [CrossRef] [PubMed]
- Raposeiras-Roubin, S.; Adamo, M.; Freixa, X.; Arzamendi, D.; Benito-González, T.; Montefusco, A.; Pascual, I.; Nombela-Franco, L.; Rodes-Cabau, J.; Shuvy, M.; et al. A Score to Assess Mortality After Percutaneous Mitral Valve Repair. J. Am. Coll. Cardiol. 2022, 79, 562–573. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.-H.; Makar, M.; Kar, S.; Chakravarty, T.; Oakley, L.; Sekhon, N.; Koseki, K.; Nakamura, M.; Hamilton, M.; Patel, J.K.; et al. Outcomes After Transcatheter Edge-to-Edge Mitral Valve Repair According to Mitral Regurgitation Etiology and Cardiac Remodeling. JACC Cardiovasc. Interv. 2022, 15, 1711–1722. [Google Scholar] [CrossRef]
- Feldman, T.; Foster, E.; Glower, D.D.; Kar, S.; Rinaldi, M.J.; Fail, P.S.; Smalling, R.W.; Siegel, R.; Rose, G.A.; Engeron, E.; et al. Percutaneous Repair or Surgery for Mitral Regurgitation. N. Engl. J. Med. 2011, 364, 1395–1406. [Google Scholar] [CrossRef] [PubMed]
- Mesana, T.G. MitraClip Real-World Data: What Is Missing and Looking into the Future. Cardiovasc. Revascularization Med. 2020, 21, 1063–1064. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Kubo, S.; Izumo, M.; Mizuno, S.; Shirai, S.; on behalf of the MitraClip Japan PMS Investigators. MitraClip Treatment of Moderate-to-Severe and Severe Mitral Regurgitation in High Surgical Risk Patients―Real-World 1-Year Outcomes from Japan. Circ. J. 2022, 86, 402–411. [Google Scholar] [CrossRef]
- Carrabba, N.; Migliorini, A.; Fumagalli, C.; Berteotti, M.; Matteo, V.; Cerillo, A.; Stefano, P.; Marchionni, N.; Valenti, R. MitraClip implantation in real-world: Clinical relevance of different patterns of left ventricular remodeling. Hell. J. Cardiol. 2022, 64, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Mack, M.J.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Mishell, J.M.; Whisenant, B.K.; Grayburn, P.A.; Rinaldi, M.J.; Kapadia, S.R.; et al. 3-Year Outcomes of Transcatheter Mitral Valve Repair in Patients with Heart Failure. J. Am. Coll. Cardiol. 2021, 77, 1029–1040. [Google Scholar] [CrossRef] [PubMed]
- Iung, B.; Armoiry, X.; Vahanian, A.; Boutitie, F.; Mewton, N.; Trochu, J.; Lefèvre, T.; Messika-Zeitoun, D.; Guerin, P.; Cormier, B.; et al. Percutaneous repair or medical treatment for secondary mitral regurgitation: Outcomes at 2 years. Eur. J. Heart Fail 2019, 21, 1619–1627. [Google Scholar] [CrossRef] [PubMed]
- Leurent, G.; Auffret, V.; Donal, E.; Corbineau, H.; Grinberg, D.; Bonnet, G.; Leroux, P.-Y.; Guérin, P.; Wautot, F.; Lefèvre, T.; et al. Delayed hospitalisation for heart failure after transcatheter repair or medical treatment for secondary mitral regurgitation: A landmark analysis of the MITRA-FR trial. EuroInterv. J. EuroPCR Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2022. [Google Scholar] [CrossRef]
- Pibarot, P.; Delgado, V.; Bax, J.J. MITRA-FR vs. COAPT: Lessons from two trials with diametrically opposed results. Eur. Heart J.-Cardiovasc. Imaging 2019, 20, 620–624. [Google Scholar] [CrossRef] [PubMed]
- De Backer, O.; Wong, I.; Taramasso, M.; Maisano, F.; Franzen, O.; Søndergaard, L. Transcatheter mitral valve repair: An overview of current and future devices. Open Heart 2021, 8, e001564. [Google Scholar] [CrossRef] [PubMed]
