Robot-Assisted Pedicle Screw Placement Led to Lower Screw Loosening Rate than Fluoroscopy-Guided Technique in Transforaminal Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Single-Center Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. FG TLIF Procedure
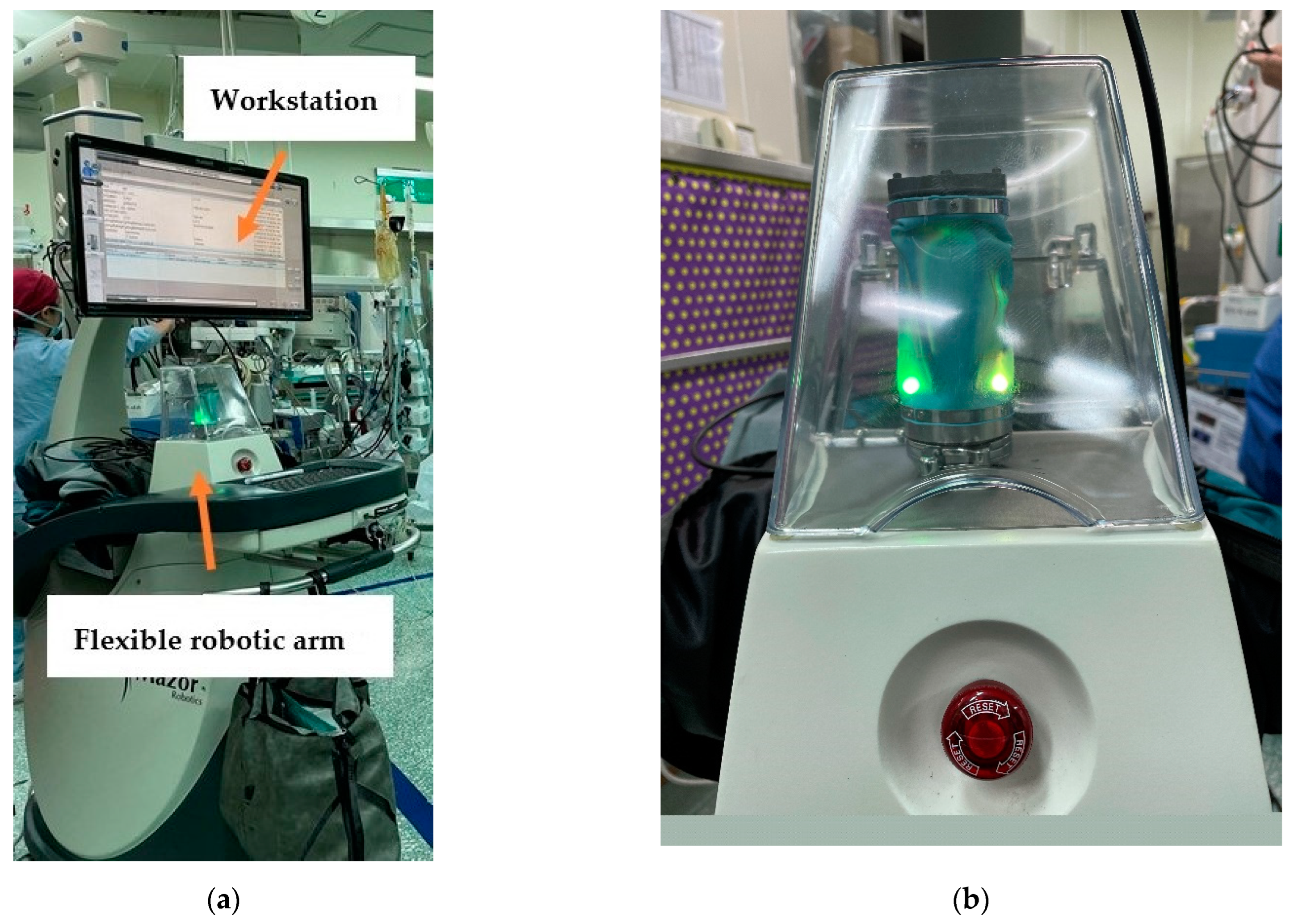
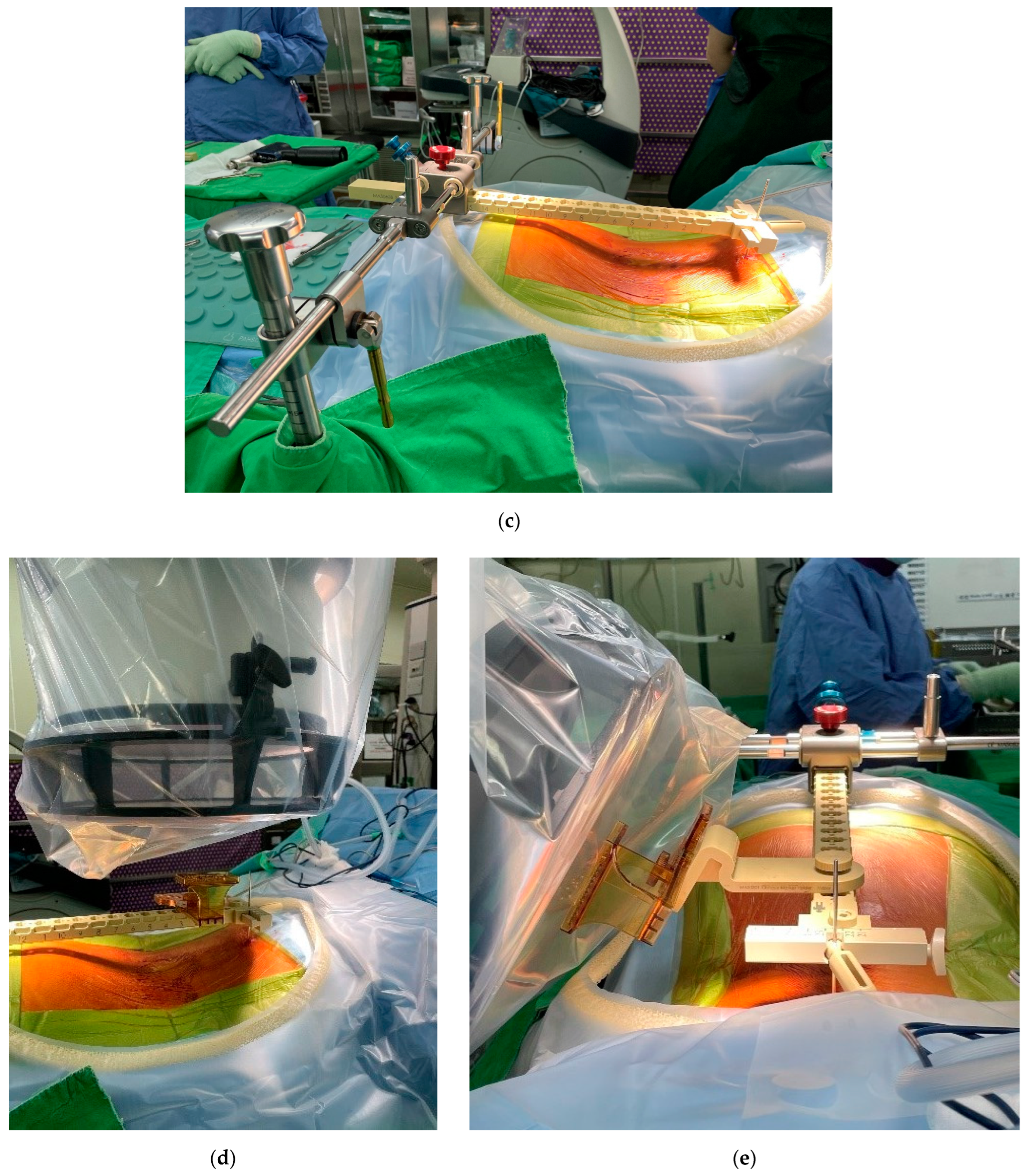
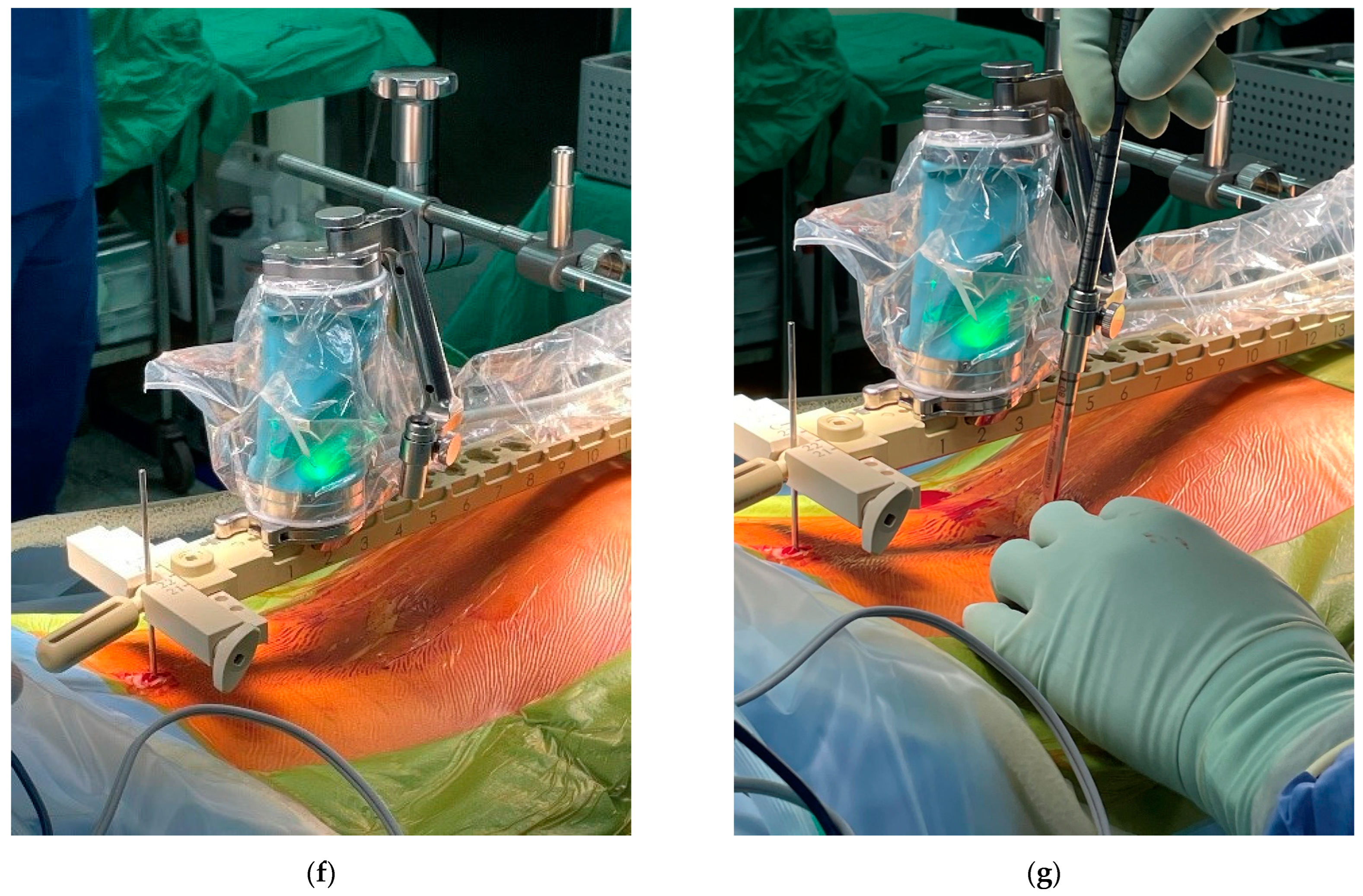
2.3. Ro TLIF Procedure
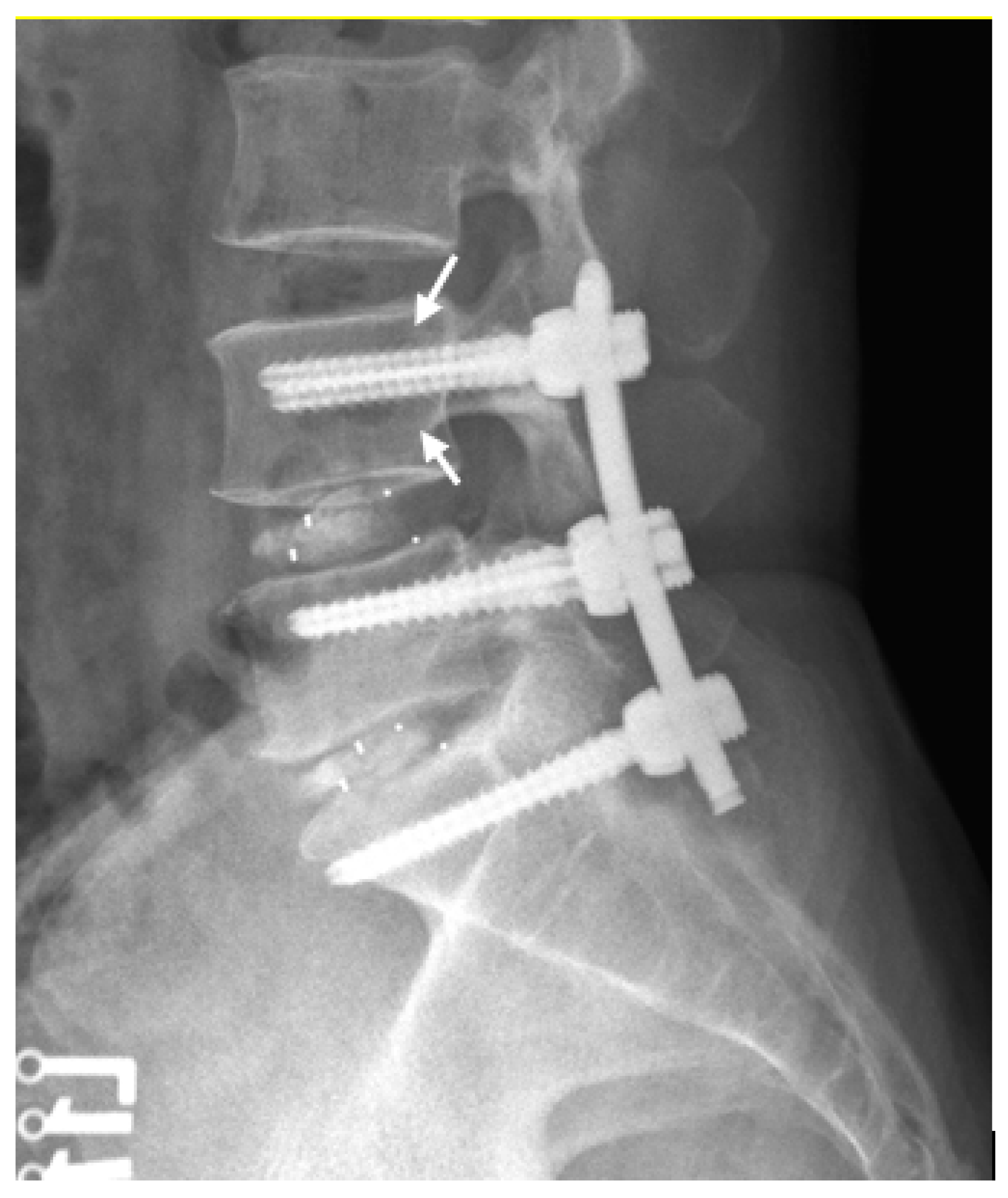
2.4. Measurements of Radiographic Parameters
2.5. Definition of Screw Loosening and Cage Subsidence
2.6. Clinical Outcomes
2.7. Statistical Analysis
3. Results
3.1. Patients’ Profile
3.2. Perioperative and Postoperative Outcomes
3.3. Pedicle Screw Measurements in the FG TLIF and Ro TLIF Groups
3.4. Intraclass Correlation Coefficient (ICC) for Pedicle Screw Measurements
3.5. Screw Loosening Risk Factor Variables
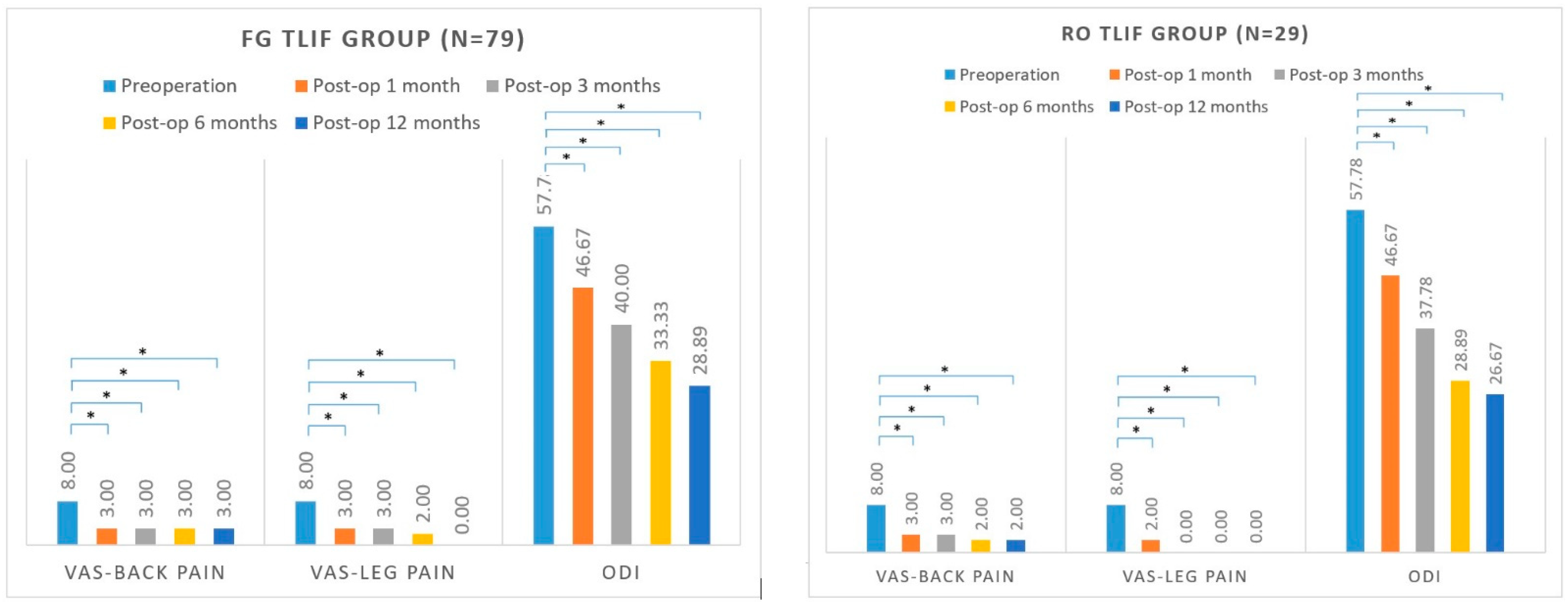
3.6. Patient-Reported Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boucher, H.H. A method of spinal fusion. J. Bone Joint Surg. 1959, 41, 248–259. [Google Scholar] [CrossRef]
- Zhang, Q.; Han, X.G.; Xu, Y.F.; Liu, Y.J.; Liu, B.; He, D.; Sun, Y.Q.; Tian, W. Robot-Assisted Versus Fluoroscopy-Guided Pedicle Screw Placement in Transforaminal Lumbar Interbody Fusion for Lumbar Degenerative Disease. World Neurosurg. 2019, 125, 429–434. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, D.M.; Westrup, A.M.; O’Neal, C.M.; Lee, B.J.; Shi, H.H.; Dunn, I.F.; Snyder, L.A.; Smith, Z.A. Robotics in spine surgery: A systematic review. J. Clin. Neurosci. 