Prognostic Value of Coronary Calcium Score in Asymptomatic Individuals: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Planning and Conducting the Review
2.3. Quality Assessment
3. Results
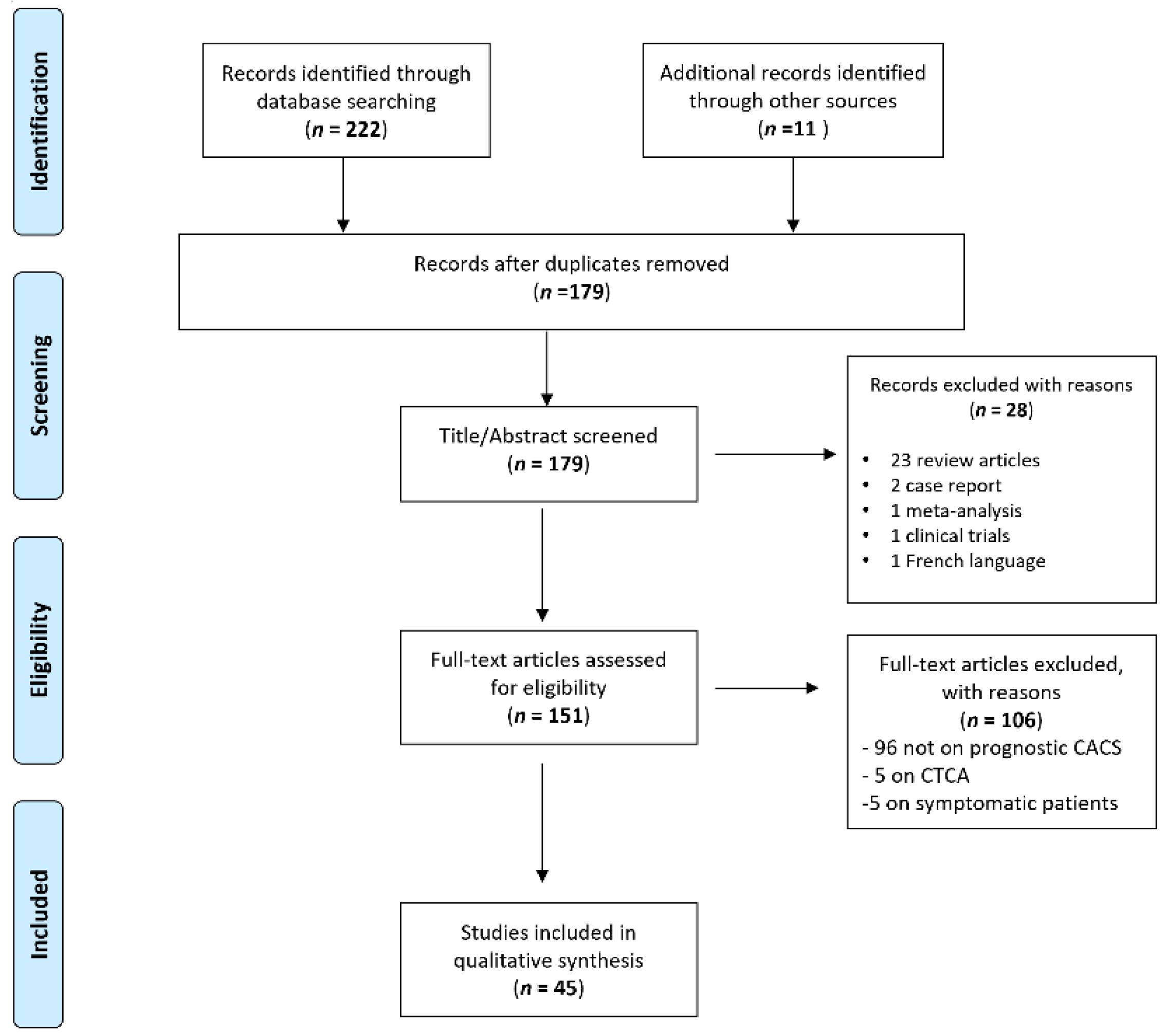
3.1. Study Selection
3.2. Characteristics of the Included Studies
3.3. Prognostic Value of Coronary Calcium Score
3.3.1. Coronary Calcium Score
3.3.2. CAC Score in Diabetic Patients
3.3.3. CAC Score Associated with SPECT
3.3.4. CAC Score Associated with Biomarkers, Imaging, and Clinical Parameters
3.3.5. Coronary Computed Tomography Angiography (CCTA) vs. CAC Score
3.3.6. Quality Assessment
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Greenland, P.; Alpert, J.S.; Beller, G.A.; Benjamin, E.J.; Budoff, M.J.; Fayad, Z.A.; Foster, E.; Hlatky, M.A.; Hodgson, J.M.; Kushner, F.G.; et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: A report of the American Col-lege of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2010, 56, e50–e103. [Google Scholar] [CrossRef] [PubMed]
- Greenland, P.; Blaha, M.J.; Budoff, M.J.; Erbel, R.; Watson, K.E. Coronary Calcium Score and Cardiovascular Risk. J. Am. Coll. Cardiol. 2018, 72, 434–447. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-H.; Youn, H.-J.; Jung, H.-O.; Chang, K.; Choi, Y.-S.; Jung, J.I. Coronary artery calcium score plays an important role for cardiovascular risk stratification in the statin benefit groups of asymptomatic individuals. Lipids Health Dis. 2017, 16, 172. [Google Scholar] [CrossRef] [PubMed]
- Budoff, M.J.; Mayrhofer, T.; Ferencik, M.; Bittner, D.; Lee, K.L.; Lu, M.T.; Coles, A.; Jang, J.; Krishnam, M.; Douglas, P.S.; et al. Prognostic Value of Coronary Artery Calcium in the PROMISE Study (Prospective Multicenter Imaging Study for Evaluation of Chest Pain). Circulation 2017, 136, 1993–2005. [Google Scholar] [CrossRef]
- Elias-Smale, S.E.; Proença, R.V.; Koller, M.T.; Kavousi, M.; van Rooij, F.J.; Hunink, M.G.; Steyerberg, E.W.; Hofman, A.; Oudkerk, M.; Witteman, J.C. Coronary Calcium Score Improves Classification of Coronary Heart Disease Risk in the Elderly: The Rotterdam Study. J. Am. Coll. Cardiol. 2010, 56, 1407–1414. [Google Scholar] [CrossRef]
- Agarwal, S.; Morgan, T.; Herrington, D.M.; Xu, J.; Cox, A.J.; Freedman, B.I.; Carr, J.J.; Bowden, D.W. Coronary Calcium Score and Prediction of All-Cause Mortality in Diabetes: The diabetes heart study. Diabetes Care 2011, 34, 1219–1224. [Google Scholar] [CrossRef]
- Agarwal, S.; Cox, A.J.; Herrington, D.M.; Jorgensen, N.W.; Xu, J.; Freedman, B.I.; Carr, J.J.; Bowden, D.W. Coronary Calcium Score Predicts Cardiovascular Mortality in Diabetes: Diabetes heart study. Diabetes Care 2013, 36, 972–977. [Google Scholar] [CrossRef]
- Chung, S.-L.; Yang, C.-C.; Chen, C.-C.; Hsu, Y.-C.; Lei, M.-H. Coronary Artery Calcium Score Compared with Cardio-Ankle Vascular Index in the Prediction of Cardiovascular Events in Asymptomatic Patients with Type 2 Diabetes. J. Atheroscler. Thromb. 2015, 22, 1255–1265. [Google Scholar] [CrossRef]
- Faustino, A.; Providência, R.; Mota, P.; Barra, S.; Silva, J.; Fernandes, A.; Catarino, R.; Basso, S.; Costa, M.; Leitão-Marques, A. Can cardiac computed tomography predict cardiovascular events in asymptomatic type-2 diabetics?: Results of a long term follow-up. BMC Cardiovasc. Disord. 2014, 14, 2. [Google Scholar] [CrossRef]
- Erbel, R.; Möhlenkamp, S.; Moebus, S.; Schmermund, A.; Lehmann, N.; Stang, A.; Dragano, N.; Grönemeyer, D.; Seibel, R.; Kälsch, H.; et al. Coronary Risk Stratification, Discrimination, and Reclassification Improvement Based on Quantification of Subclinical Coronary Atherosclerosis: The Heinz Nixdorf Recall Study. J. Am. Coll. Cardiol. 2010, 56, 1397–1406. [Google Scholar] [CrossRef]
- Budoff, M.J.; Hokanson, J.E.; Nasir, K.; Shaw, L.J.; Kinney, G.L.; Chow, D.; DeMoss, D.; Nuguri, V.; Nabavi, V.; Ratakonda, R.; et al. Progression of Coronary Artery Calcium Predicts All-Cause Mortality. JACC: Cardiovasc. Imaging 2010, 3, 1229–1236. [Google Scholar] [CrossRef] [PubMed]
- Koulaouzidis, G.; Charisopoulou, D.; Maffrett, S.; Tighe, M.; Jenkins, P.J.; McArthur, T. Coronary Artery Calcification Progression in Asymptomatic Individuals with Initial Score of Zero. Angiology 2013, 64, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.; Suh, J.-W.; Chang, H.-J.; Kim, K.-I.; Jeon, E.J.; Choi, S.I.; Cho, Y.-S.; Youn, T.-J.; Chae, I.-H.; Kim, C.-H.; et al. Prevalence and Prognostic Implication of Non-Calcified Plaque in Asymptomatic Population with Coronary Artery Calcium Score of Zero. Korean Circ. J. 2013, 43, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Descalzo, M.; Vidal-Perez, R.; Leta, R.; AlOmar, X.; Pons-Llado, G.; Carreras, F. Usefulness of coronary artery calcium for detecting significant coronary artery disease in asymptomatic individuals. Rev. Clin. Esp. 2014, 214, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Fathala, A.; Alreshoodi, S.; Al Rujaib, M.; Shoukri, M.; Al Sergani, H.; Al Buriki, J.; Al Sugair, A. Coronary artery calcium score in high-risk asymptomatic women in Saudi Arabia. Ann. Saudi Med. 2015, 35, 298–302. [Google Scholar] [CrossRef]
