The Association between Idiopathic Pulmonary Fibrosis and Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
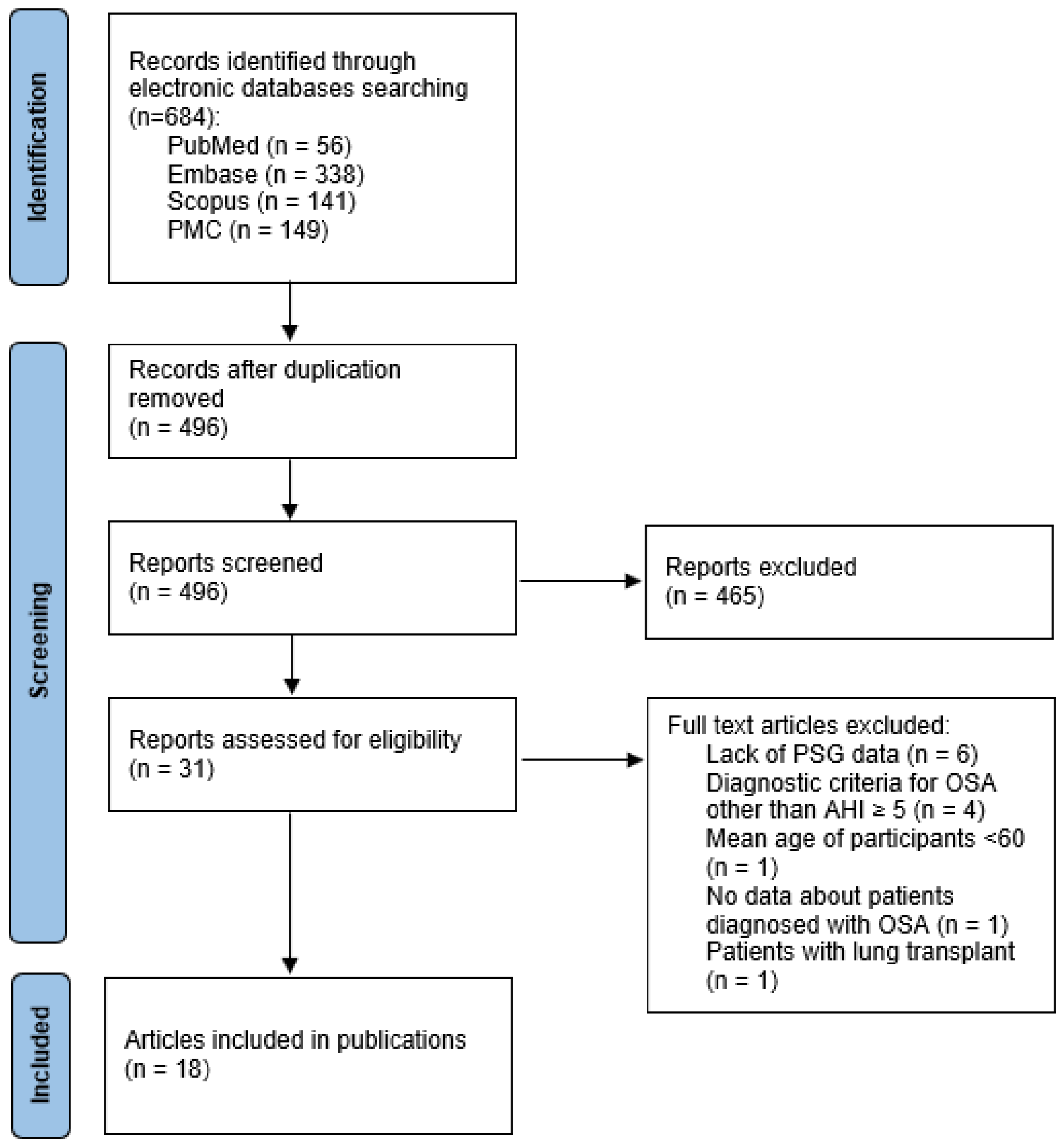
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Study Selection
2.4. Data Extraction
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Eligible Studies
3.2. Prevalence of OSA in IPF Patients
3.3. Prevalence of OSA in Ethnically Matched Population
4. Discussion
Strengths & Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Senaratna, C.V.; Perret, J.L.; Lodge, C.J.; Lowe, A.J.; Campbell, B.E.; Matheson, M.C.; Hamilton, G.S.; Dharmage, S.C. Prevalence of Obstructive Sleep Apnea in the General Population: A Systematic Review. Sleep Med. Rev. 2017, 34, 70–81. [Google Scholar] [CrossRef]
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.-L.; et al. Estimation of the Global Prevalence and Burden of Obstructive Sleep Apnoea: A Literature-Based Analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef]
- Laratta, C.R.; Ayas, N.T.; Povitz, M.; Pendharkar, S.R. Diagnosis and Treatment of Obstructive Sleep Apnea in Adults. Can. Med Assoc. J. 2017, 189, E1481–E1488. [Google Scholar] [CrossRef]
- Gabryelska, A.; Sochal, M.; Wasik, B.; Szczepanowski, P.; Białasiewicz, P. Factors Affecting Long-Term Compliance of CPAP Treatment—A Single Centre Experience. J. Clin. Med. 2021, 11, 139. [Google Scholar] [CrossRef]
- Lancaster, L.H.; Mason, W.R.; Parnell, J.A.; Rice, T.; Loyd, J.; Milstone, A.P.; Collard, H.R.; Malow, B.A. Obstructive Sleep Apnea Is Common in Idiopathic Pulmonary Fibrosis. Chest 2009, 136, 772–778. [Google Scholar] [CrossRef]
- Gundogdu, S.; Borekci, S.; Atahan, E.; Musellim, B. Increased Frequency of Obstructive Sleep Apnea in the Patients with Systemic Sclerosis. Sleep Breath. 2020, 25, 237–242. [Google Scholar] [CrossRef]
- Petta, S.; Marrone, O.; Torres, D.; Buttacavoli, M.; Cammà, C.; Di Marco, V.; Licata, A.; Bue, A.L.; Parrinello, G.; Pinto, A.; et al. Obstructive Sleep Apnea Is Associated with Liver Damage and Atherosclerosis in Patients with Non-Alcoholic Fatty Liver Disease. PLoS ONE 2015, 10, e0142210. [Google Scholar] [CrossRef]
- Wynn, T.A.; Ramalingam, T.R. Mechanisms of Fibrosis: Therapeutic Translation for Fibrotic Disease. Nat. Med. 2012, 18, 1028–1040. [Google Scholar] [CrossRef]
- Sgalla, G.; Iovene, B.; Calvello, M.; Ori, M.; Varone, F.; Richeldi, L. Idiopathic Pulmonary Fibrosis: Pathogenesis and Management. Respir. Res. 2018, 19, 32. [Google Scholar] [CrossRef]
- Philip, K.; Mills, W.T.; Davies, J.; Chen, N.; Karmouty-Quintana, H.; Luo, F.; Molina, J.G.; Amione-Guerra, J.; Sinha, N.; Guha, A.; et al. HIF1A up-regulates the ADORA2B Receptor on Alternatively Activated Macrophages and Contributes to Pulmonary Fibrosis. FASEB J. 2017, 31, 4745–4758. [Google Scholar] [CrossRef]
- Gabryelska, A.; Szmyd, B.; Panek, M.; Szemraj, J.; Kuna, P.; Białasiewicz, P. Serum Hypoxia-Inducible Factor-1α Protein Level as a Diagnostic Marker of Obstructive Sleep Apnea. Pol. Arch. Intern. Med. 2020, 130, 158–160. [Google Scholar] [CrossRef]
- Gabryelska, A.; Karuga, F.F.; Szmyd, B.; Białasiewicz, P. HIF-1α as a Mediator of Insulin Resistance, T2DM, and Its Complications: Potential Links with Obstructive Sleep Apnea. Front. Physiol. 2020, 11, 1035. [Google Scholar] [CrossRef]
