Correlation between the Control of Blood Glucose Level and HbA1C and the Incidence of Surgical Site Infection after Emergent Surgery for the Lower Limb Fracture among Type II DM Patients Aged More Than 50 Years Old
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
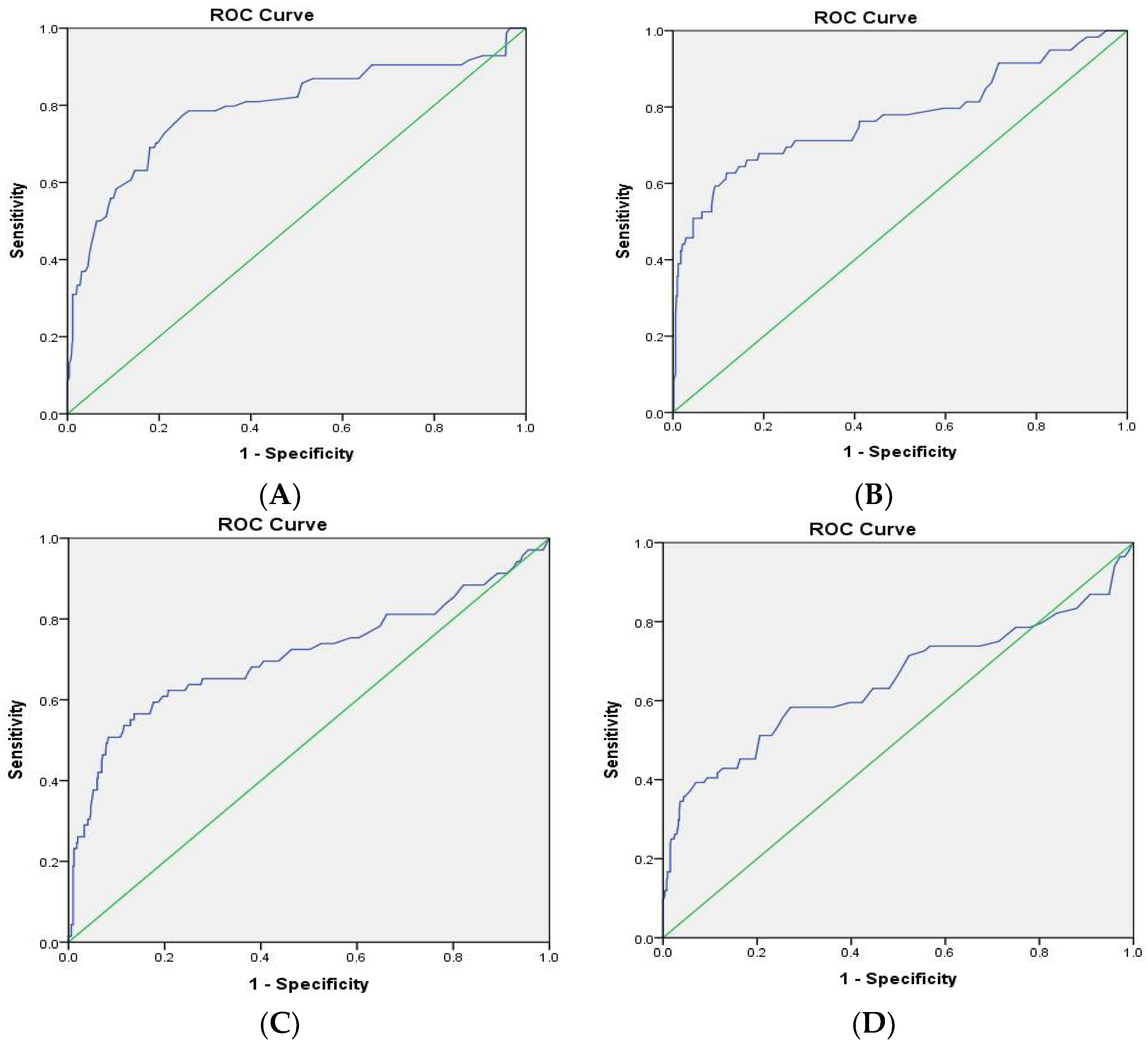
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119. [Google Scholar] [CrossRef] [PubMed]
- Biancari, F.; Giordano, S. Glycated Hemoglobin and the Risk of Sternal Wound Infection after Adult Cardiac Surgery: A Systematic Review and Meta-Analysis. Semin. Thorac. Cardiovasc. Surg. 2019, 31, 465–467. [Google Scholar] [CrossRef] [PubMed]
- Chow, A.; Switzer, N.J.; Dang, J.; Shi, X.; de Gara, C.; Birch, D.W.; Gill, R.S.; Karmali, S. A Systematic Review and Meta-Analysis of Outcomes for Type 1 Diabetes after Bariatric Surgery. J. Obes. 2016, 2016, 6170719. [Google Scholar] [CrossRef] [PubMed]
- Shohat, N.; Muhsen, K.; Gilat, R.; Rondon, A.J.; Chen, A.F.; Parvizi, J. Inadequate Glycemic Control Is Associated with Increased Surgical Site Infection in Total Joint Arthroplasty: A Systematic Review and Meta-Analysis. J. Arthroplast. 2018, 33, 2312–2321.e3. [Google Scholar] [CrossRef]
- Schipper, O.N.; Jiang, J.J.; Chen, L.; Koh, J.; Toolan, B.C. Effect of diabetes mellitus on perioperative complications and hospital outcomes after ankle arthrodesis and total ankle arthroplasty. Foot Ankle Int. 2015, 36, 258–267. [Google Scholar] [CrossRef]
- Toor, A.S.; Jiang, J.J.; Shi, L.L.; Koh, J.L. Comparison of perioperative complications after total elbow arthroplasty in patients with and without diabetes. J. Shoulder Elb. Surg. 2014, 23, 1599–1606. [Google Scholar] [CrossRef]
