The Prognostic Value of Pre-Treatment Circulating Biomarkers of Systemic Inflammation (CRP, dNLR, YKL-40, and IL-6) in Vulnerable Older Patients with Metastatic Colorectal Cancer Receiving Palliative Chemotherapy—The Randomized NORDIC9-Study
Abstract
1. Introduction
2. Patients and Methods
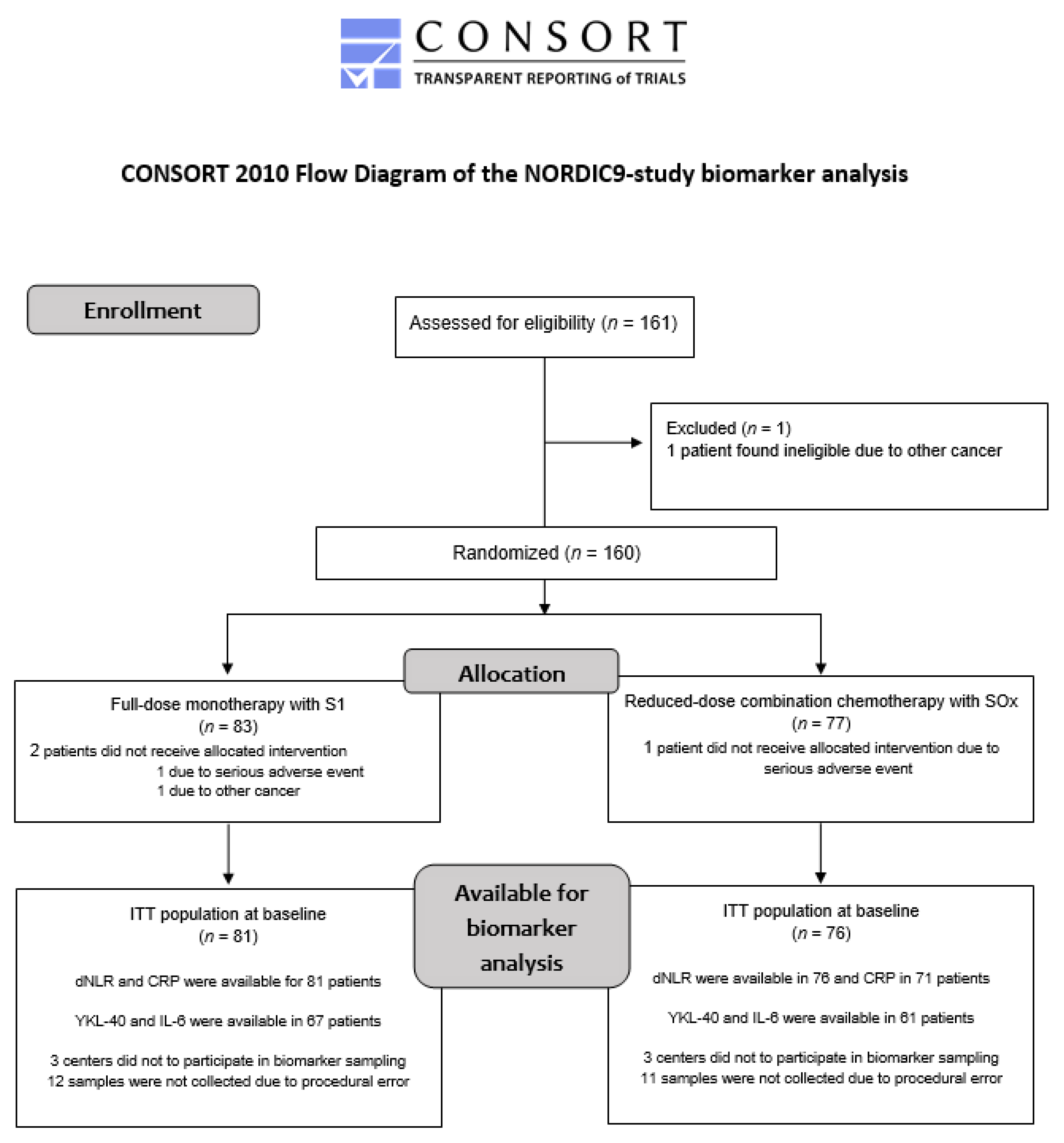
2.1. Study Design and Participants
2.2. Interventions
2.3. Biomarker Analysis
2.4. Covariates
2.5. Statistics
2.6. Survival Analyses
2.7. Multivariable Analyses
2.8. Missing Data
2.9. Sample Size
3. Results
3.1. Patient Population
3.2. Univariate Analyses
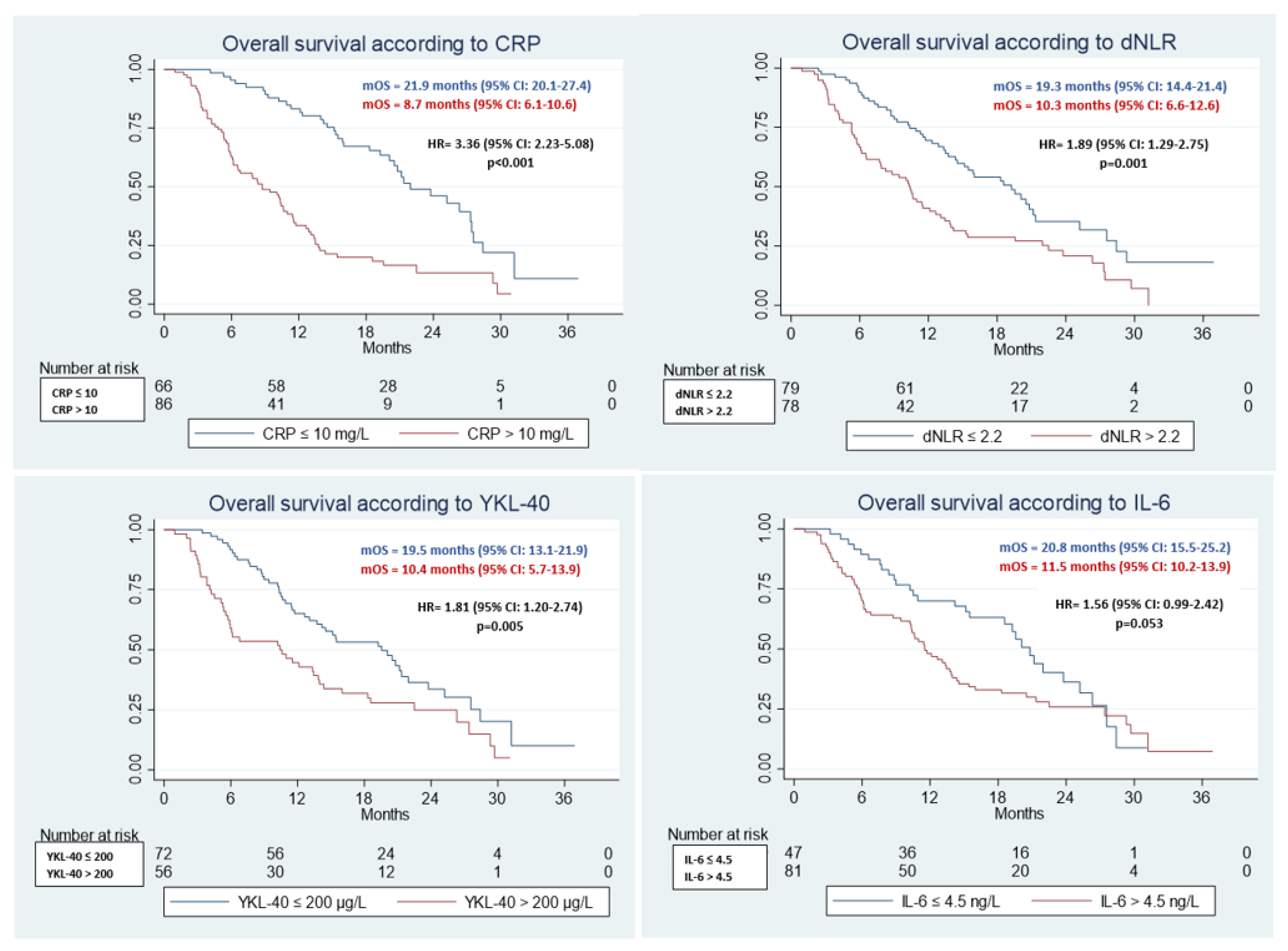
3.2.1. OS
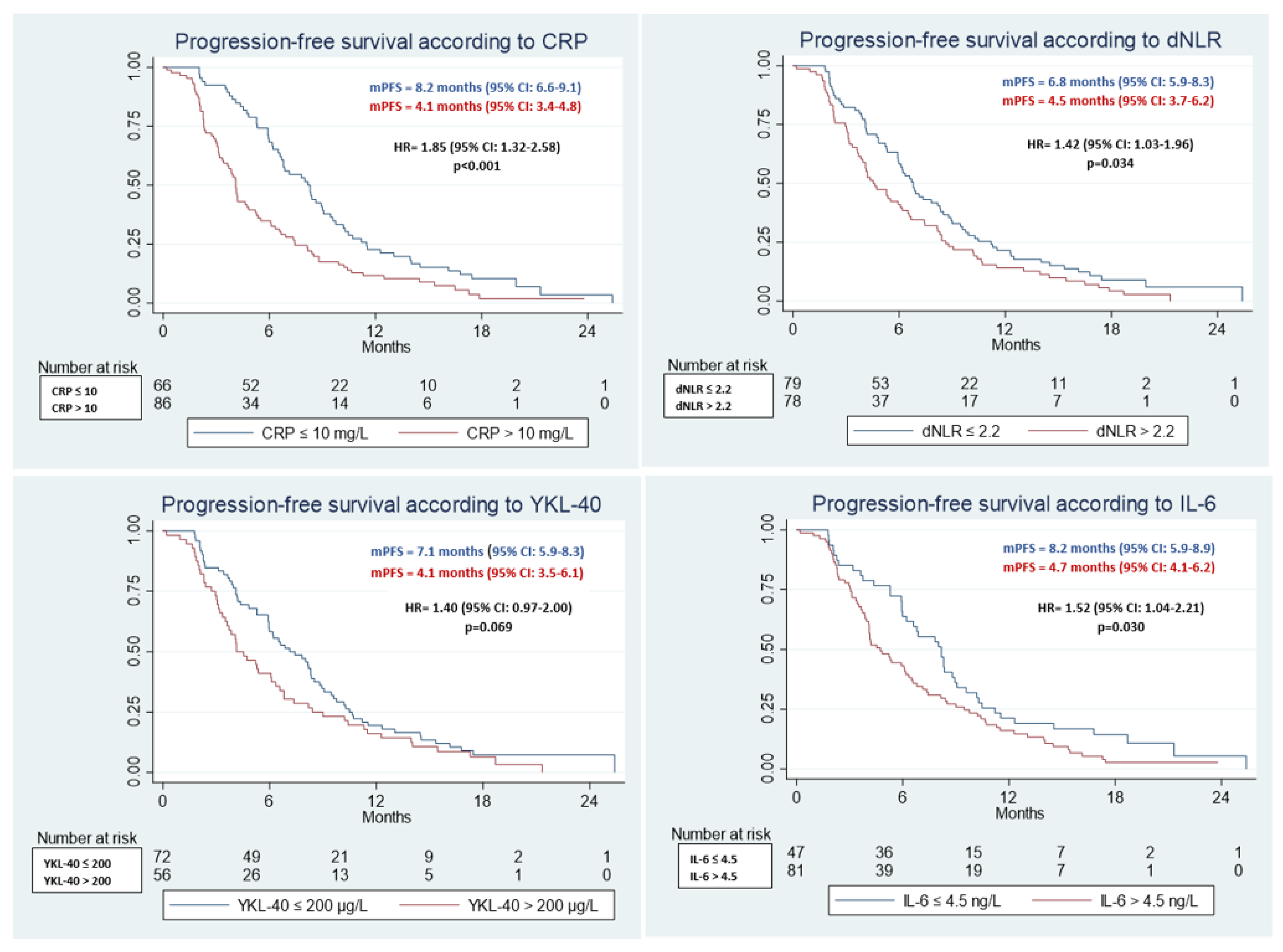
3.2.2. PFS
3.3. Multivariable Analyses
3.3.1. OS
3.3.2. PFS
3.3.3. C-Statistics
4. Discussion
4.1. Explanation, Interpretation
4.2. Comparison to Other Studies
4.3. Methodological Considerations—Strengths and Limitations
4.4. Implication for Clinical Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Douaiher, J.; Ravipati, A.; Grams, B.; Chowdhury, S.; Alatise, O.; Are, C. Colorectal cancer-global burden, trends, and geographical variations. J. Surg. Oncol. 2017, 115, 619–630. [Google Scholar] [CrossRef] [PubMed]
- Yancik, R. Population aging and cancer: A cross-national concern. Cancer J. 2005, 11, 437–441. [Google Scholar] [CrossRef]
- Christensen, K.; Doblhammer, G.; Rau, R.; Vaupel, J.W. Ageing populations: The challenges ahead. Lancet 2009, 374, 1196–1208. [Google Scholar] [CrossRef]
- Sedrak, M.S.; Freedman, R.A.; Cohen, H.J.; Muss, H.B.; Jatoi, A.; Klepin, H.D.; Wildes, T.M.; Le-Rademacher, J.G.; Kimmick, G.G.; Tew, W.P.; et al. Older adult participation in cancer clinical trials: A systematic review of barriers and interventions. CA Cancer J. Clin. 2020, 71, 78–92. [Google Scholar] [CrossRef]
- Sorbye, H.; Pfeiffer, P.; Cavalli-Björkman, N.; Qvortrup, C.; Holsen, M.H.; Wentzel-Larsen, T.; Glimelius, B. Clinical trial enrollment, patient characteristics, and survival differences in prospectively registered metastatic colorectal cancer patients. Cancer 2009, 115, 4679–4687. [Google Scholar] [CrossRef]
- Handforth, C.; Clegg, A.; Young, C.; Simpkins, S.; Seymour, M.T.; Selby, P.J.; Young, J. The prevalence and outcomes of frailty in older cancer patients: A systematic review. Ann. Oncol. 2014, 26, 1091–1101. [Google Scholar] [CrossRef]
- Seymour, M.T.; Thompson, L.C.; Wasan, H.S.; Middleton, G.; Brewster, A.E.; Shepherd, S.F.; O’Mahony, M.S.; Maughan, T.S.; Parmar, M.; Langley, R.E. Chemotherapy options in elderly and frail patients with metastatic colorectal cancer (MRC FOCUS2): An open-label, randomised factorial trial. Lancet 2011, 377, 1749–1759. [Google Scholar] [CrossRef]
