Laryngeal Cancer Surgery: History and Current Indications of Transoral Laser Microsurgery and Transoral Robotic Surgery
Abstract
1. Introduction
2. Transoral Laser Microsurgery
2.1. The Beginning: Albert Einstein and Colleagues
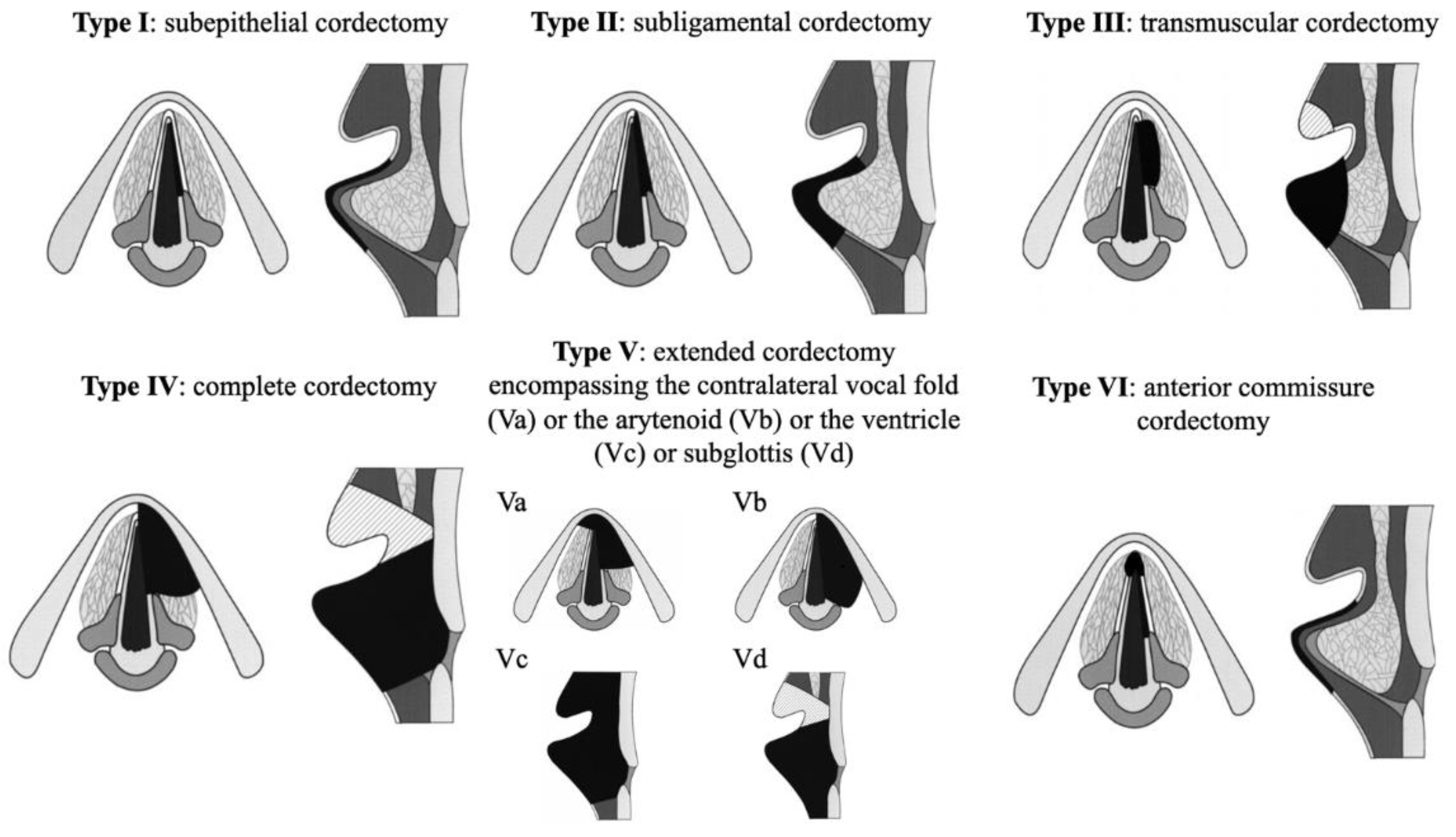
2.2. Concept of TLM
2.3. Indications and Limitations of TLM
2.4. Benefits of TLM
2.5. Barriers to TLM
2.5.1. Learning Curve
2.5.2. Exposure of the Larynx
2.5.3. Anterior Commissure Involvement
2.5.4. Resection Margins
2.6. Voice Quality
3. Transoral Robotic Surgery
3.1. History of Robotic Surgery
3.2. Concept
3.3. Indications and Contraindications
3.3.1. TORS Supraglottic Laryngectomy
3.3.2. TORS-Cordectomy and Total Laryngectomy
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Mendelsohn, A.H.; Remacle, M. Transoral robotic surgery for laryngeal cancer. Curr. Opin. Otolaryngol. Head Neck Surg. 2015, 23, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Hans, S.; Crevier-Buchman, L.; Circiu, M.; Idrissi, Y.C.; Distinguin, L.; de Mones, E.; Brasnu, D.; Lechien, J.R. Oncological and Surgical Outcomes of Patients Treated by Transoral CO2 Laser Cordectomy for Early-Stage Glottic Squamous Cell Carcinoma: A Ret-rospective Chart Review. Ear Nose Throat J. 2021, 100 (Suppl. 1), 33S–37S. [Google Scholar] [CrossRef] [PubMed]
- Strong, M.S.; Jako, G.J. Laser surgery in the larynx. Early clinical experience with continuous CO2 laser. Ann. Otol. Rhinol. Laryngol. 1972, 81, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Lindholm, C.E.; Elner, A. Transoral laser surgery of laryngeal carcinomas. State of the art in Sweden. Adv. Otorhinolaryngol. 1995, 49, 250–253. [Google Scholar]
- Shapshay, S.M.; Hybels, R.L.; Bohigian, R.K. Laser Excision of Early Vocal Cord Carcinoma: Indications, Limitations, and Precautions. Ann. Otol. Rhinol. Laryngol. 1990, 99, 46–50. [Google Scholar] [CrossRef]
- Myers, E.N.; Wagner, R.L.; Johnson, J.T. Microlaryngoscopic Surgery for T1 Glottic Lesions: A Cost-Effective Option. Ann. Otol. Rhinol. Laryngol. 1994, 103, 28–30. [Google Scholar] [CrossRef]
- Eckel, H.E.; Thumfart, W.F. Laser Surgery for the Treatment of Larynx Carcinomas: Indications, Techniques, and Preliminary Results. Ann. Otol. Rhinol. Laryngol. 1992, 101 Pt 1, 113–118. [Google Scholar] [CrossRef]
- Steiner, W. Results of curative laser microsurgery of laryngeal carcinomas. Am. J. Otolaryngol. 1993, 14, 116–121. [Google Scholar] [CrossRef]
