Predictive Factors of Surgical Recurrence in Patients with Crohn’s Disease on Long-Term Follow-Up: A Focus on Histology
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ye, Y.; Manne, S.; Treem, W.R.; Bennett, D. Prevalence of Inflammatory Bowel Disease in Pediatric and Adult Populations: Recent Estimates From Large National Databases in the United States, 2007–2016. Inflamm. Bowel. Dis. 2020, 26, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Momozawa, Y.; Dmitrieva, J.; Théâtre, E.; Deffontaine, V.; Rahmouni, S.; Charloteaux, B.; Crins, F.; Docampo, E.; Elansary, M.; Gori, A.S.; et al. IBD risk loci are enriched in multigenic regulatory modules encompassing putative causative genes. Nat. Commun. 2018, 9, 2427. [Google Scholar] [CrossRef] [PubMed]
- Caviglia, G.P.; Rosso, C.; Ribaldone, D.G.; Dughera, F.; Fagoonee, S.; Astegiano, M.; Pellicano, R. Physiopathology of intestinal barrier and the role of zonulin. Minerva Biotecnol. 2019, 31, 83–92. [Google Scholar] [CrossRef]
- Holleran, G.; Lopetuso, L.R.; Ianiro, G.; Pecere, S.; Pizzoferrato, M.; Petito, V.; Graziani, C.; McNamara, D.; Gasbarrini, A.; Scaldaferri, F. Gut microbiota and inflammatory bowel disease: So far so gut! Minerva Gastroenterol. Dietol. 2017, 63, 373–384. [Google Scholar] [CrossRef]
- Shaffer, V.O.; Wexner, S.D. Surgical management of Crohn’s disease. Langenbecks Arch. Surg. 2013, 398, 13–27. [Google Scholar] [CrossRef]
- Valibouze, C.; Desreumaux, P.; Zerbib, P. Post-surgical recurrence of Crohn’s disease: Situational analysis and future prospects. J. Visc. Surg. 2021, 158, 401–410. [Google Scholar] [CrossRef]
- Aksan, A.; Farrag, K.; Blumenstein, I.; Schröder, O.; Dignass, A.U.; Stein, J. Chronic intestinal failure and short bowel syndrome in Crohn’s disease. World J. Gastroenterol. 2021, 27, 3440–3465. [Google Scholar] [CrossRef]
- Lock, M.R.; Farmer, R.G.; Fazio, V.W.; Jagelman, D.G.; Lavery, I.C.; Weakley, F.L. Recurrence and reoperation for Crohn’s disease: The role of disease location in prognosis. N. Engl. J. Med. 1981, 304, 1586–1588. [Google Scholar] [CrossRef]
- Michelassi, F.; Balestracci, T.; Chappell, R.; Block, G.E. Primary and recurrent Crohn’s disease. Experience with 1379 patients. Ann. Surg. 1991, 214, 230–238. [Google Scholar] [CrossRef]
- Fichera, A.; Lovadina, S.; Rubin, M.; Cimino, F.; Hurst, R.D.; Michelassi, F. Patterns and operative treatment of recurrent Crohn’s disease: A prospective longitudinal study. Surgery 2006, 140, 649–654. [Google Scholar] [CrossRef]