- Aparicio, T.; Bouché, O.; Taieb, J.; Maillard, E.; Kirscher, S.; Etienne, P.-L.; Faroux, R.; Akouz, F.K.; El Hajbi, F.; Locher, C.; et al. Bevacizumab+chemotherapy versus chemotherapy alone in elderly patients with untreated metastatic colorectal cancer: A randomized phase II trial—PRODIGE 20 study results. Ann. Oncol. 2017, 29, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Winther, S.B.; Österlund, P.; Berglund, Å.; Glimelius, B.; Qvortrup, C.; Sorbye, H.; Pfeiffer, P. Randomized study comparing full dose monotherapy (S-1 followed by irinotecan) and reduced dose combination therapy (S-1/oxaliplatin followed by S-1/irinotecan) as initial therapy for older patients with metastatic colorectal cancer: NORDIC 9. BMC Cancer 2017, 17, 548. [Google Scholar] [CrossRef]
- Mohile, S.G.; Dale, W.; Somerfield, M.R.; Schonberg, M.A.; Boyd, C.M.; Burhenn, P.; Canin, B.; Cohen, H.J.; Holmes, H.M.; Hopkins, J.O.; et al. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Chemotherapy: ASCO Guideline for Geriatric Oncology. J. Clin. Oncol. 2018, 36, 2326–2347. [Google Scholar] [CrossRef]
- Wildiers, H.; Heeren, P.; Puts, M.; Topinkova, E.; Janssen-Heijnen, M.L.; Extermann, M.; Falandry, C.; Artz, A.; Brain, E.; Colloca, G.; et al. International Society of Geriatric On-cology consensus on geriatric assessment in older patients with cancer. J. Clin. Oncol. 2014, 32, 2595–2603. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, J.M.; Cohen, H.J.; Muss, H.B. Incorporating Biomarkers Into Cancer and Aging Research. J. Clin. Oncol. 2014, 32, 2611–2616. [Google Scholar] [CrossRef] [PubMed]
- Winther, S.B.; Liposits, G.; Skuladottir, H.; Hofsli, E.; Shah, C.H.; Poulsen, L.; Ryg, J.; Osterlund, P.; Berglund, Å.; Qvortrup, C.; et al. Reduced-dose combination chemotherapy (S-1 plus oxaliplatin) versus full-dose monotherapy (S-1) in older vulnerable patients with metastatic colorectal cancer (NOR-DIC9): A randomised, open-label phase 2 trial. Lancet Gastroenterol Hepatol. 2019, 4, 376–388. [Google Scholar] [CrossRef]
- Liposits, G.; Eshøj, H.; Möller, S.; Winther, S.; Skuladottir, H.; Ryg, J.; Hofsli, E.; Shah, C.-H.; Poulsen, L.; Berglund, Å.; et al. Quality of Life in Vulnerable Older Patients with Metastatic Colorectal Cancer Receiving Palliative Chemotherapy—The Randomized NORDIC9-Study. Cancers 2021, 13, 2604. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Kim, J.W.; Hwang, I.G.; Jang, J.S.; Hong, S.; Kim, T.-Y.; Baek, J.Y.; Shin, S.H.; Sun, D.S.; Hong, D.-S.; et al. Serum biomarkers for predicting overall survival and early mortality in older patients with metastatic solid tumors. J. Geriatr. Oncol. 2019, 10, 749–756. [Google Scholar] [CrossRef]
- Nishijima, T.F.; Deal, A.M.; Lund, J.L.; Nyrop, K.A.; Muss, H.B.; Sanoff, H.K. Inflammatory markers and overall survival in older adults with cancer. J. Geriatr. Oncol. 2019, 10, 279–284. [Google Scholar] [CrossRef]
- Nishijima, T.F.; Deal, A.M.; Williams, G.R.; Guerard, E.J.; Nyrop, K.A.; Muss, H.B. Frailty and inflammatory markers in older adults with cancer. Aging 2017, 9, 650–664. [Google Scholar] [CrossRef]
- Lehtomäki, K.; Mustonen, H.; Kellokumpu-Lehtinen, P.-L.; Joensuu, H.; Hermunen, K.; Soveri, L.-M.; Boisen, M.; Dehlendorff, C.; Johansen, J.; Haglund, C.; et al. Lead Time and Prognostic Role of Serum CEA, CA19-9, IL-6, CRP, and YKL-40 after Adjuvant Chemotherapy in Colorectal Cancer. Cancers 2021, 13, 3892. [Google Scholar] [CrossRef]
