Influence of Occupation on the Prevalence of Spinal Pain among Physiotherapists and Nurses
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Selection Criteria
2.3. Instruments
- 0–4 points (0–8%): no disability;
- 5–14 points (10–28%): minimal disability;
- 15–24 points (30–48%): moderate disability;
- 25–34 points (50–64%): severe disability;
- 35–50 points (70–100%): extreme suffering, crippled;
- The intensity of spinal pain was measured with the Visual Analogue Scale (VAS).
2.4. Procedure
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Glowinski, S.; Bryndal, A.; Grochulska, A. Prevalence and risk of spinal pain among physiotherapists in Poland. PeerJ 2021, 9, e11715. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: A systematic analysis for the global burden of disease study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef]
- Nordin, N.A.; Leonard, J.H.; Thye, N.C. Work-related injuries among physiotherapists in public hospitals: A Southeast Asian picture. Clinics 2011, 66, 373–378. [Google Scholar] [PubMed]
- Smith, D.R.; Mihashi, M.; Adachi, Y.; Koga, H.; Ishitake, T. A detailed analysis of musculoskeletal disorder risk factors among Japanese nurses. J. Saf. Res. 2006, 37, 195–200. [Google Scholar] [CrossRef]
- Trinkoff, A.M.; Lipscomb, J.A.; Geiger-Brown, J.; Brady, B. Musculoskeletal problems of the neck, shoulder, and back and functional consequences in nurses. Am. J. Ind. Med. 2002, 41, 170–178. [Google Scholar] [CrossRef]
- Long, M.H.; Johnston, V.; Bogossian, F. Work-related upper quadrant musculoskeletal disorders in midwives, nurses and physicians: A systematic review of risk factors and functional consequences. Appl. Ergon. 2012, 43, 455–467. [Google Scholar] [CrossRef]
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann. Transl. Med. 2020, 8, 299. [Google Scholar] [CrossRef]
- Marras, W.S. Occupational low back disorder causation and control. Ergonomics 2000, 43, 880–902. [Google Scholar] [CrossRef]
- Punnett, L.; Prüss-Utün, A.; Nelson, D.I.; Fingerhut, M.A.; Leigh, J.; Tak, S.; Phillips, S. Estimating the global burden of low back pain attributable to combined occupational exposures. Am. J. Ind. Med. 2005, 48, 459–469. [Google Scholar] [CrossRef]
- Spasova, S.; Bouget, D.; Vanhercke, B. Sickpay and Sickness Benefit Schemes in the European Union: Background Report for the Social Protection Committee’s In-Depth Review on Sickness Benefits; European Commission: Brussels, Belgium, 2016. [Google Scholar]
- Thorsen, S.V.; Friborg, C.; Lundstrøm, B.; Kausto, J.; Örnelius, K.; Sundell, T.; Kalstø, A.M.; Thune, O.; Gross, B.-O.; Petersen, H.; et al. Sickness absence in the Nordic countries. Nord. Soc. Stat. Comm. 2015, 59. Available online: http://norden.diva-portal.org/smash/get/diva2:811504/FULLTEXT06.pdf (accessed on 5 August 2022).
- Employee Absenteeism: A Guide to Managing Absence; Ibec International Research Unit: Dublin, Ireland, 2011. Available online: http://www.ibec.ie/IBEC/DFB.nsf/vPages/Research_and_surveys~Employer_issues~ibec-guide-to-managing-absence-16-05-2013/$file/Employee%20Absenteeism%20-%20A%20Guide%20to%20Managing%20Absence.pdf (accessed on 20 August 2022).
- Schneider, E.; Irastorza, X. OSH in Figures: Work-Related Musculoskeletal Diseases in the EU—Facts and Figures; European Agency for Health and Safety Work (OSHA): Luxembourg, 2010; Available online: https://osha.europa.eu/en/tools-andpublications/publications/reports/TERO09009ENC (accessed on 20 August 2022).
