Analysis of White and Dark without Pressure in a Young Myopic Group Based on Ultra-Wide Swept-Source Optical Coherence Tomography Angiography
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Assessment of Dark and White without Pressure
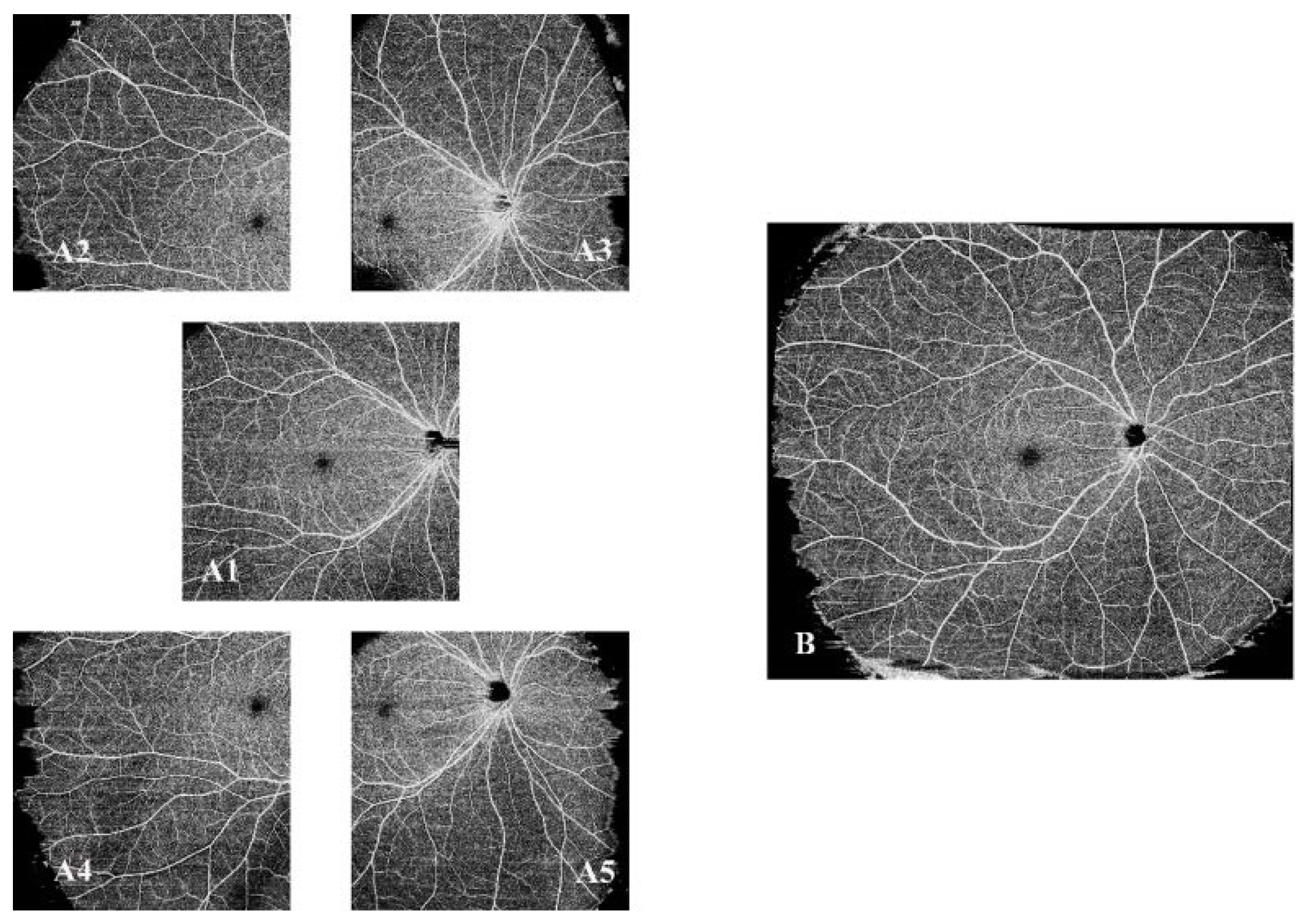
2.3. SS-OCTA Image Acquisition and Processing
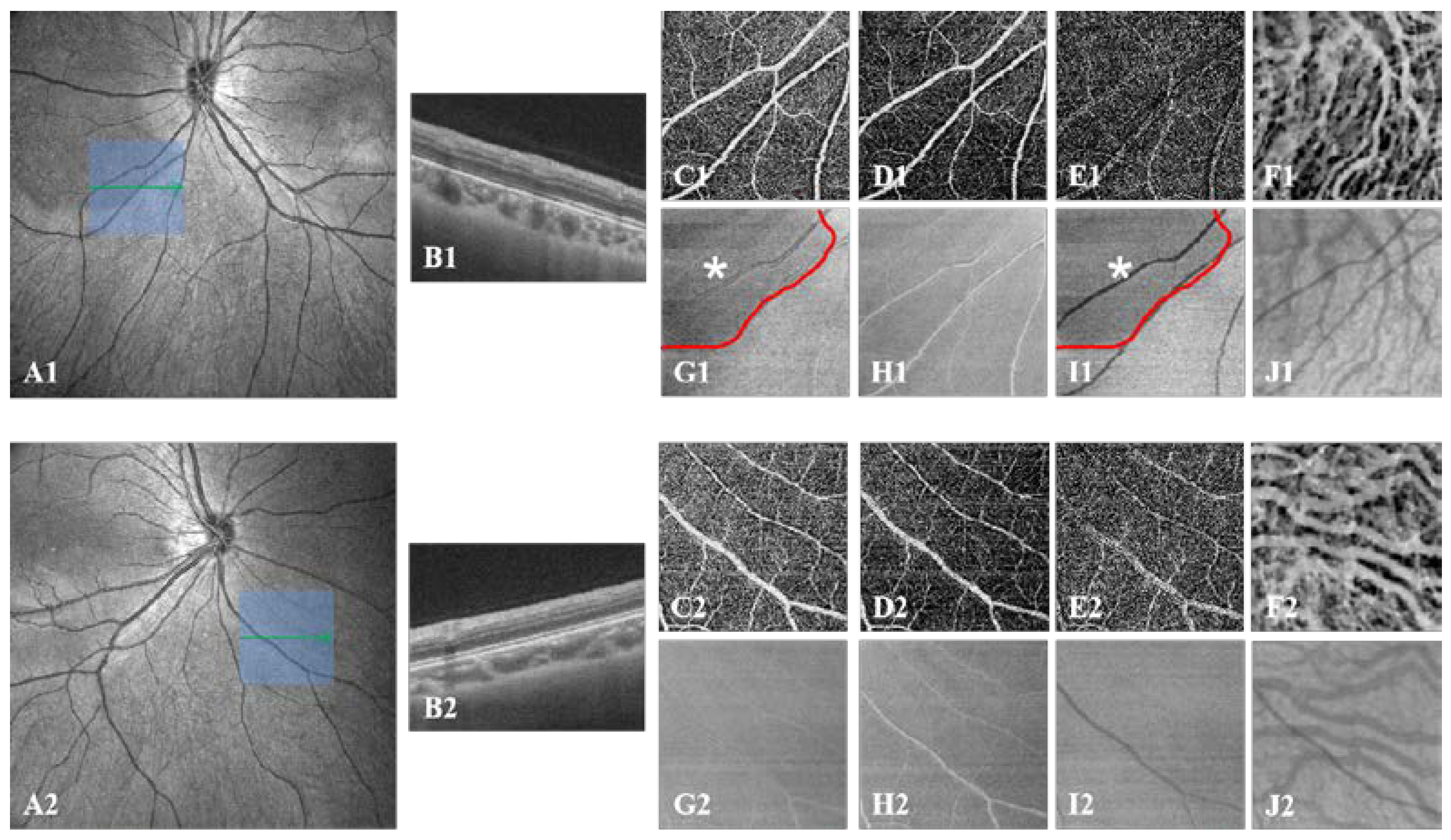
2.4. SS-OCTA Image Quantification of DWOP Lesion Areas
2.5. Reproducibility of SS-OCTA Measurements
2.6. Statistical Analysis
3. Results
3.1. Repeatability of Retinal and Choroidal Structural Measurement
3.2. The Incidence Rate of WWOP and DWOP
3.3. Risk Factors for WWOP and DWOP
3.4. OCTA Quantitative Change in DWOP Lesions
4. Discussion
4.1. Incidence Rate and Risk Factors of WWOP and DWOP
4.2. The Mechanisms of WWOP and DWOP
4.3. New Insights Brought by Ultra-Wide SS-OCTA
4.4. Limitations of the Current Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Morgan, I.G.; French, A.N.; Ashby, R.S.; Guo, X.; Ding, X.; He, M.; Rose, K.A. The epidemics of myopia: Aetiology and prevention. Prog. Retin. Eye Res. 2018, 62, 134–149. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zuo, Y.; Wei, Y.; Huang, W.; Zhou, X.; Liu, R.; Zhong, L.; Peng, M.; Zhang, S. The Prevalence and associations of peripheral retinopathy: Baseline study of Guangzhou office computer workers. J. Ophthalmol. 2018, 2018, 2358690. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.-Y.; Hung, K.-C.; Wang, S.-W.; Chen, M.-S.; Ho, T.-C. Spectral-domain optical coherence tomography of peripheral lattice degeneration of myopic eyes before and after laser photocoagulation. J. Formos. Med. Assoc. 2019, 118, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.Z.; Koh, V.; Tan, M.; Tan, C.S.; Nah, G.; Shen, L.; Bhargava, M.; Cheng, C.-Y.; Zhao, P.; Wong, T.Y.; et al. Peripheral retinal changes in highly myopic young Asian eyes. Acta Ophthalmol. 2018, 96, e846–e851. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Wei, Y.-T.; Huang, W.-B.; Liu, R.-J.; Zuo, Y.-J.; He, L.-W.; Zhong, L.-T.; Zhang, S.-C. Prevalence and characteristics of peripheral myopic retinopathy in Guangzhou office workers. Int. J. Ophthalmol. 2018, 11, 1390–1395. [Google Scholar] [PubMed]