2021, 89, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Cui, G.Y.; Han, X.G.; Wei, Y.; Liu, Y.J.; He, D.; Sun, Y.Q.; Liu, B.; Tian, W. Robot-Assisted Minimally Invasive Trans-foraminal Lumbar Interbody Fusion in the Treatment of Lumbar Spondylolisthesis. Orthop. Surg. 2021, 13, 1960–1968. [Google Scholar] [CrossRef] [PubMed]
- Kantelhardt, S.R.; Martinez, R.; Baerwinkel, S.; Burger, R.; Giese, A.; Rohde, V. Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur. Spine J. 2011, 20, 860–868. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Jung, W.I.; Chang, B.S.; Lee, C.K.; Kang, K.T.; Yeom, J.S. A prospective, randomized, controlled trial of robot-assisted vs. freehand pedicle screw fixation in spine surgery. Int. J. Med. Robot. Comput. Assist. Surg. 2017, 13, e1779. [Google Scholar] [CrossRef] [PubMed]
- Hyun, S.J.; Kim, K.J.; Jahng, T.A.; Kim, H.J. Minimally Invasive Robotic Versus Open Fluoroscopic-guided Spinal Instrumented Fusions: A Randomized Controlled Trial. Spine 2017, 42, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Biase, G.; Gassie, K.; Garcia, D.; Abode-Iyamah, K.; Deen, G.; Nottmeier, E.; Chen, S. Perioperative Comparison of Robotic-Assisted Versus Fluoroscopically Guided Minimally Invasive Transforaminal Lumbar Interbody Fusion. World Neurosurg. 2021, 149, 570–575. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.C.; Huang, W.C.; Tsai, H.W.; Ko, C.C.; Wu, C.L.; Tu, T.H.; Cheng, H. Pedicle screw loosening in dynamic stabilization: Incidence, risk, and outcome in 126 patients. Neurosurg. Focus 2011, 31, E9. [Google Scholar] [CrossRef]