- Karlsson, N.E.; Carstensen, J.M.; Gjesadl, S.; Alexanderson, K.A.E. Risk factors for disability pension in a population-based cohort of men and women on long-term sick leave in Sweden. Eur. J. Public Health 2008, 18, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Onishi, T.; Kurimoto, S.; Suzuki, M.; Imaeda, T.; Hirata, H. Work-related musculoskeletal disorders in the upper extremity among the staff of a Japanese university hospital. Int. Arch. Occup. Environ. Health 2014, 87, 547–555. [Google Scholar] [CrossRef] [PubMed]
- Yassi, A.; Lockhart, K. Work-relatedness of low back pain in nursing personnel: A systematic review. Int. J. Occup. Environ. Health 2013, 19, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Fronteira, I.; Ferrinho, P. Do nurses have a different physical health profile? A systematic review of experimental and observational studies on nurses’ physical health. J. Clin. Nurs. 2011, 20, 2404–2424. [Google Scholar] [CrossRef]
- Karahan, A.; Kavs, S. Abbasouglu, A.; Aognan, N. Low back pain: Prevalence and associated risks factors among hospital staff. J. Adv. Nurs. 2009, 65, 516–524. [Google Scholar] [CrossRef]
- Violante, F.S.; Fiori, M.; Fiorentini, C.; Risi, A.; Garagnani, G.; Bonfiglioli, R.; Mattioli, S. Association of psychosocial and individual factors with three different categories of back disorder among nursing staff. J. Occup. Health. 2004, 46, 100–108. [Google Scholar] [CrossRef]
- Bryndal, A.; Glowinski, S.; Majchrzycki, M. Influence of Pregnancy on the Occurrence of Lumbar Spine Pain in Polish Women: A Retrospective Study. J. Pers. Med. 2022, 12, 357. [Google Scholar] [CrossRef]
- Kivimäki, M.; Head, J.; Ferrie, J.E.; Hemingway, H.; Shipley, M.J.; Vahtera, J.; Marmot, M.G. Working while ill as a risk factor for serious coronary events: The Whitehall II study. Am. J. Public Health. 2005, 95, 98–102. [Google Scholar] [CrossRef]
- Corona, G.; Monduzzi, G.; Minerva, M.; Amedei, F.; Franco, G. Individual, ergonomic and psychosocial risk factors affect musculoskeletal disorders in nurses, physiotherapists and VDU users. G. Ital. Med. Lav. Erg. 2004, 26, 201–202. [Google Scholar]
- Ghilan, K.; Al-Taiar, A.; Al Yousfi, N.; Al Zubaidi, R.; Awadh, I.; Al-Obeyed, Z. Low back pain among female nurses in Yemen. Int. J. Occup. Med. Environ. Health 2013, 26, 605–614. [Google Scholar] [CrossRef]
- Bryndal, A.; Majchrzycki, M.; Grochulska, A.; Glowinski, S.; Seremak-Mrozikiewicz, A. Risk Factors Associated with Low Back Pain among A Group of 1510 Pregnant Women. J. Pers. Med. 2020, 10, 51. [Google Scholar] [CrossRef] [PubMed]
- Tinubu, B.M.; Mbada, C.E.; Oyeyemi, A.L.; Fabunmi, A.A. Work-related musculoskeletal disorders among nurses in Ibadan. South-west Nigeria: A cross-sectional survey. BMC Musculoskelet. Disord. 2010, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Moreira, R.F.; Sato, T.O.; Foltran, F.A.; Silva, L.C.; Coury, H.J. Prevalence of musculoskeletal symptoms in hospital nurse technicians and licensed practical nurses: Associations with demographic factors. Braz. J. Phys. Ther. 2014, 18, 323–333. [Google Scholar] [CrossRef]
- Asadi, P.; Monsef Kasmaei, V.; Zia, Z.S.; Zohrevandi, B. The prevalence of low back pain among nurses working in Poursina hospital in Rasht, Iran. J. Emerg. Pract Trauma. 2016, 2, 11–15. [Google Scholar] [CrossRef]
- Misterska, E.; Jankowski, R.; Glowacki, M. Cross-cultural adaptation of the Neck Disability Index and Copenhagen Neck Functional Disability Scale for patients with neck pain due to degenerative and discopathic disorders. Psychometric properties of the Polish versions. BMC Musculoskelet. Disord. 2011, 12, 84. [Google Scholar] [CrossRef] [PubMed]
- Misterska, E.; Jankowski, R.; Glowacki, M. Quebec Back Pain Disability Scale, Low Back Outcome Score and revised Oswestry low back pain disability scale for patients with low back pain due to degenerative disc disease: Evaluation of Polish versions. Spine 2011, 36, 1722–1729. [Google Scholar] [CrossRef] [PubMed]
- Eurofund, Sixth European Working Conditions Survey—Overview report (2017 Update); Publications Office of the European Union, European Foundation for the Improvement of Living and Working Conditions: Luxemburg, 2017. Available online: https://op.europa.eu/en/publication-detail/-/publication/b4f8d4a5-b540-11e7-837e-01aa75ed71a1/language-en (accessed on 10 August 2022).