- Cheng, S.C.; Lam, C.S.; Yap, M.K. Prevalence of myopia-related retinal changes among 12–18 year old Hong Kong Chinese high myopes. Ophthalmic Physiol. Opt. 2013, 33, 652–660. [Google Scholar] [CrossRef] [PubMed]
- Fawzi, A.; Nielsen, J.S.; Mateo-Montoya, A.; Somkijrungroj, T.; Li, H.K.; Gonzales, J.; Mauget-Faÿsse, M.; Jampol, L.M. Multimodal imaging of white and dark without pressure fundus lesions. Retina 2014, 34, 2376–2387. [Google Scholar] [CrossRef]
- Li, M.; Yang, Y.; Jiang, H.; Gregori, G.; Roisman, L.; Zheng, F.; Ke, B.; Qu, D.; Wang, J. Retinal microvascular network and microcirculation assessments in high myopia. Am. J. Ophthalmol. 2017, 174, 56–67. [Google Scholar] [CrossRef]
- He, J.; Chen, Q.; Yin, Y.; Zhou, H.; Fan, Y.; Zhu, J.; Zou, H.; Xu, X. Association between retinal microvasculature and optic disc alterations in high myopia. Eye 2019, 33, 1494–1503. [Google Scholar] [CrossRef]
- Zhang, Q.; Rezaei, K.A.; Saraf, S.S.; Chu, Z.; Wang, F.; Wang, R.K. Ultra-wide optical coherence tomography angiography in diabetic retinopathy. Quant. Imaging Med. Surg. 2018, 8, 743–753. [Google Scholar] [CrossRef]
- Pichi, F.; Smith, S.D.; Abboud, E.B.; Neri, P.; Woodstock, E.; Hay, S.; Levine, E.; Baumal, C.R. Wide-field optical coherence tomography angiography for the detection of proliferative diabetic retinopathy. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 1901–1909. [Google Scholar] [CrossRef]
- Kalra, G.; Pichi, F.; Menia, N.K.; Shroff, D.; Phasukkijwatana, N.; Aggarwal, K.; Agarwal, A. Recent advances in wide field and ultrawide field optical coherence tomography angiography in retinochoroidal pathologies. Expert Rev. Med. Devices 2021, 18, 375–386. [Google Scholar] [CrossRef]