- Ziello, J.E.; Jovin, I.S.; Huang, Y. Hypoxia-Inducible Factor (HIF)-1 Regulatory Pathway and Its Potential for Therapeutic Intervention in Malignancy and Ischemia. Yale J. Biol. Med. 2007, 80, 51–60. [Google Scholar]
- Gabryelska, A.; Stawski, R.; Sochal, M.; Szmyd, B.; Białasiewicz, P. Influence of One-Night CPAP Therapy on the Changes of HIF-1α Protein in OSA Patients: A Pilot Study. J. Sleep Res. 2020, 29, e12995. [Google Scholar] [CrossRef]
- Shochet, G.E.; Bardenstein-Wald, B.; McElroy, M.; Kukuy, A.; Surber, M.; Edelstein, E.; Pertzov, B.; Kramer, M.; Shitrit, D. Hypoxia Inducible Factor 1A Supports a Pro-Fibrotic Phenotype Loop in Idiopathic Pulmonary Fibrosis. Int. J. Mol. Sci. 2021, 22, 3331. [Google Scholar] [CrossRef]
- Rasmussen, L.N.; Montgomery, P. The Prevalence of and Factors Associated with Inclusion of Non-English Language Studies in Campbell Systematic Reviews: A Survey and Meta-Epidemiological Study. Syst. Rev. 2018, 7, 129. [Google Scholar] [CrossRef]
- Meltzer, E.B.; Noble, P.W. Idiopathic Pulmonary Fibrosis. Orphanet J. Rare Dis. 2008, 3, 8. [Google Scholar] [CrossRef]
- Kärkkäinen, M.; Kettunen, H.-P.; Nurmi, H.; Selander, T.; Purokivi, M.; Kaarteenaho, R. Effect of Smoking and Comorbidities on Survival in Idiopathic Pulmonary Fibrosis. Respir. Res. 2017, 18, 160. [Google Scholar] [CrossRef]
- Fisher, J.H.; Kolb, M.; Algamdi, M.; Morisset, J.; Johannson, K.A.; Shapera, S.; Wilcox, P.; To, T.; Sadatsafavi, M.; Manganas, H.; et al. Baseline Characteristics and Comorbidities in The Canadian Registry for Pulmonary Fibrosis. BMC Pulm. Med. 2019, 19, 223. [Google Scholar] [CrossRef]
- Kärkkäinen, M.; Kettunen, H.-P.; Nurmi, H.; Selander, T.; Purokivi, M.; Kaarteenaho, R. Comparison of Disease Progression Subgroups in Idiopathic Pulmonary Fibrosis. BMC Pulm. Med. 2019, 19, 228. [Google Scholar] [CrossRef]
- Moore, I.; Wrobel, J.; Rhodes, J.; Lin, Q.; Webster, S.; Jo, H.; Troy, L.; Grainge, C.; Glaspole, I.; Corte, T.J.; et al. Australasian Interstitial Lung Disease Registry (AILDR): Objectives, Design and Rationale of a Bi-National Prospective Database. BMC Pulm. Med. 2020, 20, 257. [Google Scholar] [CrossRef]
- Root, E.D.; Graney, B.; Baird, S.; Churney, T.; Fier, K.; Korn, M.; McCormic, M.; Sprunger, D.; Vierzba, T.; Wamboldt, F.S.; et al. Physical Activity and Activity Space in Patients with Pulmonary Fibrosis Not Prescribed Supplemental Oxygen. BMC Pulm. Med. 2017, 17, 154. [Google Scholar] [CrossRef]
- Mermigkis, C.; Chapman, J.; Golish, J.; Mermigkis, D.; Budur, K.; Kopanakis, A.; Polychronopoulos, V.; Burgess, R.; Foldvary-Schaefer, N. Sleep-Related Breathing Disorders in Patients with Idiopathic Pulmonary Fibrosis. Lung 2007, 185, 173–178. [Google Scholar] [CrossRef]
- Papadogiannis, G.; Bouloukaki, I.; Mermigkis, C.; Michelakis, S.; Ermidou, C.; Mauroudi, E.; Moniaki, V.; Tzanakis, N.; Antoniou, K.M.; Schiza, S.E. Patients with Idiopathic Pulmonary Fibrosis with and Without Obstructive Sleep Apnea: Differences in Clinical Characteristics, Clinical Outcomes, and the Effect of PAP Treatment. J. Clin. Sleep Med. 2021, 17, 533–544. [Google Scholar] [CrossRef]