- Ohmoto-Sekine, Y.; Yanagibori, R.; Amakawa, K.; Ishihara, M.; Tsuji, H.; Ogawa, K.; Ishimura, R.; Ishiwata, S.; Ohno, M.; Yamaguchi, T.; et al. Prevalence and distribution of coronary calcium in asymptomatic Japanese subjects in lung cancer screening computed tomography. J. Cardiol. 2016, 67, 449–454. [Google Scholar] [CrossRef]
- Orimoloye, O.A.; Budoff, M.J.; Dardari, Z.A.; Mirbolouk, M.; Uddin, S.I.; Berman, D.S.; Rozanski, A.; Shaw, L.J.; Rumberger, J.A.; Nasir, K.; et al. Race/Ethnicity and the Prognostic Implications of Coronary Artery Calcium for All-Cause and Cardiovascular Disease Mortality: The Coronary Artery Calcium Consortium. J. Am. Heart Assoc. 2018, 7, e010471. [Google Scholar] [CrossRef]
- Arnson, Y.; Rozanski, A.; Gransar, H.; Friedman, J.D.; Hayes, S.W.; Thomson, L.E.; Tamarappoo, B.; Slomka, P.; Wang, F.; Germano, G.; et al. Comparison of the Coronary Artery Calcium Score and Number of Calcified Coronary Plaques for Predicting Patient Mortality Risk. Am. J. Cardiol. 2017, 120, 2154–2159. [Google Scholar] [CrossRef]
- Dayan, A.; Narin, B.; Biteker, M.; Aksoy, S.; Fotbolcu, H.; Duman, D. Coronary calcium score, albuminuria and inflammatory markers in type 2 diabetic patients: Associations and prognostic implications. Diabetes Res. Clin. Pract. 2012, 98, 98–103. [Google Scholar] [CrossRef]
- Von Scholten, B.J.; Reinhard, H.; Hansen, T.W.; Lindhardt, M.; Petersen, C.L.; Wiinberg, N.; Hansen, P.R.; Parving, H.-H.; Jacobsen, P.K.; Rossing, P. Additive prognostic value of plasma N-terminal pro-brain natriuretic peptide and coronary artery calcification for cardiovascular events and mortality in asymptomatic patients with type 2 diabetes. Cardiovasc. Diabetol. 2015, 14, 59. [Google Scholar] [CrossRef]
- Kemmer, N.; Case, J.; Chandna, S.; Neff, G. The Role of Coronary Calcium Score in the Risk Assessment of Liver Transplant Candidates. Transplant. Proc. 2014, 46, 230–233. [Google Scholar] [CrossRef]
- Park, H.-B.; Jeong, H.; Lee, J.H.; Suh, Y.; Hwang, E.-S.; Cho, Y.-H.; Cho, D.-K. Predictors of Severe or Moderate Coronary Artery Disease in Asymptomatic Individuals with Extremely Low Coronary Calcium Scores. Yonsei Med. J. 2019, 60, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Cademartiri, F.; Maffei, E.; Palumbo, A.; Seitun, S.; Martini, C.; Tedeschi, C.; La Grutta, L.; Midiri, M.; Weustink, A.C.; Mollet, N.R.; et al. Coronary calcium score and computed tomography coronary angiography in high-risk asymptomatic subjects: Assessment of diagnostic accuracy and prevalence of non-obstructive coronary artery disease. Eur. Radiol. 2010, 20, 846–854. [Google Scholar] [CrossRef] [PubMed]
- Han, D.; Hartaigh, B.; Gransar, H.; Lee, J.H.; Rizvi, A.; Baskaran, L.; Schulman-Marcus, J.; Dunning, A.; Achenbach, S.; Al-Mallah, M.H.; et al. Incremental prognostic value of coronary computed tomography angiography over coronary calcium scoring for major adverse cardiac events in elderly asymptomatic individuals. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Dedic, A.; Kate, G.-J.R.T.; Roos, C.J.; Neefjes, L.A.; De Graaf, M.A.; Spronk, A.; Delgado, V.; Van Lennep, J.E.R.; Moelker, A.; Ouhlous, M.; et al. Prognostic Value of Coronary Computed Tomography Imaging in Patients at High Risk Without Symptoms of Coronary Artery Disease. Am. J. Cardiol. 2016, 117, 768–774. [Google Scholar] [CrossRef]
- Gräni, C.; Vontobel, J.; Benz, D.C.; Bacanovic, S.; A Giannopoulos, A.; Messerli, M.; Grossmann, M.; Gebhard, C.; Pazhenkottil, A.P.; Gaemperli, O.; et al. Ultra-low-dose coronary artery calcium scoring using novel scoring thresholds for low tube voltage protocols—A pilot study. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 1362–1371. [Google Scholar] [CrossRef]
- Tesche, C.; De Cecco, C.N.; Schoepf, U.J.; Duguay, T.M.; Albrecht, M.H.; De Santis, D.; Varga-Szemes, A.; Lesslie, V.W.; Ebersberger, U.; Bayer, R.R.; et al. CT coronary calcium scoring with tin filtration using iterative beam-hardening calcium correction reconstruction. Eur. J. Radiol. 2017, 91, 29–34. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Hayden, J.A.; Côté, P.; Bombardier, C. Evaluation of the Quality of Prognosis Studies in Systematic Reviews. Ann. Intern. Med. 2006, 144, 427–437. [Google Scholar] [CrossRef]
- Hayden, J.A.; Van Der Windt, D.A.; Cartwright, J.L.; Côté, P.; Bombardier, C. Assessing Bias in Studies of Prognostic Factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef]
- Dudum, R.; Dzaye, O.; Mirbolouk, M.; Dardari, Z.A.; Orimoloye, O.A.; Budoff, M.J.; Berman, D.S.; Rozanski, A.; Miedema, M.D.; Nasir, K.; et al. Coronary artery calcium scoring in low risk patients with family history of coronary heart disease: Validation of the SCCT guideline approach in the coronary artery calcium consortium. J. Cardiovasc. Comput. Tomogr. 2019, 13, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.; Hartaigh, B.; Gransar, H.; Valenti, V.; Lin, F.Y.; Achenbach, S.; Berman, D.S.; Budoff, M.J.; Callister, T.Q.; Al-Mallah, M.H.; et al. Prognostic implications of coronary artery calcium in the absence of coronary artery luminal narrowing. Atherosclerosis 2017, 262, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Carr, J.J.; Jacobs, D.R.; Terry, J.G.; Shay, C.M.; Sidney, S.; Liu, K.; Schreiner, P.J.; Lewis, C.E.; Shikany, J.M.; Reis, J.P.; et al. Association of Coronary Artery Calcium in Adults Aged 32 to 46 Years with Incident Coronary Heart Disease and Death. JAMA Cardiol. 2017, 2, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Han, D.; Hartaigh, B.; Gransar, H.; Yoon, J.H.; Kim, K.-J.; Kim, M.-K.; Choi, S.-Y.; Sung, J.; Chang, H.-J. Incremental Benefit of Coronary Artery Calcium Score Above Traditional Risk Factors for All-Cause Mortality in Asymptomatic Korean Adults. Circ. J. 2015, 79, 2445–2451. [Google Scholar] [CrossRef]