- Croft, P.R.; Papageorgiou, A.C.; Thomas, E.; Macfarlane, G.J.; Silman, A.J. Short-Term Physical Risk Factors for New Episodes of Low Back Pain: Prospective Evidence from the South Manchester Back Pain Study. Spine 1999, 24, 1561–2556. [Google Scholar] [CrossRef] [PubMed]
- Chiou, W.K.; Wong, M.K.; Lee, Y.H. Epidemiology of low back pain in Chinese nurses. Int. J. Nurs. Stud. 1994, 31, 361–368. [Google Scholar] [CrossRef]
- Terzi, R.; Altin, F. The prevalence of low back pain in hospital staff and its relationship with chronic fatigue syndrome and occupational factors. Agri 2015, 27, 149–154. [Google Scholar]
- Mannion, A.F.; Dolan, P.; Adams, M.A. Psychological questionnaires: Do ‘abnormal’ scores precede or follow first-time low back pain? Spine J. 1996, 21, 2603–2611. [Google Scholar] [CrossRef]
- Losa Iglesias, M.E.; Becerro De Bengoa Vallejo, R.; Salvadores Fuentes, P. Self-reported musculoskeletal disorders in podiatrists at work. Med. Lav. 2011, 102, 502–510. [Google Scholar] [PubMed]
- Bernal, D.; Campos-Serna, J.; Tobias, A.; Vargas-Prada, S.; Benavides, F.G.; Serra, C. Work-related psychosocial risk factors and musculoskeletal disorders in hospital nurses and nursing aides: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2015, 52, 635–648. [Google Scholar] [CrossRef] [PubMed]
- Hafner, N.D.; Milek, D.M.; Fikfak, M.D. Hospital Staff’s Risk of Developing Musculoskeletal Disorders, Especially Low Back Pain. Slov. J. Public Health 2018, 57, 133–139. [Google Scholar] [CrossRef]
- Anap, D.B.; Iyer, C.; Rao, K. Work related musculoskeletal disorders among hospital nurses in rural Maharashtra, India. Int. J. Res. Med. Sci. 2013, 1, 101–107. [Google Scholar] [CrossRef]
- Ellapen, T.J.; Narsigan, S. Work related musculoskeletal disorders among nurses: Systematic review. J. Ergon. 2014, 4, S4-003. [Google Scholar] [CrossRef]
- Stubbs, D.A.; Buckle, P.W.; Hudson, M.P.; Rivers, P.M.; Worringham, C.J. Back pain in the nursing profession. I. Epidemiology and pilot methodology. Ergonomics 1983, 26, 755–765. [Google Scholar] [CrossRef]
- Smedley, J.; Egger, P.; Cooper, C.; Coggon, D. Manual handling activities and risk of low back pain in nurses. Occup. Environ. Med. 1995, 52, 160–163. [Google Scholar] [CrossRef]
- Sikiru, L.; Shmaila, H. Prevalence and risk factors of low back pain among nurses in Africa: Nigerian and Ethiopian specialized hospitals survey study. East Afr. J. Public Health. 2009, 6, 22–25. [Google Scholar] [CrossRef]
