Change in Physical and Mental Quality-of-Life between the Short- and Mid-Term Periods after Cervical Laminoplasty for Cervical Spondylotic Myelopathy: A Retrospective Cohort Study with Minimum 5 Years Follow-up
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics
2.2. Patient Population
2.3. Surgical Procedure
2.4. Radiological Evaluations
2.5. Clinical Evaluations
2.6. QOL Parameters
2.7. Study Design & Statistical Analysis
2.7.1. Main Analysis
2.7.2. Sub-Analysis
3. Results
3.1. Patient Details
3.2. Main Analysis
3.2.1. Average Change in PCS and MCS Scores
3.2.2. Individual Change in PCS and MCS Scores
3.3. Sub-Analysis
3.3.1. Comparison of the Change in SF-36 Subdomain Scores
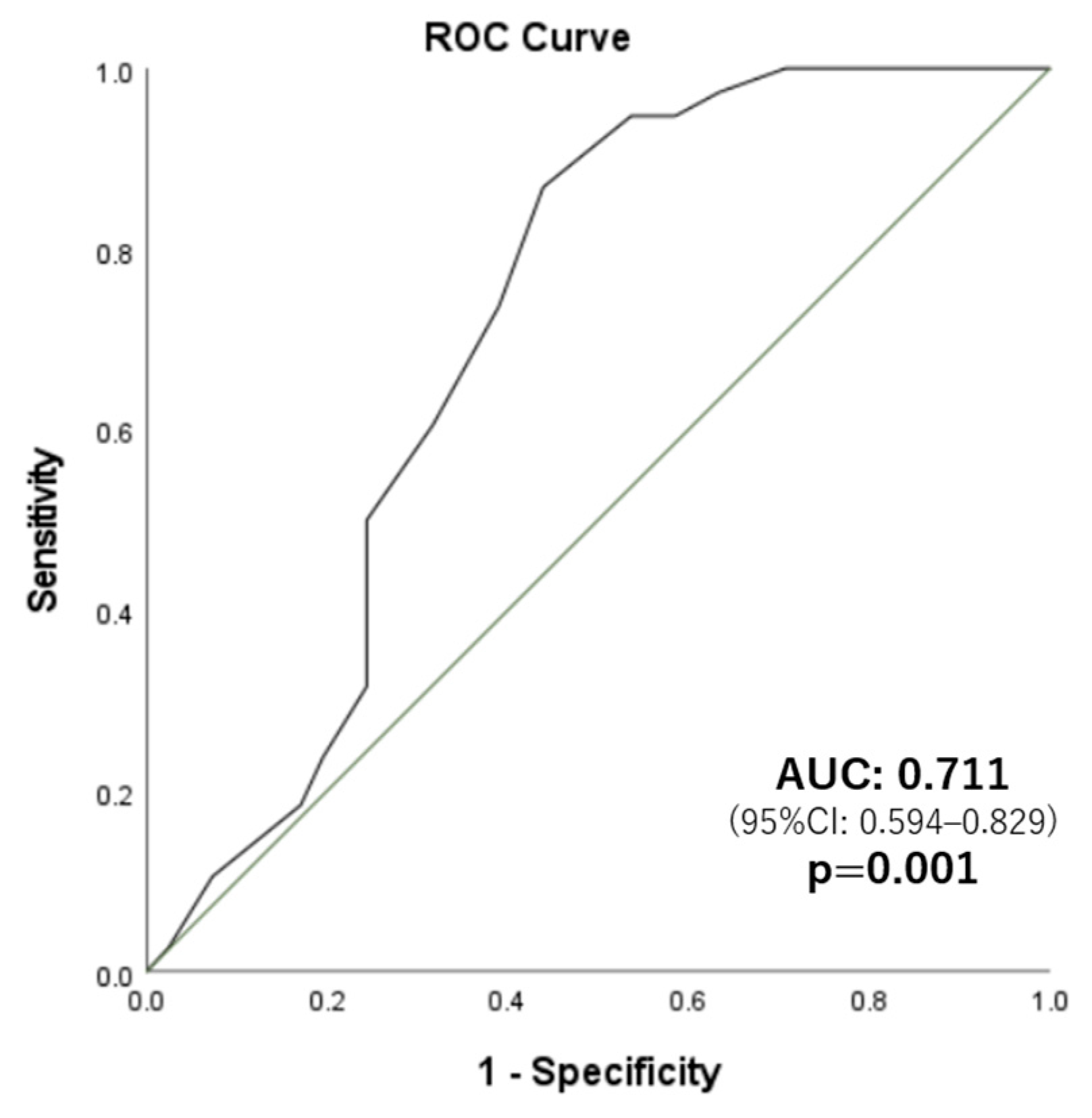
3.3.2. Predictive Factors for the Deterioration in PCS Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Quality of Life Assessment Group. What quality of life? World Health Forum 1996, 17, 354–356. [Google Scholar]
- Ware, J.E., Jr.; Gandek, B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J. Clin. Epidemiol. 1998, 51, 903–912. [Google Scholar] [CrossRef]
- Ware, J.E., Jr. SF-36 health survey update. Spine 2000, 25, 3130–3139. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, J.N.; Tosteson, T.D.; Lurie, J.D.; Osteson, A.N.; Blood, E.; Hanscom, B.; Herkowitz, H.; Cammisa, F.; Albert, T.; Boden, S.D.; et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N. Engl. J. Med. 2008, 358, 794–810. [Google Scholar] [CrossRef] [PubMed]
- Fehlings, M.G.; Wilson, J.R.; Kopjar, B.; Yoon, S.T.; Arnold, P.M.; Massicotte, E.M.; Vaccaro, A.R.; Brodke, D.S.; Shaffrey, C.I.; Smith, J.S.; et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: Results of the AOSpine North America prospective multi-center study. J. Bone Jt. Surg. Am. 2013, 95, 1651–1658. [Google Scholar] [CrossRef] [PubMed]
- Nouri, A.; Tetreault, L.; Singh, A.; Karadimas, S.K.; Fehlings, M.G. Degenerative cervical myelopathy: Epidemiology, genetics, and pathogenesis. Spine 2015, 40, E675–E693. [Google Scholar] [CrossRef]
- Ghogawala, Z.; Terrin, N.; Dunbar, M.R.; Breeze, J.L.; Freund, K.M.; Kanter, A.S.; Mummaneni, P.V.; Bisson, E.F.; Barker, F.G., 2nd; Schwartz, J.S.; et al. Effect of ventral vs dorsal spinal surgery on patient-reported physical functioning in patients with cervical spondylotic myelopathy: A randomized clinical trial. JAMA 2021, 325, 942–951. [Google Scholar] [CrossRef]
- Arrojas, A.; Jackson, J.B., 3rd; Grabowski, G. Trends in the treatment of single and multilevel cervical stenosis: A review of the American Board of Orthopaedic Surgery Database. J. Bone Jt. Surg. Am. 2017, 99, e99. [Google Scholar] [CrossRef]
- Perfetti, D.C.; Galina, J.M.; Derman, P.B.; Guyer, R.D.; Ohnmeiss, D.D.; Satin, A.M. Risk factors for reoperation after lumbar total disc replacement at short-, mid-, and long-term follow-up. Spine J. 2021, 21, 1110–1117. [Google Scholar] [CrossRef]