- Troy, L.K.; Young, I.H.; Lau, E.M.; Wong, K.K.; Yee, B.J.; Torzillo, P.J.; Corte, T.J. Nocturnal Hypoxaemia Is Associated with Adverse Outcomes in Interstitial Lung Disease. Respirology 2019, 24, 996–1004. [Google Scholar] [CrossRef]
- Adegunsoye, A.; Neborak, J.M.; Zhu, D.; Cantrill, B.; Garcia, N.; Oldham, J.M.; Noth, I.; Vij, R.; Kuzniar, T.J.; Bellam, S.K.; et al. CPAP Adherence, Mortality, and Progression-Free Survival in Interstitial Lung Disease and OSA. Chest 2020, 158, 1701–1712. [Google Scholar] [CrossRef]
- Zhang, X.L.; Dai, H.P.; Zhang, H.; Gao, B.; Zhang, L.; Han, T.; Wang, C. Obstructive Sleep Apnea in Patients with Fibrotic Interstitial Lung Disease and COPD. J. Clin. Sleep Med. 2019, 15, 1807–1815. [Google Scholar] [CrossRef]
- A Ahmed, M.; Awadalla, N.J. Burden of Sleep-Related Breathing Disorders, Air Trapping, and Obesity in Idiopathic Pulmonary Fibrosis Patie. Egypt. J. Chest Dis. Tuberc. 2018, 67, 300. [Google Scholar] [CrossRef]
- Sommerwerck, U.; Kleibrink, B.E.; Kruse, F.; Scherer, M.J.; Wang, Y.; Kamler, M.; Teschler, H.; Weinreich, G. Predictors of Obstructive Sleep Apnea in Lung Transplant Recipients. Sleep Med. 2016, 21, 121–125. [Google Scholar] [CrossRef]
- Reid, T.; Vennelle, M.; McKinley, M.; Macfarlane, P.A.; Hirani, N.; Simpson, A.J.; Riha, R.L. Sleep-Disordered Breathing and Idiopathic Pulmonary Fibrosis—Is There an Association? Sleep Breath. 2015, 19, 719–721. [Google Scholar] [CrossRef]
- Pihtili, A.; Bingol, Z.; Kiyan, E.; Cuhadaroglu, C.; Issever, H.; Gulbaran, Z. Obstructive Sleep Apnea Is Common in Patients with Interstitial Lung Disease. Sleep Breath. 2013, 17, 1281–1288. [Google Scholar] [CrossRef]
- Mermigkis, C.; Bouloukaki, I.; Antoniou, K.; Papadogiannis, G.; Giannarakis, I.; Varouchakis, G.; Siafakas, N.; Schiza, S.E. Obstructive sleep apnea should be treated in patients with idiopathic pulmonary fibrosis. Sleep Breath. 2014, 19, 385–391. [Google Scholar] [CrossRef]
- Mermigkis, C.; Stagaki, E.; Tryfon, S.; Schiza, S.; Amfilochiou, A.; Polychronopoulos, V.; Panagou, P.; Galanis, N.; Kallianos, A.; Mermigkis, D.; et al. How common is sleep-disordered breathing in patients with idiopathic pulmonary fibrosis? Sleep Breath. 2010, 14, 387–390. [Google Scholar] [CrossRef]
- Pillai, M.; Olson, A.L.; Huie, T.J.; Solomon, J.J.; Fernandez-Perez, E.R.; Brown, K.K.; Hanna, P.; Lee-Chiong, T.; Swigris, J.J. Obstructive Sleep Apnea Does Not Promote Esophageal Reflux in Fibrosing Interstitial Lung Disease. Respir. Med. 2012, 106, 1033–1039. [Google Scholar] [CrossRef]
- Kolilekas, L.; Manali, E.; Vlami, K.A.; Lyberopoulos, P.; Triantafillidou, C.; Kagouridis, K.; Baou, K.; Gyftopoulos, S.; Vougas, K.; Karakatsani, A.; et al. Sleep Oxygen Desaturation Predicts Survival in Idiopathic Pulmonary Fibrosis. J. Clin. Sleep Med. 2013, 9, 593–601. [Google Scholar] [CrossRef]
- Lee, R.; Kelly, E.; Nolan, G.; Eigenheer, S.; Boylan, D.; Murphy, D.; Dodd, J.; Keane, M.; McNicholas, W. Disordered Breathing During Sleep and Exercise in Idiopathic Pulmonary Fibrosis and the Role of Biomarkers. QJM: Int. J. Med. 2014, 108, 315–323. [Google Scholar] [CrossRef]
