Cognitive Function Decline in the Third Trimester of Pregnancy Is Associated with Sleep Fragmentation
Abstract
1. Introduction
1.1. Sleep and Cognition in the Third Trimester of Pregnancy
1.2. Relationship between Pregnancy and Cognitive Function—Review of the Literature
1.3. Sleep and Pregnancy—Review of the Literature
1.4. Memory and Sleep Quality
2. Materials and Methods
3. Instruments and Procedures
3.1. Cognitive Performance
- Wechsler Adult Intelligence Test (The Verbal Comprehension Index; WAIS-III)—The vocabulary subtest from WAIS-III measures expressive vocabulary and verbal knowledge that is purported to be a good estimate of crystallized intelligence and general intelligence. Subjects were expected to verbally define 33 words (nouns, verbs, adjectives, adverbs) from the list. The test was interrupted if the participant gave five consecutive incorrect answers in describing words [32].
- The D2 Test of Attention—a cancellation test of attention and concentration, is a neuropsychological test designed to measure processing speed, rule compliance, and quality of performance, allowing for a neuropsychological estimation of individual attention and concentration performance. Its performance depends on a combination of visual, motor, and attention skills. The test contains 14 lines and participants have 20 s to work on each line in order to cancel out any “d” letter with two marks around the letter. Crucial difficulty in this test is related to distractors, very similar to the target. They are also built with the letters—“d” and “p” with marks, but in another arrangement than the target. Three indices of task performance were computed: concentration performance (CP), defined as the number of ‘hits’ (marked targets) minus the number of distractors, which were marked (errors of commission). The CP score is a measure of processing speed adjusted for errors made. Processed targets (PT), defined as the number of target symbols in the ‘processed’ portion of the test up to and including the last response marked on each screen. It equals the number of ‘hits’ (targets found) plus the number of overlooked targets. The PT score is a measure of processing speed without consideration of accuracy. Accuracy (%), was defined as the total number of errors (errors of omission and commission) by the number of processed targets (PT) and expressing this fraction as a percentage. This score is then reversed so that a high standard score reflects a highly accurate response [33,34].
- The OSPAN task (operational span task)—a modified online version (GEX Immergo, Funds Auxilium Sp. z o.o.) of the operation span (OSPAN) task—measures working memory capacity (WMC) and is closely related to other higher-order intellectual functions. Participants were asked to perform simple mathematical verifications while simultaneously trying to remember a series of letters. After a series of practice trials, participants completed 15 trials ranging from three to seven letters in load. Only trials in which all letters were remembered and recalled in correct order were coded as correct, and this absolute OSPAN score was treated as our individual WMC measure [35,36,37].
3.2. Sleep Quality Measurement
3.3. Psychological Measurement
- Athens Insomnia Scale (AIS)—An eight-item self-reported questionnaire based on the ICD-10 criteria designed for quantitative measurement of severity of insomnia. Each item is rated from 0 (not a problem) to 3 (a very serious problem) with a total score from 0 to 24. The scale is characterized by a very good consistency (Cronbach’s alpha = 0.90) and reliability (test–retest reliability, r2 = 0.92) [41,42]. AIS is one of the most commonly used scales for diagnostic purposes as well as research on the effectiveness of insomnia treatment. The scale was validated in Poland with 8 points as a cut-off score.
- Epworth Sleepiness Scale (ESS)—An eight-item self-reported questionnaire with a range from 0 to 24 points, used to determine the level of daytime sleepiness in populations suffering from a variety of sleep disorders [43]. A score ≥10 is usually considered abnormal, indicating excessive daytime sleepiness (EDS). It was assessed in pregnant women and is characterized by a good consistency (Cronbach’s alpha = 0.8) [44].
- Ford Insomnia Response to Stress Test (FIRST)—A nine-item self-report measure of susceptibility to stress manifested by a deterioration of sleep with four possible answers scored from 1 to 4 points according to the possibility of sleep deterioration after described in items situation. The total score ranges from 9 to 36 [45]. The scale has been tested as reliable for assessing susceptibility to insomnia among women at their early pregnancy [46].
- Beck Depression Inventory (BDI)—A 21-item self-report scale; responses for each item are scored from 0 to 3 depending on severity of symptoms. The score ranges from 0 to 63 and the cut-off point for the Polish population is 12. BDI is used to assess the severity of depressive symptoms with good internal consistency (Cronbach’s alpha = 0.85) [47,48].