- Galbusera, F.; Volkheimer, D.; Reitmaier, S.; Berger-Roscher, N.; Kienle, A.; Wilke, H.J. Pedicle screw loosening: A clinically relevant complication? Eur. Spine J. 2015, 24, 1005–1016. [Google Scholar] [CrossRef]
- Bokov, A.; Bulkin, A.; Aleynik, A.; Kutlaeva, M.; Mlyavykh, S. Pedicle Screws Loosening in Patients with Degenerative Diseases of the Lumbar Spine: Potential Risk Factors and Relative Contribution. Global Spine J. 2019, 9, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Ohba, T.; Ebata, S.; Oba, H.; Koyama, K.; Haro, H. Risk Factors for Clinically Relevant Loosening of Percutaneous Pedicle Screws. Spine Surg. Relat. Res. 2018, 3, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, K.; Abe, E.; Suzuki, T.; Tamura, Y.; Chiba, M.; Sato, K. Posterior lumbar interbody fusion: A retrospective study of complications after facet joint excision and pedicle screw fixation in 148 cases. Acta Orthop. Scand. 1999, 70, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, K.; Abe, E.; Suzuki, T.; Tamura, Y.; Chiba, M.; Sato, K. Can insertional torque predict screw loosening and related failures? An in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine 2000, 25, 858–864. [Google Scholar] [CrossRef]
- Okuyama, K.; Abe, E.; Suzuki, T.; Tamura, Y.; Chiba, M.; Sato, K. Influence of bone mineral density on pedicle screw fixation: A study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J. 2001, 1, 402–407. [Google Scholar] [CrossRef]