- Ahmad, S.S.; Hoos, L.; Perka, C.; Stöckle, U.; Braun, K.F.; Konrads, C. Follow-up definitions in clinical orthopaedic research: A systematic review. Bone Jt. Open 2021, 2, 344–350. [Google Scholar] [CrossRef]
- Chiba, K.; Ogawa, Y.; Ishii, K.; Takaishi, H.; Nakamura, M.; Maruiwa, H.; Matsumoto, M.; Toyama, Y. Long-term results of expansive open-door laminoplasty for cervical myelopathy—Average 14-year follow-up study. Spine 2006, 31, 2998–3005. [Google Scholar] [CrossRef] [PubMed]
- Sakaura, H.; Hosono, N.; Mukai, Y.; Iwasaki, M.; Yoshikawa, H. C3-6 laminoplasty for cervical spondylotic myelopathy maintains satisfactory long-term surgical outcomes. Glob. Spine J. 2014, 4, 169–174. [Google Scholar] [CrossRef]
- Satomi, K.; Nishu, Y.; Kohno, T.; Hirabayashi, K. Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine 1994, 19, 507–510. [Google Scholar] [CrossRef] [PubMed]
- Seichi, A.; Takeshita, K.; Ohishi, I.; Kawaguchi, H.; Akune, T.; Anamizu, Y.; Kitagawa, T.; Nakamura, K. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine 2001, 26, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Tamai, K.; Suzuki, A.; Terai, H.; Hoshino, M.; Toyoda, H.; Takahashi, S.; Hori, Y.; Yabu, A.; Nakamura, H. Time course of physical and mental well-being improvements after cervical surgery. Spine 2021, 46, E303–E309. [Google Scholar] [CrossRef]
- Hirabayashi, K.; Watanabe, K.; Wakano, K.; Suzuki, N.; Satomi, K.; Ishii, Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine 1983, 8, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Tamai, K.; Suzuki, A.; Terai, H.; Toyoda, H.; Hoshino, M.; Nakamura, H. Laminar closure after expansive open-door laminoplasty: Fixation methods and cervical alignments impact on the laminar closure and surgical outcomes. Spine J. 2016, 16, 1062–1069. [Google Scholar] [CrossRef]
- Japanese Orthopedic Association. Scoring system for cervical myelopathy. J. Jpn. Orthop. Assoc. 1994, 68, 490–530. [Google Scholar]
- Carreon, L.Y.; Djurasovic, M.; Dimar, J.R., 2nd; Owens, R.K., 2nd; Crawford, C.H., 3rd; Puno, R.M.; Bratcher, K.R.; McGraw, K.E.; Glassman, S.D. Can the anxiety domain of EQ-5D and mental health items from SF-36 help predict outcomes after surgery for lumbar degenerative disorders? J. Neurosurg. Spine 2016, 25, 352–356. [Google Scholar] [CrossRef]
- Fukuhara, S.; Bito, S.; Green, J.; Hsiao, A.; Kurokawa, K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J. Clin. Epidemiol. 1998, 51, 1037–1044. [Google Scholar] [CrossRef]