- Regenstein Hyperarousal Scale (HS)—A 26-item self-reported scale, responses are scored from 0 to 3 with the total score ranges from 0 to 78 points. HS is used to assess hyperarousal with a good consistency (Cronbach’s alpha = 0.84) and is well correlated with objective measures of alertness [49].
4. Statistical Analysis
4.1. Comparison of Pregnant and Control Women on Cognitive Performance and Sleep Quality
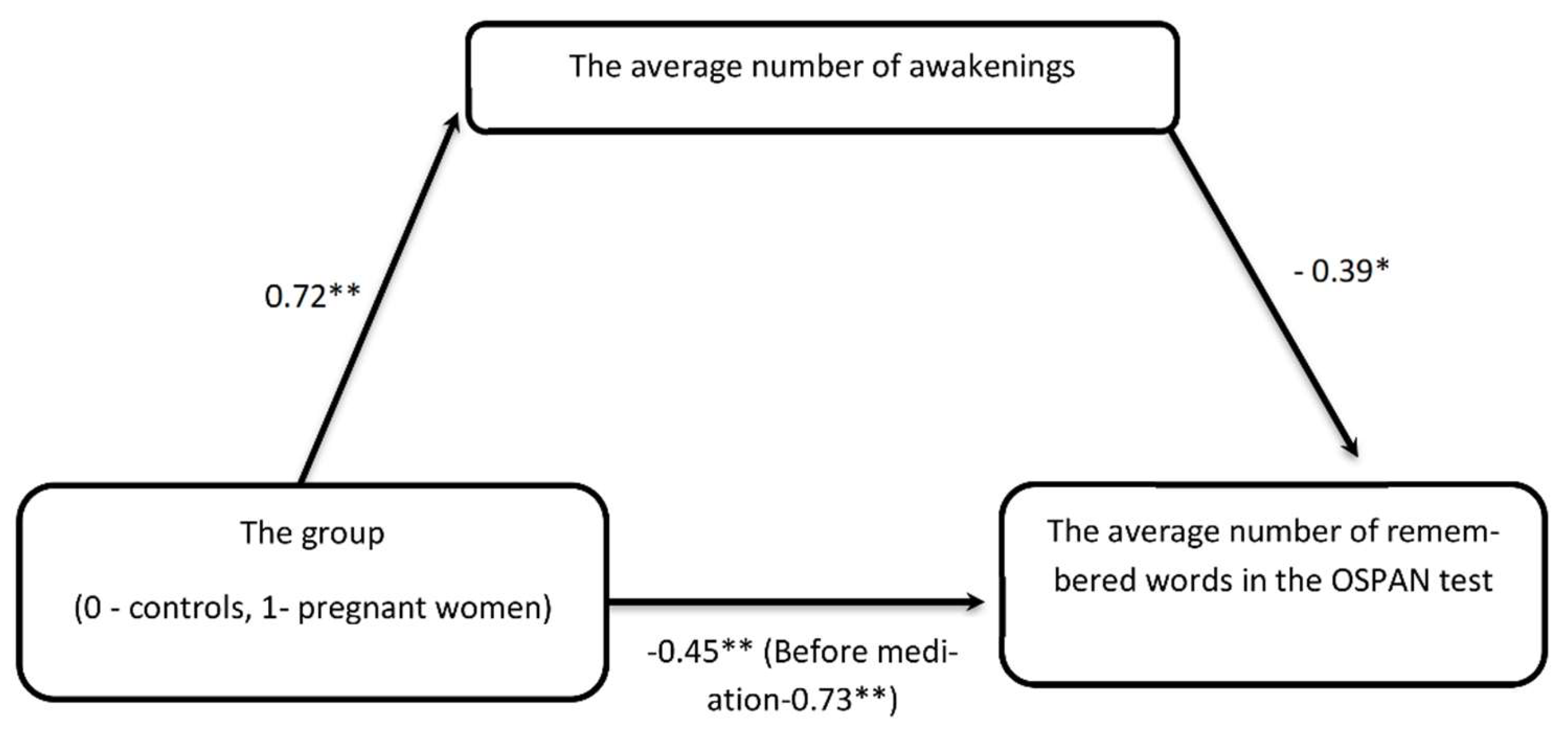
4.2. Quality of Sleep Explains Poor WM in Pregnant Women
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sharp, K.; Brindle, P.M.; Brown, M.W.; Turner, G.M. Memory loss during pregnancy. Br. J. Obstet. Gynaecol. 1993, 100, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Brett, M.; Baxendale, S. Motherhood and memory: A review. Psychoneuroendocrinology 2001, 26, 339–362. [Google Scholar] [CrossRef]
- Neau, J.P.; Texier, B.; Ingrand, P. Sleep and vigilance disorders in pregnancy. Eur. Neurol. 2009, 62, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Kizilirmak, A.; Timur, S.; Kartal, B. Insomnia in pregnancy and factors related to insomnia. Sci. World J. 2012, 2012, 197093. [Google Scholar] [CrossRef] [PubMed]
- Dørheim, S.K.; Bjorvatn, B.; Eberhard-Gran, M. Insomnia and depressive symptoms in late pregnancy: A population-based study. Behav. Sleep Med. 2012, 10, 152–166. [Google Scholar] [CrossRef]
- Lee, K.A.; Zaffke, M.E.; Baratte-Beebe, K. Restless legs syndrome and sleep disturbance during pregnancy: The role of folate and iron. J. Womens Health Gend. Based Med. 2001, 10, 335–341. [Google Scholar] [CrossRef]
- Pien, G.W.; Pack, A.I.; Jackson, N.; Maislin, G.; Macones, G.A.; Schwab, R.J. Risk factors for sleep-disordered breathing in pregnancy. Thorax 2014, 69, 371–377. [Google Scholar] [CrossRef]
- de Groot, R.H.; Vuurman, E.F.; Hornstra, G.; Jolles, J. Differences in cognitive performance during pregnancy and early motherhood. Psychol. Med. 2006, 36, 1023–1032. [Google Scholar] [CrossRef]
- Buckwalter, G.J.; Stanczyk, F.Z.; McCleary, C.A.; Bluestein, B.W.; Buckwalter, D.K.; Ranki, K.P.; Goodwin, T.M. Pregnancy, the postpartum, and steroid hormones: Effects on cognition and mood. Psychoneuroendocrinology 1999, 24, 69–84. [Google Scholar] [CrossRef]
- Rendell, P.G.; Henry, J.D. Prospective-memory functioning is affected during pregnancy and postpartum. J. Clin. Exp. Neuropsychol. 2008, 30, 913–919. [Google Scholar] [CrossRef]
- Farrar, D.; Tuffnell, D.; Neill, J.; Scally, A.; Marshall, K. Assessment of cognitive function across pregnancy using CANTAB: A longitudinal study. Brain Cogn. 2014, 84, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.D.; Rendell, P.G. A review of the impact of pregnancy on memory function. J. Clin. Exp. Neuropsychol. 2007, 29, 793–803. [Google Scholar] [CrossRef] [PubMed]
- Brindle, P.M.; Brown, M.W.; Brown, J.; Griffith, H.B.; Turner, G.M. Objective and subjective memory impairment in pregnancy. Psychol. Med. 1991, 21, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Christensen, H.; Leach, L.S.; Mackinnon, A. Cognition in pregnancy and motherhood: Prospective cohort study. Br. J. Psychiatry 2010, 196, 126–132. [Google Scholar] [CrossRef]