- Sanden, B.; Olerud, C.; Petren-Mallmin, M.; Johansson, C.; Larsson, S. The significance of radiolucent zones surrounding pedicle screws. Definition of screw loosening in spinal instrumentation. J. Bone Joint Surg. 2004, 86, 457–461. [Google Scholar] [CrossRef]
- Ozawa, T.; Takahashi, K.; Yamagata, M.; Ohtori, S.; Aoki, Y.; Saito, T.; Inoue, G.; Ito, T.; Moriya, H. Insertional torque of the lumbar pedicle screw during surgery. J. Orthop. Sci. 2005, 10, 133–136. [Google Scholar] [CrossRef]
- Marchi, L.; Abdala, N.; Oliveira, L.; Amaral, R.; Coutinho, E.; Pimenta, L. Stand-alone lateral interbody fusion for the treatment of low-grade degenerative spondylolisthesis. Sci. World J. 2012, 2012, 456346. [Google Scholar] [CrossRef]
- Berjano, P.; Bassani, R.; Casero, G.; Sinigaglia, A.; Cecchinato, R.; Lamartina, C. Failures and revisions in surgery for sagittal imbalance: Analysis of factors influencing failure. Eur. Spine J. 2013, 22 (Suppl. S6), S853–S858. [Google Scholar] [CrossRef]
- McLachlin, S.D.; Beaton, B.J.B.; Sabo, M.T.; Gurr, K.R.; Bailey, S.I.; Bailey, C.S.; Dunning, C.E. Comparing the fixation of a novel hollow screw versus a conventional solid screw in human sacra under cyclic loading. Spine 2008, 33, 1870–1875. [Google Scholar] [CrossRef] [Green Version]
- Kim, D.H.; Hwang, R.W.; Lee, G.H.; Joshi, R.; Baker, K.C.; Arnold, P.; Sasso, R.; Park, D.; Fischgrund, J. Comparing rates of early pedicle screw loosening in posterolateral lumbar fusion with and without transforaminal lumbar interbody fusion. Spine J. 2020, 20, 1438–1445. [Google Scholar] [CrossRef] [PubMed]

| FG TLIF Group (n = 79) | Ro TLIF Group (n = 29) | p Value | |
|---|---|---|---|