- Dolin, T.G.; Christensen, I.J.; Johansen, A.Z.; Nielsen, H.J.; Jakobsen, H.L.; Klein, M.F.; Lund, C.M.; Bojesen, S.E.; Nielsen, D.L.; Jensen, B.V.; et al. Pre- and Perioperative Inflammatory Bi-omarkers in Older Patients Resected for Localized Colorectal Cancer: Associations with Complications and Prognosis. Cancers 2021, 14, 161. [Google Scholar] [CrossRef] [PubMed]
- Hermunen, K.; Soveri, L.-M.; Boisen, M.K.; Mustonen, H.K.; Dehlendorff, C.; Haglund, C.H.; Johansen, J.S.; Osterlund, P. Postoperative serum CA19-9, YKL-40, CRP and IL-6 in combination with CEA as prognostic markers for recurrence and survival in colorectal cancer. Acta Oncol. 2020, 59, 1416–1423. [Google Scholar] [CrossRef]
- Thomsen, M.; Kersten, C.; Sorbye, H.; Skovlund, E.; Glimelius, B.; Pfeiffer, P.; Johansen, J.S.; Kure, E.H.; Ikdahl, T.; Tveit, K.M.; et al. Interleukin-6 and C-reactive protein as prog-nostic biomarkers in metastatic colorectal cancer. Oncotarget 2016, 7, 75013–75022. [Google Scholar] [CrossRef] [PubMed]
- Marcos-Pérez, D.; Sánchez-Flores, M.; Proietti, S.; Bonassi, S.; Costa, S.; Teixeira, J.P.; Fernández-Tajes, J.; Pásaro, E.; Laffon, B.; Valdiglesias, V. Association of inflammatory mediators with frailty status in older adults: Results from a systematic review and meta-analysis. GeroScience 2020, 42, 1451–1473. [Google Scholar] [CrossRef] [PubMed]
- Reuben, D.B.; Cheh, A.I.; Harris, T.B.; Ferrucci, L.; Rowe, J.W.; Tracy, R.P.; Seeman, T.E. Peripheral blood markers of inflammation predict mortality and functional decline in high-functioning community-dwelling older persons. J. Am. Geriatr. Soc. 2002, 50, 638–644. [Google Scholar] [CrossRef] [PubMed]
- Soysal, P.; Stubbs, B.; Lucato, P.; Luchini, C.; Solmi, M.; Peluso, R.; Sergi, G.; Isik, A.T.; Manzato, E.; Maggi, S.; et al. Inflammation and frailty in the elderly: A systematic review and meta-analysis. Ageing Res. Rev. 2016, 31, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Harneshaug, M.; Kirkhus, L.; Benth, J.; Grønberg, B.H.; Bergh, S.; Whist, J.E.; Rostoft, S.; Jordhøy, M.S. Screening for frailty among older patients with cancer using blood biomarkers of inflammation. J. Geriatr. Oncol. 2018, 10, 272–278. [Google Scholar] [CrossRef]
- Loh, K.P.; Tooze, J.A.; Nicklas, B.J.; Kritchevsky, S.B.; Williamson, J.D.; Ellis, L.R.; Powell, B.L.; Pardee, T.S.; Goyal, N.G.; Klepin, H.D. Inflammatory biomarkers, geriatric assessment, and treatment outcomes in acute myeloid leukemia. J. Geriatr. Oncol. 2019, 11, 410–416. [Google Scholar] [CrossRef]
- Stojkovic Lalosevic, M.; Pavlovic Markovic, A.; Stankovic, S.; Stojkovic, M.; Dimitrijevic, I.; Radoman Vujacic, I.; Lalic, D.; Milovanovic, T.; Dumic, I.; Krivokapic, Z. Combined Diagnostic Efficacy of Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), and Mean Platelet Volume (MPV) as Biomarkers of Systemic Inflammation in the Diagnosis of Colorectal Cancer. Dis Markers. 2019, 2019, 6036979. [Google Scholar] [CrossRef]
