Sex-Specific Cut-Off Values for Low Skeletal Muscle Mass to Identify Patients at Risk for Treatment-Related Adverse Events in Head and Neck Cancer
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
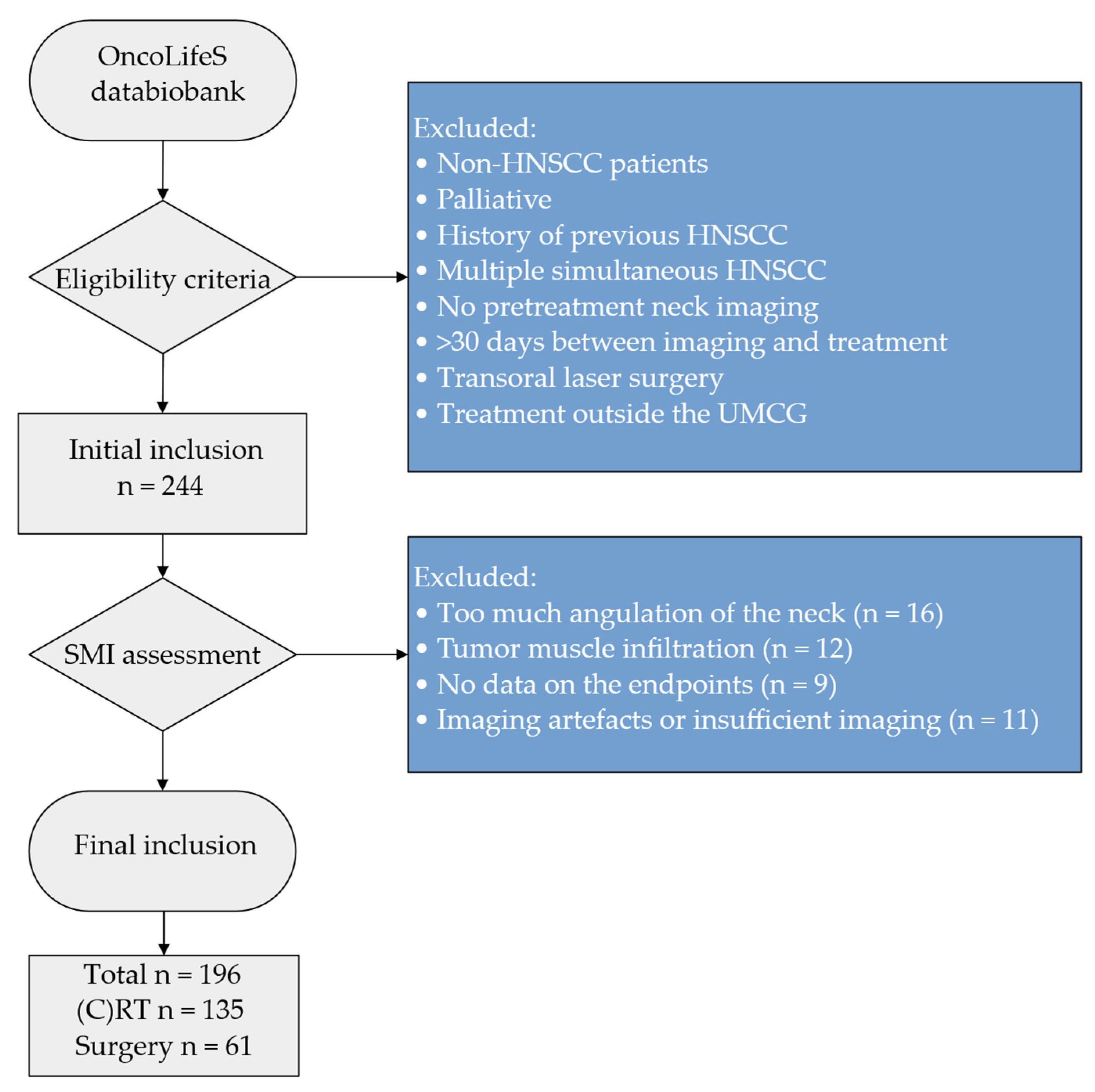
2.2. Patient Population
2.3. Baseline Characteristics
2.4. Skeletal Muscle Mass Analysis
2.5. Endpoints for Adverse Events
2.6. Statistical Analysis
3. Results
3.1. Patients’ and Baseline Characteristics
3.2. Occurrence of Adverse Events
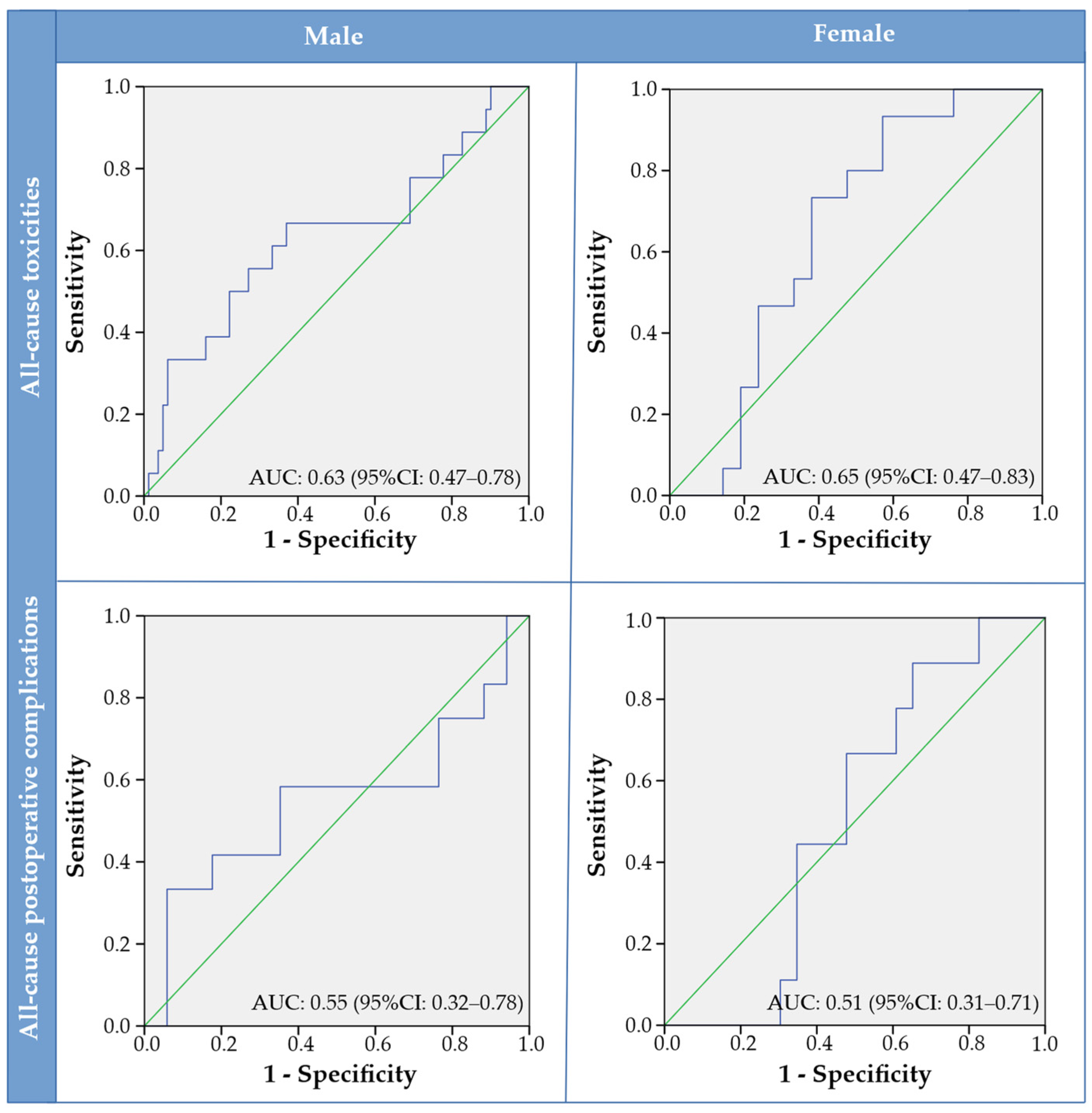
3.3. Observer Analysis, Skeletal Muscle Quantification and SMI Cut-Off Values
3.4. Relationship between Low Skeletal Muscle Mass and Adverse Events
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crozier, E.; Sumer, B.D. Head and neck cancer. Med. Clin. N. Am. 2010, 94, 1031–1046. [Google Scholar] [CrossRef] [PubMed]
- Mascarella, M.A.; Richardson, K.; Mlynarek, A.; Forest, V.-I.; Hier, M.; Sadeghi, N.; Mayo, N. Evaluation of a Preoperative Adverse Event Risk Index for Patients Undergoing Head and Neck Cancer Surgery. JAMA Otolaryngol. Neck Surg. 2019, 145, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Pfister, D.G.; Spencer, S.; Adelstein, D.; Adkins, D.; Anzai, Y.; Brizel, D.M.; Bruce, J.Y.; Busse, P.M.; Caudell, J.J.; Cmelak, A.J.; et al. Head and Neck Cancers, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2020, 18, 873–898. [Google Scholar] [CrossRef] [PubMed]
- Niska, J.R.; Thorpe, C.S.; Halyard, M.Y.; Tan, A.D.; Atherton, P.J.; Dueck, A.C.; Patel, S.H.; Sloan, J.A. Patient-reported quality-of-life outcomes in relation to provider-assessed adverse events during head and neck radiotherapy. J. Patient-Rep. Outcomes 2020, 4, 60. [Google Scholar] [CrossRef]
- Hua, X.; Liao, J.-F.; Huang, X.; Huang, H.-Y.; Wen, W.; Long, Z.-Q.; Guo, L.; Yuan, Z.-Y.; Lin, H.-X. Sarcopenia is associated with higher toxicity and poor prognosis of nasopharyngeal carcinoma. Ther. Adv. Med. Oncol. 2020, 12, 1758835920947612. [Google Scholar] [CrossRef]
- Findlay, M.; White, K.; Lai, M.; Luo, D.; Bauer, J.D. The Association Between Computed Tomography–Defined Sarcopenia and Outcomes in Adult Patients Undergoing Radiotherapy of Curative Intent for Head and Neck Cancer: A Systematic Review. J. Acad. Nutr. Diet. 2020, 120, 1330–1347.e8. [Google Scholar] [CrossRef]
- Surov, A.; Wienke, A. Low skeletal muscle mass predicts relevant clinical outcomes in head and neck squamous cell carcinoma. A Meta Analysis. Ther. Adv. Med. Oncol. 2021, 13, 17588359211008844. [Google Scholar] [CrossRef]