- Nasir, K.; Rubin, J.; Blaha, M.J.; Shaw, L.J.; Blankstein, R.; Rivera, J.J.; Khan, A.N.; Berman, D.; Raggi, P.; Callister, T.; et al. Interplay of Coronary Artery Calcification and Traditional Risk Factors for the Prediction of All-Cause Mortality in Asymptomatic Individuals. Circ. Cardiovasc. Imaging 2012, 5, 467–473. [Google Scholar] [CrossRef]
- Shaw, L.J.; Giambrone, A.E.; Blaha, M.J.; Knapper, J.T.; Berman, D.S.; Bellam, N.; Quyyumi, A.; Budoff, M.J.; Callister, T.Q.; Min, J.K. Long-Term Prognosis After Coronary Artery Calcification Testing in Asymptomatic Patients: A Cohort Study. Ann. Intern. Med. 2015, 163, 14–21. [Google Scholar] [CrossRef]
- Patel, J.; Blaha, M.J.; McEvoy, J.; Qadir, S.; Tota-Maharaj, R.; Shaw, L.J.; Rumberger, J.A.; Callister, T.Q.; Berman, D.S.; Min, J.K.; et al. All-cause mortality in asymptomatic persons with extensive Agatston scores above 1000. J. Cardiovasc. Comput. Tomogr. 2014, 8, 26–32. [Google Scholar] [CrossRef]
- Valenti, V.; Hartaigh, B.; Heo, R.; Cho, I.; Schulman-Marcus, J.; Gransar, H.; Truong, Q.A.; Shaw, L.J.; Knapper, J.; Kelkar, A.A.; et al. A 15-Year Warranty Period for Asymptomatic Individuals without Coronary Artery Calcium: A Prospective Follow-Up of 9715 Individuals. JACC Cardiovasc. Imaging 2015, 8, 900–909. [Google Scholar] [CrossRef]
- Lee, J.H.; Han, D.; Hartaigh, B.; Rizvi, A.; Gransar, H.; Park, H.-B.; Park, H.E.; Choi, S.-Y.; Chun, E.J.; Sung, J.; et al. Warranty Period of Zero Coronary Artery Calcium Score for Predicting All-Cause Mortality According to Cardiac Risk Burden in Asymptomatic Korean Adults. Circ. J. 2016, 80, 2356–2361. [Google Scholar] [CrossRef]
- Blaha, M.J.; Cainzos-Achirica, M.; Dardari, Z.; Blankstein, R.; Shaw, L.J.; Rozanski, A.; Rumberger, J.A.; Dzaye, O.; Michos, E.D.; Berman, D.S.; et al. All-cause and cause-specific mortality in individuals with zero and minimal coronary artery calcium: A long-term, competing risk analysis in the Coronary Artery Calcium Consortium. Atherosclerosis 2020, 294, 72–79. [Google Scholar] [CrossRef]
- Knapper, J.T.; Khosa, F.; Blaha, M.J.; Lebeis, T.A.; Kay, J.; Sandesara, P.B.; Kelkar, A.A.; Berman, D.S.; Quyyumi, A.A.; Budoff, M.J.; et al. Coronary calcium scoring for long-term mortality prediction in patients with and without a family history of coronary disease. Heart 2016, 102, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Radford, N.B.; DeFina, L.F.; Barlow, C.E.; Lakoski, S.G.; Leonard, D.; Paixao, A.R.; Khera, A.; Levine, B.D. Progression of CAC Score and Risk of Incident CVD. JACC Cardiovasc. Imaging 2016, 9, 1420–1429. [Google Scholar] [CrossRef] [PubMed]
- Graham, G.; Blaha, M.J.; Budoff, M.J.; Rivera, J.J.; Agatston, A.; Raggi, P.; Shaw, L.J.; Berman, D.; Rana, J.S.; Callister, T.; et al. Impact of coronary artery calcification on all-cause mortality in individuals with and without hypertension. Atherosclerosis 2012, 225, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Shemesh, J.; Motro, M.; Morag-Koren, N.; Tenenbaum, A.; Apter, S.; Weiss, A.; Grossman, E. Coronary Artery Calcification Predicts Long-Term Mortality in Hypertensive Adults. Am. J. Hypertens. 2011, 24, 681–686. [Google Scholar] [CrossRef]
- McEvoy, J.W.; Blaha, M.J.; Rivera, J.J.; Budoff, M.J.; Khan, A.N.; Shaw, L.J.; Berman, D.S.; Raggi, P.; Min, J.K.; Rumberger, J.A.; et al. Mortality rates in smokers and nonsmokers in the presence or absence of coronary artery calcification. JACC Cardiovasc. Imaging 2012, 5, 1037–1045, Corrected in JACC Cardiovasc. Imaging 2013, 6, 747. [Google Scholar] [CrossRef]
- Kelkar, A.A.; Schultz, W.M.; Khosa, F.; Schulman-Marcus, J.; O’Hartaigh, B.W.; Gransar, H.; Blaha, M.J.; Knapper, J.T.; Berman, D.S.; Quyyumi, A.; et al. Long-Term Prognosis After Coronary Artery Calcium Scoring Among Low-Intermediate Risk Women and Men. Circ. Cardiovasc. Imaging 2016, 9, e003742. [Google Scholar] [CrossRef]
- Lahti, S.J.; Feldman, D.I.; Dardari, Z.; Mirbolouk, M.; Orimoloye, O.A.; Osei, A.D.; Graham, G.; Rumberger, J.; Shaw, L.; Budoff, M.J.; et al. The association between left main coronary artery calcium and cardiovascular-specific and total mortality: The Coronary Artery Calcium Consortium. Atherosclerosis 2019, 286, 172–178. [Google Scholar] [CrossRef]
- Cho, I.; Al’Aref, S.J.; Berger, A.; Hartaigh, B.; Gransar, H.; Valenti, V.; Lin, F.Y.; Achenbach, S.; Berman, D.S.; Budoff, M.J.; et al. Prognostic value of coronary computed tomographic angiography findings in asymptomatic individuals: A 6-year follow-up from the prospective multicentre international CONFIRM study. Eur. Heart J. 2018, 39, 934–941. [Google Scholar] [CrossRef]