- Schertel, A.; Funke-Chambour, M.; Geiser, T.; Brill, A.-K. Novel Insights in Cough and Breathing Patterns of Patients with Idiopathic Pulmonary Fibrosis Performing Repeated 24-Hour-Respiratory Polygraphies. Respir. Res. 2017, 18, 190. [Google Scholar] [CrossRef]
- Bosi, M.; Milioli, G.; Fanfulla, F.; Tomassetti, S.; Ryu, J.; Parrino, L.; Riccardi, S.; Melpignano, A.; Vaudano, A.E.; Ravaglia, C.; et al. OSA and Prolonged Oxygen Desaturation During Sleep are Strong Predictors of Poor Outcome in IPF. Lung 2017, 195, 643–651. [Google Scholar] [CrossRef]
- Gille, T.; Didier, M.; Boubaya, M.; Moya, L.; Sutton, A.; Carton, Z.; Baran-Marszak, F.; Sadoun-Danino, D.; Israël-Biet, D.; Cottin, V.; et al. Obstructive Sleep Apnoea and Related Comorbidities in Incident Idiopathic Pulmonary Fibrosis. Eur. Respir. J. 2017, 49, 1601934. [Google Scholar] [CrossRef]
- Cardoso, A.V.; Pereira, N.; Neves, I.; Santos, V.; Jesus, J.M.; Melo, N.; Mota, P.C.; Morais, A.; Drummond, M. Obstructive Sleep Apnoea in Patients with Fibrotic Diffuse Parenchymal Lung Disease-Characterization and Treatment Compliance Assessment. Can. J. Respir. Ther. 2018, 54, 35–40. [Google Scholar] [CrossRef]
- Mavroudi, M.; Papakosta, D.; Kontakiotis, T.; Domvri, K.; Kalamaras, G.; Zarogoulidou, V.; Zarogoulidis, P.; Latka, P.; Huang, H.; Hohenforst-Schmidt, W.; et al. Sleep Disorders and Health-Related Quality of Life in Patients with Interstitial Lung Disease. Sleep Breath. 2017, 22, 393–400. [Google Scholar] [CrossRef]
- Canora, A.; Nicoletta, C.; Ghinassi, G.; Bruzzese, D.; Rea, G.; Capaccio, A.; Castaldo, S.; Coppola, A.; Polistina, G.E.; Sanduzzi, A.; et al. First Description of the Hyperpnea–Hypopnea Periodic Breathing in Patients with Interstitial Lung Disease-Obstructive Sleep Apnea: Treatment Implications in a Real-Life Setting. Int. J. Environ. Res. Public Health 2019, 16, 4712. [Google Scholar] [CrossRef]
- Tudorache, V.; Traila, D.; Marc, M.; Oancea, C.; Manolescu, D.; Tudorache, E.; Timar, B.; Albai, A.; Fira-Mladinescu, O. Impact of Moderate to Severe Obstructive Sleep Apnea on the Cognition in Idiopathic Pulmonary Fibrosis. PLoS ONE 2019, 14, e0211455. [Google Scholar] [CrossRef]
- Sarac, S.; Kavas, M.; Sahin, M.; Aras, G.; Afsar, G.C.; Tezel, Y.B. Relation of Warrick Score and Polysomnographic Parameters in Patients with Interstitial Lung Disease. Med Sci. Monit. 2019, 25, 2087–2095. [Google Scholar] [CrossRef]
- Pereira, N.; Cardoso, A.; Mota, P.; Santos, A.; Melo, N.; Morais, A.; Drummond, M. Predictive Factors of Obstructive Sleep Apnoea in Patients with Fibrotic Lung Diseases. Sleep Med. 2019, 56, 123–127. [Google Scholar] [CrossRef]
- Bosi, M.; Milioli, G.; Parrino, L.; Fanfulla, F.; Tomassetti, S.; Melpignano, A.; Trippi, I.; Vaudano, A.E.; Ravaglia, C.; Mascetti, S.; et al. Quality of Life in Idiopathic Pulmonary Fibrosis: The Impact of Sleep Disordered Breathing. Respir. Med. 2019, 147, 51–57. [Google Scholar] [CrossRef]
- Lee, J.H.; Park, C.S.; Song, J.W. Obstructive Sleep Apnea in Patients with Interstitial Lung Disease: Prevalence and Predictive Factors. PLoS ONE 2020, 15, e0239963. [Google Scholar] [CrossRef]
- Suomi, J.; Hess, G.; Won, C.; Bron, M.; Acquavella, J. Prevalence of Diagnosed Obstructive Sleep Apnea in the United States 2013-2016: Insured Patients Actively Seeking Care. J. Curr. Med Res. Opin. 2020, 3, 478–486. [Google Scholar] [CrossRef]