- Wong, A.; Zhu, D.; Kraus, D.; Tham, T. Radiologically Defined Sarcopenia Affects Survival in Head and Neck Cancer: A Meta-Analysis. Laryngoscope 2020, 131, 333–341. [Google Scholar] [CrossRef]
- Couch, M.E.; Dittus, K.; Toth, M.J.; Willis, M.S.; Guttridge, D.C.; George, J.R.; Barnes, C.A.; Gourin, C.G.; Der-Torossian, H. Cancer cachexia update in head and neck cancer: Definitions and diagnostic features. Head Neck 2014, 37, 594–604. [Google Scholar] [CrossRef]
- Mitsiopoulos, N.; Baumgartner, R.N.; Heymsfield, S.B.; Lyons, W.; Gallagher, D.; Ross, R. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J. Appl. Physiol. 1998, 85, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Mourtzakis, M.; Prado, C.M.; Lieffers, J.R.; Reiman, T.; McCargar, L.J.; Baracos, V.E. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl. Physiol. Nutr. Metab. 2008, 33, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Swartz, J.E.; Pothen, A.J.; Wegner, I.; Smid, E.J.; Swart, K.M.; de Bree, R.; Leenen, L.P.; Grolman, W. Feasibility of using head and neck CT imaging to assess skeletal muscle mass in head and neck cancer patients. Oral Oncol. 2016, 62, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Zwart, A.T.; Becker, J.N.; Lamers, M.J.; Dierckx, R.A.J.O.; de Bock, G.H.; Halmos, G.B.; van der Hoorn, A. Skeletal muscle mass and sarcopenia can be determined with 1.5-T and 3-T neck MRI scans, in the event that no neck CT scan is performed. Eur. Radiol. 2020, 31, 4053–4062. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [Green Version]
- Hilmi, M.; Jouinot, A.; Burns, R.; Pigneur, F.; Mounier, R.; Gondin, J.; Neuzillet, C.; Goldwasser, F. Body composition and sarcopenia: The next-generation of personalized oncology and pharmacology? Pharmacol. Ther. 2019, 196, 135–159. [Google Scholar] [CrossRef]
- Shachar, S.S.; Williams, G.R.; Muss, H.B.; Nishijima, T.F. Prognostic value of sarcopenia in adults with solid tumours: A meta-analysis and systematic review. Eur. J. Cancer 2016, 57, 58–67. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Landi, F.; Schneider, S.M.; Zuniga, C.; Arai, H.; Boirie, Y.; Chen, L.K.; Fielding, R.A.; Martin, F.C.; Michel, J.P.; et al. Prevalence of and interventions for sarcopenia in ageing adults: A systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 2014, 43, 748–759. [Google Scholar] [CrossRef]
- Huiskamp, L.F.J.; Chargi, N.; Devriese, L.A.; May, A.M.; Huitema, A.D.R.; De Bree, R. The Predictive Value of Low Skeletal Muscle Mass Assessed on Cross-Sectional Imaging for Anti-Cancer Drug Toxicity: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 3780. [Google Scholar] [CrossRef]