- Hikata, T.; Iwanami, A.; Hosogane, N.; Watanabe, K.; Ishii, K.; Nakamura, M.; Toyama, Y.; Matsumoto, M.; Kamata, M. High preoperative hemoglobin A1c is a risk factor for surgical site infection after posterior thoracic and lumbar spinal instrumentation surgery. J. Orthop. Sci. 2014, 19, 223–228. [Google Scholar] [CrossRef]
- Harris, A.H.; Bowe, T.R.; Gupta, S.; Ellerbe, L.S.; Giori, N.J. Hemoglobin A1C as a marker for surgical risk in diabetic patients undergoing total joint arthroplasty. J. Arthroplast. 2013, 28, 25–29. [Google Scholar] [CrossRef]
- Yang, L.; Sun, Y.; Li, G.; Liu, J. Is hemoglobin A1c and perioperative hyperglycemia predictive of periprosthetic joint infection following total joint arthroplasty? A systematic review and meta-analysis. Medicine 2017, 96, e8805. [Google Scholar] [CrossRef]
- Dhatariya, K.; Levy, N.; Kilvert, A.; Watson, B.; Cousins, D.; Flanagan, D.; Hilton, L.; Jairam, C.; Leyden, K.; Lipp, A.; et al. NHS Diabetes guideline for the perioperative management of the adult patient with diabetes. Diabet. Med. 2012, 29, 420–433. [Google Scholar] [CrossRef]
- Joshi, G.P.; Chung, F.; Vann, M.A.; Ahmad, S.; Gan, T.J.; Goulson, D.T.; Merrill, D.G.; Twersky, R.; Society for Ambulatory Anesthesia. Society for Ambulatory Anesthesia consensus statement on perioperative blood glucose management in diabetic patients undergoing ambulatory surgery. Anesth. Analg. 2010, 111, 1378–1387. [Google Scholar] [CrossRef] [PubMed]
- Society, A.D. Peri-Operative Diabetes Management Guidelines. Available online: https://diabetessociety.com.au/documents/PerioperativeDiabetesManagementGuidelinesFINALCleanJuly2012.pdf (accessed on 1 July 2012).