- McDowall, J.; Moriarty, R.Q. Implicit and explicit memory in pregnant women: An analysis of data-driven and conceptually driven processes. J. Exp. Psychol. A 2000, 53, 729–740. [Google Scholar] [CrossRef]
- Onyper, S.V.; Searleman, A.; Thacher, P.V.; Maine, E.E.; Johnson, A.G. Executive functioning and general cognitive ability in pregnant women and matched controls. J. Clin. Exp. Neuropsychol. 2010, 32, 986–995. [Google Scholar] [CrossRef]
- Crawley, R.A.; Dennison, K.; Carter, C. Cognition in pregnancy and the first year post-partum. Psychol. Psychother. 2003, 76, 69–84. [Google Scholar] [CrossRef]
- Roth, R.S.; Geisser, M.E.; Theisen-Goodvich, M. Cognitive complaints are associated with depression, fatigue, female sex, and pain catastrophizing in patients with chronic pain., Dix Pregnancy leads to long-lasting changes in human brain structure. Arch. Phys. Med. Rehabil. 2005, 86, 1147–1154. [Google Scholar] [CrossRef]
- Hoekzema, E.; Barba-Müller, E.; Pozzobon, C.; Picado, M.; Lucco, F.; García-García, D.; Soliva, J.C.; Tobeña, A.; Desco, M.; Crone, E.A. Pregnancy leads to long-lasting changes in human brain structure. Nat. Neurosci. 2017, 20, 287–296. [Google Scholar] [CrossRef]
- Brunner, D.P.; Münch, M.; Biedermann, K.; Huch, R.; Huch, A.; Borbély, A.A. Changes in sleep and sleep electroencephalogram during pregnancy. Sleep 1994, 17, 576–582. [Google Scholar] [CrossRef]
- Orff, H.J.; Meliska, C.J.; Lopez, A.; Martinez, F.; Sorenson, D.; Parry, B.L. Polysomnographic evaluation of sleep quality and quantitative variables in women as a function of mood, reproductive status, and age. Dialogues Clin. Neurosci. 2012, 14, 413–424. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.L.; Barnes, M.; Ellett, L.; Permezel, M.; Jackson, M.; Crowe, S.F.; Aust, N.Z. Decreased sleep efficiency, increased wake after sleep onset and increased cortical arousals in late pregnancy. J. Obstet. Gynaecol. 2011, 51, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.D.; Tucker, M.A.; Stickgold, R.; Wamsley, E.J. Overnight Sleep Enhances Hippocampus-Dependent Aspects of Spatial Memory. Sleep 2013, 36, 1051–1057. [Google Scholar] [CrossRef] [PubMed]
- Diekelmann, S.; Born, J. The memory function of sleep. Nat. Rev. Neurosci. 2010, 11, 114–126. [Google Scholar] [CrossRef] [PubMed]
- Gevers, W.; Deliens, G.; Hoffmann, S.; Notebaert, W.; Peigneux, P. Sleep deprivation selectively disrupts top-down adaptation to cognitive conflict in the Stroop test. J. Sleep Res. 2015, 24, 666–672. [Google Scholar] [CrossRef] [PubMed]
- Cipolli, C.; Mazzetti, M.; Plazzi, G. Sleep-dependent memory consolidation in patients with sleep disorders. Sleep Med. Rev. 2013, 17, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, B.; Candida, M.; Monteiro, S. Working memory dysfunction in insomniac adults: A systematic metanalytical review. Med. Express 2016, 3, 1–8. [Google Scholar] [CrossRef]