- Wendrich, A.W.; Swartz, J.E.; Bril, S.I.; Wegner, I.; de Graeff, A.; Smid, E.J.; de Bree, R.; Pothen, A.J. Low skeletal muscle mass is a predictive factor for chemotherapy dose-limiting toxicity in patients with locally advanced head and neck cancer. Oral Oncol. 2017, 71, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.; Hsu, C.; Tsai, Y.; Chang, G.; Tsai, M.; Huang, E.I.; Tsai, Y. Prognostic Value of Third Cervical Vertebra Skeletal Muscle Index in Oral Cavity Cancer: A Retrospective Study. Laryngoscope 2021, 131, E2257–E2265. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, H.; Makiguchi, T.; Yamaguchi, T.; Suzuki, K.; Yokoo, S. Impact of sarcopenia on postoperative surgical site infections in patients undergoing flap reconstruction for oral cancer. Int. J. Oral Maxillofac. Surg. 2020, 49, 576–581. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, D.; Hanai, N.; Suzuki, H.; Koide, Y.; Beppu, S.; Hasegawa, Y. The Impact of Skeletal Muscle Depletion on Head and Neck Squamous Cell Carcinoma. ORL 2018, 80, 1–9. [Google Scholar] [CrossRef]
- Shodo, R.; Yamazaki, K.; Ueki, Y.; Takahashi, T.; Horii, A. Sarcopenia predicts a poor treatment outcome in patients with head and neck squamous cell carcinoma receiving concurrent chemoradiotherapy. Eur. Arch. Oto-Rhino-Laryngol. 2020, 278, 2001–2009. [Google Scholar] [CrossRef]
- van Rijn-Dekker, M.I.; Bosch, L.V.D.; Hoek, J.G.V.D.; Bijl, H.P.; van Aken, E.; van der Hoorn, A.; Oosting, S.F.; Halmos, G.B.; Witjes, M.; van der Laan, H.P.; et al. Impact of sarcopenia on survival and late toxicity in head and neck cancer patients treated with radiotherapy. Radiother. Oncol. 2020, 147, 103–110. [Google Scholar] [CrossRef]
- Karavolia, E.; van Rijn-Dekker, M.I.; Bosch, L.V.D.; Hoek, J.G.V.D.; Oldehinkel, E.; Meijer, T.W.; Halmos, G.B.; Witjes, M.J.; Oosting, S.F.; van der Hoorn, A.; et al. Impact of sarcopenia on acute radiation-induced toxicity in head and neck cancer patients. Radiother. Oncol. 2022, 170, 122–128. [Google Scholar] [CrossRef]
- Parker, N.H.; Gorzelitz, J.; Ngo-Huang, A.; Caan, B.J.; Prakash, L.; Garg, N.; Petzel, M.Q.B.; Schadler, K.; Basen-Engquist, K.; Katz, M.H.G. The Role of Home-Based Exercise in Maintaining Skeletal Muscle During Preoperative Pancreatic Cancer Treatment. Integr. Cancer Ther. 2021, 20, 1534735420986615. [Google Scholar] [CrossRef]
- Capozzi, L.C.; McNeely, M.L.; Lau, H.Y.; Reimer, R.A.; Giese-Davis, J.; Fung, T.S.; Culos-Reed, S.N. Patient-reported outcomes, body composition, and nutrition status in patients with head and neck cancer: Results from an exploratory randomized controlled exercise trial. Cancer 2016, 122, 1185–1200. [Google Scholar] [CrossRef] [Green Version]