- Hahn, R.T.; Zamorano, J.L. The need for a new tricuspid regurgitation grading scheme. Eur. Heart J.-Cardiovasc. Imaging 2017, 18, 1342–1343. [Google Scholar] [CrossRef]
- Lancellotti, P.; Tribouilloy, C.; Hagendorff, A.; Popescu, B.A.; Edvardsen, T.; Pierard, L.A.; Badano, L.; Zamorano, J.L. Recommendations for the echocardiographic assessment of native valvular regurgitation: An executive summary from the European Association of Cardiovascular Imaging. Eur. Heart J.-Cardiovasc. Imaging 2013, 14, 611–644. [Google Scholar] [CrossRef] [PubMed]
- Zoghbi, W.A.; Adams, D.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation. J. Am. Soc. Echocardiogr. 2017, 30, 303–371. [Google Scholar] [CrossRef] [PubMed]
| Variable | FMR N = 148 (%) | DMR N = 60 (%) | p Value |
|---|---|---|---|
| Age | 77.2 ± 8.4 | 80.2 ± 7.2 | 0.02 |
| Gender-Female | 47 (31.8) | 19 (31.7) | 0.26 |
| BMI | 25.4 ± 3.1 | 26.1 ± 4.2 | 0.21 |
| Hemoglobin (g/dL) | 11.6 ± 1.7 | 12.2 ± 1.2 | 0.11 |
| GFR (mL/min) | 58.4 ± 27.2 | 58.1 ± 20.1 | 0.36 |
| Hypertension | 118 (79.8) | 38 (63.3) | 0.42 |
| Diabetes Mellitus | 71 (48.0) | 21 (35.0) | 0.27 |
| Dyslipidemia | 101 (68.2) | 43 (71.7) | 0.10 |
| Smoking | 38 (25.7) | 26 (43.3) | 0.31 |
| COPD | 24 (16.2) | 11 (18.3) | 0.23 |
| Stroke (CVA or TIA) | 36 (24.3) | 8 (13.3) | 0.09 |
| Coronary Artery disease | 80 (54.1) | 6 (10.0) | 0.02 |
| Cardiac Surgery | 47 (31.8) | 6 (10.0) | 0.09 |
| Atrial Fibrillation/Flutter | 105 (70.9) | 23 (38.3) | 0.02 |
| Pacemaker | 31 (20.9) | 13 (21.7) | 0.41 |
| Oncologic disease | 17 (11.5) | 12 (20.0) | 0.12 |
| Previous MitraClip | 4 (2.7) | 1 (1.7) | 0.22 |
| Peripheral pitting edema | 21 (14.2) | 9 (15.0) | 0.34 |
| NYHA class - no. (%) | 0.18 | ||
| II | 42 (28.4) | 21 (35.0) | |
| III | 60 (40.5) | 23 (38.3) | |
| IV | 46 (31.1) | 16 (26.7) | |
| STS score- for MV repair mortality | 5.8 ± 4.1 | 5.4 ± 3.3 | 0.37 |
| Medications | |||
| Antiplatelets | 67 (45.3) | 20 (33.3) | 0.12 |
| Anticoagulants | 38 (25.7) | 19 (31.7) | 0.29 |
| ACEi/ARB | 100 (67.6) | 41 (68.3) | 0.32 |
| Beta blockers | 126 (85.1) | 47 (78.3) | 0.39 |
| MRA | 42 (28.4) | 12 (20.0) | 0.42 |
| Variable | FMR N = 148 (%) | DMR N = 60 (%) | p Value |
|---|---|---|---|
| LVEDd (mm) | 53.8 ± 7.8 | 50.9 ± 5.1 | 0.03 |
| LVESd (mm) | 38.2 ± 9.8 | 34.5 ± 6.9 | 0.04 |
| IVS (mm) | 10.8 ± 4.2 | 10.7 ± 3.9 | 0.62 |
| PWT (mm) | 10.2 ± 5.4 | 10.0 ± 5.2 | 0.42 |
| Simpson EF (%) | 42.4 ± 12.1 | 52.1 ± 10.9 | <0.01 |
| Mitral anulus calcification | 27 (18.2) | 8 (13.3) | 0.42 |
| Effective regurgitant orifice area (cm2) | 0.4 ± 0.1 | 0.4 ± 0.2 | 0.82 |
| MR Volume (mL) | 60.4 ± 22.3 | 68.1 ± 23.1 | 0.04 |
| Tricuspid Regurgitation Severity | |||
| No TR (0) | 23 (15.5) | 5 (8.3) | 0.24 |
| Mild TR (1) | 107 (72.3) | 42 (70.0) | |
| Moderate TR (2) | 10 (6.8) | 11 (18.3) | |
| Severe TR (3) | 8 (5.4) | 2 (3.3) | |
| Estimated PA pressure (mmHg) | 53.2 ± 14.4 | 50.5 ± 14.1 | 0.04 |
| Right ventricular dysfunction (Grade) | 0.30 | ||
| Normal (0) | 82 (55.4) | 42 (70.0) | |
| Mild (1) | 61 (41.2) | 16 (26.7) | |
| Moderate (2) | 5 (3.4) | 2 (3.3) | |
| Left Atrial Area (cm2) | 30.7 ± 8.1 | 31.6 ± 9.0 | 0.27 |