- Remacle, M.; Eckel, H.E.; Antonelli, A.; Brasnu, D.; Chevalier, D.; Friedrich, G.; Olofsson, J.; Rudert, H.H.; Thumfart, W.; de Vincentiis, M.; et al. Endoscopic cordectomy. A proposal for a classification by the Working Committee, European Laryngological Society. Eur. Arch. Otorhinolaryngol. 2000, 257, 227–231. [Google Scholar] [CrossRef]
- Remacle, M.; Van Haverbeke, C.; Eckel, H.; Bradley, P.; Chevalier, D.; Djukic, V.; de Vicentiis, M.; Friedrich, G.; Olofsson, J.; Peretti, G.; et al. Proposal for revision of the European Laryngological Society classification of endoscopic cordectomies. Eur. Arch. Otorhinolaryngol. 2007, 264, 709. [Google Scholar] [CrossRef]
- Peretti, G.; Piazza, C.; Mora, F.; Garofolo, S.; Guastini, L. Reasonable limits for transoral laser microsurgery in laryngeal cancer. Curr. Opin. Otolaryngol. Head Neck Surg. 2016, 24, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Day, A.T.; Sinha, P.; Nussenbaum, B.; Kallogjeri, R.; Haughey, B.H. Management of primary T1-T4 glottic squamous cell carcinoma by transoral laser microsurgery. Laryngoscope 2016, 127, 597–604. [Google Scholar] [CrossRef]
- Remacle, M.; Hantzakos, A.; Eckel, H.; Evrard, A.-S.; Bradley, P.J.; Chevalier, D.; Djukic, V.; de Vincentiis, M.; Friedrich, G.; Olofsson, J.; et al. Endoscopic supraglottic laryngectomy: A proposal for a classification by the working committee on nomenclature, European Laryngological Society. Eur. Arch. Otorhinolaryngol. 2009, 266, 993–998. [Google Scholar] [CrossRef]
- Weiss, B.G.; Ihler, F.; Wolff, H.A.; Schneider, S.; Canis, M.; Steiner, W.; Welz, C. Transoral laser microsurgery for treatment for hypopharyngeal cancer in 211 patients. Head Neck 2017, 39, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Canis, M.; Martin, A.; Ihler, F.; Wolff, H.A.; Kron, M.; Matthias, C.; Steiner, W. Results of transoral laser microsurgery for supraglottic carcinoma in 277 patients. Eur. Arch. Otorhinolaryngol. 2013, 270, 2315–2326. [Google Scholar] [CrossRef] [PubMed]
- Canis, M.; Ihler, F.; Martin, A.; Wolff, H.A.; Matthias, C.; Steiner, W. Organ preservation in T4a laryngeal cancer: Is transoral laser microsurgery an option? Eur. Arch. Otorhinolaryngol. 2013, 270, 2719–2727. [Google Scholar] [CrossRef]
- Hoffmann, C.; Cornu, N.; Hans, S.; Sadoughi, B.; Badoual, C.; Brasnu, D. Early glottic cancer involving the anterior commissure treated by transoral laser cordectomy. Laryngoscope 2015, 126, 1817–1822. [Google Scholar] [CrossRef]
- Breda, E.; Catarino, R.; Monteiro, E. Transoral laser microsurgery for laryngeal carcinoma: Survival analysis in a hospital-based population. Head Neck 2014, 37, 1181–1186. [Google Scholar] [CrossRef]