- Strazdins, E.; Nie, Y.F.; Ramli, R.; Palesy, T.; Christensen, J.M.; Alvarado, R.; Marcells, G.N.; Harvey, R.J. Association between mental health status and patient satisfaction with the functional outcomes of rhinoplasty. JAMA Facial Plast. Surg. 2018, 20, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Badhiwala, J.H.; Witiw, C.D.; Nassiri, F.; Akbar, M.A.; Jaja, B.; Wilson, J.R.; Fehlings, M.G. Minimum clinically important difference in SF-36 scores for use in degenerative cervical myelopathy. Spine 2018, 43, E1260–E1266. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E. Understanding the relevance of measured change through studies of responsiveness. Spine 2000, 25, 3192–3199. [Google Scholar] [CrossRef] [PubMed]
- Jenkinson, C.; Coulter, A.; Wright, L. Short form 36 (SF36) health survey questionnaire: Normative data for adults of working age. BMJ 1993, 306, 1437–1440. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhou, F.; Sun, Y. Assessment of health-related quality of life using the SF-36 in Chinese cervical spondylotic myelopathy patients after surgery and its consistency with neurological function assessment: A cohort study. Health Qual. Life Outcomes 2015, 13, 39. [Google Scholar] [CrossRef] [PubMed]
- Fehlings, M.G.; Barry, S.; Kopjar, B.; Yoon, S.T.; Arnold, P.; Massicotte, E.M.; Vaccaro, A.; Brodke, D.S.; Shaffrey, C.; Smith, J.S.; et al. Anterior versus posterior surgical approaches to treat cervical spondylotic myelopathy: Outcomes of the prospective multicenter AOSpine North America CSM study in 264 patients. Spine 2013, 38, 2247–2252. [Google Scholar] [CrossRef]
- Tamai, K.; Suzuki, A.; Terai, H.; Hoshino, M.; Toyoda, H.; Takahashi, S.; Ohyama, S.; Hori, Y.; Yabu, A.; Nakamura, H. Improvement in patient mental well-being after surgery for cervical spondylotic myelopathy. Spine 2020, 45, E568–E575. [Google Scholar] [CrossRef]
- Thakar, S.; Christopher, S.; Rajshekhar, V. Quality of life assessment after central corpectomy for cervical spondylotic myelopathy: Comparative evaluation of the 36-Item Short Form Health Survey and the World Health Organization Quality of Life-Bref. J. Neurosurg. Spine 2009, 11, 402–412. [Google Scholar] [CrossRef]

| Variables | Values | p-Value |
|---|---|---|
| Total numbers (cases) | 80 | |
| Age (years) | 64.0 ± 11.2 | |
| Sex (female/male) | 25/55 | |
| MRI findings | ||
| Number of stenosis levels | ||
| Single-level stenosis | 12 (15.0%) | |
| Double-level stenosis | 48 (60.0%) | |
| Triple-level stenosis | 20 (25.0%) | |
| Snake-eye appearance (+) | 31 (38.8%) | |
| Complications | ||
| C5 palsy | 3 (3.8%) | |
| Surgical site infection | 1 (1.3%) | |
| Reoperation within 5 years | 2 (2.6%) | |
| cJOA score | ||
| Preoperative | 9.7 ± 3.4 | <0.001 * |
| 3 months postop | 13.3 ± 2.1 | |
| 2 years postop | 13.5 ± 2.5 | |
| 5 years postop | 13.1 ± 2.8 | |
| Neck pain VAS | 0.018 * | |
| Preoperative | 24.7 ± 29.0 | |
| 3 months postop | 13.9 ± 20.4 | |
| 2 years postop | 12.9 ± 21.1 | |
| 5 years postop | 12.6 ± 20.8 | |
| Arm pain VAS | 0.045 * | |
| Preoperative | 31.4 ± 33.0 | |
| 3 months postop | 20.0 ± 25.6 | |
| 2 years postop | 17.0 ± 25.6 | |
| 5 years postop | 16.6 ± 27.1 | |
| Arm numbness | <0.001 * | |