- Freimann, T.; Pääsuke, M.; Merisalu, E. Work-related psychosocial factors and mental health problems associated with musculoskeletal pain in nurses: A cross-sectional study. Pain Res. Manag. 2016, 2016, 9361016. [Google Scholar] [CrossRef]
- Skela-Savič, B.; Pesjak, K.; Hvalič-Touzery, S. Low back pain among nurses in Slovenian hospitals: Cross-sectional study. Int. Nurs. Rev. 2017, 64, 544–551. [Google Scholar] [CrossRef]
- Ellis, B.E. Moving and Handling Patients: An evaluation of current training for physiotherapy students. Physiotherapy 1993, 79, 323–326. [Google Scholar] [CrossRef]
- Glover, W. Work-related Strain Injuries in Physiotherapists: Prevalence and prevention of musculoskeletal disorders. Physiotherapy 2002, 88, 364–372. [Google Scholar] [CrossRef]
- Molumphy, M.; Unger, B.; Jensen, G.M.; Lopopolo, R.B. Incidence of work-related low back pain in physical therapists. Phys. Ther. 1985, 65, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Scholey, M.; Hair, M. Back pain in physiotherapists involved in back care education. Ergonomics 1989, 32, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Rugelj, D. Low back pain and other work-related musculoskeletal problems among physiotherapists. Appl. Ergon. 2003, 34, 635–639. [Google Scholar] [CrossRef]
- Bork, B.E.; Cook, T.M.; Rosecrance, J.C.; Engelhardt, K.A.; Thomason, M.E.J.; Wauford, I.J.; Worley, R.K. Work-related musculoskeletal disorders among physical therapists. Phys. Ther. 1996, 76, 827–835. [Google Scholar] [CrossRef]
- Rahimi, F.; Kazemi, K.; Zahednejad, S.; López-López, D.; Calvo-Lobo, C. Prevalence of Work-Related Musculoskeletal Disorders in Iranian Physical Therapists: A Cross-sectional Study. J. Manip. Physiol. Ther. 2018, 41, 503–507. [Google Scholar] [CrossRef]
- Kuijer, P.P.; Verbeek, J.H.; Seidler, A.; Ellegast, R.; Hulshof, C.T.; Frings-Dresen, M.H.; Van der Molen, H.F. Work-relatedness of lumbosacral radiculopathy syndrome. Review and dose-response meta-analysis. Neurology 2018, 91, 558–564. [Google Scholar] [CrossRef]
- Coenen, P.; Gouttebarge, V.; van der Burght, A.S.; van Dieën, J.H.; Frings-Dresen, M.H.; van der Beek, A.J.; Burdorf, A. The effect of lifting during work on low back pain: A health impact assessment based on a meta-analysis. Occup. Environ. Med. 2014, 71, 871–877. [Google Scholar] [CrossRef]