- Lee, H.S.; Chun, B.-G.; Kim, S.W.; Kim, S.T.; Oh, J.H.; Hong, J.C.; Lee, K.D. Transoral laser microsurgery for early glottic cancer as one-stage single-modality therapy. Laryngoscope 2013, 123, 2670–2674. [Google Scholar] [CrossRef]
- Ambrosch, P.; Fazel, A. Functional organ preservation in laryngeal and hypopharyngeal cancer. GMS Curr. Top. Otorhinolaryngol. Head Neck Surg. 2012, 10, Doc02. [Google Scholar] [CrossRef]
- Vaculik, M.; Mackay, C.A.; Taylor, S.M.; Trites, J.R.B.; Hart, R.D.; Rigby, M.H. Systematic review and meta-analysis of T1 glottic cancer outcomes comparing CO2 transoral laser microsurgery and radiotherapy. J. Otolaryngol. Head Neck Surg. 2019, 48, 44. [Google Scholar] [CrossRef] [PubMed]
- Karatzanis, A.D.; Psychogios, G.; Zenk, J.; Waldfahrer, F.; Hornung, J.; Velegrakis, G.A.; Iro, H. Comparison among different available surgical approaches in T1 glottic cancer. Laryngoscope 2009, 119, 1704–1708. [Google Scholar] [CrossRef] [PubMed]
- Vilaseca, I.; Bernal-Sprekelsen, M.; Him, R.; Mandry, A.; Lehrer, E.; Blanch, J.L. Prognostic factors of quality of life after transoral laser microsurgery for laryngeal cancer. Eur. Arch. Otorhinolaryngol. 2014, 272, 1203–1210. [Google Scholar] [CrossRef] [PubMed]
- Diaz-De-Cerio, P.; Preciado, J.; Santaolalla, F.; Sanchez-Del-Rey, A. Cost-minimisation and cost-effectiveness analysis comparing transoral CO2 laser cordectomy, laryngofissure cordectomy and radiotherapy for the treatment of T1–2, N0, M0 glottic carcinoma. Eur. Arch. Otorhinolaryngol. 2012, 270, 1181–1188. [Google Scholar] [CrossRef]
- Van Loon, Y.; Hendriksma, M.; Langeveld, T.P.; De Jong, M.A.; De Jong, R.J.B.; Sjogren, E.V. Treatment Preferences in Patients With Early Glottic Cancer. Ann. Otol. Rhinol. Laryngol. 2017, 127, 139–145. [Google Scholar] [CrossRef]
- Peretti, G.; Piazza, C.; Cocco, D.; De Benedetto, L.; Del Bon, F.; De Zinis, L.O.R.; Nicolai, P. Transoral CO2 laser treatment for Tis-T3 glottic cancer: The University of Brescia experience on 595 patients. Head Neck 2009, 32, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Bernal-Sprekelsen, M.; Blanch, J.-L.; Caballero, M.; Vilaseca, I. The learning curve in transoral laser microsurgery for malignant tumors of the larynx and hypopharynx: Parameters for a levelled surgical approach. Eur. Arch. Otorhinolaryngol. 2012, 270, 623–628. [Google Scholar] [CrossRef]