| Age (years) | 64.0 [54.5, 71.0] | 66.0 [60.0, 76.5] | 0.213 |
| Sex | 0.700 | ||
| Female (%) | 46 (58.2%) | 15 (51.7%) | |
| Male (%) | 33 (41.8%) | 14 (48.3%) | |
| BMI (kg/m2) | 25.9 [23.4, 29.0] | 27.4 [23.3, 30.6] | 0.448 |
| DM | 21 (26.6%) | 7 (24.1%) | 0.993 |
| Diagnosis | 0.014 * | ||
| Spinal stenosis (%) | 21 (26.6%) | 17 (58.6%) | |
| Spondylolisthesis (%) | 44 (55.7%) | 10 (34.5%) | |
| Spondylolysis (%) | 8 (10.1%) | 2 (6.9%) | |
| Other degenerative disease (%) | 6 (7.6%) | 0 (0.0%) | |
| Number of level(s) fused | 0.499 | ||
| One (%) | 39 (49.4%) | 18 (62.1%) | |
| L1/L2 | 1 (1.3%) | 0 (0.0%) | |
| L2/L3 | 2 (2.5%) | 0 (0.0%) | |
| L3/L4 | 1 (1.3%) | 2 (6.9%) | |
| L4/L5 | 22 (27.8%) | 12 (41.4%) | |
| L5/L6 | 0 (0.0%) | 1 (3.4%) | |
| L5/S1 | 13 (16.5%) | 3 (10.3%) | |
| Two (%) | 32 (40.5%) | 9 (31.0%) | |
| L2/L3/L4 | 1 (1.3%) | 1 (3.4%) | |
| L3/L4/L5 | 14 (17.7%) | 5 (17.2%) | |
| L4/L5/L6 | 0 (0.0%) | 1 (3.4%) | |
| L4/L5/S1 | 17 (21.5%) | 2 (6.9%) | |
| Three (%) | 8 (10.1%) | 2 (6.9%) | |
| L2/L3/L4/L5 | 2 (2.5%) | 0 (0.0%) | |
| L3/L4/L5/S1 | 6 (7.6%) | 1 (3.4%) | |
| L4/L5/S1/S2 | 0 (0.0%) | 1 (3.4%) | |
| Cage type | 1.000 | ||
| Trabecular Metal (%) | 19 (24.1%) | 7 (24.1%) | |
| Polyetheretherketone (%) | 60 (75.9%) | 22 (75.9%) | |
| Screw type | <0.001 * | ||
| Solid (%) | 60 (75.9%) | 0 (0.0%) | |
| Hollow (%) | 19 (24.1%) | 29 (100.0%) | |
| Pre-op pain VAS—leg | 8.0 [7.0, 10.0] | 8.0 [6.0, 9.5] | 1.000 |
| Pre-op pain VAS—back | 8.0 [6.0, 9.0] | 8.0 [6.0, 9.0] | 0.972 |