- Wu, H.; Xie, Z.; Wang, P.; Liu, M.; Wang, Y.; Zhu, J.; Chen, X.; Xu, Z.; Mao, X.; Zhou, X. Differences in Retinal and Choroidal Vasculature and Perfusion Related to Axial Length in Pediatric Anisomyopes. Investig. Opthalmol. Vis. Sci. 2021, 62, 40. [Google Scholar] [CrossRef]
- Shukla, M.; Ahuja, O.P. White with pressure (WWP) and white without pressure (WWOP) lesions. Indian J. Ophthalmol. 1982, 30, 129–132. [Google Scholar]
- Nagpal, K.C.; Goldberg, M.F.; Asdourian, G.E.O.R.G.E.; Goldbaum, M.; Huamonte, F. Dark-without-pressure fundus lesions. Br. J. Ophthalmol. 1975, 59, 476–479. [Google Scholar] [CrossRef]
- Littmann, H. Determination of the real size of an object on the fundus of the living eye. Klin. Mon. Augenheilkd. 1982, 180, 286–289. [Google Scholar] [CrossRef]
- Bennett, A.G.; Rudnicka, A.R.; Edgar, D.F. Improvements on littmann’s method of determining the size of retinal features by fundus photography. Graefe’s Arch. Clin. Exp. Ophthalmol. 1994, 232, 361–367. [Google Scholar] [CrossRef]
- Malone, H.E.; Nicholl, H.; Coyne, I. Fundamentals of estimating sample size. Nurse Res. 2016, 23, 21–25. [Google Scholar] [CrossRef]
- Yang, J.; Wang, E.; Yuan, M.; Chen, Y. Three-dimensional choroidal vascularity index in acute central serous chorioretinopathy using swept-source optical coherence tomography. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 241–247. [Google Scholar] [CrossRef]
- Moysidis, S.N.; Koulisis, N.; Ameri, H.; Matsunaga, D.; Yi, J.; Isozaki, V.L.; Kashani, A.H.; de Koo, L.C.O. Multimodal imaging of geographic areas of retinal darkening. Retin. Cases Brief Rep. 2015, 9, 347–351. [Google Scholar] [CrossRef]
- Dai, Y.; Xin, C.; Zhang, Q.; Chu, Z.; Zhou, H.; Zhou, X.; Qiao, L.; Wang, R.K. Impact of ocular magnification on retinal and choriocapillaris blood flow quantification in myopia with swept-source optical coherence tomography angiography. Quant. Imaging Med. Surg. 2020, 11, 948–956. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.Y.; McBeath, J.B.; McCannel, C.A.; McCannel, T.A. ‘Shadow sign’ in congenital hypertrophy of the retinal pigment epithelium of young myopic pigmented patients. Eye 2016, 30, 160–163. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, P.J.; Momorie, F.; Fornah, A.D.; Komba, P.; Emsley, E.; Scott, J.T.; Williams, S.J.; Harding, S.P.; Vandy, M.J.; Sahr, F.; et al. Evolving longitudinal retinal observations in a cohort of survivors of Ebola virus disease. JAMA Ophthalmol. 2020, 138, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Sherman, T.; Palileo, B.M.; Adam, C.R.; Abrams, G.W. Dark without pressure in a case of Choroidal Osteoma. Retin. Cases Brief Rep. 2020. [Google Scholar] [CrossRef] [PubMed]
- Rutnin, U.; Schepens, C.L. Fundus appearance in normal eyes. Am. J. Ophthalmol. 1967, 64, 1040–1062. [Google Scholar] [CrossRef]
- Verkicharla, P.K.; Ohno-Matsui, K.; Saw, S.M. Current and predicted demographics of high myopia and an update of its associated pathological changes. Ophthalmic Physiol. Opt. 2015, 35, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, R.; Ding, J.; Sen, P.; Rousselot, A.; Chan, A.; Nivison-Smith, L.; Wei, X.; Mahajan, S.; Kim, R.; Mishra, C.; et al. Exploring choroidal angioarchitecture in health and disease using choroidal vascularity index. Prog. Retin. Eye Res. 2020, 77, 100829. [Google Scholar] [CrossRef] [PubMed]
- Iovino, C.; Pellegrini, M.; Bernabei, F.; Borrelli, E.; Sacconi, R.; Govetto, A.; Vagge, A.; Di Zazzo, A.; Forlini, M.; Finocchio, L.; et al. Choroidal vascularity index: An in-depth analysis of this novel optical coherence tomography parameter. J. Clin. Med. 2020, 9, 595. [Google Scholar] [CrossRef]
- Li, H.; Zhu, R.; Zhao, R.; Qian, L.; Jiang, L. Role of TGF-Beta1/SMAD2/3 pathway in retinal outer deep vascular plexus and photoreceptor damage in Rat 50/10 oxygen-induced retinopathy. BioMed Res. Int. 2019, 2019, 4072319. [Google Scholar] [CrossRef]