- Piazza, C.; Mangili, S.; Bon, F.D.; Paderno, A.; Grazioli, P.; Barbieri, D.; Perotti, P.; Garofolo, S.; Nicolai, P.; Peretti, G. Preoperative clinical predictors of difficult laryngeal exposure for microlaryngoscopy: The Laryngoscore. Laryngoscope 2014, 124, 2561–2567. [Google Scholar] [CrossRef]
- Incandela, F.; Paderno, A.; Missale, F.; Laborai, A.; Filauro, M.; Mora, F.; Del Bon, F.; Piazza, C.; Peretti, G. Glottic exposure for transoral laser microsurgery: Proposal of a mini-version of the laryngoscore. Laryngoscope 2019, 129, 1617–1622. [Google Scholar] [CrossRef]
- Sjögren, E. Transoral Laser Microsurgery in Early Glottic Lesions. Curr. Otorhinolaryngol. Rep. 2017, 5, 56–68. [Google Scholar] [CrossRef]
- Hoffmann, C.; Hans, S.; Sadouhki, B.; Brasnu, D. Identifying outcome predictors of transoral laser cordectomy for early glottic cancer. Head Neck 2016, 38 (Suppl. 1), E406–E411. [Google Scholar] [CrossRef] [PubMed]
- Blanch, J.L.; Vilaseca, I.; Caballero, M.; Moragas, M.; Berenguer, J.; Bernal-Sprekelsen, M. Outcome of transoral laser microsurgery for T2-T3 tumors growing in the laryngeal anterior commissure. Head Neck 2011, 33, 1252–1259. [Google Scholar] [CrossRef] [PubMed]
- Simo, R.; Bradley, P.; Chevalier, D.; Dikkers, F.; Eckel, H.; Matar, N.; Peretti, G.; Piazza, C.; Remacle, M.; Quer, M. European Laryngological Society: ELS recommendations for the follow-up of patients treated for laryngeal cancer. Eur. Arch. Otorhinolaryngol. 2014, 271, 2469–2479. [Google Scholar] [CrossRef] [PubMed]
- Jumaily, M.; Faraji, F.; Osazuwa-Peters, N.; Walker, R.J.; Ward, G.M. Prognostic significance of surgical margins after transoral laser microsurgery for early-stage glottic squamous cell carcinoma. Oral Oncol. 2019, 97, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Crevier-Buchman, L.; Circiu, M.P.; De Mones, E.; de Pemille, G.V.; Julien-Laferriere, A.; Saussez, S.; Baudouin, R.; Remacle, M.; Hans, S. Voice Quality Outcomes After Transoral CO2 Laser Cordectomy: A Longi-tudinal Prospective Study. Otolaryngol. Head Neck Surg. 2022, 23, 01945998221114762. [Google Scholar] [CrossRef] [PubMed]
- Bolzoni Villaret, A.; Piazza, C.; Redaelli De Zinis, L.O.; Cattaneo, A.; Cocco, D.; Peretti, G. Phonosurgery after endoscopic cordectomies. I. Primary intracordal autologous fat injection after transmuscular resection: Preliminary results. Eur. Arch. Otorhinolaryngol. 2007, 264, 1179–1184. [Google Scholar] [CrossRef]
- Hans, S.; Delas, B.; Gorphe, P.; Ménard, M.; Brasnu, D. Transoral robotic surgery in head and neck cancer. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2012, 129, 32–37. [Google Scholar] [CrossRef]