- Kassas, P.; Vavougios, G.D.; Hatzoglou, C.; Gourgoulianis, K.I.; Zarogiannis, S.G. Cross Sectional Study of the Community Self-Reported Risk of Obstructive Sleep Apnoea (OSA) and Awareness in Thessaly, Greece. Clocks Sleep 2022, 4, 16–22. [Google Scholar] [CrossRef]
- Demir, A.U.; Ardic, S.; Firat, H.; Karadeniz, D.; Aksu, M.; Ucar, Z.Z.; Sevim, S.; Ozgen, F.; Yilmaz, H.; Itil, O.; et al. Prevalence of Sleep Disorders in the Turkish Adult Population Epidemiology of Sleep Study. Sleep Biol. Rhythm. 2015, 13, 298–308. [Google Scholar] [CrossRef]
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef]
- Armeni, P.; Borsoi, L.; Costa, F.; Donin, G.; Gupta, A. Final Report Cost-of-Illness Study of Obstructive Sleep Apnea Syndrome (OSAS) in Italy. Rep. SDA Bocconi Sch. Manag. 2019. Available online: https://www.semanticscholar.org/paper/Final-report-Cost-of-illness-study-of-Obstructive-Armeni-Borsoi/e7ff5e80facbbdebe3cf0f3a5f0b16cdaa2110cd (accessed on 20 August 2022).
- Fuhrman, C.; Fleury, B.; Nguyên, X.-L.; Delmas, M.-C. Symptoms of Sleep Apnea Syndrome: High Prevalence and Underdiagnosis in the French Population. Sleep Med. 2012, 13, 852–858. [Google Scholar] [CrossRef]
- Rodrigues, A.; Pinto, P.; Nunes, B.; Bárbara, C. Obstructive Sleep Apnea: Epidemiology and Portuguese Patients Profile. Rev. Port. Pneumol. 2017, 23, 57–61. [Google Scholar] [CrossRef]
- Sleep Apnea in Canada, 2016 and 2017. Available online: https://www150.statcan.gc.ca/n1/pub/82-625-x/2018001/article/54979-eng.htm (accessed on 27 July 2022).
- Kim, J.; In, K.; Kim, J.; You, S.; Kang, K.; Shim, J.; Lee, S.; Lee, J.; Lee, S.; Park, C.; et al. Prevalence of Sleep-disordered Breathing in Middle-aged Korean Men and Women. Am. J. Respir. Crit. Care Med. 2004, 170, 1108–1113. [Google Scholar] [CrossRef]
- Caminati, A.; Lonati, C.; Cassandro, R.; Elia, D.; Pelosi, G.; Torre, O.; Zompatori, M.; Uslenghi, E.; Harari, S. Comorbidities in Idiopathic Pulmonary Fibrosis: An Underestimated Issue. Eur. Respir. Rev. 2019, 28, 190044. [Google Scholar] [CrossRef]
- Raghu, G.; Amatto, V.C.; Behr, J.; Stowasser, S. Comorbidities in Idiopathic Pulmonary Fibrosis Patients: A Systematic Literature Review. Eur. Respir. J. 2015, 46, 1113–1130. [Google Scholar] [CrossRef]
- Aronson, R.M.; Carley, D.W.; Önal, E.; Wilborn, J.; Lopata, M. Upper Airway Muscle Activity and the Thoracic Volume Dependence of Upper Airway Resistance. J. Appl. Physiol. 1991, 70, 430–438. [Google Scholar] [CrossRef]
- Won, C.H.; Kryger, M. Sleep in Patients with Restrictive Lung Disease. Clin. Chest Med. 2014, 35, 505–512. [Google Scholar] [CrossRef]
- A Sands, S.; I Terrill, P.A.; Edwards, B.; Taranto-Montemurro, L.; Azarbarzin, A.; Marques, M.; De Melo, C.M.; Loring, S.H.; Butler, J.P.; White, D.P.; et al. Quantifying the Arousal Threshold Using Polysomnography in Obstructive Sleep Apnea. Sleep 2017, 41, zsx183. [Google Scholar] [CrossRef]
- Pathophysiology of Upper Airway Obstruction in Obstructive Sleep Apnea in Adults-UpToDate. Available online: https://www.uptodate.com/contents/pathophysiology-of-upper-airway-obstruction-in-obstructive-sleep-apnea-in-adults (accessed on 27 July 2022).