| Preoperative ODI | 57.78 [51.11, 64.44] | 57.78 [47.78, 71.11] | 0.868 |
| FG TLIF Group (n = 79) | Ro TLIF Group (n = 29) | p Value | |
|---|---|---|---|
| Blood loss for single-level TLIF (mL) | 366.7 [300.0, 600.0] | 400.0 [250.0, 675.0] | 0.677 |
| Operative time for single-level TLIF (min) | 225.0 [170.0, 293.0] | 259.0 [222.8, 296.5] | 0.101 |
| Length of hospital stay (days) | 6.0 [5.0, 8.0] | 7.0 [6.0, 8.0] | 0.090 |
| Complication (%) | 19 (24.1%) | 7 (24.1%) | 1.000 |
| Complication requiring revision surgery (%) | 1 (1.3%) | 0 (0%) | 1.000 |
| FG TLIF Group (n = 412) | Ro TLIF Group (n = 140) | p Value | |
|---|---|---|---|
| Distance from pedicle screw to upper endplate/vertebral body height | 0.39 [0.36, 0.42] | 0.35 [0.29, 0.37] | <0.001 * |
| Distance from screw tip to anterior cortex/vertebral body AP diameter | 0.14 [0.06, 0.22] | 0.12 [0.04, 0.19] | 0.124 |
| Screw loosening (%) | 42 (10.2%) | 6 (4.3%) | 0.049 * |
| Screw Loosening Group (n = 48) | Non-Screw Loosening Group (n = 504) | p Value | |
|---|---|---|---|
| Distance from pedicle screw to upper endplate/ vertebral body height | 0.40 [0.38, 0.41] | 0.37 [0.34, 0.41] | <0.001 * |
| Distance from screw tip to anterior cortex/ vertebral body AP diameter | 0.16 [0.06, 0.25] | 0.13 [0.05, 0.20] | 0.100 |
| Components of Regression Model | Odds Ratio per Unit Change [95% CI] | p Value |
|---|---|---|
| Age | 1.12 [1.04, 1.20] | 0.001 * |
| Sex | ||
| Female | Reference | |
| Male | 1.19 [0.42, 3.35] | 0.749 |
| BMI | 0.91 [0.80, 1.04] | 0.177 |
| Diagnosis | ||
| Spinal stenosis | Reference | |