- Marescaux, J.; Leroy, J.; Gagner, M.; Rubino, F.; Mutter, D.; Vix, M.; Butner, S.E.; Smith, M.K. Transatlantic robot-assisted telesurgery. Nature 2001, 413, 379–380. [Google Scholar] [CrossRef]
- Samalavicius, N.E.; Janusonis, V.; Siaulys, R.; Jasėnas, M.; Deduchovas, O.; Venckus, R.; Ezerskiene, V.; Paskeviciute, R.; Klimaviciute, G. Robotic surgery using Senhance® robotic platform: Single center experience with first 100 cases. J. Robot. Surg. 2019, 14, 371–376. [Google Scholar] [CrossRef]
- Weinstein, G.S.; O’Malley, B.W., Jr.; Snyder, W.; Hockstein, N.G. Transoral robotic surgery: Supraglottic partial laryngectomy. Ann. Otol. Rhinol. Laryngol. 2007, 116, 19–23. [Google Scholar] [CrossRef]
- Solares, C.A.; Strome, M. Transoral robot-assisted CO2 laser supraglottic laryngectomy: Experimental and clinical data. Laryngoscope 2007, 117, 817–820. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Fakhry, N.; Saussez, S.; Chiesa-Estomba, C.-M.; Chekkoury-Idrissi, Y.; Cammaroto, G.; Melkane, A.E.; Barillari, M.R.; Crevier-Buchman, L.; Ayad, T.; et al. Surgical, clinical and functional outcomes of transoral robotic surgery for supraglottic laryngeal cancers: A systematic review. Oral Oncol. 2020, 109, 104848. [Google Scholar] [CrossRef] [PubMed]
- Hans, S.; Hans, S.; Chekkoury-Idrissi, Y.; Chekkoury-Idrissi, Y.; Circiu, M.P.; Circiu, M.P.; Distinguin, L.; Distinguin, L.; Crevier-Buchman, L.; Crevier-Buchman, L.; et al. Surgical, Oncological, and Functional Outcomes of Transoral Robotic Supraglottic Laryngectomy. Laryngoscope 2020, 131, 1060–1065. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, B.W.; Weinstein, G.S.; Hockstein, N.G. Transoral Robotic Surgery (TORS): Glottic Microsurgery in a Canine Model. J. Voice 2006, 20, 263–268. [Google Scholar] [CrossRef]
- Lechien, J.R.; Baudouin, R.; Circiu, M.P.; Chiesa-Estomba, C.M.; Crevier-Buchman, L.; Hans, S. Transoral robotic cordectomy for glottic carcinoma: A rapid review. Eur. Arch. Otorhinolaryngol. 2022, 1–8. [Google Scholar] [CrossRef]
- Remacle, M.; Prasad, V.M.N. Preliminary experience in transoral laryngeal surgery with a flexible robotic system for benign lesions of the vocal folds. Eur. Arch. Otorhinolaryngol. 2018, 275, 761–765. [Google Scholar] [CrossRef]
- Hans, S.; Chebib, E.; Lisan, Q.; Chekkoury-Idrissi, Y.; Distinguin, L.; Circiu, M.P.; Crevier-Buchman, L.; Lechien, J.R. Oncological, Surgical and Functional Outcomes of Transoral Robotic Cordectomy for Early Glottic Carcinoma. J. Voice, 2021; Online ahead of print. [Google Scholar] [CrossRef]