- Absenger, G.; Szkandera, J.; Pichler, M.; Stotz, M.; Arminger, F.; Weissmueller, M.; Schaberl-Moser, R.; Samonigg, H.; Stojakovic, T.; Gerger, A. A derived neutrophil to lymphocyte ratio predicts clinical outcome in stage II and III colon cancer patients. Br. J. Cancer 2013, 109, 395–400. [Google Scholar] [CrossRef]
- Grenader, T.; Nash, S.; Adams, R.; Kaplan, R.S.; Fisher, D.; Maughan, T.; Bridgewater, J. Derived neutrophil lymphocyte ratio is predictive of survival from intermittent therapy in advanced colorectal cancer: A post hoc analysis of the MRC COIN study. Br. J. Cancer 2016, 114, 612–615. [Google Scholar] [CrossRef]
- Proctor, M.J.; McMillan, D.C.; Morrison, D.S.; Fletcher, C.D.; Horgan, P.G.; Clarke, S.J. A derived neutrophil to lymphocyte ratio pre-dicts survival in patients with cancer. Br. J. Cancer 2012, 107, 695–699. [Google Scholar] [CrossRef]
- Zhao, T.; Su, Z.; Li, Y.; Zhang, X.; You, Q. Chitinase-3 like-protein-1 function and its role in diseases. Signal Transduct. Target. Ther. 2020, 5, 201. [Google Scholar] [CrossRef] [PubMed]
- Bojesen, S.E.; Johansen, J.S.; Nordestgaard, B.G. Plasma YKL-40 levels in healthy subjects from the general population. Clin. Chim. Acta 2011, 412, 709–712. [Google Scholar] [CrossRef] [PubMed]
- Bian, B.; Li, L.; Yang, J.; Liu, Y.; Xie, G.; Zheng, Y.; Zeng, L.; Zeng, J.; Shen, L. Prognostic value of YKL-40 in solid tumors: A meta-analysis of 41 cohort studies. Cancer Cell Int. 2019, 19, 259. [Google Scholar] [CrossRef]
- Cintin, C.; Johansen, J.S.; Christensen, I.J.; Price, P.A.; Sørensen, S.; Nielsen, H.J. High serum YKL-40 level after surgery for colorectal carcinoma is related to short survival. Cancer 2002, 95, 267–274. [Google Scholar] [CrossRef]
- Fuksiewicz, M.; Kotowicz, B.; Rutkowski, A.; Achinger-Kawecka, J.; Wagrodzki, M.; Kowalska, M.M. The Assessment of Clinical Usage and Prognostic Value of YKL-40 Serum Levels in Patients with Rectal Cancer Without Distant Metastasis. Technol. Cancer Res. Treat. 2018, 17, 1533033818765209. [Google Scholar] [CrossRef]
- Tarpgaard, L.S.; Guren, T.K.; Glimelius, B.; Christensen, I.J.; Pfeiffer, P.; Kure, E.H.; Sorbye, H.; Ikdahl, T.; Yilmaz, M.; Johansen, J.S.; et al. Plasma YKL-40 in patients with metastatic colorectal cancer treated with first line oxaliplatin-based regimen with or without cetuximab: Results from the Nordic VII study. PLoS ONE 2014, 9, e87746. [Google Scholar] [CrossRef]
- Caruso, C.; Lio, D.; Cavallone, L.; Franceschi, C. Aging, longevity, inflammation, and cancer. Ann. N. Y. Acad. Sci. 2004, 1028, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Campisi, J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J. Gerontol. A Ser. Biol. Sci. Med. Sci. 2014, 69 (Suppl. S1), S4–S9. [Google Scholar] [CrossRef]