- Dzaye, O.; Dudum, R.; Mirbolouk, M.; Orimoloye, O.; Osei, A.D.; Dardari, Z.; Berman, D.S.; Miedema, M.D.; Shaw, L.; Rozanski, A.; et al. Validation of the Coronary Artery Calcium Data and Reporting System (CAC-DRS): Dual importance of CAC score and CAC distribution from the Coronary Artery Calcium (CAC) consortium. J. Cardiovasc. Comput. Tomogr. 2020, 14, 12–17. [Google Scholar] [CrossRef]
- Valenti, V.; Hartaigh, B.; Cho, I.; Schulman-Marcus, J.; Gransar, H.; Heo, R.; Truong, Q.A.; Shaw, L.J.; Knapper, J.; Kelkar, A.A.; et al. Absence of Coronary Artery Calcium Identifies Asymptomatic Diabetic Individuals at Low Near-Term but Not Long-Term Risk of Mortality: A 15-Year Follow-Up Study of 9715 Patients. Circ. Cardiovasc. Imaging 2016, 9, e003528. [Google Scholar] [CrossRef]
- Malik, S.; Zhao, Y.; Budoff, M.; Nasir, K.; Blumenthal, R.S.; Bertoni, A.G.; Wong, N.D. Coronary Artery Calcium Score for Long-term Risk Classification in Individuals with Type 2 Diabetes and Metabolic Syndrome from the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol. 2017, 2, 1332–1340. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, K.; Li, D.; Nakanishi, R.; Kinninger, A.; Almeida, S.; Cherukuri, L.; Shekar, C.; Roy, S.K.; Birudaraju, D.; Rai, K.; et al. Low short-term and long-term cardiovascular and all-cause mortality in absence of coronary artery calcium: A 22-year follow-up observational study from large cohort. J. Diabetes Its Complicat. 2019, 33, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, V.; Gravino, E.; Russo, C.; Salvati, A.; Lombardi, C.; Sauro, R.; Rosato, G. Coronary atherosclerosis burden by coronary computed tomography in type II diabetes with preclinical non-obstructive carotid atherosclerosis and without inducible myocardial ischemia. Diabetes Res. Clin. Pract. 2017, 123, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Tang, J.; Zheng, S.; Jiang, H.; Deng, L.; Wang, P. Prognostic significance of coronary artery calcium scoring and single-photon emission computed tomographic myocardial perfusion imaging on major adverse cardiac events in patients at low risk for suspected coronary artery disease. Acta Cardiol. 2019, 74, 508–514. [Google Scholar] [CrossRef]
- Chang, S.M.; Nabi, F.; Xu, J.; Pratt, C.M.; Mahmarian, A.C.; Frias, M.E.; Mahmarian, J.J. Value of CACS Compared with ETT and Myocardial Perfusion Imaging for Predicting Long-Term Cardiac Outcome in Asymptomatic and Symptomatic Patients at Low Risk for Coronary Disease: Clinical implications in a multimodality imaging world. JACC Cardiovasc. Imaging 2015, 8, 134–144. [Google Scholar] [CrossRef]
- Havel, M.; Kaminek, M.; Metelkova, I.; Budikova, M.; Henzlova, L.; Koranda, P.; Zadražil, J.; Kincl, V. Prognostic value of myocardial perfusion imaging and coronary artery calcium measurements in patients with end-stage renal disease. Hell. J. Nucl. Med. 2015, 18, 199–206. [Google Scholar] [CrossRef]
- Serra, C.M.; López-Perna, Y.; Getino, A.M.; Sánchez-Vizcaíno, E.; Amat, J.D.; Utset, J.M. Long-term risk of cardiovascular events after detecting silent coronary atheromatosis using computed tomography. Coron. Artery Dis. 2019, 30, 131–136. [Google Scholar] [CrossRef]
- Dikic, M.; Tesic, M.; Markovic, Z.; Giga, V.; Djordjevic-Dikic, A.; Stepanovic, J.; Beleslin, B.; Jovanović, I.; Mladenovič, A.; Seferović, J.; et al. Prognostic value of calcium score and coronary flow velocity reserve in asymptomatic diabetic patients. Cardiovasc. Ultrasound 2015, 13, 41. [Google Scholar] [CrossRef][Green Version]
- Park, H.E.; Chun, E.-J.; Choi, S.-I.; Lee, S.-P.; Yoon, C.-H.; Kim, H.-K.; Youn, T.-J.; Kim, Y.-J.; Choi, N.-J.; Sohn, D.-W.; et al. Clinical and imaging parameters to predict cardiovascular outcome in asymptomatic subjects. Int. J. Cardiovasc. Imaging 2013, 29, 1595–1602. [Google Scholar] [CrossRef]
- Rana, J.S.; Gransar, H.; Wong, N.D.; Shaw, L.; Pencina, M.; Nasir, K.; Rozanski, A.; Hayes, S.W.; Thomson, L.E.; Friedman, J.D.; et al. Comparative Value of Coronary Artery Calcium and Multiple Blood Biomarkers for Prognostication of Cardiovascular Events. Am. J. Cardiol. 2012, 109, 1449–1453. [Google Scholar] [CrossRef]
- Choi, S.-Y.; Sung, J.; Park, H.E.; Han, D.; Chang, H.-J. Combined effects of exercise capacity and coronary atherosclerotic burden on all-cause mortality in asymptomatic Koreans. Atherosclerosis 2016, 251, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.J.; Chun, E.J.; Yoon, Y.E.; Park, K.S.; Jang, H.C.; Lim, S. Long-Term Prognostic Value of Coronary Computed Tomography Angiography in an Asymptomatic Elderly Population. J. Am. Heart Assoc. 2019, 8, e013523. [Google Scholar] [CrossRef]
- Takamura, K.; Fujimoto, S.; Kondo, T.; Hiki, M.; Kawaguchi, Y.; Kato, E.; Daida, H. Incremental Prognostic Value of Coronary Computed Tomography Angiography: High-Risk Plaque Characteristics in Asymptomatic Patients. J. Atheroscler. Thromb. 2017, 24, 1174–1185. [Google Scholar] [CrossRef] [PubMed]
- Plank, F.; Friedrich, G.; Dichtl, W.; Klauser, A.; Jaschke, W.; Franz, W.-M.; Feuchtner, G. The diagnostic and prognostic value of coronary CT angiography in asymptomatic high-risk patients: A cohort study. Open Heart 2014, 1, e000096. [Google Scholar] [CrossRef]