- Mroczek, B.; Łubkowska, W.; Jarno, W.; Jaraczewska, E.; Mierzecki, A. Occurrence and impact of back pain on the quality of life of healthcare workers. Ann. Agric. Environ. Med. 2020, 27, 36–42. [Google Scholar] [CrossRef]
- Jabłońska, R.; Gralik, M.; Królikowska, A.; Haor, B.; Antczak, A. The problem of back pain among nurses of neurology and neurosurgery wards. J. Neurol. Neurosurg. Nurs. 2016, 5, 84–91. [Google Scholar] [CrossRef]
- Kupcewicz, E. Jakość życia pielęgniarek a strategie radzenia sobie ze stresem doświadczanym w środowisku pracy [Quality of life of nurses and strategies for coping with stress experienced in the work environment]. Med. Og. Nauk. Zdr. 2017, 23, 62–67. [Google Scholar] [CrossRef]
- Fidecki, W.; Wysokiński, M.; Ochap, M.; Wrońska, I.; Przylepa, K.; Kulina, D.; Sienkiewicz, Z.; Chruściel, P. Selected aspects of life quality of nurses at neurological wards. J. Neurol. Neurosurg. Nurs. 2016, 5, 151–155. [Google Scholar] [CrossRef]
- Maciuk, M.; Krajewska-Kulak, E.; Klimaszewska, K. Samoocena występowania zespołów bólowych kręgosłupa u zawodowo czynnych pielęgniarek [Self-assessment of low back pain incidence in professionally active nurses]. Probl. Hig. Epidemiol. 2012, 93, 728–738. (In Polish) [Google Scholar]
- Nowotny, J.; Nowotny-Czupryna, O.; Brzęk, A.; Kowalczyk, A.; Czupryna, K. Body posture and syndromes of back pain. Ortop. Traumatol. Rehabil. 2011, 13, 59–71. [Google Scholar] [CrossRef]

| KERRYPNX | Study Population, Total (N = 544) | Physiotherapists (n1 = 240) | Nurses (n2 = 304) | p-Value | |
|---|---|---|---|---|---|
| Sex | Number (% of study population) | Women 462 (84.9%) Men 82 (15.1%) | Women 169 (70.4%) Men 71 (29.6%) | Women 293 (95.8%) Men 11 (4.2%) | |
| Age (categories) | Number (% of study population) | ||||
| 20–29 | 56 (10.3%) | 39 (16.3%) | 17 (5.6%) | ||
| 30–39 | 161 (29.6%) | 109 (45.4%) | 52 (17.1%) | ||
| 40–49 | 130 (23.9%) | 33 (13.8%) | 97 (31.9%) | ||
| ≥50 | 197 (36.2%) | 59 (24.6%) | 138 (45.4%) | ||
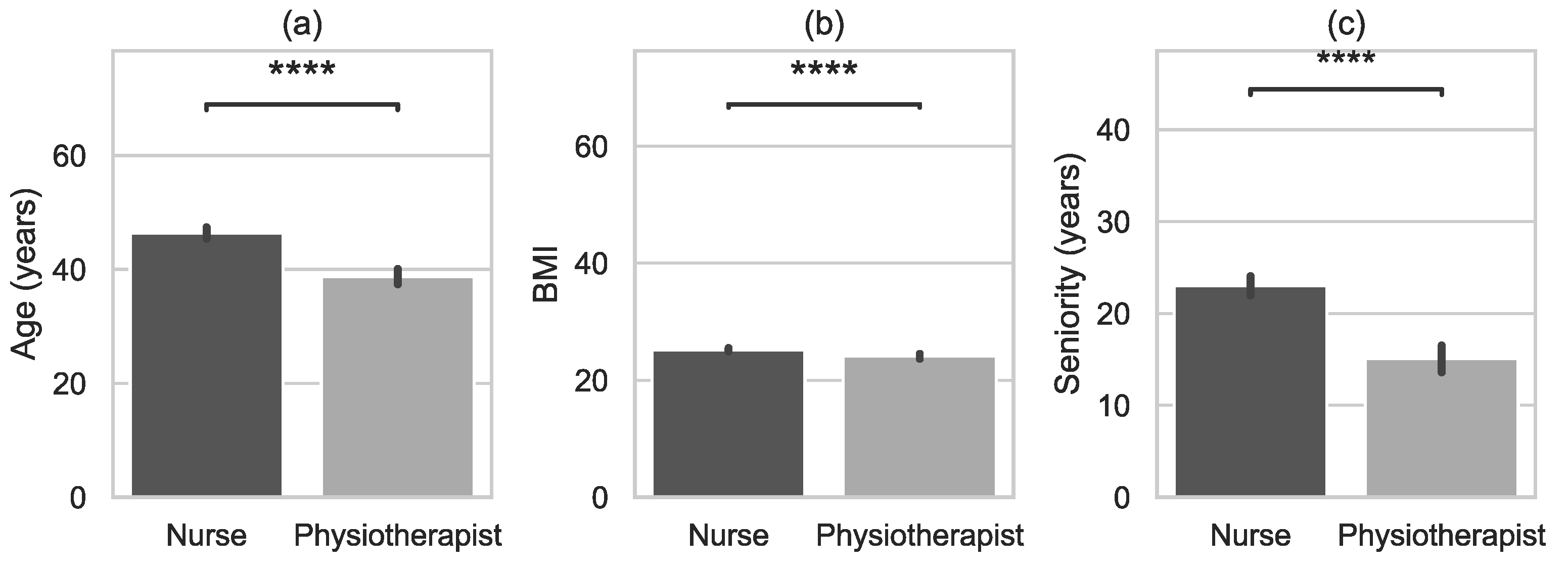
| Age (years) | Mean (SD) | 43.0 (10.6) | 38.7 (11.0) | 46.4 (9.0) | 0.0001 1 |
| Range | 19–65 | 19–63 | 24–65 | ||
| Me | 43 | 35 | 48 | ||
| (95% CI) | (42.1; 43.9) | (37.3; 40.1) | (45.4; 47.4) | ||
| Height (cm) | Mean (SD) | 168.4 (7.7) | 171.0 (8.6) | 166.4 (6.2) | 0.0001 1 |
| Range | 150–199 | 153–199 | 150–198 | ||
| Me | 168 | 170 | 166 | ||
| (95% CI) | (167.7; 169.0) | (169.9; 172.1) | (165.7; 167.0) | ||