- Rauchs, G.H.C.; Bertran, F.; Desgranges, B.; Eustache, F. Sleep and episodic memory: A review of the literature in young healthy subjects and potential links between sleep changes and memory impairment observed during aging and Alzheimer’s disease. Rev. Neurol. 2010, 166, 873–881. [Google Scholar] [CrossRef]
- Bloom, H.G.; Ahmed, I.; Alessi, C.A.; Ancoli-Israel, S.; Buysse, D.J.; Kryger, M.H.; Phillips, B.A.; Thorpy, M.J.; Vitiello, M.V.; Zee, P.C. Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J. Am. Geriatr. Soc. 2009, 57, 761. [Google Scholar] [CrossRef]
- Downe, R.; Bonnet, M.H. Sleep. Performance during frequent sleep disruption.Bonnet MH. Performance and sleepiness as a function of frequency and placement of sleep disruption. Psychophysiology 1987, 10, 354–363. [Google Scholar]
- Dinges, D.F.; Rogers, N.L.; Baynard, M.D. Chronic Sleep Deprivation. In Principles and Practice of Sleep Medicine, 4th ed.; Kryger, M.H., Roth, T., Dement, W.C., Eds.; WB Saunders Company: Philadelphia, PA, USA, 2005; pp. 67–76. [Google Scholar]
- Wechsler, D. Wechsler Adult Intelligence Scale (WAIS-III), 3rd ed.; The Psychological Corporation: San Antonio, TX, USA, 1997. [Google Scholar]
- Brickenkamp, R.; Zillmer, E. The d2 Test of Attention; Hogrefe & Huber: Seattle, WA, USA, 1998. [Google Scholar]
- Dajek, E.R. Polska Standaryzacja Testu D2 Do Badania Uwagi R. Brickenkampa; Wydawnictwo Erda: Warsaw, Poland, 2003. [Google Scholar]
- Unsworth, N.; Heitz, R.P.; Schrock, J.C.; Engle, R.W. An automated version of the operation span task. Behav. Res. Methods 2005, 37, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Engle, R.W.; Tuholski, S.W.; Laughlin, J.E.; Conway, A.R.A. Working memory, short-term memory, and general fluid intelligence: A latent-variable approach. J. Exp. Psychol. 1999, 128, 309–331. [Google Scholar] [CrossRef] [PubMed]
- Conway, A.R.A.; Kane, M.J.; Bunting, M.F.; Hambrick, D.Z.; Wilhelm, O.; Engle, R.W. Working memory span tasks: A methodological review and user’s guide. Psychon. Bull. Rev. 2005, 12, 769–786. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, L.J.; Walsh, C.M.; Traylor, J.; Westin, A.M. Direct comparison of two new actigraphs and polysomnography in children and adolescents. Sleep 2012, 1, 159–166. [Google Scholar] [CrossRef]
- Lichstein, K.L.; Stone, K.C.; Donaldson, J.; Nau, S.D.; Soeffing, J.P.; Murray, D.; Lester, K.W.; Aguillard, R.N. Actigraphy validation with insomnia. Sleep 2006, 29, 232–239. [Google Scholar]
- Sadeh, A.; Sharkey, K.M.; Carskadon, M.A. Activity-based sleep-wake identification: An empirical test of methodological issues. Sleep 1994, 17, 201–207. [Google Scholar] [CrossRef]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. The diagnostic validity of the Athens Insomnia Scale. J. Psychosom. Res. 2003, 55, 263–267. [Google Scholar] [CrossRef]