- Cesari, M.; Penninx, B.W.; Pahor, M.; Lauretani, F.; Corsi, A.M.; Williams, G.R.; Guralnik, J.M.; Ferrucci, L. Inflammatory markers and physical per-formance in older persons: The InCHIANTI study. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Ferrucci, L.; Harris, T.B.; Guralnik, J.M.; Tracy, R.P.; Corti, M.-C.; Cohen, H.J.; Penninx, B.; Pahor, M.; Wallace, R.; Havlik, R.J. Serum IL-6 level and the development of disability in older persons. J. Am. Geriatr. Soc. 1999, 47, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Ferrucci, L.; Penninx, B.W.; Volpato, S.; Harris, T.B.; Bandeen-Roche, K.; Balfour, J.; Leveille, S.G.; Fried, L.P.; Guralnik, J.M. Change in muscle strength explains accel-erated decline of physical function in older women with high interleukin-6 serum levels. J. Am. Geriatr. Soc. 2002, 50, 1947–1954. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, N.; Kadambi, S.; Lei, L.; Loh, K.P.; Mohamed, M.; Magnuson, A.; Cole, S.; Esparaz, B.T.; Giguere, J.K.; Mohile, S.; et al. Associations of inflammation with frailty in pa-tients with breast cancer aged 50 and over receiving chemotherapy. J. Geriatr. Oncol. 2020, 11, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group. WITHDRAWN: CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2010, 152, 726–732. [Google Scholar] [CrossRef]
- Altman, D.G.; McShane, L.M.; Sauerbrei, W.; Taube, S.E. Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK): Explanation and elaboration. PLoS Med. 2012, 9, e1001216. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tu-mours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- Knudsen, L.S.; Christensen, I.J.; Lottenburger, T.; Svendsen, M.N.; Nielsen, H.J.; Nielsen, L.; Hørslev-Petersen, K.; Jensen, J.E.B.; Kollerup, G.; Johansen, J.S. Pre-analytical and biological varia-bility in circulating interleukin 6 in healthy subjects and patients with rheumatoid arthritis. Biomarkers 2008, 13, 59–78. [Google Scholar] [CrossRef]
- Øgaard, N.; Reinert, T.; Henriksen, T.V.; Frydendahl, A.; Aagaard, E.; Ørntoft, M.-B.W.; Larsen, M.; Knudsen, A.R.; Mortensen, F.V.; Andersen, C.L. Tumour-agnostic circulating tumour DNA analysis for improved recurrence surveillance after resection of colorectal liver metastases: A prospective cohort study. Eur. J. Cancer 2022, 163, 163–176. [Google Scholar] [CrossRef]
- Schraa, S.J.; van Rooijen, K.L.; Koopman, M.; Vink, G.R.; Fijneman, R.J.A. Cell-Free Circulating (Tumor) DNA before Surgery as a Prognostic Factor in Non-Metastatic Colorectal Cancer: A Systematic Review. Cancers 2022, 14, 2218. [Google Scholar] [CrossRef]
- Arnold, D.; Lueza, B.; Douillard, J.-Y.; Peeters, M.; Lenz, H.-J.; Venook, A.; Heinemann, V.; Van Cutsem, E.; Pignon, J.-P.; Tabernero, J.; et al. Prognostic and predictive value of primary tumour side in patients with RAS wild-type metastatic colorectal cancer treated with chemotherapy and EGFR directed antibodies in six randomized trials. Ann. Oncol. 2017, 28, 1713–1729. [Google Scholar] [CrossRef]
- Jin, Z.; Sinicrope, F. Prognostic and Predictive Values of Mismatch Repair Deficiency in Non-Metastatic Colorectal Cancer. Cancers 2021, 13, 300. [Google Scholar] [CrossRef]
- Adolfsson, J.; Steineck, G. Prognostic and treatment-predictive factors-is there a difference? Prostate Cancer Prostatic Dis. 2000, 3, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Italiano, A. Prognostic or predictive? It’s time to get back to definitions! J. Clin. Oncol. 2011, 29, 4718, author reply 9. [Google Scholar] [CrossRef] [PubMed]