- Khor, Y.H.; Ryerson, C.J.; Landry, S.A.; Howard, M.E.; Churchward, T.J.; Edwards, B.A.; Hamilton, G.S.; Joosten, S.A. Interstitial Lung Disease and Obstructive Sleep Apnea. Sleep Med. Rev. 2021, 58, 101442. [Google Scholar] [CrossRef]
- Cheng, Y.; Wang, Y.; Dai, L. The Prevalence of Obstructive Sleep Apnea in Interstitial Lung Disease: A Systematic Review and Meta-Analysis. Sleep Breath. 2021, 25, 1219–1228. [Google Scholar] [CrossRef]
- Lal, C.; Medarov, B.I.; Judson, M.A. Interrelationship Between Sleep-Disordered Breathing and Sarcoidosis. Chest 2015, 148, 1105–1114. [Google Scholar] [CrossRef]
- Antoniou, K.M.; Margaritopoulos, G.A.; Tomassetti, S.; Bonella, F.; Costabel, U.; Poletti, V. Interstitial Lung Disease. Eur. Respir. Rev. 2014, 23, 40–54. [Google Scholar] [CrossRef]
- Series, F.; Cormier, Y.; Lampron, N.; La Forge, J. Influence of Lung Volume in Sleep Apnoea. Thorax 1989, 44, 52–57. [Google Scholar] [CrossRef]
- Kirkness, J.P.; Madronio, M.; Stavrinou, R.; Wheatley, J.; Amis, T.C. Surface Tension of Upper Airway Mucosal Lining Liquid in Obstructive Sleep Apnea/Hypopnea Syndrome. Sleep 2005, 28, 457–463. [Google Scholar] [CrossRef][Green Version]
- Hilditch, C.J.; McEvoy, R.D.; George, K.E.; Thompson, C.C.; Ryan, M.; Rischmueller, M.; Catcheside, P.G. Upper Airway Surface Tension but not Upper Airway Collapsibility is Elevated in Primary Sjögren’s Syndrome. Sleep 2008, 31, 367–374. [Google Scholar] [CrossRef][Green Version]
- Usmani, Z.A.; Hlavac, M.; Rischmueller, M.; Heraganahally, S.S.; Hilditch, C.J.; Lester, S.; Catcheside, P.G.; Antic, N.A.; Chai-Coetzer, C.L.; McEvoy, R.D. Sleep disordered Breathing in Patients with Primary Sjögren’s Syndrome: A Group Controlled Study. Sleep Med. 2012, 13, 1066–1070. [Google Scholar] [CrossRef]
- Nathan, S.D.; Noble, P.W.; Tuder, R.M. Idiopathic Pulmonary Fibrosis and Pulmonary Hypertension: Connecting the Dots. Am J Respir Crit Care Med. 2007, 175, 875–880. [Google Scholar] [CrossRef]
- Kholdani, C.; Fares, W.H.; Mohsenin, V. Pulmonary Hypertension in Obstructive Sleep Apnea: Is it Clinically Significant? A Critical Analysis of the Association and Pathophysiology. Pulm. Circ. 2015, 5, 220–227. [Google Scholar] [CrossRef]
- Trakada, G.; Nikolaou, E.; Pouli, A.; Tsiamita, M.; Spiropoulos, K. Endothelin-1 Levels in Interstitial Lung Disease Patients During Sleep. Sleep Breath. 2003, 7, 111–118. [Google Scholar] [CrossRef]
- Wang, Z.; Li, A.-Y.; Guo, Q.-H.; Zhang, J.-P.; An, Q.; Guo, Y.-J.; Chu, L.; Weiss, J.W.; Ji, E.-S. Effects of Cyclic Intermittent Hypoxia on ET-1 Responsiveness and Endothelial Dysfunction of Pulmonary Arteries in Rats. PLoS ONE 2013, 8, e58078. [Google Scholar] [CrossRef]
- Foresi, A.; Leone, C.; Olivieri, D.; Cremona, G. Alveolar-Derived Exhaled Nitric Oxide Is Reduced in Obstructive Sleep Apnea Syndrome. Chest 2007, 132, 860–867. [Google Scholar] [CrossRef]
- Rajagopal, K.; Bryant, A.J.; Sahay, S.; Wareing, N.; Zhou, Y.; Pandit, L.M.; Karmouty-Quintana, H. Idiopathic Pulmonary Fibrosis and Pulmonary Hypertension: Heracles Meets the Hydra. J. Cereb. Blood Flow Metab. 2020, 178, 172–186. [Google Scholar] [CrossRef]
- Pillai, M.; Lee-Chiong, T.; Hanna, P.; Swigris, J. Obstructive Sleep Apnea (OSA) and Gastroesophageal Reflux Disease (GERD) Are Common in Patients with Fibrotic Interstitial Lung Disease (Fild). Chest 2011, 140, 792A. [Google Scholar] [CrossRef]
- Durgan, D.J.; Bryan, R.M. Cerebrovascular Consequences of Obstructive Sleep Apnea. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Disease. 2012, 1, e000091. [Google Scholar] [CrossRef]
- Schiza, S.; Mermigkis, C.; Margaritopoulos, G.A.; Daniil, Z.; Harari, S.; Poletti, V.; Renzoni, E.; Torre, O.; Visca, D.; Bouloukaki, I.; et al. Idiopathic Pulmonary Fibrosis and Sleep Disorders: No Longer Strangers in the Night. Eur. Respir. Rev. 2015, 24, 327–339. [Google Scholar] [CrossRef]