- Fornal-Pawłowsk, M.; Wołyńczyk-Gmaj, D.; Szelenberger, W. Validation of the Polish version of the Athens Insomnia Scale. Psychiatr. Pol. 2011, 45, 211–221. [Google Scholar]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Sarberg, M.; Bladh, M.; Josefsson, A.; Svanborg, E. Sleepiness and sleep-disordered breathing during pregnancy. Sleep Breath 2016, 20, 1231–1237. [Google Scholar] [CrossRef]
- Drake, C.; Richardson, G.; Roehrs, T.; Scofield, H.; Roth, T. Vulnerability to stress-related sleep disturbance and hyperarousal. Sleep 2004, 27, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Gelaye, B.; Zhong, Q.Y.; Barrios, Y.V.; Drake, C.L.; Williams, M.A. Psychometric Evaluation of the Ford Insomnia Response to Stress Test (FIRST) in Early Pregnancy. J. Clin. Sleep Med. 2016, 12, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.E.; Erbaugh, J.K. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Parnowski, T.; Jernajczyk, W. Inwentarz Depresji Becka w ocenie nastroju osób zdrowych i chorych na choroby afektywne. Psychiatr. Pol. 1977, 11, 417–421. [Google Scholar]
- Regestein, Q.R.; Dambrosia, J.; Hallet, M.; Murawski, B.; Paine, M. Daytime alertness in patients with primary insomnia. Am. J. Psychaitry 1993, 150, 1529–1534. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis Second Edition: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 51, 1173. [Google Scholar] [CrossRef]
- Henry, J.F.; Sherwin, B.B. Hormones and cognitive functioning during late pregnancy and postpartum: A longitudinal study. Behav. Neurosci. 2012, 126, 73–85. [Google Scholar] [CrossRef]
- Szelenberger, W.; Niemcewicz, S. Event-related current density in primary insomnia. Acta Neurobiol. Exp. 2001, 61, 299–308. [Google Scholar]
- Varkevisser, M.; Kerkhof, G.A. Chronic insomnia and performance in a 24-h constant routine study. J. Sleep Res. 2005, 14, 49–59. [Google Scholar] [CrossRef]
- Ballesio, A.; Aquino, M.R.J.V.; Kyle, S.D.; Ferlazzo, F.; Lombardo, C.A. Systematic Review and Exploratory Meta-Analysis. Executive Functions in Insomnia Disorder. Front. Psychol. 2019, 10, 101. [Google Scholar] [CrossRef]
- Siegel, J.M.; Rogawski, M.A. A function for REM sleep: Regulation of noradrenergic receptor sensitivity. Brain Res. 1988, 472, 213–233. [Google Scholar] [CrossRef]
- Born, J.; Rasch, B.; Gais, S. Sleep to remember. Neuroscientist 2006, 12, 410–424. [Google Scholar] [CrossRef]
- Wilson, M.A.; McNaughton, B.L. Reactivation of hippocampal ensemble memories during sleep. Science 1994, 265, 676–679. [Google Scholar] [CrossRef]
- Rasch, B.; Born, J. Maintaining memories by reactivation. Curr. Opin. Neurobiol. 2007, 17, 698–703. [Google Scholar] [PubMed]
- Chee, M.W.; Chuah, L.Y.; Venkatraman, V.; Chan, W.Y.; Philip, P.; Dinges, D.F. Functional imaging of working memory following normal sleep and after 24 and 35 h of sleep deprivation: Correlations of fronto-parietal activation with performance. NeuroImage 2006, 31, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Monroe, L.J. Psychological and physiological differences between good and poor sleepers. J. Abnorm. Psychol. 1967, 72, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Reite, M.; Buysse, D.; Reynolds, C.; Mendelson, W. The use of polysomnography in the evaluation of insomnia. Sleep 1995, 18, 58–70. [Google Scholar] [CrossRef]