| Weight (kg) | Mean (SD) | 70.2 (10.9) | 70.9 (13.9) | 69.6 (7.7) | 0.4054 1 |
| Range | 42–120 | 42–120 | 48–102 | ||
| Me | 69 | 67 | 70 | ||
| (95% CI) | (69.2; 71.1) | (69.1; 72.6) | (68.7; 70.5) | ||
| BMI | Mean (SD) | 24.7 (3.1) | 24.1 (3.4) | 25.2 (2.8) | 0.0001 1 |
| Range | 17.0–37.9 | 17.0–33.9 | 18.0–37.9 | ||
| Me | 24.7 | 23.5 | 25.0 | ||
| (95% CI) | (24.4; 25.0) | (23.7; 24.5) | (24.9; 25.5) | ||
| Seniority (years) | Mean (SD) | 19.5 (11.3) | 15.1 (11.8) | 23.0 (9.6) | 0.0001 1 |
| Range | 1–42 | 1–42 | 1–41 | ||
| Me | 20 | 12 | 25 | ||
| (95% CI) | (18.6; 20.5) | (13.6; 16.6) | (21.9; 24.1) |
| Back Pain at A Certain Level n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Neck Pain | Th Spine Pain | Low Back Pain | ||||||
| Total population | 164 (30.2%) | 96 (17.7%) | 438 (80.5%) | |||||
| Physiotherapists | 99 (41.3%) | 76 (31.7%) | 169 (70.4%) | |||||
| Nurses | 64 (21.1%) | 20 (6.6%) | 269 (88.5%) | |||||
| Central | To 1 limb | To 2 limbs | Central | Radiation | Central | To 1 limb | To 2 limbs | |
| Total population | 82 (15.1%) | 57 (10.5%) | 22 (4.0%) | 74 (13.6%) | 29 (5.3%) | 255 (46.9%) | 185 (34.0%) | 21 (3.9%) |
| Physiotherapists | 67 (27.5%) | 36 (14.8%) | 10 (4.1%) | 56 (23.0%) | 29 (11.9%) | 109 (44.7%) | 80 (32.8%) | 5 (2.1%) |
| Nurses | 15 (4.9%) | 21 (6.9%) | 12 (7.5%) | 18 (6.9%) | 0 (0.0%) | 146 (48.0%) | 105 (34.5%) | 16 (5.3%) |
| Total Population (N = 544) | Physiotherapists (n1 = 240) | Nurses (n2 = 304) | p-Value | ||
|---|---|---|---|---|---|
| Spinal pain experienced during working life | Yes | 517 (95.0%) | 220 (90.9%) | 297 (97.7%) | |
| No | 27 (5.0%) | 20 (9.1%) | 7 (2.3%) | ||
| Intensity of pain episodes (VAS) | Mean (SD) | 4.94 (1.6) | 4.64 (1.6%) | 5.37 (1.3) | 0.0000 1 |
| Range | 0–10 | 0–10 | 2–8 | ||
| Me | 5 | 5 | 5 | ||
| (95% CI) | (4.8; 5.1) | (4.4; 4.8) | (5.2; 5.6) | ||
| First episode of spinal pain (years) | 1 year ago | 69 (13.1%) | 52 (23.2%) | 17 (5.6%) | |
| 2–3 years ago | 91 (17.2%) | 31 (13.8%) | 60 (19.7%) | ||
| 4–6 years ago | 157 (29.7%) | 53 (23.7%) | 104 (34.3%) | 0.0000 1 | |
| 7–9 years ago | 130 (24.6%) | 56 (25.0%) | 74 (24.3%) | ||
| ≥10 years ago | 77 (14.6%) | 32 (14.3%) | 45 (14.8%) | ||
| missing data | 4 (0.8%) | 0 (0%) | 4 (1.3%) | ||
| Number of experienced episodes of spinal pain (number) | 0 | 38 (7%) | 22 (9.2%) | 16 (5.3%) | |
| 1–5 | 231 (42.7%) | 115 (47.8%) | 116 (38.5%) | ||