- Mermigkis, C.; Mermigkis, D.; Varouchakis, G.; Schiza, S. CPAP Treatment in Patients with Idiopathic Pulmonary Fibrosis and Obstructive Sleep Apnea—Therapeutic Difficulties and Dilemmas. Sleep Breath. 2011, 16, 1–3. [Google Scholar] [CrossRef]
- Sériès, F.; Cormier, Y.; LaForge, J. Influence of Continuous Positive Airway Pressure on Sleep Apnea-Related Desaturation in Sleep Apnea Patients. Lung 1992, 170, 281–290. [Google Scholar] [CrossRef]
- Mermigkis, C.; Bouloukaki, I.; Antoniou, K.M.; Mermigkis, D.; Psathakis, K.; Giannarakis, I.; Varouchakis, G.; Siafakas, N.; Schiza, S.E. CPAP Therapy in Patients with Idiopathic Pulmonary Fibrosis and Obstructive Sleep Apnea: Does It Offer a Better Quality of Life and Sleep? Sleep Breath. 2013, 17, 1137–1143. [Google Scholar] [CrossRef]
- Alchanatis, M.; Tourkohoriti, G.; Kakouros, S.; Kosmas, E.; Podaras, S.; Jordanoglou, J.B. Daytime Pulmonary Hypertension in Patients with Obstructive Sleep Apnea: The Effect of Continuous Positive Airway Pressure on Pulmonary Hemodynamics. Respiration 2001, 68, 566–572. [Google Scholar] [CrossRef]
- Sajkov, D.; Wang, T.; Saunders, N.A.; Bune, A.J.; McEVOY, R.D. Continuous Positive Airway Pressure Treatment Improves Pulmonary Hemodynamics in Patients with Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2002, 165, 152–158. [Google Scholar] [CrossRef]
- Arizono, S.; Furukawa, T.; Taniguchi, H.; Sakamoto, K.; Kimura, T.; Kataoka, K.; Ogawa, T.; Watanabe, F.; Kondoh, Y. Supplemental Oxygen Improves Exercise Capacity in IPF Patients with Exertional Desaturation. Respirology 2020, 25, 1152–1159. [Google Scholar] [CrossRef]
- Böing, S.; Randerath, W.J. Chronic Hypoventilation Syndromes and Sleep-Related Hypoventilation. J. Thorac. Dis. 2015, 7, 1273–1285. [Google Scholar] [CrossRef]
- Berthon-Jones, M.; E Sullivan, C. Time Course of Change in Ventilatory Response to CO2 with Long-Term CPAP Therapy for Obstructive Sleep Apnea. Am. Rev. Respir. Dis. 1987, 135, 144–147. [Google Scholar] [CrossRef]
- Plantier, L.; Cazes, A.; Dinh-Xuan, A.-T.; Bancal, C.; Marchand-Adam, S.; Crestani, B. Physiology of the Lung in Idiopathic Pulmonary Fibrosis. Eur. Respir. Rev. 2018, 27, 170062. [Google Scholar] [CrossRef]
- Lederer, D.J.; Jelic, S.; Basner, R.C.; Ishizaka, A.; Bhattacharya, J. Circulating KL-6, a Biomarker of Lung Injury, in Obstructive Sleep Apnoea. Eur. Respir. J. 2009, 33, 793–796. [Google Scholar] [CrossRef]
- Aihara, K.; Oga, T.; Harada, Y.; Chihara, Y.; Handa, T.; Tanizawa, K.; Watanabe, K.; Tsuboi, T.; Hitomi, T.; Mishima, M.; et al. Comparison of Biomarkers of Subclinical Lung Injury in Obstructive Sleep Apnea. Respir. Med. 2011, 105, 939–945. [Google Scholar] [CrossRef]
- Lederer, D.J.; Jelic, S.; Basner, R.C.; Bhattacharya, J. Is Obstructive Sleep Apnea a Cause of Idiopathic Pulmonary Fibrosis? Arch. Pathol. Lab. Med. 2012, 136, 470. [Google Scholar] [CrossRef]
- Kim, J.S.; Podolanczuk, A.J.; Borker, P.; Kawut, S.M.; Raghu, G.; Kaufman, J.D.; Stukovsky, K.D.H.; Hoffman, E.A.; Barr, R.G.; Gottlieb, D.J.; et al. Obstructive Sleep Apnea and Subclinical Interstitial Lung Disease in the Multi-Ethnic Study of Atherosclerosis (MESA). Ann. Am. Thorac. Soc. 2017, 14, 1786–1795. [Google Scholar] [CrossRef]

| Database | Search Query |
|---|---|
| PubMed (on PubMed.gov (accessed on 4 October 2021)) | (“Idiopathic Pulmonary Fibrosis”[Mesh] OR “IPF”) AND (“Sleep Apnea, Obstructive”[Mesh] OR “OSA”) |
| PubMed Central (PMC) | “OSA AND IPF” |
| Scopus (on Scopus.com (accessed on 4 October 2021)) | (TITLE-ABS-KEY (obstructive AND sleep AND apnea OR osa) AND TITLE-ABS-KEY (idiopathic AND pulmonary AND fibrosis OR ipf)) AND (LIMIT-TO (SUBJAREA, “MEDI”)) |