- Cho, I.; Chang, H.-J.; Hartaigh, B.; Shin, S.; Sung, J.M.; Lin, F.Y.; Achenbach, S.; Heo, R.; Berman, D.S.; Budoff, M.J.; et al. Incremental prognostic utility of coronary CT angiography for asymptomatic patients based upon extent and severity of coronary artery calcium: Results from the COronary CT Angiography EvaluatioN for Clinical Outcomes InteRnational Multicenter (CONFIRM) Study. Eur. Heart J. 2014, 36, 501–508, Corrected in Eur. Heart J. 2015, 36, 3287. [Google Scholar] [CrossRef]
- Yoo, D.H.; Chun, E.J.; Choi, S.I.; Kim, J.A.; Jin, K.N.; Yeon, T.-J.; Choi, N.-J. Significance of noncalcified coronary plaque in asymptomatic subjects with low coronary artery calcium score: Assessment with coronary computed tomography angiography. Int. J. Cardiovasc. Imaging 2011, 27 (Suppl. S1), 27–35. [Google Scholar] [CrossRef]
- Hoogen, I.J.V.D.; De Graaf, M.A.; Roos, C.J.; Leen, A.C.; Kharagjitsingh, A.V.; Wolterbeek, R.; Kroft, L.J.; Jukema, J.W.; Bax, J.J.; Scholte, A.J. Prognostic value of coronary computed tomography angiography in diabetic patients without chest pain syndrome. J. Nucl. Cardiol. 2015, 23, 24–36. [Google Scholar] [CrossRef]
- Halon, D.A.; Azencot, M.; Rubinshtein, R.; Zafrir, B.; Flugelman, M.Y.; Lewis, B.S. Coronary Computed Tomography (CT) Angiography as a Predictor of Cardiac and Noncardiac Vascular Events in Asymptomatic Type 2 Diabetics: A 7-Year Population-Based Cohort Study. J. Am. Heart Assoc. 2016, 5, e003226. [Google Scholar] [CrossRef] [PubMed]
- Min, J.K.; Labounty, T.M.; Gomez, M.J.; Achenbach, S.; Al-Mallah, M.; Budoff, M.J.; Cademartiri, F.; Callister, T.Q.; Chang, H.-J.; Cheng, V.; et al. Incremental prognostic value of coronary computed tomographic angiography over coronary artery calcium score for risk prediction of major adverse cardiac events in asymptomatic diabetic individuals. Atherosclerosis 2014, 232, 298–304. [Google Scholar] [CrossRef]
- Hur, J.; Lee, K.H.; Hong, S.R.; Suh, Y.J.; Hong, Y.; Lee, H.S.; Kim, Y.J.; Chang, H.-J.; Choi, B.W. Prognostic value of coronary computed tomography angiography in stroke patients. Atherosclerosis 2015, 238, 271–277. [Google Scholar] [CrossRef]

| Author, Year | N. of Patients | Mean Age (Years) | Study Design (P/R) | Pts | Risk Factors | Imaging | Scan Details | Follow-Up (Years) | Statistical Analysis | Main Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Dzaye et al. [49], 2020 | 54,678 | 54.2 | R | ASX | DLP, HT, DM, SS, FH of CAD | EBCT, CT | MDCT manifacturer NR | 11.7 | CPhM AUC analysis | The CAC-DRS system, combining the Agatston score and the number of vessels with CAC provides better stratification of risk for CHD, CVD, and all-cause death than the Agatston score alone. |
| Blaha et al. [40], 2020 | 66,363 | 54.5 | R | ASX | DLP, HT, DM, SS, FH of CAD | EBCT, CT | NR | 12 | Multivariate regression CPhM | CAC = 0 represents a unique population with favorable all-cause prognosis. Detection of any CAC in young adults could be used to trigger aggressive preventive interventions. |
| Dudum et al [31], 2019 | 14,169 | 48.1 | R | ASX | DLP, HT, DM, SS | CT | C-speed scanner GE Imatron, 4 slice MDCT scanner Siemens, GE 64 slice lightspeed | 11.6 | KMA, unvariate CPhM, ROC curves | CAC scoring was a reliable predictor of all-cause, CVD, and CHD mortality. |
| Lahti et al. [47], 2019 | 28,147 | 58.3 | R | ASX | DLP, HT, DM, SS, FH of CAD, BMI | CT, EBCT | 64 slice GE | NR | Regression CPhM | The presence and high burden of left main CAC are independently associated with a 20–30% greater hazard for cardiovascular and total mortality in asymptomatic adults. |
| Orimoloye et al. [17], 2018 | 42,224 | 54.7 | P | ASX | DLP, HT, DM, SS, FH of CAD | EBCT, CT | NR | 11.7 | KMA, multivariate CPhM, Fine and Gray proportional subhazards model | CAC predicts all-cause and CVD mortality in all studied race/ethnicity groups, including Asians and Hispanics, who may be poorly represented by the Pooled Cohort Equations. |
| Cho et al. [48], 2018 | 1226 | 58 | P | ASX | DLP, HT, DM, SS, FH of CAD | CT | CT 64 slices or greater | 5.9 ± 1.2 | KMA, regression CPhM | CCTA does not offer added value when CCTA findings were added to model RF + CACS at 6 years of follow-up. |
| Cho et al. [32], 2017 | 6656 | 59 | P | NR | NR | CT | MDCT 64 rows or greater | 5.1 | KMA, uvariate and multivariate CPhM | Patients with CAC score ≥100 and no coronary luminal narrowing experience death rates similar to those with non-obstructive CAD. |
| Carr et al. [33], 2017 | 5115 | 32 to 56 | P | NR | DLP, HT, DM, SS, FH of CAD, BMI | CT | NR | 12.5 | Regression CPhM | The presence of CAC among individuals aged between 32 and 46 years was associated with increased risk of fatal and nonfatal CHD during 12.5 years of follow-up. |
| Radford et al. [42], 2016 | 5933 | 49.2 | P | NR | DLP, HT, DM, SS, FH of CAD, CFR | EBCT | C-150XP or C-300 models (Siemens); slices of 3 mm thickness were obtained with 2 mm table increments | 7.3 | The Ionckheere-Terpstra nonparametric method; the Wald method, CPhM, Harrell’s c-index | If serial CAC scanning is performed, the latest scan should be used for risk assessment, and in this context, CAC progression provides no additional prognostic information. |