| 6–10 | 147 (27.2%) | 46 (19.2%) | 101 (33.2%) | 0.0045 1 | |
| ≥11 | 125 (23.1%) | 57 (23.8%) | 68 (22.4%) | ||
| missing data | 3 (0.6%) | 0 | 3 (1.0%) | ||
| Frequency of pain episodes | no pain | 21 (3.9%) | 16 (6.7%) | 5 (1.6%) | |
| once in a lifetime | 8 (1.5%) | 6 (2.5%) | 2 (0.7%) | ||
| several times in a lifetime | 101 (18.6%) | 84 (35.0%) | 17 (5.6%) | ||
| once a year | 21 (3.9%) | 19 (7.9%) | 2 (0.7%) | 0.0000 1 | |
| once a month | 63 (11.6%) | 46 (19.2%) | 17 (5.6%) | ||
| once a week | 78 (14.3%) | 25 (10.4%) | 53 (17.4%) | ||
| once a day | 192 (35.3%) | 20 (8.3%) | 172 (56.6%) | ||
| all the time | 60 (11.0%) | 24 (10.0%) | 36 (11.8%) | ||
| Limitation of physical activity | no | 151 (27.8%) | 106 (44.2%) | 45 (14.8%) | |
| minimal | 243 (44.7%) | 106 (43.4%) | 137 (45.1%) | ||
| significant | 147 (27.0%) | 26 (10.7%) | 121 (39.8%) | 0.0058 1 | |
| disabling | 3 (0.6%) | 2 (0.9%) | 1 (0.3%) |
| Total Population (N = 544) | Physiotherapists (n1 = 240) | Nurses (n2 = 304) | |
|---|---|---|---|
| Lifting | 320 (58.8%) | 142 (59.2%) | 178 (58.6%) |
| Bending | 244 (44.9%) | 79 (32.9%) | 165 (54.3%) |
| Standing | 169 (31.1%) | 90 (37.5%) | 79 (26.0%) |
| Sitting | 165 (30.3%) | 84 (35.0%) | 81 (26.6%) |
| Torso twist | 84 (145.4%) | 52 (21.7%) | 32 (10.5%) |
| Torso hyperextension | 35 (6.4%) | 21 (8.8%) | 14 (4.6%) |
| Total Population | Physiotherapists | Nurses | ||
|---|---|---|---|---|
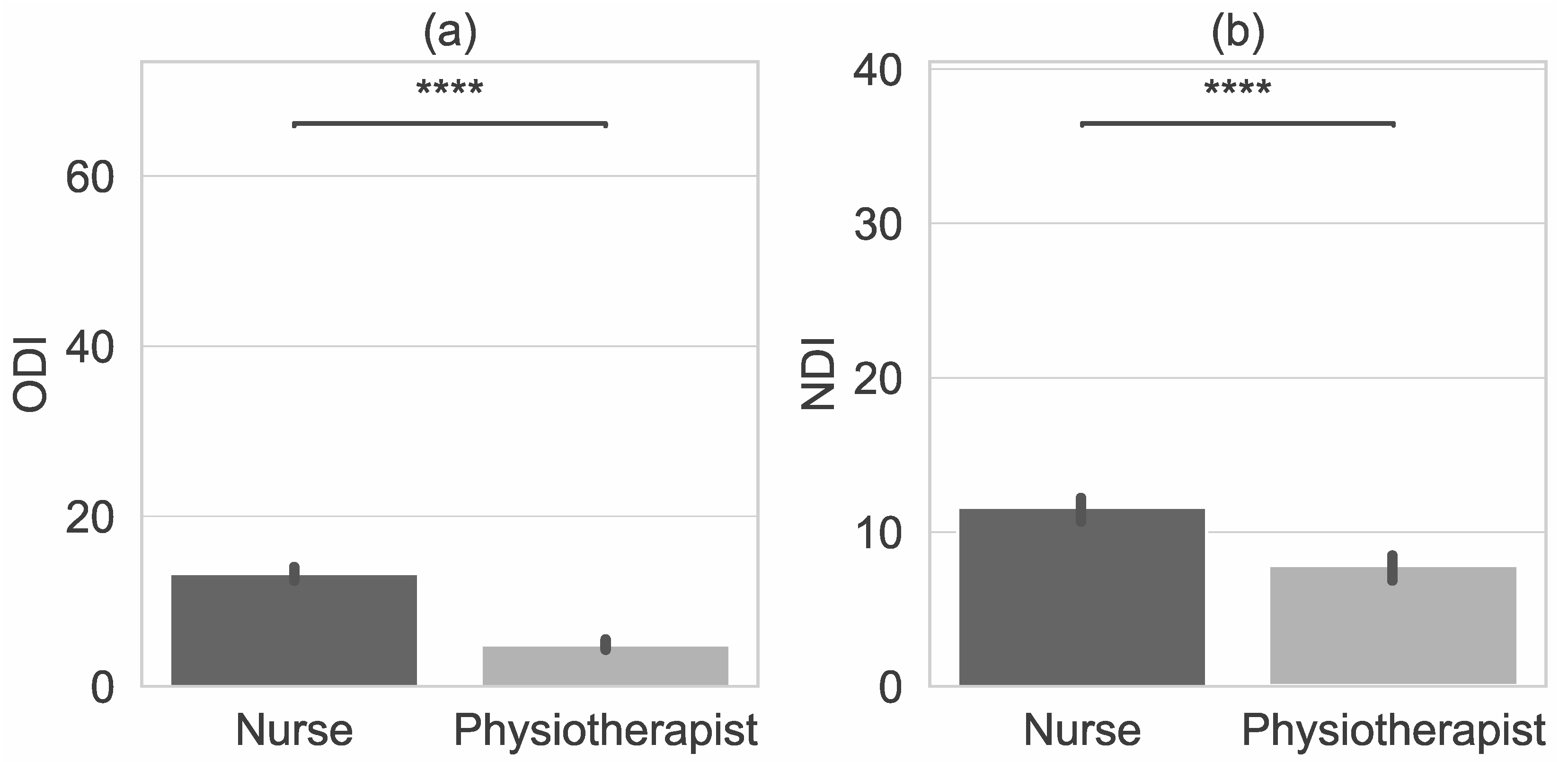
| ODI | ||||
| Number of participants with LBP who completed the ODI questionnaire | 438 | 169 | 269 | |
| ODI | Mean (SD) | 10.4 (7.3) | 6.0 (4.9) | 13.2 (7.2) |
| Range | 0–30 | 0–25 | 0–30 | |
| Me | 10 | 5 | 14 | |
| (95% CI) | (9.8; 11.0) | (5.3; 6.7) | (12.4; 14.0) | |
| 0–4 points (0–8%) no disability | Number (% of total population, or any of the subgroup) | no 177 (32.5%) | no 128 (53.3%) | no 49 (16.1%) |
| 5–14 points (10–28%) minimal disability | minimal 216 (39.7%) | minimal 100 (41.7%) | minimal 116 (38.5%) | |
| 15–24 points (30–48%) moderate disability | moderate 135 (24.9%) | moderate 11 (4.6%) | moderate 124 (40.8%) | |
| 25–34 points (50–64%) severe disability | severe 16 (2.9%) | severe 1 (0.4%) | severe 15 (4.9%) | |
| 35–50 points (70–100%) crippled | crippled 0 (0%) | crippled 0 (0%) | crippled 0 (0%) | |
| NDI | ||||
| Number of participants with NP who completed the NDI questionnaire | 163 | 99 | 64 | |