- Tonade, D.; Kern, T.S. Photoreceptor cells and RPE contribute to the development of diabetic retinopathy. Prog. Retin. Eye Res. 2021, 83, 100919. [Google Scholar] [CrossRef]
- Ali, Z.; Zang, J.; Lagali, N.; Schmitner, N.; Salvenmoser, W.; Mukwaya, A.; Neuhauss, S.C.; Jensen, L.D.; Kimmel, R.A. Photoreceptor degeneration accompanies vascular changes in a zebrafish model of diabetic retinopathy. Investig. Opthalmol. Vis. Sci. 2020, 61, 43. [Google Scholar] [CrossRef]



| Variables | Overall | Group 1 | Group 2 | Group 3 | p Value |
|---|---|---|---|---|---|
| SE ≥ −8, <−6 | SE ≥ −10, <−8 | SE < −10 | |||
| No. of eyes | 227 | 130 | 62 | 35 | |
| Age, years | 24.18 ± 13.55 | 24.62 ± 17.82 | 23.44 ± 2.43 | 23.89 ± 1.78 | 0.067 |
| IOP, mmHg | 15.99 ± 2.41 | 15.94 ± 2.38 | 15.98 ± 2.18 | 16.18 ± 2.96 | 0.825 |
| SE, D | −8.28 ± 2.21 | −6.93 ± 0.58 | −8.82 ± 0.50 | −12.29 ± 2.61 | <0.001 a |
| Sphere, D | −7.65 ± 2.03 | −6.47 ± 0.69 | −8.10 ± 0.60 | −11.26 ± 2.40 | <0.001 a |
| Cylindrical, D | −1.25 ± 0.97 | −0.94 ± 0.70 | −1.45 ± 0.97 | −2.06 ± 1.24 | <0.001 a |
| AL, mm | 26.56 ± 1.10 | 26.12 ± 0.85 | 26.73 ± 0.66 | 27.93 ± 1.36 | <0.001 a |
| Gender | 0.967 | ||||
| Female | 162 (71.37%) | 92 (70.77%) | 45 (72.58%) | 25 (71.43%) | |
| Male | 65 (28.63%) | 38 (29.23%) | 17 (27.42%) | 10 (28.57%) | |
| Bilateral | 0.739 | ||||
| OD | 116 (51.10%) | 65 (50.00%) | 31 (50.00%) | 20 (57.14%) | |
| OS | 111 (48.90%) | 65 (50.00%) | 31 (50.00%) | 15 (42.86%) | |
| WWOP | <0.001 a | ||||
| No | 147 (64.76%) | 91 (70.00%) | 45 (72.58%) | 11 (31.43%) | |
| Yes | 80 (35.24%) | 39 (30.00%) | 17 (27.42%) | 24 (68.57%) | |
| DWOP | 0.121 | ||||
| No | 159 (70.04%) | 97 (74.62%) | 42 (67.74%) | 20 (57.14%) | |
| Yes | 68 (29.96%) | 33 (25.38%) | 20 (32.26%) | 15 (42.86%) |
| Exposure | Non-Adjusted | Adjusted | ||
|---|---|---|---|---|
| OR (95%CI) | p Value | OR (95%CI) | p Value | |
| WWOP | ||||
| AL | 1.33 (1.03, 1.71) | 0.0263 a | 1.54 (1.17, 2.03) | 0.0020 a |