- Grote, M.; Maihöfer, C.; Weigl, M.; Davies-Knorr, P.; Belka, C. Progressive resistance training in cachectic head and neck cancer patients undergoing radiotherapy: A randomized controlled pilot feasibility trial. Radiat. Oncol. 2018, 13, 215. [Google Scholar] [CrossRef]
- Sidorenkov, G.; Nagel, J.; Meijer, C.; Duker, J.J.; Groen, H.J.M.; Halmos, G.B.; Oonk, M.H.M.; Oostergo, R.J.; van der Vegt, B.; Witjes, M.J.H.; et al. The OncoLifeS data-biobank for oncology: A comprehensive repository of clinical data, biological samples, and the patient’s perspective. J. Transl. Med. 2019, 17, 374. [Google Scholar] [CrossRef] [PubMed]
- Bosch, L.V.D.; van der Laan, H.P.; van der Schaaf, A.; Oosting, S.F.; Halmos, G.B.; Witjes, M.J.; Oldehinkel, E.; Meijer, T.W.; Hoek, J.G.V.D.; Steenbakkers, R.J.; et al. Patient-Reported Toxicity and Quality-of-Life Profiles in Patients with Head and Neck Cancer Treated with Definitive Radiation Therapy or Chemoradiation. Int. J. Radiat. Oncol. 2021, 111, 456–467. [Google Scholar] [CrossRef]
- Sobin, L.; Gospodarowicz, M.; Wittekind, C. (Eds.) TNM Classification of Malignant Tumours, 7th ed.; Wiley-Blackwell: Oxford, UK, 2009. [Google Scholar]
- Soubeyran, P.; Bellera, C.A.; Gregoire, F.; Blanc, J.; Ceccaldi, J.; Blanc-Bisson, C.; Mertens, C.; Mathoulin-Pélissier, S.; Fonck, M.; Rainfray, M. Validation of a screening test for elderly patients in oncology. J. Clin. Oncol. 2008, 26, 20568. [Google Scholar] [CrossRef]
- Steverink, N.; Slaets, J.; Schuurmans, H.; van Lis, M. Measuring frailty: Developing and testing of the Groningen Frailty Indicator (GFI). Gerontologist 2001, 41, 236–237. [Google Scholar]
- Riper, H.; Kramer, J.; Smit, F.; Conijn, B.; Schippers, G.; Cuijpers, P. Web-based self-help for problem drinkers: A pragmatic randomized trial. Addiction 2008, 103, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Zwart, A.T.; van der Hoorn, A.; van Ooijen, P.M.A.; Steenbakkers, R.J.H.M.; de Bock, G.H.; Halmos, G.B. CT-measured skeletal muscle mass used to assess frailty in patients with head and neck cancer. J. Cachexia Sarcopenia Muscle 2019, 10, 1060–1069. [Google Scholar] [CrossRef] [Green Version]
- Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0. In: Health NIo, editor. Sep 2009 ed: U.S.DEPARTMENT OF HEALTH AND HUMAN SERVICES. 2009. Available online: https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/Archive/CTCAE_4.0_2009-05-29_QuickReference_8.5x11.pdf (accessed on 5 May 2022).