| Embase (on Ovid) | 1# idiopathic pulmonary fibrosis.mp. or exp fibrosing alveolitis 2# IPF.mp. 3# 1 OR 2 4# sleep apnea syndrome.mp. or exp sleep disordered breathing 5# (sleep adj3 (apnea or apnoea or hypopnea)).ti,ab. 6# OSA.mp. 7# 4 OR 5 OR 6 8# 3 AND 7 |
| Paper | Year | Mean/Median Age of IPF Patients | Mean/Median BMI | IPF–Total | IPF Severity (FVC% Predicted) | IPF–OSA | Referral OSA Prevalence in Ethnically Matched Population | Mean/Median Age of General Population Study | Reference to OSA Prevalence |
|---|---|---|---|---|---|---|---|---|---|
| Lancaster et al. [5] | 2009 | 64.9 | 32.3 | 50 | ND | 44.0 (88.0%) | 3.4% | 58.0 | [48] |
| Mermigkis et al. [33] | 2010 | 65 ± 10.6 | 27.3±4.0 | 34 | 72.5±18.1 | 20.0 (58.8%) | 26.8% | 54.1 ± 16.1 | [49] |
| Pillai et al. [34] | 2012 | 69.2 ± 7.0 | 30.4 ± 6.9 | 54 | 64.0 ± 15.9 | 35.0 (64.8%) | 3.4% | 58.0 | [48] |
| Kolilekas et al. [35] | 2013 | 67.96 ± 7.88 | 28,7 ± 4.3 | 31 | 77.6 ± 17.1 | 28.0 (90.3%) | 26.8% | 54.1 ± 16.1 | [49] |
| Pihtiliet al. [31] | 2013 | 60.94 ± 8.11 | 26.4±2.0 | 17 | 79.0 ± 23.9 | 14.0 (82.4%) | 13.7% | 40.7 ± 15.1 | [50] |
| Lee et al. [36] | 2015 | 67.9 ± 12.3 | 28.5 ± 4.6 | 20 | 82.2 ± 15.3 | 9.0 (45.0%) | 3.4% | 58.0 | [48] |
| Mermigkiset al. [32] | 2015 | 70.3 ± 7.9 | ND | 92 | ND | 78.0 (84.0%) | 26.0% | 54.1 ± 16.1 | [49] |
| Schertel et al. [37] | 2017 | 67.0 (IQR: 60.0–77.0) | 24.9 (IQR: 24.0–29.8) | 9 | 58 (IQR: 56–77) | 6.0 (66.7%) | 19.0% | 57.0 (IQR: 49.0–68.0) | [51] |
| Bosi et al. [38] | 2017 | 68.7 ± 9.2 | 22.7 ± 3.7 | 35 | 72.2 ± 19.6 | 25.9 (71.4%) | 72.0% | 40.0–85.0 | [52] |
| Gille et al. [39] | 2017 | 68.8 ± 8.7 | 28 ± 3.5 | 45 | 72.8 ± 20.3 | 40.0 (88.9%) | 4.9% | 46.8 | [53] |
| Cardoso et al. [40] | 2018 | >60.0 | <30.0 | 12 | 86.1 ± 18.9 | 10.0 (83.3%) | 0.9% | 62.8 (95%CI: 61.6–64.1) | [54] |
| Mavroudi et al. [41] | 2018 | 69.8 ± 8.1 | 29.2 ± 5.3 | 19 | 75.6 ± 16.2 | 15.0 (79.0%) | 26.8% | 54.10 ± 16.1 | [49] |
| Canora et al. [42] | 2019 | 69 ± 7.8 | 28.7 | 54 | 71.5 ± 23.2 | 42.0 (77.8%) | 72.0% | 40.0–85.0 | [52] |
| Tudorache et al. [43] | 2019 | 67.6 ± 8.7 | 27.7 ± 4.5 | 23 | 71.3 ± 16.4 | 19.0 (82.6%) | 6.4% | >18.0 | [55] |
| Sarac et al. [44] | 2019 | 62.0 ± 9.4 | 27.9 ± 4.8 | 16 | 71.0 (62.0–85.3) | 12.0 (75.0%) | 13.7% | 40.7 ± 15.1 | [50] |
| Pereira et al. [45] | 2019 | 67.16 ± 12.18 | 25.6 ± 2.9 | 12 | 86.1 ± 18.9 | 10.0 (83.3%) | 0.9% | 62.8 (95% CI: 61.6–64.1) | [54] |
| Bosi et al. [46] | 2019 | 69.7 (IQR: 64.8–74.7) | 21.9 | 34 | 75.5 (IQR: 56.8–87.0) | 25.0 (73.5%) | 72.0% | 40.0–85.0 | [52] |
| Lee et al. [47] | 2020 | 72.5 ± 7.2 | 24.1 ± 3.6 | 57 | 72.4 ± 14.8 | 37.0 (64.9%) | 23.0% | 49.6 ± 7.7 | [56] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karuga, F.F.; Kaczmarski, P.; Szmyd, B.; Białasiewicz, P.; Sochal, M.; Gabryelska, A. The Association between Idiopathic Pulmonary Fibrosis and Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 5008. https://doi.org/10.3390/jcm11175008
Karuga FF, Kaczmarski P, Szmyd B, Białasiewicz P, Sochal M, Gabryelska A. The Association between Idiopathic Pulmonary Fibrosis and Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(17):5008. https://doi.org/10.3390/jcm11175008
Chicago/Turabian StyleKaruga, Filip Franciszek, Piotr Kaczmarski, Bartosz Szmyd, Piotr Białasiewicz, Marcin Sochal, and Agata Gabryelska. 2022. "The Association between Idiopathic Pulmonary Fibrosis and Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 17: 5008. https://doi.org/10.3390/jcm11175008
APA StyleKaruga, F. F., Kaczmarski, P., Szmyd, B., Białasiewicz, P., Sochal, M., & Gabryelska, A. (2022). The Association between Idiopathic Pulmonary Fibrosis and Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 11(17), 5008. https://doi.org/10.3390/jcm11175008