- Moghissi, E.S.; Korytkowski, M.T.; DiNardo, M.; Einhorn, D.; Hellman, R.; Hirsch, I.B.; Inzucchi, S.E.; Ismail-Beigi, F.; Kirkman, M.S.; Umpierrez, G.E. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Endocr. Pract. 2009, 15, 353–369. [Google Scholar] [CrossRef] [PubMed]
- Jacobi, J.; Bircher, N.; Krinsley, J.; Agus, M.; Braithwaite, S.S.; Deutschman, C.; Freire, A.X.; Geehan, D.; Kohl, B.; Nasraway, S.A.; et al. Guidelines for the use of an insulin infusion for the management of hyperglycemia in critically ill patients. Crit. Care Med. 2012, 40, 3251–3276. [Google Scholar] [CrossRef]
- Qaseem, A.; Humphrey, L.L.; Chou, R.; Snow, V.; Shekelle, P. Clinical Guidelines Committee of the American College of Phy-sicians. Use of intensive insulin therapy for the management of glycemic control in hospitalized patients: A clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 2011, 154, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Abdelmalak, B.B.; Knittel, J.; Abdelmalak, J.B.; Dalton, J.E.; Christiansen, E.; Foss, J.; Argalious, M.; Zimmerman, R.; Van den Berghe, G. Preoperative blood glucose concentrations and postoperative outcomes after elective non-cardiac surgery: An observational study. Br. J. Anaesth. 2014, 112, 79–88. [Google Scholar] [CrossRef]
- Frisch, A.; Chandra, P.; Smiley, D.; Peng, L.; Rizzo, M.; Gatcliffe, C.; Hudson, M.; Mendoza, J.; Johnson, R.; Lin, E.; et al. Prevalence and Clinical Outcome of Hyperglycemia in the Perioperative Period in Noncardiac Surgery. Diabetes Care 2010, 33, 1783–1788. [Google Scholar] [CrossRef]
- Noordzij, P.G.; Boersma, E.; Schreiner, F.; Kertai, M.; Feringa, H.H.H.; Dunkelgrun, M.; Bax, J.J.; Klein, J.; Poldermans, D. Increased preoperative glucose levels are associated with perioperative mortality in patients undergoing noncardiac, nonvascular surgery. Eur. J. Endocrinol. 2007, 156, 137–142. [Google Scholar] [CrossRef]
- Jämsen, E.; Nevalainen, P.; Kalliovalkama, J.; Moilanen, T. Preoperative hyperglycemia predicts infected total knee replacement. Eur. J. Intern. Med. 2010, 21, 196–201. [Google Scholar] [CrossRef]
- Kwon, S.; Thompson, R.; Dellinger, P.; Rogers, T.; Flum, D. Importance of Perioperative Glycemic Control in General Surgery: A Report from the Surgical Care and Outcomes Assessment Program. Ann. Surg. 2013, 257, 8–14. [Google Scholar] [CrossRef]
- Ramos, M.; Khalpey, Z.; Lipsitz, S.; Steinberg, J.; Panizales, M.T.; Zinner, M.; Rogers, S.O. Relationship of perioperative hy-perglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann. Surg. 2008, 248, 585–591. [Google Scholar]
- Horan, T.C.; Gaynes, R.P.; Martone, W.J.; Jarvis, W.R.; Emori, T.G. CDC definitions of nosocomial surgical site infections, 1992: A modification of CDC definitions of surgical wound infections. Infect. Control Hosp. Epidemiol. 1992, 13, 606–608. [Google Scholar] [CrossRef]
- Blankush, J.M.; Leitman, I.M.; Soleiman, A.; Tran, T. Association between elevated pre-operative glycosylated hemoglobin and post-operative infections after non-emergent surgery. Ann. Med. Surg. 2016, 10, 77–82. [Google Scholar] [CrossRef]
- Werner, B.C.; Teran, V.A.; Cancienne, J.; Deal, D.N. The Association of Perioperative Glycemic Control with Postoperative Surgical Site Infection Following Open Carpal Tunnel Release in Patients with Diabetes. Hand 2019, 14, 324–328. [Google Scholar] [CrossRef]
- Kohzuma, T.; Tao, X.; Koga, M. Glycated albumin as biomarker: Evidence and its outcomes. J. Diabetes Complicat. 2021, 35, 108040. [Google Scholar] [CrossRef]