- Dell’Aquila, E.; Cremolini, C.; Zeppola, T.; Lonardi, S.; Bergamo, F.; Masi, G.; Stellato, M.; Marmorino, F.; Schirripa, M.; Urbano, F.; et al. Prognostic and predictive role of neutro-phil/lymphocytes ratio in metastatic colorectal cancer: A retrospective analysis of the TRIBE study by GONO. Ann. Oncol. 2018, 29, 924–930. [Google Scholar] [CrossRef] [PubMed]
| Demographic and Baseline Clinical Characteristics Data Presented as Median (Interquartile Range) or n (%) | NORDIC9-Study Population Available for Biomarker Analysis n = 157 | NORDIC9-Study Treatment Arms | |
|---|---|---|---|
| Full-Dose Monotherapy Arm A n = 81 | Reduced-Dose Combination CT Arm B n = 76 | ||
| Age | |||
| Median age in years (IQR) | 78 (75–81) | 78 (76–81) | 77 (75–80) |
| Sex | |||
| Female | 78 (50%) | 40 (49%) | 38 (50%) |
| Male | 79 (50%) | 41 (51%) | 38 (50%) |
| ECOG Performance status | |||
| 0 | 52 (33%) | 29 (36%) | 23 (30%) |
| 1 | 75 (48%) | 37 (46%) | 38 (50%) |
| 2 | 30 (19%) | 15 (18%) | 15 (20%) |
| Surgery for primary tumor | |||
| No | 68 (43%) | 36 (44%) | 32 (42%) |
| Yes | 89 (57%) | 45 (56%) | 44 (58%) |
| Prior adjuvant chemotherapy | |||
| Yes | 29 (18%) | 18 (22%) | 11 (14%) |
| No | 128 (82%) | 63 (78%) | 65 (86%) |
| Number of metastatic sites | |||
| 1–2 | 95 (61%) | 47 (58%) | 38 (63%) |
| ≥3 | 62 (39%) | 34 (42%) | 28 (37%) |
| Self-reported weight loss > 5% within the last 2 months | |||
| No | 122 (78%) | 58 (72%) | 64 (84%) |
| Yes | 35 (22%) | 23 (28%) | 12 (16%) |
| RAS and BRAF status | |||
| RAS and BRAF wild-type | 36 (23%) | 21 (26%) | 15 (20%) |
| RAS or BRAF mutated | 78 (50%) | 39 (48%) | 39 (51%) |
| Unknown | 43 (27%) | 21 (26%) | 22 (29%) |
| Lactate dehydrogenase (U/L) | |||
| ≤255 | 93 (59%) | 44 (54%) | 49 (64%) |
| >255 | 54 (34%) | 29 (36%) | 25 (33%) |
| Unknown | 10 (7%) | 8 (10%) | 2 (3%) |
| Alkaline phosphatase (U/L) | |||
| ≤105 | 90 (57%) | 49 (60%) | 41 (54%) |
| >105 | 66 (42%) | 32 (40%) | 34 (45%) |
| Unknown | 2 (1%) | 0 (0%) | 1 (1%) |
| White blood cells (109/L) | |||
| ≤10 | 113 (72%) | 56 (69%) | 57 (75%) |
| >10 | 44 (28%) | 25 (31%) | 19 (25%) |
| Neutrophil granulocytes (109/L) | |||
| ≤8 | 127 (81%) | 65 (80%) | 62 (82%) |
| >8 | 30 (19%) | 16 (20%) | 14 (18%) |
| C-reactive protein (mg/L) | |||
| ≤10 | 65 (41%) | 27 (33%) | 38 (50%) |
| >10 | 84 (54%) | 53 (65%) | 32 (42%) |
| Unknown | 8 (5%) | 2 (2%) | 6 (8%) |
| Derived neutrophil-to-lymphocyte ratio | |||
| ≤2.2 | 79 (50%) | 41 (50%) | 38 (50%) |
| >2.2 | 78 (50%) | 40 (50%) | 38 (50%) |
| YKL-40 (µg/L) | |||
| ≤200 | 70 (45%) | 32 (40%) | 38 (50%) |
| >200 | 56 (36%) | 34 (42%) | 22 (29%) |
| Unknown | 31 (19%) | 15 (18%) | 16 (21%) |
| Interleukin-6 (ng/L) | |||
| ≤4.5 | 48 (31%) | 21 (26%) | 27 (36%) |
| >4.5 | 78 (50%) | 45 (56%) | 33 (43%) |
| Unknown | 31 (19%) | 15 (18%)) | 16 (21%) |
| Carcinoembryonic antigen (µg/L) | |||
| ≤5 | 30 (19%) | 12 (15%) | 18 (24%) |
| >5 | 121 (77%) | 65 (80%) | 56 (74%) |