| Lee et al. [39], 2016 | 48,215 | 54.1 | R | ASX | DLP, HT, DM, SS, FH of CAD | CT | Philips Brilliance 256 iCT, Philips Brilliance 40 channel MDCT, Siemens 16-slice Sensation and GE 64-slice Lightspeed,225–400-ms gantry rotation time | 4.4 | KMA, unvariate and multivariate regression CPhM | In asymptomatic Korean adults, the absence of CAC evoked a strong protective effect against ACM as reflected by longer warranty period, when no other RF were present. |
| Kelkar et al. [46], 2016 | 2363 | 55.0 | P | ASX | DLP, HT, DM, SS, FH of CAD | EBCT, CT | NR | 14.6 | Unvariate and multivariate regression CPhM, Harrel C-statistic | CAC effectively identifies high-risk women with a low-intermediate risk factor burden. |
| Knapper et al. [41], 2016 | 9715 | 40 to 70 | P | ASX | DLP, HT, DM, SS | EBCT, CT | NR | 14.6 | Unvariate and multivariate regression CPhM | For younger and lower-risk FH cohorts, CAC screening did not provide additive prognostic information beyond that of the traditional cardiac risk factors. |
| Han et al. [34], 2015 | 34,386 | 53.8 | R | NR | DLP, HT, DM, SS, FH of CAD, BMI | CT | Philips Brilliance 256 iCT, Philips Brilliance 40 channel multi-detector CT, Siemens 16-slice Sensation, and GE 64-slice Lightspeed | 4.9 | KMA, regression CPhM | In an asymptomatic Korean population, CACS improved prediction of all-cause mortality over and above that of a conventional risk tool. |
| Valenti et al. [38], 2015 | 9715 | 53.4 | P | ASX | DLP, HT, DM, SS, FH of CAD, BMI | EBCT | C-100 or C-150 Ultrafast CT GE Imatron, slice thickness of 3 mm, slices = 40, using a 100 ms/slice scanning time | 14.6 | Mann–Whitney test, multivariate regression CPhM, AUC analysis | In individuals considered at high risk by clinical risk scores, a CAC score of O confers better survival than in individuals at low-to-intermediate risk but with any CAC score. |
| Shaw et al. [36], 2015 | 9715 | 40 to 80 | R | ASX | DLP, HT, DM, SS, FH of CAD | EBCT, CT | NR | 14.6 | Univariable and multivariable Cox regression model, Hosmer–Lemeshow test | The extent of CAC accurately predicts 15-year mortality in a large cohort of asymptomatic patients. |
| Patel et al. [37], 2014 | 44,052 | 60 | P | ASX | DLP, HT, DM, SS, FH of CAD, BMI | EBCT | C-100 or C-150 Ultrafast CT GE Imatron, slice thickness of 3 mm, slices= 40, using a 100 ms/slice scanning time | 5.6 ± 2.6 | KMA CPhRM | Increasing calcified plaque in coronary arteries continued to predict a graded decrease in survival among patients with extensive Agatston score > 1000 with no apparent upper threshold. |
| Graham et al. [43], 2012 | 44,052 | 55 | P | ASX | DLP, HT, DM, SS, FH of CAD, BMI | EBCT | NR | 5.6 ± 2.6 | KMA, regression CPhM | Addition of CAC scores contributed significantly to predicting mortality in addition to only traditional risk factors alone among those with and without hypertension. |
| Mcevoy et al. [45], 2012 | 44,042 | 54 | R | ASX | DLP, HT, DM, SS, FH of CAD, BMI | EBCT | C-100 or 150 Ultrafast CT GE | 5.6 ± 2.6 | KMA, regression CPhM | Smokers with any CAC had significantly higher mortality than smokers without CAC. |
| Nasir et al. [35], 2012 | 44,052 | 54 | P | ASX | DLP, HT, DM, SS, FH of CAD, BMI | EBCT | C-100 or a C-150 Ultrafast CT GE, slice thickness of 3 mm, slices = 40, 100 ms/slice scanning time | 5.6 ± 2.6 | KMA, regression CPhM | Individuals without RFs but elevated CAC have a substantially higher event rates than those who have multiple RFs but no CAC; these findings challenge the exclusive use of traditional risk assessment algorithms for guiding the intensity of primary prevention therapies. |
| Shemesh et al. [44], 2011 | 423 | 64 | R | ASX | DLP, HT, DM, SS, FH of CAD, left ventricular hypertrophy | CT | Dual detector spiral CT without electrocardiogram gating | 14 ± 0.5 | Mann–Whitney test, CPhM, C-index | CAC is associated with long-term mortality in asymptomatic hypertensive adults. |
| Author, Year | N. of Patients | Mean Age (Years) | Study Design (P/R) | Pts | Risk Factors | Imaging | Scan Details | Follow-Up (Years) | Statistical Analysis | Main Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Shaik et al. [52], 2019 | 25,663 | 55.27 | P | ASX DM, not DM | DLP, HT, DM, SS, FH of CAD | EBCT, CT | C-150 XL Ultrafast CT GE, MDCT 64 slice lightspeed GE, FOV = 35 cm, matrix size = 512 × 512,120 kVp, slice thickness = 3 mm. | 14.7 ± 3.8 | KMA, unvariate and multivariate CPhM | The absence of CAC was associated with very low cardiovascular as well as all-cause mortality events in all subgroups during long-term follow-up. |
| Malik et al. [51], 2017 | 6814 | 62.2 | P | MetS and diabetes | DLP, HT, DM | EBCT, CT | NR | Follow-up, extended to the first occurrence of CE | KMA, regression CPhM | The addition of CAC score to global risk assessment was associated with significantly improved risk classification in those with MetS and diabetes. |
| Palmieri et al. [53], 2017 | 38 | 64 | P | ASX | DLP, HT, DM, SS, FH of CAD | CT | Aquilion 64 multislice scanner Toshiba, slice thickness 0.5 mm, 120 kV and 300–450 mA | 180 days | Chisquare and Fisher’s exact test | On the basis of CAC, in the presence of non-obstructive carotid atherosclerosis, asymptomatic DM may show significantly higher CAD burden than non-DM, even in the absence of inducible myocardial ischemia. |