| SE | 0.83 (0.73, 0.95) | 0.0075 a | 0.82 (0.72, 0.94) | 0.0046 a |
| DWOP | ||||
| AL | 2.03 (1.49, 2.76) | <0.0001 a | 2.09 (1.51, 2.91) | <0.0001 a |
| SE | 0.84 (0.74, 0.96) | 0.0129 a | 0.84 (0.73, 0.97) | 0.0153 a |
 | Variables (Control-DWOP) | * Area | # Area | ||
| Z Value | p Value | Z Value | p Value | ||
| AL | −0.556 | 0.535 | −0.556 | 0.535 | |
| VD | |||||
| Inner retina | 5.873 | <0.001 a | 1.236 | 0.106 | |
| SVC | −1.132 | 0.159 | −0.853 | 0.302 | |
| DVC | 5.231 | <0.001 a | 1.568 | 0.091 | |
| CVI | −0.463 | 0.628 | 0.168 | 0.970 | |
| Thickness | |||||
| All retina | 1.098 | 0.175 | −0.737 | 0.413 | |
| Inner retina | −0.791 | 0.384 | −0.363 | 0.729 | |
| Outer retina | 6.114 | <0.001 a | 1.676 | 0.086 | |
| Choroid | −0.432 | 0.662 | −0.998 | 0.201 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, H.; Luo, H.; Zhang, X.; Sun, J.; Zhong, Z.; Sun, X. Analysis of White and Dark without Pressure in a Young Myopic Group Based on Ultra-Wide Swept-Source Optical Coherence Tomography Angiography. J. Clin. Med. 2022, 11, 4830. https://doi.org/10.3390/jcm11164830
Yu H, Luo H, Zhang X, Sun J, Zhong Z, Sun X. Analysis of White and Dark without Pressure in a Young Myopic Group Based on Ultra-Wide Swept-Source Optical Coherence Tomography Angiography. Journal of Clinical Medicine. 2022; 11(16):4830. https://doi.org/10.3390/jcm11164830
Chicago/Turabian StyleYu, Huimin, Huan Luo, Xian Zhang, Jinfu Sun, Zheng Zhong, and Xufang Sun. 2022. "Analysis of White and Dark without Pressure in a Young Myopic Group Based on Ultra-Wide Swept-Source Optical Coherence Tomography Angiography" Journal of Clinical Medicine 11, no. 16: 4830. https://doi.org/10.3390/jcm11164830
APA StyleYu, H., Luo, H., Zhang, X., Sun, J., Zhong, Z., & Sun, X. (2022). Analysis of White and Dark without Pressure in a Young Myopic Group Based on Ultra-Wide Swept-Source Optical Coherence Tomography Angiography. Journal of Clinical Medicine, 11(16), 4830. https://doi.org/10.3390/jcm11164830