| NDI | Mean (SD) | 9.6 (7.0) | 8.0 (6.3) | 12.3 (7.3) |
| Range | 1–36 | 1–26 | 1–36 | |
| Me | 8 | 7 | 12 | |
| (95% CI) | (9.0; 10.2) | (7.3; 8.7) | (11.5; 8.1) | |
| 0–4 points (0–8%) no disability | Number (% of total population, or any of the subgroup) | no 43 (26%) | no 35 (35%) | no 8 (13%) |
| 5–14 points (10–28%) minimal disability | minimal 84 (52%) | minimal 54 (55%) | minimal 30 (47%) | |
| 15–24 points (30–48%) moderate disability | moderate 31 (19%) | moderate 9 (9%) | moderate 22 (34%) | |
| 25–34 points (50–64%) severe disability | severe 4 (2%) | severe 1 (1%) | severe 3 (5%) | |
| 35–50 points (70–100%) crippled | crippled 1 (1%) | crippled 0 (0%) | crippled 1 (1%) | |
| Pain | p-Value | |||
|---|---|---|---|---|
| Yes | No | |||
| Age (years) | Total population | 43.0 (10.6) | 32.1 (8.3) | 0.0001 1 |
| Physiotherapists Nurses | 39.3 (10.9) 46.7 (8.7) | 32.4 (9.1) 31.6 (5.7) | 0.0021 1 0.0002 1 | |
| BMI | Total population | 24.8 (3.1) | 23.4 (3.3) | 0.0920 1 |
| Physiotherapists Nurses | 24.2 (3.4) 25.2 (2.8) | 23.1 (3.5) 24.1 (2.8) | 0.3210 1 0.4209 1 | |
| Seniority (years) | Total population Physiotherapists Nurses | 20.1 (11.1) 15.6 (11.8) 23.4 (9.3) | 8.8 (8.9) 9.8 (9.8) 6.0 (5.5) | 0.0001 1 0.0152 1 0.0001 1 |
| Total Population (N = 544) | Physiotherapists (n1 = 240) | Nurses (n2 = 304) | p-Value | ||
|---|---|---|---|---|---|
| Pain | Yes | 5.0 (1.5) | 4.7 (1.6) | 5.3 (1.3) | 0.0001 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bryndal, A.; Glowinski, S.; Grochulska, A. Influence of Occupation on the Prevalence of Spinal Pain among Physiotherapists and Nurses. J. Clin. Med. 2022, 11, 5600. https://doi.org/10.3390/jcm11195600
Bryndal A, Glowinski S, Grochulska A. Influence of Occupation on the Prevalence of Spinal Pain among Physiotherapists and Nurses. Journal of Clinical Medicine. 2022; 11(19):5600. https://doi.org/10.3390/jcm11195600
Chicago/Turabian StyleBryndal, Aleksandra, Sebastian Glowinski, and Agnieszka Grochulska. 2022. "Influence of Occupation on the Prevalence of Spinal Pain among Physiotherapists and Nurses" Journal of Clinical Medicine 11, no. 19: 5600. https://doi.org/10.3390/jcm11195600
APA StyleBryndal, A., Glowinski, S., & Grochulska, A. (2022). Influence of Occupation on the Prevalence of Spinal Pain among Physiotherapists and Nurses. Journal of Clinical Medicine, 11(19), 5600. https://doi.org/10.3390/jcm11195600