- Kavin, M.; Yayac, M.; Grosso, M.J.; Courtney, P.M. Preoperative Hemoglobin A1c > 7.5 Is Associated with Increased Bundled Payment Costs in Total Hip and Knee Arthroplasties. J. Am. Acad. Orthop. Surg. 2021, 29, 970–976. [Google Scholar] [CrossRef]
- Jämsen, E.; Nevalainen, P.I.; Eskelinen, A.; Kalliovalkama, J.; Moilanen, T. Risk factors for perioperative hyperglycemia in primary hip and knee replacements. Acta Orthop. 2015, 86, 175–182. [Google Scholar] [CrossRef]
- Wexler, D.J.; Nathan, D.M.; Grant, R.; Regan, S.; Van Leuvan, A.L.; Cagliero, E. Prevalence of Elevated Hemoglobin A1c among Patients Admitted to the Hospital without a Diagnosis of Diabetes. J. Clin. Endocrinol. Metab. 2008, 93, 4238–4244. [Google Scholar] [CrossRef]
- Listing, J.; Gerhold, K.; Zink, A. The risk of infections associated with rheumatoid arthritis, with its comorbidity and treatment. Rheumatology 2013, 52, 53–61. [Google Scholar] [CrossRef]
- Sun, Y.; Wang, H.; Tang, Y.; Zhao, H.; Qin, S.; Xu, L.; Xia, Z.; Zhang, F. Incidence and risk factors for surgical site infection after open reduction and internal fixation of ankle fracture: A retrospective multicenter study. Medicine 2018, 97, e9901. [Google Scholar] [CrossRef]
- Molina, C.S.; Stinner, D.J.; Fras, A.R.; Evans, J.M. Risk factors of deep infection in operatively treated pilon fractures (AO/OTA: 43). J. Orthop. 2015, 12 (Suppl. 1), S7–S13. [Google Scholar] [CrossRef]
- Cichos, K.H.; Churchill, J.L.; Phillips, S.G.; Watson, S.L.; McGwin, G., Jr.; Ghanem, E.S.; Ponce, B.A. Metabolic syndrome and hip fracture: Epidemiology and perioperative outcomes. Injury 2018, 49, 2036–2041. [Google Scholar] [CrossRef] [PubMed]
| Male | Female | Total | p Value | |
|---|---|---|---|---|
| N | 215 | 389 | 604 | |
| Age | 66.98 ± 15.08 | 73.55 ± 11.87 | 71.21 ± 13.46 | <0.001 * |
| BMI | 25.10 ± 4.50 | 25.34 ± 4.78 | 25.26 ± 4.68 | 0.551 |
| Preoperative HbA1c (%) | 7.60 ± 2.24 | 7.53 ± 1.99 | 7.55 ± 2.08 | 0.680 |
| Preoperative AC Glucose (mg/dL) | 150.26 ± 61.08 | 144.96 ± 54.05 | 146.83 ± 56.64 | 0.284 |
| Medical comorbidities | ||||
| HTN (%) | 167 (77.7%) | 328 (84.3%) | 495 (82.0%) | 0.042 * |
| Dyslipidemia (%) | 88 (40.9%) | 179 (46.0%) | 267 (44.2%) | 0.228 |
| CAD (%) | 70 (32.6%) | 120 (30.8%) | 190 (31.5%) | 0.665 |
| CVA (%) | 54 (25.1%) | 109 (28.0%) | 163 (27.0%) | 0.441 |
| Hepatic disease (%) | 51 (23.7%) | 60 (15.4%) | 111 (18.4%) | 0.012 * |
| CRF (%) | 71 (33.0%) | 116 (29.8%) | 187 (31.0%) | 0.415 |
| RA (%) | 78 (36.3%) | 159 (40.9%) | 237 (39.2%) | 0.268 |
| Surgical site infection (%) | 36 (16.7%) | 48 (12.3%) | 84 (13.9%) | 0.134 |
| Superficial | Deep | |
|---|---|---|
| N | 62 | 22 |
| Days after ORIF | 2–74 | 11–110 |
| Pathogens | methicillin-resistant Staphylococcus aureus (6) | methicillin-resistant Staphylococcus aureus (4) |
| methicillin-susceptible Staphylococcus aureus (34) | methicillin-susceptible Staphylococcus aureus (9) | |
| Pseudomonas aeruginosa (12) | Pseudomonas aeruginosa (3) | |
| Enterococcus faecalis (3) | Enterobacter cloacae (1) | |
| Mixed bacteria (4) | Escherichia coli (1) | |
| Acinetobacter baumannii (1) | ||
| Mixed bacteria (3) |
| Crude | Adjusted (Model 1) | Adjusted (Model 2) | Adjusted (Model 3) | Adjusted (Model 4) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age | 0.97 (0.95, 0.99) | <0.001 * | 0.99 (0.97, 1.02) | 0.635 | 0.99 (0.97, 1.01) | 0.222 | 0.97 (0.95, 0.99) | 0.021 * | 0.98 (0.95, 0.99) | 0.026 * |