| Valenti et al. [50], 2016 | 9715 | 53.4 | P | ASX DM and not DM | DLP, HT, DM, SS, FH of CAD | EBCT | C-100 or C-150 Ultrafast CT GE Imatron, slice thickness = 3 mm, slices = 40, using a 100 ms/slice scanning time | 15 | Mann–Whitney test, multivariate regression CPhM, KMA | CAC = 0 is associated with a favorable 5-year prognosis for asymptomatic diabetic and nondiabetic individuals. |
| Faustino et al. [9], 2014 | 85 | 60 | P | ASX DM type 2 | DLP, HT, DM, SS, FH of CAD | CT | CACS: 8 × 3 mm collimation, 55 mAs, 120 kV, 3 mm width. CTA: 16 × 0.75 mm collimation, 400 ms gantry rotation, pitch = 0.298, 120 kV, 600–800 mAs | 48 months | Cox regression (method forward conditional), ROC curve, AUC analysis | CS showed great value in T2DP risk stratification, and its prognostic value was further enhanced by CTA data. |
| Author, Year | N. of Patients | Mean Age (Years) | Study Design (P/R) | Pts | Risk Factors | Imaging | Scan Details | Follow-Up (Years) | Statistical Analysis | Main Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Huang et al. [54], 2019 | 1876 | 58.0 | R | ASX | DLP, HT, DM, SS, FH of CAD, BMI | CT, SPECT | CT: High-Definition XT GE, 40/48 slices, 2.5 mm section thickness; 120 kV,125 mA; SPECT: triple-head camera using a low-energy, high-resolution, parallel-hole collimator with a rotation in a continuous mode | 28.4 ± 9.1 | KMSA, regression CPhM | The authors support adding a CACS testing in addition to SPECT in asymptomatic patients to better define the risk of cardiac events during follow-up. |
| Chang et al. [55], 2015 | 988 | 57.5 | P | ASX or SX | DLP, HT, DM, SS, FH of CAD | EBCT, ETT, SPECT | Imatron C-150 | 6.9 | KMA, unvariate CPhM, AUC, global chi-squared | CACS as a first-line test over ETT or SPECT for accurability assessing long-term risk in such patients. |
| Havel et al. [56], 2015 | 77 | 59.5 | P | 35 DM patients; there was a history of previous MI in 6 patients | NR | SPECT, CACS FROM PET/TC | PET/TC Biograph 16 Siemens | 26.4 months | KMA, CPhM | This study suggests that combined evaluation of MPI and CAC can predict the outcome in ESRD individuals, while severe perfusion abnormality on gated-SPET and high CAC score ≥ 1000 are predictors of future cardiac events. |
| Author, Year | N. of Patients | Mean Age (Years) | Study Design (P/R) | Pts | Risk Factors | Imaging | Scan Details | Follow-Up (Years) | Statistical Analysis | Main Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Serra et al. [57], 2019 | 266 | 55.4 | P | ASX | HT, HCL, DM, serum C reactive protein | CT | 16-slice MDCT Philips | >10 | KMA, the Mantel–Haenszel test | CTA and CCS assessments had a higher OR than that associated with assessments of patients at intermediate risk using the SCORE algorithm. |
| Choi et al. [61], 2016 | 25,972 | 53.7 | R | ASX | DLP, HT, DM | CT | Philips brilliance 256 iCT, Philips 40 channel multidetector, Siemens 16 slice sensation, GE 64 slice lightspeed with 225–400 ms gantry rotation | 5.5 | CPhM | The effect of high CACS on all-cause mortality is lessened by good exercise capacity in the asymptomatic population. |
| Dikic et al. [58], 2015 | 200 | 57.7 | P | 101 ASX with DM and 99 ASX without DM | DLP, HT, DM, SS, FH of CAD | CT | Somatom Sensation 64 Siemens; 100 ms scan time, 3 mm slice tickness, 40–45 slices | 1 | KMA, unvariate CPhM, AUC | DM patients with CACS > 200 and CFVR < 2 had the worst outcome. |
| Von Sholten et al. [20], 2015 | 200 | 54 to 65 | P | ASX with type 2 DM | DLP, HT, DM, SS, FH of CAD | CT | 16 MDCT Philips, slice thickness 3 mm | 6.4 | Mann–Whitney µ test, KMA; CPhM | In patients with type 2 diabetes and microalbuminuria but without known coronary artery disease, NT-proBNP and CAC were strongly associated with fatal and nonfatal CVD, as well as with mortality. |
| Park et al. [59], 2013 | 5182 | 53 | R | ASX | DLP, HT, DM, SS, FH of CAD, BMI | CT | 64 slice Brilliance Philips, 64 × 0.625 mm section collimation, 420 ms rotation time, 120 kV, 800 mA | 48 months | KMA, regression CPhM | Biomarkers and imaging parameters of cardiovascular disease, both FRS and degree of coronary artery stenosis, are independent parameters to predict adverse outcome in an asymptomatic population. |
| Rana et al. [60], 2012 | 1286 | 58.6 | P | ASX | HT, HCL, DM, serum C-reactive protein, left ventricular disfunction and fibrinolysis | EBCT, CT | EBCT GE, MDCT Siemens | 4.1 ± 0.4 | Multivariate regression CPhM, Harrell c-statistic and AUC curves | Asymptomatic subjects without known CVD; addition of CAC but not biomarkers substantially improved risk reclassification for future CVD events beyond traditional risk factors. |
| Author, Year | N. of Patients | Mean Age (Years) | Study Design (P/R) | Pts | Risk Factors | Imaging | Scan Details | Follow-Up (Years) | Statistical Analysis | Main Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Moon et al. [62], 2019 | 470 | 75.1 | P | ASX | DLP, HT, DM, SS, FH of CAD, BMI, CACS | CT | 64-slice MDCT Brilliance Philips | 8.2 | KMA, unvariate or multivariate CPhM, C-statistics, categorical and category-free NRI | CCTA showed better long-term prognostic value for MACE than coronary artery calcium score in this asymptomatic older population. |