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Mandrekar, J.N. Receiver Operating Characteristic Curve in Diagnostic Test Assessment. J. Thorac. Oncol. 2010, 5, 1315–1316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, S.-W.; Tsai, Y.-H.; Hsu, C.-M.; Huang, E.I.; Chang, G.-H.; Tsai, M.-S.; Tsai, Y.-T. Masticatory muscle index for indicating skeletal muscle mass in patients with head and neck cancer. PLoS ONE 2021, 16, e0251455. [Google Scholar] [CrossRef]
- Prado, C.M.; Lieffers, J.R.; McCargar, L.J.; Reiman, T.; Sawyer, M.B.; Martin, L.; Baracos, V.E. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: A population-based study. Lancet Oncol. 2008, 9, 629–635. [Google Scholar] [CrossRef]
- Martin, L.; Birdsell, L.; Macdonald, N.; Reiman, T.; Clandinin, M.T.; McCargar, L.J.; Murphy, R.; Ghosh, S.; Sawyer, M.B.; Baracos, V.E. Cancer cachexia in the age of obesity: Skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J. Clin. Oncol. 2013, 31, 1539–1547. [Google Scholar] [CrossRef] [PubMed]
- Huiskamp, L.F.J.; Chargi, N.; Devriese, L.A.; De Jong, P.A.; De Bree, R. The predictive and prognostic value of low skeletal muscle mass for dose-limiting toxicity and survival in head and neck cancer patients receiving concomitant cetuximab and radiotherapy. Eur. Arch. Oto-Rhino-Laryngol. 2020, 277, 2847–2858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lere-Chevaleyre, A.; Bernadach, M.; Lambert, C.; Cassagnes, L.; Puechmaille, M.; Mom, T.; Gilain, L.; Lapeyre, M.; Boirie, Y.; Biau, J.; et al. Toxicity of induction chemotherapy in head and neck cancer: The central role of skeletal muscle mass. Head Neck 2021, 44, 681–690. [Google Scholar] [CrossRef] [PubMed]
- Thureau, S.; Lebret, L.; Lequesne, J.; Cabourg, M.; Dandoy, S.; Gouley, C.; Lefebvre, L.; Mallet, R.; Mihailescu, S.-D.; Moldovan, C.; et al. Prospective Evaluation of Sarcopenia in Head and Neck Cancer Patients Treated with Radiotherapy or Radiochemotherapy. Cancers 2021, 13, 753. [Google Scholar] [CrossRef]
- Prado, C.M.; Baracos, V.E.; McCargar, L.J.; Reiman, T.; Mourtzakis, M.; Tonkin, K.; Mackey, J.R.; Koski, S.; Pituskin, E.; Sawyer, M.B. Sarcopenia as a Determinant of Chemotherapy Toxicity and Time to Tumor Progression in Metastatic Breast Cancer Patients Receiving Capecitabine Treatment. Clin. Cancer Res. 2009, 15, 2920–2926. [Google Scholar] [CrossRef] [Green Version]
- Yamahara, K.; Mizukoshi, A.; Lee, K.; Ikegami, S. Sarcopenia with inflammation as a predictor of survival in patients with head and neck cancer. Auris Nasus Larynx 2021, 48, 1013–1022. [Google Scholar] [CrossRef]
- Murimwa, G.Z.; Venkat, P.S.; Jin, W.; Leuthold, S.; Latifi, K.; Almhanna, K.; Pimiento, J.M.; Fontaine, J.P.; Hoffe, S.E.; Frakes, J.M. Impact of sarcopenia on outcomes of locally advanced esophageal cancer patients treated with neoadjuvant chemoradiation followed by surgery. J. Gastrointest. Oncol. 2017, 8, 808–815. [Google Scholar] [CrossRef] [Green Version]
- Crowder, S.L.; Douglas, K.G.; Pepino, M.Y.; Sarma, K.P.; Arthur, A.E. Nutrition impact symptoms and associated outcomes in post-chemoradiotherapy head and neck cancer survivors: A systematic review. J. Cancer Surviv. 2018, 12, 479–494. [Google Scholar] [CrossRef]