| Unknown | 6 (4%) | 4 (5%) | 2 (2%) |
| Baseline Demographic and Clinical Characteristics | n* (%) | CRP Median (mg/L) (IQR) | p-Value | n* (%) | dNLR Median (IQR) | p-Value | n* (%) | YKL-40 Median (µg/L) (IQR) | p-Value | n* (%) | IL-6 Median (ng/L) (IQR) | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Male | 78 | 12 (5–36) | 0.889 | 79 | 2.2 (1.75–2.98) | 0.416 | 68 | 179 (116–323) | 0.371 | 68 | 6.9 (3.6–17.8) | 0.463 |
| Female | 74 | 17 (5–43) | 78 | 2.2 (1.6–2.9) | 60 | 168 (109–268) | 60 | 7.0 (2.6–14.2) | |||||
| ECOG PS | 0–1 | 122 | 11 (5–33) | 0.004 | 127 | 2.1 (1.6–2.6) | 0.004 | 101 | 159 (110–276) | 0.069 | 101 | 6.0 (2.9–12.7) | 0.001 |
| 2 | 30 | 29 (10–80) | 30 | 2.9 (2.0–3.3) | 27 | 224 (143–402) | 27 | 18.1 (4.2–40.2) | |||||
| Treatment arm | S1 | 81 | 19 (6–48) | 0.034 | 81 | 2.2 (1.6–2.9) | 0.864 | 67 | 204 (118–301) | 0.440 | 67 | 7.1 (3.7–17.4) | 0.469 |
| SOx | 71 | 9 (5–33) | 76 | 2.2 (1.7–2.9) | 61 | 163 (98–282) | 61 | 6.6 (2.9–14.7) | |||||
| Resection of primary tumor | Yes | 88 | 10 (4–28) | 0.001 | 89 | 2.0 (1.5–2.5) | 0.003 | 76 | 144 (95–273) | 0.005 | 76 | 5.0 (2.4–13.8) | 0.013 |
| No | 64 | 25 (8–55) | 68 | 2.5 (1.8–3.0) | 52 | 224 (156–318) | 52 | 9.3 (4.1–23.7) | |||||
| Adjuvant chemotherapy | Yes | 29 | 6.0 (4–19) | 0.026 | 29 | 2.0 (1.4–2.5) | 0.058 | 26 | 133 (80–273) | 0.196 | 26 | 4.9 (2.1–9.4) | 0.022 |
| No | 123 | 17 (5–48) | 128 | 2.3 (1.7–3.0) | 102 | 177 (118–296) | 102 | 8.3 (3.4–18.2) | |||||
| Number of metastatic sites | ≤2 | 92 | 10.0 (4–28) | 0.001 | 95 | 2.0 (1.5–2.6) | 0.016 | 79 | 145 (97–263) | 0.003 | 79 | 5.6 (2.8–13.6) | 0.036 |
| ≥3 | 60 | 24 (7–57) | 62 | 2.4 (1.8–3.1) | 49 | 224 (154–345) | 49 | 9.8 (3.9–23.7) | |||||
| Weight loss > 5% in the last 2 months | No | 116 | 11.0 (4–30) | 0.001 | 122 | 2.2 (1.6–2.8) | 0.037 | 97 | 157 (100–272) | 0.006 | 97 | 5.6 (2.7–13.0) | 0.005 |
| Yes | 36 | 32 (12–86) | 35 | 2.5 (2.0–4.0) | 31 | 245 (133–556) | 31 | 15.1 (5.6–34.9) | |||||
| RAS and BRAF mutation status | RAS and BRAF wild type | 34 | 10.5 (5–35) | 0.866 | 36 | 2.2 (1.6–2.6) | 0.846 | 33 | 204 (143–272) | 0.194 | 33 | 8.7 (3.4–14.7) | 0.881 |
| RAS or BRAF mutated | 76 | 14.5 (5–44) | 77 | 2.1 (1.7–2.9) | 62 | 157 (95–296) | 62 | 6.8 (3.8–14.5) | |||||
| Carcinoembryonic-antigen (µg/L) | ≤5 | 29 | 5 (4–17) | 0.012 | 30 | 1.9 (1.5–2.3) | 0.043 | 25 | 149 (80–204) | 0.026 | 25 | 5.0 (2.9–8.7) | 0.029 |
| >5 | 117 | 17 (6–45) | 121 | 2.3 (1.7–2.9) | 98 | 189 (119–301) | 98 | 7.9 (3.4–21.7) | |||||
| Alkaline-phosphatase (U/L) | ≤105 | 85 | 7 (4–21) | <0.001 | 90 | 2.1 (1.6–2.8) | 0.103 | 74 | 139 (95–212) | <0.001 | 74 | 4.6 (2.5–12.2) | 0.002 |
| >105 | 67 | 28 (14–59) | 67 | 2.4 (1.8–3.1) | 54 | 262 (154–556) | 54 | 12.1 (5.1–30.6) | |||||
| Lactate-dehydrogenase (U/L) | ≤255 | 90 | 10 (5–27) | 0.001 | 93 | 2.1 (1.6–2.8) | 0.073 | 80 | 154 (87–258) | 0.009 | 80 | 5.0 (2.6–11.8) | 0.001 |
| >255 | 62 | 27 (7–59) | 64 | 2.4 (1.8–3.1) | 48 | 216 (142–363) | 48 | 12.8 (4.9–27.5) | |||||