| Spondylolisthesis | 0.93 [0.29, 2.93] | 0.898 |
| Spondylolysis | 0.59 [0.06, 5.58] | 0.647 |
| Other degenerative disease | 2.67 [0.40, 17.98] | 0.314 |
| Number of level(s) fused | ||
| 1 | Reference | |
| 2 | 2.52 [0.76, 8.37] | 0.131 |
| 3 | 6.93 [1.45, 33.09] | 0.015 * |
| Screw type | ||
| Hollow screw | Reference | |
| Solid screw | 1.17 [0.41, 3.35] | 0.768 |
| Cage type | ||
| Polyetheretherketone | Reference | |
| Trabecular Metal | 0.63 [0.17, 2.40] | 0.502 |
| Distance from pedicle screw to upper endplate/vertebral body height | 63.24 [1.83, 2181.2] | 0.022 * |
| Distance from screw tip to anterior cortex/vertebral body AP diameter | 2.09 [0.23, 18.75] | 0.509 |
| FG TLIF Group (n = 79) | Ro TLIF Group (n = 29) | p Value | |
|---|---|---|---|
| △VAS-Back-1 | −4.0 [−6.0, −3.0] | −5.0 [−7.0, −3.0] | 0.321 |
| △VAS-Back-3 | −5.0 [−7.0, −3.0] | −6.0 [−7.0, −4.0] | 0.569 |
| △VAS-Back-6 | −5.0 [−7.0, −3.0] | −6.0 [−8.0, −4.0] | 0.392 |
| △VAS-Back-12 | −5.0 [−7.0, −3.0] | −6.0 [−8.0, −3.0] | 0.304 |
| △VAS-Leg-1 | −5.0 [−6.0, −3.0] | −6.0 [−8.0, −4.0] | 0.137 |
| △VAS-Leg-3 | −5.0 [−7.0, −3.0] | −6.0 [−8.0, −4.0] | 0.237 |
| △VAS-Leg-6 | −6.0 [−8.0, −4.0] | −7.0 [−8.5, −4.0] | 0.278 |
| △VAS-Leg-12 | −6.0 [−8.0, −4.0] | −7.0 [−8.0, −3.0] | 0.936 |
| △ODI-1 | −11.11 [−17.78, −4.45] | −13.33 [−21.11, −2.22] | 0.579 |
| △ODI-3 | −20.00 [−26.66, −11.11] | −20.00 [−30.00, −7.78] | 0.768 |
| △ODI-6 | −24.44 [−35.55, −13.34] | −26.67 [−35.56, −16.66] | 0.456 |