- Karsten, R.T.; Al-Mamgani, A.; Bril, S.I.; Msc, S.T.; Molen, L.; Boer, J.P.; Hilgers, F.J.M.; Smeele, L.E.; Brekel, M.W.M.; Stuiver, M.M. Sarcopenia, a strong determinant for prolonged feeding tube dependency after chemoradiotherapy for head and neck cancer. Head Neck 2019, 41, 4000–4008. [Google Scholar] [CrossRef]
- Bril, S.I.; Pezier, T.F.; Tijink, B.M.; Janssen, L.M.; Braunius, W.W.; De Bree, R. Preoperative low skeletal muscle mass as a risk factor for pharyngocutaneous fistula and decreased overall survival in patients undergoing total laryngectomy. Head Neck 2019, 41, 1745–1755. [Google Scholar] [CrossRef] [Green Version]
- Ansari, E.; Chargi, N.; Gemert, J.; Es, R.; Dieleman, F.; Rosenberg, A.J.W.P.; Cann, E.; Bree, R. Low skeletal muscle mass is a strong predictive factor for surgical complications and a prognostic factor in oral cancer patients undergoing mandibular reconstruction with a free fibula flap. Oral Oncol. 2020, 101, 104530. [Google Scholar] [CrossRef] [PubMed]
- Alwani, M.M.; Jones, A.J.; Novinger, L.J.; Pittelkow, E.; Bonetto, A.; Sim, M.W.; Moore, M.G.; Mantravadi, A.V. Impact of Sarcopenia on Outcomes of Autologous Head and Neck Free Tissue Reconstruction. J. Reconstr. Microsurg. 2020, 36, 369–378. [Google Scholar] [PubMed]
- Meccariello, G.; Maniaci, A.; Bianchi, G.; Cammaroto, G.; Iannella, G.; Catalano, A.; Sgarzani, R.; De Vito, A.; Capaccio, P.; Pelucchi, S.; et al. Neck dissection and trans oral robotic surgery for oropharyngeal squamous cell carcinoma. Auris Nasus Larynx 2021, 49, 117–125. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total | (Chemo-) Radiotherapy | Surgery | p-Value |
|---|---|---|---|---|
| n = 196 | n = 135 | n = 61 | ||
| Sex | ||||
| Male | 128 (65.3%) | 99 (73.3%) | 29 (47.5%) | <0.001 * |
| Female | 68 (34.7%) | 36 (26.7%) | 32 (52.5%) | |
| Age (years) | 64.2 (±11.2) | 63.5 (±10.5) | 65.8 (±12.5) | 0.176 ** |
| BMI (kg2/m2) | 25.8 (±5.3) | 25.4 (±5.4) | 26.5 (±5.0) | 0.184 ** |
| Tumour site | ||||
| Oropharynx | 69 (35.2%) | 67 (49.6%) | 2 (3.3%) | <0.001 *** |
| Oral cavity | 60 (30.6%) | 5 (3.7%) | 55 (90.2%) | |
| Larynx | 56 (28.6%) | 52 (38.5%) | 4 (6.6%) | |
| Hypopharynx | 10 (5.1%) | 10 (7.4%) | 0 (0%) | |
| Nasopharynx | 1 (0.5%) | 1 (0.7%) | 0 (0%) | |
| Stage | ||||
| I | 23 (11.7%) | 3 (2.2%) | 20 (32.8%) | <0.001 * |
| II | 24 (12.2%) | 17 (12.6%) | 7 (11.5%) | |
| III | 37 (18.0%) | 31 (23.0%) | 6 (9.8%) | |
| IV | 112 (57.1%) | 84(62.2%) | 28 (45.9%) | |
| HPV (Oropharynx) | ||||
| + | 22 (40.7%) | 21 (39.6%) | 1 (100%) | 0.223 * |
| − | 32 (59.3%) | 32 (60.4%) | 0 (0%) | |
| Missing | 15 | 14 | 1 | |
| ACE-27 | ||||
| None | 32 (28.3%) | 24 (28.6%) | 8 (37.6%) | 0.113 * |
| Mild | 37 (32.7%) | 32 (38.1%) | 5 (17.2%) | |
| Moderate | 30 (26.5%) | 20 (23.8%) | 10 (34.5%) | |
| Severe | 14 (12.4%) | 8 (9.5%) | 6 (20.7%) | |
| Missing | 83 | 51 | 32 | |
| Smoking | ||||
| Never | 9 (8.8%) | 3 (4.0%) | 6 (22.2%) | 0.004 * |
| Active/quit | 93 (91.2%) | 72 (96.0%) | 21 (77.8%) | |
| Missing | 94 | 60 | 34 | |
| Alcohol | ||||
| No abuse | 72 (77.4%) | 51 (73.9%) | 21 (87.5%) | 0.170 * |
| Abuse | 21 (22.6%) | 18 (26.1%) | 3 (12.5%) | |
| Missing | 103 | 66 | 37 | |
| GFI | ||||
| Non-frail | 67 (69.1%) | 50 (71.4%) | 18 (64.3%) | 0.419 * |
| Frail | 30 (30.9%) | 20 (28.6%) | 10 (35.7%) | |
| Missing | 99 | 65 | 34 | |
| G8 | ||||
| Non-frail | 41 (42.7%) | 32 (46.4%) | 9 (33.3%) | 0.245 * |
| Frail | 55 (57.3%) | 37 (53.6%) | 18 (66.7%) | |
| Missing | 100 | 66 | 34 |