- Smith, R.V.; Schiff, B.A.; Sarta, C.; Hans, S.; Brasnu, D. Transoral robotic total laryngectomy. Laryngoscope 2013, 123, 678–682. [Google Scholar] [CrossRef]
- Dowthwaite, S.; Nichols, A.C.; Yoo, J.; Smith, R.V.; Dhaliwal, S.; Basmaji, J.; Franklin, J.H.; Fung, K. Transoral robotic total laryngectomy: Report of 3 cases. Head Neck 2013, 35, E338–E342. [Google Scholar] [CrossRef]
- Krishnan, G.; Krishnan, S. Transoral Robotic Surgery Total Laryngectomy: Evaluation of Functional and Survival Outcomes in a Retrospective Case Series at a Single Institution. ORL J. Otorhinolaryngol. Relat. Spec. 2017, 79, 191–201. [Google Scholar] [CrossRef]
- Lawson, G.; Mendelsohn, A.; Fakhoury, R.; Van der Vorst, S.; Remacle, M.; Bachy, V.; Delahaut, G. Transoral Robotic Surgery Total Laryngectomy. ORL J. Otorhinolaryngol. Relat. Spec. 2018, 80, 171–177. [Google Scholar] [CrossRef]
- Hans, S.; Chebib, E.; Chekkoury-Idrissi, Y.; Distinguin, L.; Circiu, M.; Vialatte de Pemille, G.; Julien-Laferriere, A.; Crevier-Buchman, L.; Lechien, J.R. Surgical and oncological outcomes of transoral robotic total laryngectomy: A case series. Oral Oncol. 2021, 121, 105511. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hans, S.; Baudouin, R.; Circiu, M.P.; Couineau, F.; Lisan, Q.; Crevier-Buchman, L.; Lechien, J.R. Laryngeal Cancer Surgery: History and Current Indications of Transoral Laser Microsurgery and Transoral Robotic Surgery. J. Clin. Med. 2022, 11, 5769. https://doi.org/10.3390/jcm11195769
Hans S, Baudouin R, Circiu MP, Couineau F, Lisan Q, Crevier-Buchman L, Lechien JR. Laryngeal Cancer Surgery: History and Current Indications of Transoral Laser Microsurgery and Transoral Robotic Surgery. Journal of Clinical Medicine. 2022; 11(19):5769. https://doi.org/10.3390/jcm11195769
Chicago/Turabian StyleHans, Stéphane, Robin Baudouin, Marta P. Circiu, Florent Couineau, Quentin Lisan, Lise Crevier-Buchman, and Jerome R. Lechien. 2022. "Laryngeal Cancer Surgery: History and Current Indications of Transoral Laser Microsurgery and Transoral Robotic Surgery" Journal of Clinical Medicine 11, no. 19: 5769. https://doi.org/10.3390/jcm11195769
APA StyleHans, S., Baudouin, R., Circiu, M. P., Couineau, F., Lisan, Q., Crevier-Buchman, L., & Lechien, J. R. (2022). Laryngeal Cancer Surgery: History and Current Indications of Transoral Laser Microsurgery and Transoral Robotic Surgery. Journal of Clinical Medicine, 11(19), 5769. https://doi.org/10.3390/jcm11195769