| C-reactive protein (mg/L) | ≤10 | NA | NA | NA | 65 | 1.8 (1.5–2.3) | <0.001 | 56 | 119 (80–179) | <0.001 | 56 | 3.3 (2.1–5.4) | <0.001 |
| >10 | 84 | 2.5 (2.0–3.3) | 66 | 248 (155–481) | 66 | 13.9 (7.5–29.5) | |||||||
| Biomarker | n | Progression-Free Survival | Overall Survival | ||||
|---|---|---|---|---|---|---|---|
| Hazard Ratio (95%CI) | p-Value | Harrell’s C (95%CI) | Hazard Ratio (95%CI) | p-Value | Harrell’s C (95%CI) | ||
| CRP (mg/L) | |||||||
| ≤10 | 66 | 1.00 | 0.005 | 0.66 (0.61–0.70) | 1.00 | <0.001 | 0.72 (0.67–0.76) |
| >10 | 86 | 1.65 (1.16–2.34) | 3.40 (2.20–5.26) | ||||
| dNLR | |||||||
| ≤2.2 | 79 | 1.00 | 0.088 | 0.63 (0.58–0.68) | 1.00 | 0.013 | 0.66 (0.60–0.71) |
| >2.2 | 78 | 1.34 (0.96–1.88) | 1.65 (1.11–2.44) | ||||
| YKL-40 (µg/L) | |||||||
| ≤200 | 72 | 1.00 | 0.250 | 0.63 (0.59–0.68) | 1.00 | 0.017 | 0.66 (0.60–0.73) |
| >200 | 56 | 1.26 (0.851.87) | 1.71 (1.10–2.66) | ||||
| IL-6 (ng/L) | |||||||
| ≤4.5 | 47 | 1.00 | 0.024 | 0.64 (0.59–0.69) | 1.00 | 0.044 | 0.65 (0.59–0.71) |
| >4.5 | 81 | 1.58 (1.06–2.35) | 1.60 (1.02–2.52) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liposits, G.; Skuladottir, H.; Ryg, J.; Winther, S.B.; Möller, S.; Hofsli, E.; Shah, C.-H.; Poulsen, L.Ø.; Berglund, Å.; Qvortrup, C.; et al. The Prognostic Value of Pre-Treatment Circulating Biomarkers of Systemic Inflammation (CRP, dNLR, YKL-40, and IL-6) in Vulnerable Older Patients with Metastatic Colorectal Cancer Receiving Palliative Chemotherapy—The Randomized NORDIC9-Study. J. Clin. Med. 2022, 11, 5603. https://doi.org/10.3390/jcm11195603
Liposits G, Skuladottir H, Ryg J, Winther SB, Möller S, Hofsli E, Shah C-H, Poulsen LØ, Berglund Å, Qvortrup C, et al. The Prognostic Value of Pre-Treatment Circulating Biomarkers of Systemic Inflammation (CRP, dNLR, YKL-40, and IL-6) in Vulnerable Older Patients with Metastatic Colorectal Cancer Receiving Palliative Chemotherapy—The Randomized NORDIC9-Study. Journal of Clinical Medicine. 2022; 11(19):5603. https://doi.org/10.3390/jcm11195603
Chicago/Turabian StyleLiposits, Gabor, Halla Skuladottir, Jesper Ryg, Stine Brændegaard Winther, Sören Möller, Eva Hofsli, Carl-Henrik Shah, Laurids Østergaard Poulsen, Åke Berglund, Camilla Qvortrup, and et al. 2022. "The Prognostic Value of Pre-Treatment Circulating Biomarkers of Systemic Inflammation (CRP, dNLR, YKL-40, and IL-6) in Vulnerable Older Patients with Metastatic Colorectal Cancer Receiving Palliative Chemotherapy—The Randomized NORDIC9-Study" Journal of Clinical Medicine 11, no. 19: 5603. https://doi.org/10.3390/jcm11195603
APA StyleLiposits, G., Skuladottir, H., Ryg, J., Winther, S. B., Möller, S., Hofsli, E., Shah, C.-H., Poulsen, L. Ø., Berglund, Å., Qvortrup, C., Osterlund, P., Johansen, J. S., Glimelius, B., Sorbye, H., & Pfeiffer, P. (2022). The Prognostic Value of Pre-Treatment Circulating Biomarkers of Systemic Inflammation (CRP, dNLR, YKL-40, and IL-6) in Vulnerable Older Patients with Metastatic Colorectal Cancer Receiving Palliative Chemotherapy—The Randomized NORDIC9-Study. Journal of Clinical Medicine, 11(19), 5603. https://doi.org/10.3390/jcm11195603