| Han D. et al. [24], 2018 | 3145 | 56.6 | P | ASX | DLP, HT, DM, SS, FH of CAD, BMI, CACS | CT | 64-slice MDCT | 26 months | Regression CPhM, Harrell’s C-index, categorical NRI | CCTA provides added prognostic value beyond cardiac risk factors and CACS for the prediction of MACE in asymptomatic older adults. |
| Takamura et al. [63], 2017 | 495 | 63.4 | R | ASX | DLP, HT, DM, SS, FH of CAD, BMI | CT | 64 slices MDCT or 320 row area detector CT (ADCT) Toshiba | 716.5 ± 262.6 days | KMA, regression CPhM, ROC and AUC curves, NRI | Although the cardiac event rate was low, the evaluation of CCTA plaque characteristics may provide incremental prognostic value to CACS in asymptomatic patients. |
| Dedic et al. [25], 2016 | 665 | 56 | P/R | ASX | DLP, HT, DM, SS, FH of CAD, BMI | CT | 64-slice MDCT | 3 | KMA, unvariate regression CPhM, NRI | CCTA has incremental prognostic value and risk reclassification benefit beyond CACS in patients without CAD symptoms but with high risk of developing CVD. |
| Halon et al. [68], 2016 | 630 | 63.5 | P | ASX DM type 2 | DLP, HT, DM, SS, FH of CAD, BMI | CT | 64 slice Brilliance CT; Philips; 120 to 140 kV, 500 to 1400 mAs, slice collimation 6490.625-mm, 0.42 s gantry rotation time, pitch 0.2 mm | 6.6 ± 0.6 | KMA, CPhM, ROC curves, NRI | CTA provides additional prognostic information in asymptomatic type 2 diabetics not obtainable from clinical risk assessment and CAC alone. |
| Van den Hoogen et al. [67], 2016 | 525 | 54 | P | DM | DLP, HT, DM, SS, FH of CAD, BMI | CT | 64-slice Aquillon 64 Toshiba or 320 MDCT Aquillon ONE | 5 | KMA, unvariate regression CPhM | Coronary CTA provided prognostic value in diabetic patients without chest pain syndrome. Most importantly, the prognosis of patients with a normal CTA was excellent. |
| Cho et al. [65], 2015 | 3217 | 57 | P | ASX | DLP, HT, DM, SS, FH of CAD, BMI | CT | 64 slice or more MDCT | 2.5 | KMA, continuous NRI | CCTA provides incremental prognostic utility for prediction of mortality and non-fatal myocardial infarction for asymptomatic individuals with moderately high CACS, but not for lower or higher CACS. |
| Hur et al. [70], 2015 | 350 | 64.1 | P | Ischemic stroke patients without chest pain | DLP, HT, DM, SS, FH of CAD, BMI | CT | Somatom Definition Flash Siemens, slice thickness 3 mm, collimation 2 × 64 × 0.6 mm; gantry rotation time 280 ms; 280–380 mAs; 120 kV; pitch 0.2–0.43 | 409 days | KMA, regression CPhM, ROC curve method was used and the integrated area under the curve iAUC, NRI | In ischemic stroke patients without chest pain, CCTA findings of CAD provide additional risk-discrimination over CACS. |
| Plank et al. [64], 2014 | 711 | 54.5 | P | ASX | DLP, HT, DM, SS, FH of CAD, BMI | CT | CACS: 64-slice CT Somatom Sensation Siemens; collimation 64 × 1.5 mm, 120 kV, ECG-gating, slice thickness 3 mm filter kernel B 35, CCTA: 128 Somatom Definition Flash, Siemens, Somatom Sensation 64, Siemens, collimation 2 × 64 × 0.6 mm with a z-flying spot and 64 × 0.6 mm, rotation time 0.28 and 0.33 s | 2.65 | KMA, CPhM, ROC analysis | CAD prevalence by CTA in asymptomatic high-risk patients is high. CCS zero does not exclude CAD. CTA is highly accurate in excluding CAD. |
| Min et al. [69], 2014 | 400 | 60,4 | P | ASX DM | DLP, HT, DM, SS, FH of CAD, BMI | CT | 64-slice CT | 2.4 ± 1.1 | Cox regression analysis | For asymptomatic diabetic individuals, CCTA measures of CAD severity confer incremental risk prediction, discrimination, and reclassification on a per-patient, per-vessel, and per-segment basis. |
| Yoo et al. [66], 2011 | 7515 | 50.1 | R | ASX | DLP, HT, DM, SS, FH of CAD, BMI | CT | 64-slice MDCT Brilliance 64 CACS: 120-Kv, 55 mAs, 2,5 mm scan thickness, CCTA: 64 × 0.625 mm section collimation, 420 ms rotation time, 120 kV and 800 mA | 42 months | Chi-squared test, multiple logistic regression analysis (forward conditional) | CCTA may be useful for risk stratification of coronary artery disease as added value over CACS in selected populations with low CACS who have predictors of significant NCP. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tramontano, L.; Punzo, B.; Clemente, A.; Seitun, S.; Saba, L.; Bossone, E.; Maffei, E.; Cavaliere, C.; Cademartiri, F. Prognostic Value of Coronary Calcium Score in Asymptomatic Individuals: A Systematic Review. J. Clin. Med. 2022, 11, 5842. https://doi.org/10.3390/jcm11195842
Tramontano L, Punzo B, Clemente A, Seitun S, Saba L, Bossone E, Maffei E, Cavaliere C, Cademartiri F. Prognostic Value of Coronary Calcium Score in Asymptomatic Individuals: A Systematic Review. Journal of Clinical Medicine. 2022; 11(19):5842. https://doi.org/10.3390/jcm11195842
Chicago/Turabian StyleTramontano, Liberatore, Bruna Punzo, Alberto Clemente, Sara Seitun, Luca Saba, Eduardo Bossone, Erica Maffei, Carlo Cavaliere, and Filippo Cademartiri. 2022. "Prognostic Value of Coronary Calcium Score in Asymptomatic Individuals: A Systematic Review" Journal of Clinical Medicine 11, no. 19: 5842. https://doi.org/10.3390/jcm11195842
APA StyleTramontano, L., Punzo, B., Clemente, A., Seitun, S., Saba, L., Bossone, E., Maffei, E., Cavaliere, C., & Cademartiri, F. (2022). Prognostic Value of Coronary Calcium Score in Asymptomatic Individuals: A Systematic Review. Journal of Clinical Medicine, 11(19), 5842. https://doi.org/10.3390/jcm11195842