| Variable | FMR N = 148 (%) | DMR N = 60 (%) | p Value |
|---|---|---|---|
| Immediate post-procedure | |||
| MR up to grade 1 | 139 (93.9) | 55 (91.7) | 0.83 |
| MR grade 2 | 9 (6.1) | 5 (8.3) | |
| MR grade 3 | 0 (0.0) | 0 (0.0) | |
| MR grade 4 | 0 (0.0) | 0 (0.0) | |
| 1-month | |||
| MR grade 2 or above | 7 (4.7) | 4 (6.7) | 0.47 |
| Hospitalization for HF | 10 (6.8) | 2 (3.3) | 0.15 |
| Surgery or clip re-intervention | 5 (3.4) | 2 (3.3) | 0.89 |
| MACE | 15 (10.1) | 3 (5.0) | 0.09 |
| Death | 8 (5.4) | 1 (1.7) | 0.12 |
| 1-year | |||
| MR grade 2 or above | 13 (8.8) | 5 (8.3) | 0.17 |
| Hospitalization for HF | 45 (30.4) | 9 (15.0) | 0.03 |
| Surgery or clip re-intervention | 7 (4.7) | 3 (5.0) | 0.08 |
| MACE | 61 (41.2) | 13 (21.7) | 0.02 |
| Death | 32 (21.6) | 6 (10.0) | 0.04 |
| Variable | HR (95% CI) | p Value |
|---|---|---|
| Age (years) | 1.07 (1.02–1.92) | 0.04 |
| STS score | 1.03 (0.89–1.27) | 0.79 |
| Diabetes Mellitus | 1.39 (0.72–4.21) | 0.23 |
| GFR (mL/min) | 0.97 (0.94–1.01) | 0.07 |
| LVEF (per 1%) | 0.93 (0.87–0.97) | 0.02 |
| Functional Class (NYHA) | 1.08 (0.84–2.93) | 0.42 |
| Right ventricular dysfunction | 1.30 (0.88–5.38) | 0.38 |
| Post–procedure MR | 1.25 (0.89–2.34) | 0.25 |
| FMR vs. DMR | 1.67 (0.98–3.74) | 0.07 |
| Variable | HR (95% CI) | p Value |
|---|---|---|
| Age (years) | 1.10 (1.01–1.24) | 0.02 |
| STS score | 1.23 (0.97–1.54) | 0.09 |
| Diabetes Mellitus | 1.39 (0.73–4.21) | 0.28 |
| GFR (mL/min) | 0.97 (0.94–1.01) | 0.07 |
| LVEF (per 1%) | 0.92 (0.84–0.98) | 0.04 |
| Functional Class (NYHA) | 1.08 (0.84–2.93) | 0.42 |
| Right ventricular dysfunction | 1.32 (0.82–5.12) | 0.39 |
| Post–procedure MR | 1.96 (1.09–2.77) | 0.03 |
| FMR vs. DMR | 1.78 (1.23–2.48) | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kheifets, M.; Angelini, F.; D’Ascenzo, F.; Pidello, S.; Engelstein, H.; Bocchino, P.P.; Boretto, P.; Frea, S.; Levi, A.; Vaknin-Assa, H.; et al. Outcomes of Transcatheter Edge-to-Edge Repair in Degenerative vs. Functional Mitral Regurgitation. J. Clin. Med. 2022, 11, 6010. https://doi.org/10.3390/jcm11206010
Kheifets M, Angelini F, D’Ascenzo F, Pidello S, Engelstein H, Bocchino PP, Boretto P, Frea S, Levi A, Vaknin-Assa H, et al. Outcomes of Transcatheter Edge-to-Edge Repair in Degenerative vs. Functional Mitral Regurgitation. Journal of Clinical Medicine. 2022; 11(20):6010. https://doi.org/10.3390/jcm11206010
Chicago/Turabian StyleKheifets, Mark, Filippo Angelini, Fabrizio D’Ascenzo, Stefano Pidello, Haya Engelstein, Pier Paolo Bocchino, Paolo Boretto, Simone Frea, Amos Levi, Hana Vaknin-Assa, and et al. 2022. "Outcomes of Transcatheter Edge-to-Edge Repair in Degenerative vs. Functional Mitral Regurgitation" Journal of Clinical Medicine 11, no. 20: 6010. https://doi.org/10.3390/jcm11206010
APA StyleKheifets, M., Angelini, F., D’Ascenzo, F., Pidello, S., Engelstein, H., Bocchino, P. P., Boretto, P., Frea, S., Levi, A., Vaknin-Assa, H., Vaturi, M., Shapira, Y., Kornowski, R., & Perl, L. (2022). Outcomes of Transcatheter Edge-to-Edge Repair in Degenerative vs. Functional Mitral Regurgitation. Journal of Clinical Medicine, 11(20), 6010. https://doi.org/10.3390/jcm11206010