| △ODI-12 | −26.67 [−35.56, −15.56] | −31.11 [−38.89, −23.33] | 0.295 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lai, Y.-P.; Lin, Y.-H.; Wu, Y.-C.; Shih, C.-M.; Chen, K.-H.; Lee, C.-H.; Pan, C.-C. Robot-Assisted Pedicle Screw Placement Led to Lower Screw Loosening Rate than Fluoroscopy-Guided Technique in Transforaminal Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Single-Center Retrospective Study. J. Clin. Med. 2022, 11, 4989. https://doi.org/10.3390/jcm11174989
Lai Y-P, Lin Y-H, Wu Y-C, Shih C-M, Chen K-H, Lee C-H, Pan C-C. Robot-Assisted Pedicle Screw Placement Led to Lower Screw Loosening Rate than Fluoroscopy-Guided Technique in Transforaminal Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Single-Center Retrospective Study. Journal of Clinical Medicine. 2022; 11(17):4989. https://doi.org/10.3390/jcm11174989
Chicago/Turabian StyleLai, Yen-Po, Yu-Hsien Lin, Yun-Che Wu, Cheng-Min Shih, Kun-Hui Chen, Cheng-Hung Lee, and Chien-Chou Pan. 2022. "Robot-Assisted Pedicle Screw Placement Led to Lower Screw Loosening Rate than Fluoroscopy-Guided Technique in Transforaminal Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Single-Center Retrospective Study" Journal of Clinical Medicine 11, no. 17: 4989. https://doi.org/10.3390/jcm11174989
APA StyleLai, Y.-P., Lin, Y.-H., Wu, Y.-C., Shih, C.-M., Chen, K.-H., Lee, C.-H., & Pan, C.-C. (2022). Robot-Assisted Pedicle Screw Placement Led to Lower Screw Loosening Rate than Fluoroscopy-Guided Technique in Transforaminal Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Single-Center Retrospective Study. Journal of Clinical Medicine, 11(17), 4989. https://doi.org/10.3390/jcm11174989