- Unkart, J.T.; Anderson, L.; Li, E.; Miller, C.; Yan, Y.; Gu, C.C.; Chen, J.; Stone, C.D.; Hunt, S.; Dietz, D.W. Risk factors for surgical recurrence after ileocolic resection of Crohn’s disease. Dis. Colon Rectum 2008, 51, 1211–1216. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Li, Y.; Gong, J.; Zhu, W. Frequency and risk factors of surgical recurrence of Crohn’s disease after primary bowel resection. Turk. J. Gastroenterol. 2018, 29, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Aaltonen, G.; Carpelan-Holmström, M.; Keränen, I.; Lepistö, A. Surgical recurrence in Crohn’s disease: A comparison between different types of bowel resections. Int. J. Colorectal Dis. 2018, 33, 473–477. [Google Scholar] [CrossRef]
- Kim, S.B.; Cheon, J.H.; Park, J.J.; Kim, E.S.; Jeon, S.W.; Jung, S.A.; Park, D.I.; Lee, C.K.; Im, J.P.; Kim, Y.S.; et al. Risk Factors for Postoperative Recurrence in Korean Patients with Crohn’s Disease. Gut Liver 2020, 14, 331–337. [Google Scholar] [CrossRef]
- Maaser, C.; Sturm, A.; Vavricka, S.R.; Kucharzik, T.; Fiorino, G.; Annese, V.; Calabrese, E.; Baumgart, D.C.; Bettenworth, D.; Borralho Nunes, P.; et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J. Crohns Colitis 2019, 13, 144–164. [Google Scholar] [CrossRef] [PubMed]
- Sturm, A.; Maaser, C.; Calabrese, E.; Annese, V.; Fiorino, G.; Kucharzik, T.; Vavricka, S.R.; Verstockt, B.; van Rheenen, P.; Tolan, D.; et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 2: IBD scores and general principles and technical aspects. J. Crohns Colitis 2019, 13, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Beaugerie, L.; Seksik, P.; Nion-Larmurier, I.; Gendre, J.P.; Cosnes, J. Predictors of Crohn’s disease. Gastroenterology 2006, 130, 650–656. [Google Scholar] [CrossRef]
- Maaser, C.; Langholz, E.; Gordon, H.; Burisch, J.; Ellul, P.; Ramirez, V.H.; Karakan, T.; Katsanos, K.H.; Krustins, E.; Levine, A.; et al. European Crohn’s and Colitis Organisation Topical Review on Environmental Factors in IBD. J. Crohns Colitis 2017, 11, 905–920. [Google Scholar] [CrossRef]
- Wang, M.H.; Friton, J.J.; Raffals, L.E.; Leighton, J.A.; Pasha, S.F.; Picco, M.F.; Monroe, K.; Nix, B.D.; Newberry, R.D.; Faubion, W.A. Novel Genetic Variant Predicts Surgical Recurrence Risk in Crohn’s Disease Patients. Inflamm. Bowel Dis. 2021, 27, 1968–1974. [Google Scholar] [CrossRef]
- Gklavas, A.; Dellaportas, D.; Papaconstantinou, I. Risk factors for postoperative recurrence of Crohn’s disease with emphasis on surgical predictors. Ann. Gastroenterol. 2017, 30, 598–612. [Google Scholar] [CrossRef]