| Sex (M vs. F) | 1.43 (0.89, 2.28) | 0.135 | 1.4 (0.78, 2.52) | 0.264 | 1.26 (0.74, 2.17) | 0.393 | 1.20 (0.59, 2.44) | 0.611 | 1.12 (0.60, 2.07) | 0.720 |
| BMI | 1.01 (0.96, 1.06) | 0.711 | 1 (0.95, 1.07) | 0.873 | 1.00 (0.95, 1.06) | 0.950 | 0.98 (0.91, 1.05) | 0.558 | 0.99 (0.93, 1.05) | 0.729 |
| Preoperative HbA1c | 1.76 (1.56, 1.98) | <0.001 * | 1.77 (1.56, 2.02) | <0.001 * | - | - | - | - | - | - |
| Postoperative HbA1c | 1.42 (1.29, 1.57) | <0.001 * | - | - | 1.43 (1.28, 1.59) | <0.001 * | - | - | - | - |
| Preoperative Glucose | 1.02 (1.01, 1.02) | <0.001 * | - | - | - | - | 1.02 (1.01, 1.02) | <0.001 * | - | - |
| Postoperative Glucose | 1.01 (1.01, 1.02) | <0.001 * | - | - | - | - | - | - | 1.01 (1.01, 1.02) | <0.001 * |
| HTN vs. None | 0.49 (0.29, 0.83) | 0.008 * | 0.43 (0.21, 0.86) | 0.017 * | 0.44 (0.23, 0.84) | 0.013 * | 0.53 (0.23, 1.24) | 0.146 | 0.51 (0.24, 1.08) | 0.077 |
| Dyslipidemia vs. None | 1.31 (0.83, 2.08) | 0.250 | 0.96 (0.52, 1.77) | 0.900 | 1.08 (0.63, 1.88) | 0.774 | 0.80 (0.39, 1.63) | 0.537 | 1.21 (0.66, 2.22) | 0.543 |
| CAD vs. None | 1.25 (0.77, 2.03) | 0.366 | 1.73 (0.91, 3.31) | 0.097 | 1.67 (0.92, 3.03) | 0.090 | 2.25 (1.02, 4.95) | 0.045 * | 1.44 (0.73, 2.87) | 0.297 |
| CVA vs. None | 0.60 (0.34, 1.06) | 0.080 | 0.58 (0.28, 1.21) | 0.146 | 0.65 (0.33, 1.25) | 0.192 | 0.27 (0.10, 0.77) | 0.014 * | 0.54 (0.25, 1.13) | 0.102 |
| Hepatic disease vs. None | 1.15 (0.65, 2.05) | 0.635 | 1.08 (0.54, 2.16) | 0.821 | 0.93 (0.49, 1.79) | 0.838 | 0.88 (0.37, 2.07) | 0.767 | 0.96 (0.47, 1.95) | 0.903 |
| CRF vs. None | 1.07 (0.65, 1.75) | 0.801 | 1.60 (0.83, 3.05) | 0.158 | 1.48 (0.82, 2.69) | 0.196 | 1.26 (0.59, 2.71) | 0.555 | 1.45 (0.75, 2.80) | 0.275 |
| RA vs. None | 2.21 (1.38, 3.52) | 0.001 * | 2.50 (1.39, 4.48) | 0.002 * | 2.53 (1.48, 4.33) | 0.001 * | 2.97 (1.48, 5.99) | 0.002 * | 2.85 (1.55, 5.23) | 0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, W.-H.; Hsieh, T.-C.; Wu, W.-T.; Lee, R.-P.; Wang, J.-H.; Yeh, K.-T. Correlation between the Control of Blood Glucose Level and HbA1C and the Incidence of Surgical Site Infection after Emergent Surgery for the Lower Limb Fracture among Type II DM Patients Aged More Than 50 Years Old. J. Clin. Med. 2022, 11, 5552. https://doi.org/10.3390/jcm11195552
Wang W-H, Hsieh T-C, Wu W-T, Lee R-P, Wang J-H, Yeh K-T. Correlation between the Control of Blood Glucose Level and HbA1C and the Incidence of Surgical Site Infection after Emergent Surgery for the Lower Limb Fracture among Type II DM Patients Aged More Than 50 Years Old. Journal of Clinical Medicine. 2022; 11(19):5552. https://doi.org/10.3390/jcm11195552
Chicago/Turabian StyleWang, Wei-Hung, Tsung-Cheng Hsieh, Wen-Tien Wu, Ru-Ping Lee, Jen-Hung Wang, and Kuang-Ting Yeh. 2022. "Correlation between the Control of Blood Glucose Level and HbA1C and the Incidence of Surgical Site Infection after Emergent Surgery for the Lower Limb Fracture among Type II DM Patients Aged More Than 50 Years Old" Journal of Clinical Medicine 11, no. 19: 5552. https://doi.org/10.3390/jcm11195552
APA StyleWang, W.-H., Hsieh, T.-C., Wu, W.-T., Lee, R.-P., Wang, J.-H., & Yeh, K.-T. (2022). Correlation between the Control of Blood Glucose Level and HbA1C and the Incidence of Surgical Site Infection after Emergent Surgery for the Lower Limb Fracture among Type II DM Patients Aged More Than 50 Years Old. Journal of Clinical Medicine, 11(19), 5552. https://doi.org/10.3390/jcm11195552