| Preoperative | 58.6 ± 30.0 | |
| 3 months postop | 33.9 ± 27.7 | |
| 2 years postop | 33.4 ± 28.0 | |
| 5 years postop | 34.1 ± 28.3 |
| Improved or Stable | Deterioration | p-Value | |
|---|---|---|---|
| SF-36 PCS | 38 | 42 | 0.001 # |
| SF-36 MCS | 59 | 21 |
| Domains | Without Deterioration | Deterioration | p-Value |
|---|---|---|---|
| Physical functioning | 6.6 ± 12.0 | −19.4 ± 19.5 | <0.001 |
| Role physical | 4.4 ± 27.1 | −17.4 ± 27.3 | <0.001 |
| Bodily pain | 4.6 ± 14.6 | −12.4 ± 23.8 | <0.001 |
| General health perceptions | 0.8 ± 12.1 | −5.9 ± 12.2 | 0.015 |
| Vitality | 1.8 ± 19.0 | −7.6 ± 15.6 | 0.018 |
| Social functioning | 7.6 ± 20.0 | −3.0 ± 27.9 | 0.058 |
| Role emotional | 7.7 ± 24.2 | −8.9 ± 31.4 | 0.011 |
| Mental health | 0.7 ± 16.9 | −4.2 ± 18.3 | 0.221 |
| Explanatory Variables | Reference | Adjusted OR | p-Value | 95% CI |
|---|---|---|---|---|
| Age | Continuous | 1.05 | 0.131 | 0.98–1.11 |
| Sex (male) | Female | 1.05 | 0.937 | 0.36–3.08 |
| cJOA at 2 ys postop | Continuous | 0.57 | 0.008 | 0.38–0.86 |
| PCS at 2 ys postop | Continuous | 1.07 | 0.052 | 0.99–1.14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tamai, K.; Suzuki, A.; Terai, H.; Kato, M.; Toyoda, H.; Takahashi, S.; Yabu, A.; Sawada, Y.; Iwamae, M.; Nakamura, H. Change in Physical and Mental Quality-of-Life between the Short- and Mid-Term Periods after Cervical Laminoplasty for Cervical Spondylotic Myelopathy: A Retrospective Cohort Study with Minimum 5 Years Follow-up. J. Clin. Med. 2022, 11, 5230. https://doi.org/10.3390/jcm11175230
Tamai K, Suzuki A, Terai H, Kato M, Toyoda H, Takahashi S, Yabu A, Sawada Y, Iwamae M, Nakamura H. Change in Physical and Mental Quality-of-Life between the Short- and Mid-Term Periods after Cervical Laminoplasty for Cervical Spondylotic Myelopathy: A Retrospective Cohort Study with Minimum 5 Years Follow-up. Journal of Clinical Medicine. 2022; 11(17):5230. https://doi.org/10.3390/jcm11175230
Chicago/Turabian StyleTamai, Koji, Akinobu Suzuki, Hidetomi Terai, Minori Kato, Hiromitsu Toyoda, Shinji Takahashi, Akito Yabu, Yuta Sawada, Masayoshi Iwamae, and Hiroaki Nakamura. 2022. "Change in Physical and Mental Quality-of-Life between the Short- and Mid-Term Periods after Cervical Laminoplasty for Cervical Spondylotic Myelopathy: A Retrospective Cohort Study with Minimum 5 Years Follow-up" Journal of Clinical Medicine 11, no. 17: 5230. https://doi.org/10.3390/jcm11175230
APA StyleTamai, K., Suzuki, A., Terai, H., Kato, M., Toyoda, H., Takahashi, S., Yabu, A., Sawada, Y., Iwamae, M., & Nakamura, H. (2022). Change in Physical and Mental Quality-of-Life between the Short- and Mid-Term Periods after Cervical Laminoplasty for Cervical Spondylotic Myelopathy: A Retrospective Cohort Study with Minimum 5 Years Follow-up. Journal of Clinical Medicine, 11(17), 5230. https://doi.org/10.3390/jcm11175230