- Hammoudi, N.; Cazals-Hatem, D.; Auzolle, C.; Gardair, C.; Ngollo, M.; Bottois, H.; Nancey, S.; Pariente, B.; Buisson, A.; Treton, X.; et al. Association between Microscopic Lesions at Ileal Resection Margin and Recurrence After Surgery in Patients With Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2020, 18, 141–149.e2. [Google Scholar] [CrossRef] [PubMed]
- Simillis, C.; Jacovides, M.; Reese, G.E.; Yamamoto, T.; Tekkis, P.P. Meta-analysis of the role of granulomas in the recurrence of Crohn disease. Dis. Colon Rectum 2010, 53, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Stocchi, L.; Liu, X.; Rui, Y.; Liu, G.; Remzi, F.H.; Shen, B. Presence of Granulomas in Mesenteric Lymph Nodes Is Associated with Postoperative Recurrence in Crohn’s Disease. Inflamm. Bowel Dis. 2015, 21, 2613–2618. [Google Scholar] [CrossRef]
- Gionchetti, P.; Dignass, A.; Danese, S.; Magro Dias, F.J.; Rogler, G.; Lakatos, P.L.; Adamina, M.; Ardizzone, S.; Buskens, C.J.; Sebastian, S.; et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 2: Surgical Management and Special Situations. J. Crohns Colitis 2017, 11, 135–149. [Google Scholar] [CrossRef]
- Losurdo, G.; Brescia, I.V.; Lillo, C.; Mezzapesa, M.; Barone, M.; Principi, M.; Ierardi, E.; Di Leo, A.; Rendina, M. Liver involvement in inflammatory bowel disease: What should the clinician know? World J. Hepatol. 2021, 13, 1534–1551. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | n = 108 |
|---|---|
| Age at first surgery (years), mean ± SD | 38.8 ± 13.8 |
| Age at CD diagnosis (years), median (IQR) | 28.5 (22.0–45.0) |
| Sex (M/F), n | 60/48 |
| Smoking habit (current/ex/never), n (%) | 54 (50.0%)/22 (20.4%)/32 (29.6%) |
| Family history of CD, n (%) | 20 (18.5%) |
| Colonic involvement, n (%) | 54 (50.0%) |
| Upper gastrointestinal tract involvement (L4), n (%) 1 | 13 (12.0%) |
| Variables | Univariate (HR; 95% CI) | p Value | Multivariate * (aHR; 95%CI) | p Value |
|---|---|---|---|---|
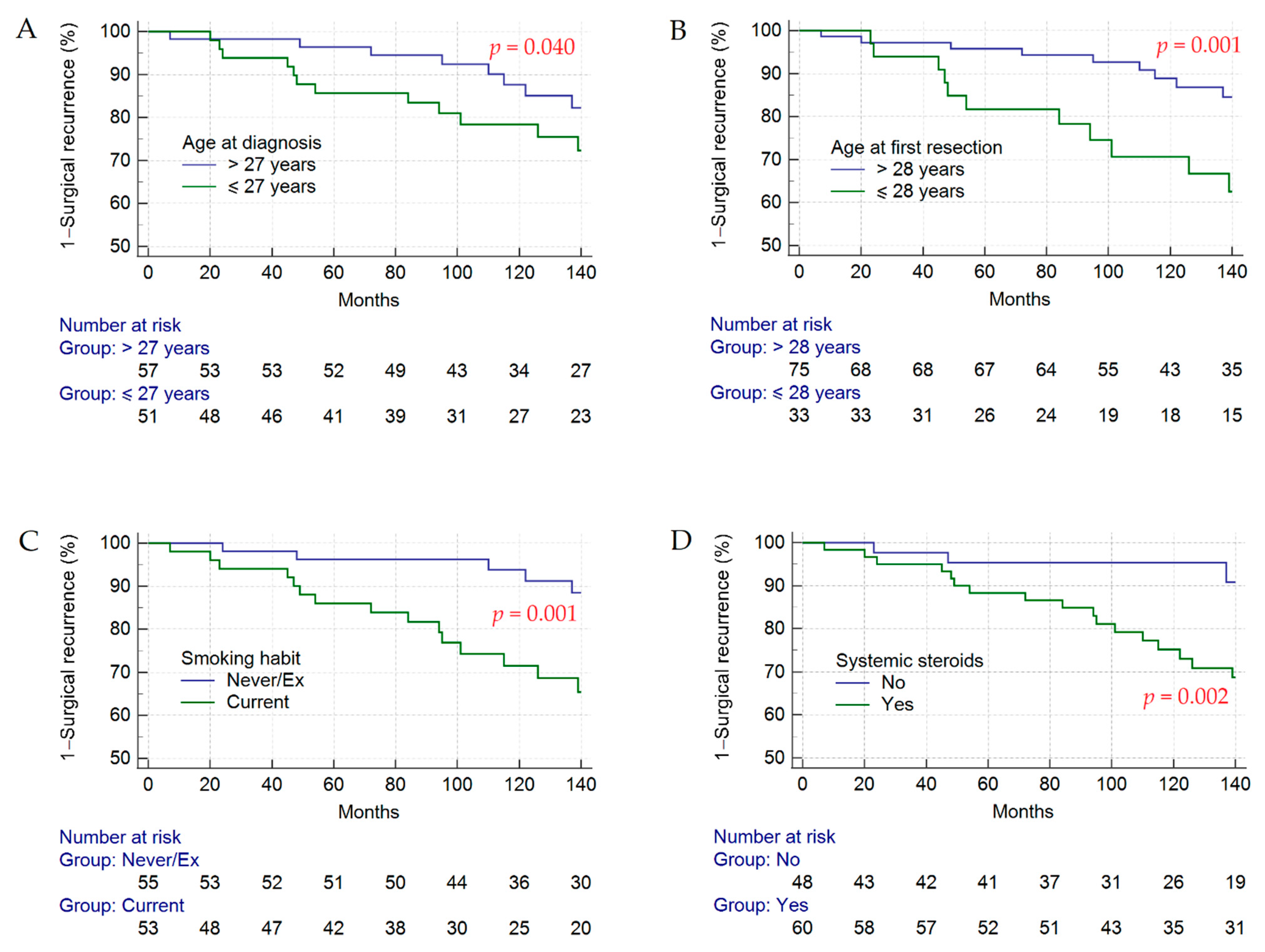
| Age at first surgery ≤ 28 years | 2.95 (1.52–5.76) | 0.001 | 16.44 (4.63–58.34) | <0.001 |
| Age at CD diagnosis ≤ 27 years | 1.98 (1.01–3.90) | 0.048 | / | / |
| Female sex | 1.24 (0.64–2.40) | 0.530 | 7.58 (2.50–22.99) | <0.001 |
| Current smoker | 3.28 (1.59–6.78) | 0.001 | 15.84 (4.80–52.23) | <0.001 |
| Family history of CD | 0.84 (0.36–1.96) | 0.840 | / | / |
| Colonic involvement | 0.57 (0.29–1.12) | 0.100 | / | / |
| Upper gastrointestinal tract involvement (L4) | 1.63 (0.63–4.27) | 0.310 | / | / |
| Perianal lesions | 1.29 (0.60–2.76) | 0.510 | / | / |
| Fistulas | 0.68 (0.34–1.34) | 0.260 | / | / |
| Stenosis | 0.70 (0.29–1.72) | 0.440 | / | / |