- Rosa, R.R.; Bonnet, M.H. Reported chronic insomnia is independent of poor sleep as measured by electroencephalography. Psychosom. Med. 2000, 62, 474–482. [Google Scholar] [CrossRef][Green Version]
| Group | Control | Pregnant | t | |
|---|---|---|---|---|
| OSPAN task | Arithmetic | 89.75 ± 5.5 | 89.81 ± 8.2 | 0.03 * |
| Overall number of remembered letters | 54.25 ± 13.9 | 42.62 ± 14.3 | 2.65 * | |
| OSPAN score (WM span index) | 35.8 ± 18.8 | 19.62 ± 14.6 | 3.08 ** | |
| D2 test | PT | 533.55 ± 54.1 | 493.52 ± 76.4 | 1.94 * |
| Acc (%) | 99.93 | 99.94 | 0.66 | |
| CT | 192.2 ± 44.6 | 176.67 ± 38.4 | 1.19 | |
| Wechsler (Vocabulary) | 43.75 ± 10.15 | 38.62 ± 13.4 | 1.38 | |
| Group | Controls | Pregnant | t |
|---|---|---|---|
| Sleep Efficiency | 0.92 ± 0.002 | 0.87 ± 0.003 | 4.57 *** |
| TTB | 427.17 ± 41.6 | 477.11 ± 45.7 | 3.69 *** |
| TST | 392.07 ± 40.3 | 418.71 ± 47.7 | 2 |
| WASO | 33.84 ± 11.3 | 57.33 ± 13.6 | 5.95 *** |
| Number of awakenings | 12.66 ± 3.7 | 15.78 ± 3.7 | 2.6 *** |
| Avgerage awakenings (time, s) | 2.36 ± 1.3 | 3.74 ± 0.9 | 2.52 *** |
| Group | Controls | Pregnant | t |
|---|---|---|---|
| AIS | 4.75 ± 4.75 | 6.58 ± 3.2 | 1.65 |
| HS | 35.50 ± 7.4 | 35.32 ± 8.0 | 0.81 |
| FIRST | 19.95 ± 5.6 | 24.11 ± 4.8 | 2.49 * |
| EPWORTH | 7.75 ± 4.15 | 9.05 ± 4.6 | 0.93 |
| BDI | 5.25 ± 6.1 | 7.32 ± 5.15 | 1.14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wołyńczyk-Gmaj, D.; Majewska, A.; Bramorska, A.; Różańska-Walędziak, A.; Ziemka, S.; Brzezicka, A.; Gmaj, B.; Czajkowski, K.; Wojnar, M. Cognitive Function Decline in the Third Trimester of Pregnancy Is Associated with Sleep Fragmentation. J. Clin. Med. 2022, 11, 5607. https://doi.org/10.3390/jcm11195607
Wołyńczyk-Gmaj D, Majewska A, Bramorska A, Różańska-Walędziak A, Ziemka S, Brzezicka A, Gmaj B, Czajkowski K, Wojnar M. Cognitive Function Decline in the Third Trimester of Pregnancy Is Associated with Sleep Fragmentation. Journal of Clinical Medicine. 2022; 11(19):5607. https://doi.org/10.3390/jcm11195607
Chicago/Turabian StyleWołyńczyk-Gmaj, Dorota, Aleksandra Majewska, Aleksandra Bramorska, Anna Różańska-Walędziak, Simon Ziemka, Aneta Brzezicka, Bartłomiej Gmaj, Krzysztof Czajkowski, and Marcin Wojnar. 2022. "Cognitive Function Decline in the Third Trimester of Pregnancy Is Associated with Sleep Fragmentation" Journal of Clinical Medicine 11, no. 19: 5607. https://doi.org/10.3390/jcm11195607
APA StyleWołyńczyk-Gmaj, D., Majewska, A., Bramorska, A., Różańska-Walędziak, A., Ziemka, S., Brzezicka, A., Gmaj, B., Czajkowski, K., & Wojnar, M. (2022). Cognitive Function Decline in the Third Trimester of Pregnancy Is Associated with Sleep Fragmentation. Journal of Clinical Medicine, 11(19), 5607. https://doi.org/10.3390/jcm11195607