| Characteristics | (Chemo-)Radiotherapy Toxicities | |
|---|---|---|
| All-cause (n = 135) | Dysphagia (n = 135) | |
| CTCAE | ||
| None | 8 (5.9%) | 40 (29.6%) |
| Grade I | 45 (33.3%) | 36 (26.7%) |
| Grade II | 49 (36.3%) | 30 (22.2%) |
| ≥Grade III | 33 (24.4%) | 29 (21.5%) |
| Characteristics | Postoperative complications | |
| All-cause (n = 61) | Wound infection (n = 61) | |
| Clavien–Dindo | ||
| None | 32 (52.5%) | 51 (78.5%) |
| Grade I | 8 (13.1%) | 3 (4.6%) |
| Grade II | 12 (19.7%) | 7 (10.8%) |
| Grade III | 9 (14.8%) | 4 (6.2%) |
| ≥Grade II | 21 (34.4.0%) | 11 (16.9%) |
| SMI Cut-Off | Sensitivity | Specificity | AUC | 95%CI | p-Value | |
|---|---|---|---|---|---|---|
| Toxicities | ||||||
| All-cause | ||||||
| Male | 46.49 | 0.67 | 0.63 | 0.632 | 0.47–0.78 | 0.082 |
| Female | 37.90 | 0.93 | 0.43 | 0.648 | 0.47–0.83 | 0.136 |
| Dysphagia | ||||||
| Male | 46.49 | 0.65 | 0.62 | 0.610 | 0.45–0.77 | 0.156 |
| Female | 34.91 | 0.75 | 0.58 | 0.642 | 0.46–0.83 | 0.169 |
| Postoperative complications | ||||||
| All-cause | ||||||
| Male | 41.97 | 0.33 | 0.94 | 0.549 | 0.32–0.78 | 0.658 |
| Female | 39.09 | 0.89 | 0.65 | 0.512 | 0.31–0.71 | 0.917 |
| Wound infection | ||||||
| Male | 40.79 | 0.14 | 0.96 | 0.409 | 0.15–0.67 | 0.476 |
| Female | 35.64 | 1.00 | 0.54 | 0.607 | 0.42–0.79 | 0.494 |
| Characteristics | (Chemo-)Radiotherapy Toxicities | |||||
|---|---|---|---|---|---|---|
| All-Cause | Dysphagia | |||||
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Sex | ||||||
| Male | Ref | Ref | ||||
| Female | 0.31 | 0.14–0.72 | 0.006 | 0.42 | 0.17–0.99 | 0.047 |
| Age (years) | 0.97 | 0.93–1.00 | 0.076 | 0.97 | 0.93–1.01 | 0.126 |
| BMI (kg/m2) | 0.84 | 0.75–0.93 | 0.001 | 0.85 | 0.77–0.95 | 0.003 |
| Tumour site | ||||||
| Oral cavity | Ref | 0.007 | Ref | 0.011 | ||
| Nasopharynx/Oropharynx | 0.83 | 0.13–5.24 | 1.91 | 0.20–18.14 | ||
| Hypopharynx/Larynx | 0.19 | 0.03–1.35 | 0.43 | 0.04–4.48 | ||
| Stage | ||||||
| I–III | Ref | 0.010 | Ref | 0.014 | ||
| IV | 3.55 | 1.35–9.34 | 3.68 | 1.30–10.38 | ||
| HPV (oropharynx) | ||||||
| + | Ref | Ref | ||||
| − | 0.73 | 0.23–2.31 | 0.593 | 0.76 | 0.26–2.65 | 0.833 |
| ACE-27 | ||||||
| None | Ref | 0.704 | Ref | 0.837 | ||
| Mild | 1.24 | 0.20–7.67 | 1.00 | 0.16–6.35 | ||
| Moderate | 1.17 | 0.20–6.94 | 1.00 | 0.14–5.99 | ||
| Severe | 0.53 | 0.07–3.98 | 0.54 | 0.07–3.98 | ||
| GFI | ||||||
| Non-frail | Ref | 0.265 | Ref | 0.482 | ||
| Frail | 1.91 | 0.61–5.95 | 1.52 | 0.47–4.88 | ||
| G8 | ||||||
| Non-frail | Ref | 0.621 | Ref | 0.810 | ||
| Frail | 1.32 | 0.44–4.01 | 1.15 | 0.37–3.54 | ||
| Smoking | ||||||
| Never | Ref | Ref | ||||
| Active/quit | 0.67 | 0.06–7.80 | 0.747 | 0.62 | 0.05–7.25 | 0.702 |
| Alcohol | ||||||
| No abuse | Ref | Ref | ||||
| Abuse | 0.53 | 0.13–2.11 | 0.336 | 0.59 | 0.15–2.35 | 0.449 |
| SMI (cm2/m2) | 0.91 | 0.86–0.96 | <0.001 | 0.92 | 0.87–0.97 | 0.002 |
| Low SMI | ||||||
| No | Ref | Ref | ||||
| Yes | 3.86 | 1.69–8.86 | 0.001 | 2.70 | 1.12–6.47 | 0.026 |
| Characteristics | Postoperative Complications | |||||
|---|---|---|---|---|---|---|
| All-Cause | Wound Infection | |||||
| OR | 95%CI | p-Value | OR | 95%CI | p-Value | |
| Sex | ||||||
| Male | Ref | Ref | ||||
| Female | 1.80 | 0.62–5.25 | 0.279 | 2.23 | 0.58–8.59 | 0.245 |
| Age (years) | 0.97 | 0.93–1.02 | 0.188 | 0.99 | 0.94–1.04 | 0.616 |
| BMI (kg/m2) | 0.96 | 0.86–1.07 | 0.479 | 1.01 | 0.89–1.15 | 0.830 |