| Laparoscopic resection | 1.14 (0.27–4.78) | 0.860 | / | / |
| Length of bowel resection (cm) | 1.01 (0.99–1.02) | 0.500 | / | / |
| Surgical margins involvement | 1.11 (0.49–2.50) | 0.800 | / | / |
| Temporary ostomy | 0.52 (0.20–1.34) | 0.180 | / | / |
| Cryptitis | 0.49 (0.17–1.38) | 0.180 | 0.02 (0.00–0.11) | <0.001 |
| Plexitis | 2.06 (0.62–6.82) | 0.240 | / | / |
| Sierositis | 0.97 (0.46–2.02) | 0.930 | / | / |
| Perivisceritis | 0.23 (0.03–1.68) | 0.150 | / | / |
| Colonic microscopic inflammation | 0.56 (0.28–1.13) | 0.110 | / | / |
| Granulomas at loco-regional lymph nodes | 2.16 (0.98–4.77) | 0.056 | 12.19 (3.27–45.46) | <0.001 |
| Reactive lymphoid hyperplasia | 1.44 (0.69–3.00) | 0.330 | / | / |
| Hyper-eosinophilia | 2.68 (0.36–19.90) | 0.330 | / | / |
| Pseudopiloric metaplasia | 0.23 (0.03–1.68) | 0.150 | / | / |
| Inflammatory pseudopolyps | 0.64 (0.19–2.09) | 0.460 | / | / |
| Anti-TNF administration | 0.63 (0.29–1.36) | 0.240 | / | / |
| Thiopurine administration | 0.55 (0.27–1.12) | 0.100 | / | / |
| Corticosteroid administration | 4.07 (1.57–10.55) | 0.002 | 7.52 (2.15–26.22) | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caviglia, G.P.; Mineo, C.A.; Rosso, C.; Armandi, A.; Astegiano, M.; Canavese, G.; Resegotti, A.; Saracco, G.M.; Ribaldone, D.G. Predictive Factors of Surgical Recurrence in Patients with Crohn’s Disease on Long-Term Follow-Up: A Focus on Histology. J. Clin. Med. 2022, 11, 5043. https://doi.org/10.3390/jcm11175043
Caviglia GP, Mineo CA, Rosso C, Armandi A, Astegiano M, Canavese G, Resegotti A, Saracco GM, Ribaldone DG. Predictive Factors of Surgical Recurrence in Patients with Crohn’s Disease on Long-Term Follow-Up: A Focus on Histology. Journal of Clinical Medicine. 2022; 11(17):5043. https://doi.org/10.3390/jcm11175043
Chicago/Turabian StyleCaviglia, Gian Paolo, Chiara Angela Mineo, Chiara Rosso, Angelo Armandi, Marco Astegiano, Gabriella Canavese, Andrea Resegotti, Giorgio Maria Saracco, and Davide Giuseppe Ribaldone. 2022. "Predictive Factors of Surgical Recurrence in Patients with Crohn’s Disease on Long-Term Follow-Up: A Focus on Histology" Journal of Clinical Medicine 11, no. 17: 5043. https://doi.org/10.3390/jcm11175043
APA StyleCaviglia, G. P., Mineo, C. A., Rosso, C., Armandi, A., Astegiano, M., Canavese, G., Resegotti, A., Saracco, G. M., & Ribaldone, D. G. (2022). Predictive Factors of Surgical Recurrence in Patients with Crohn’s Disease on Long-Term Follow-Up: A Focus on Histology. Journal of Clinical Medicine, 11(17), 5043. https://doi.org/10.3390/jcm11175043