| Tumour site | ||||||
| Oral cavity | Ref | 0.827 | Ref | 0.026 | ||
| Nasopharynx/Oropharynx | 2.44 | 0.14–41.40 | 6.86 | 0.38–122.52 | ||
| Hypopharynx/Larynx | * | * | 20.57 | 1.87–226.32 | ||
| Stage | ||||||
| I–III | Ref | 0.463 | Ref | 0.060 | ||
| IV | 1.49 | 0.52–4.30 | 4.00 | 0.95–16.93 | ||
| HPV (oropharynx) | ||||||
| + | * | * | ||||
| − | ||||||
| ACE-27 | ||||||
| None | Ref | 0.303 | Ref | 0740 | ||
| Moderate | 0.67 | 0.07–6.87 | 1.67 | 0.12–24.26 | ||
| Severe | 5.33 | 0.50–127.90 | 1.25 | 0.06–26.87 | ||
| Missing | 1.33 | 0.24–16.36 | 3.33 | 0.28–40.29 | ||
| GFI | ||||||
| Non-frail | Ref | 0.517 | Ref | 0.974 | ||
| Frail | 1.69 | 0.35–8.22 | 0.97 | 0.18–537 | ||
| G8 | ||||||
| Non-frail | Ref | 0.069 | Ref | 0.454 | ||
| Frail | 5.50 | 0.88–34.46 | 1.75 | 0.28–11.15 | ||
| Smoking | ||||||
| Never | * | * | * | * | ||
| Active/quit | ||||||
| Alcohol | ||||||
| No abuse | * | * | * | * | ||
| Abuse | ||||||
| SMI (cm2/m2) | 1.02 | 0.96–1.08 | 0.529 | 1.04 | 0.96–1.11 | 0.344 |
| Low SMI (sex-specific) | ||||||
| No | Ref | 0.377 | Ref | |||
| Yes | 0.62 | 0.21–1.81 | 0.67 | 0.17–2.58 | 0.562 | |
| Surgical intensity | ||||||
| Minor | Ref | 0.287 | Ref | 0.148 | ||
| Major | 1.80 | 0.61–5.28 | 2.89 | 0.69–12.17 | ||
| Characteristics | (Chemo-)Radiotherapy Toxicities | |||||
|---|---|---|---|---|---|---|
| All-Cause | Dysphagia | |||||
| OR | 95%CI | p-Value | OR | 95%CI | p-Value | |
| Low SMI | ||||||
| No | Ref | 0.006 | Ref | 0.046 | ||
| Yes | 3.33 | 1.41–7.82 | 2.50 | 1.02–6.14 | ||
| Stage | ||||||
| I–III | Ref | 0.014 | Ref | 0.020 | ||
| IV | 3.45 | 1.28–9.29 | 3.47 | 1.21–9.92 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zwart, A.T.; Pörtzgen, W.; van Rijn-Dekker, I.; Sidorenkov, G.A.; Dierckx, R.A.J.O.; Steenbakkers, R.J.H.M.; Wegner, I.; van der Hoorn, A.; de Bock, G.H.; Halmos, G.B. Sex-Specific Cut-Off Values for Low Skeletal Muscle Mass to Identify Patients at Risk for Treatment-Related Adverse Events in Head and Neck Cancer. J. Clin. Med. 2022, 11, 4650. https://doi.org/10.3390/jcm11164650
Zwart AT, Pörtzgen W, van Rijn-Dekker I, Sidorenkov GA, Dierckx RAJO, Steenbakkers RJHM, Wegner I, van der Hoorn A, de Bock GH, Halmos GB. Sex-Specific Cut-Off Values for Low Skeletal Muscle Mass to Identify Patients at Risk for Treatment-Related Adverse Events in Head and Neck Cancer. Journal of Clinical Medicine. 2022; 11(16):4650. https://doi.org/10.3390/jcm11164650
Chicago/Turabian StyleZwart, Aniek T., Wolf Pörtzgen, Irene van Rijn-Dekker, Grigory A. Sidorenkov, Rudi A. J. O. Dierckx, Roel J. H. M. Steenbakkers, Inge Wegner, Anouk van der Hoorn, Geertruida H. de Bock, and Gyorgy B. Halmos. 2022. "Sex-Specific Cut-Off Values for Low Skeletal Muscle Mass to Identify Patients at Risk for Treatment-Related Adverse Events in Head and Neck Cancer" Journal of Clinical Medicine 11, no. 16: 4650. https://doi.org/10.3390/jcm11164650
APA StyleZwart, A. T., Pörtzgen, W., van Rijn-Dekker, I., Sidorenkov, G. A., Dierckx, R. A. J. O., Steenbakkers, R. J. H. M., Wegner, I., van der Hoorn, A., de Bock, G. H., & Halmos, G. B. (2022). Sex-Specific Cut-Off Values for Low Skeletal Muscle Mass to Identify Patients at Risk for Treatment-Related Adverse Events in Head and Neck Cancer. Journal of Clinical Medicine, 11(16), 4650. https://doi.org/10.3390/jcm11164650








