Survival Rates and Factors Affecting the Outcome Following Immediate and Delayed Implant Placement: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
- Were at least 18 years of age at the time of the treatment;
- Had complete demographic and medical history records;
- Received implant treatment in the university dental clinics provided by residents or faculty;
- Data related to implant therapy were available.
2.2. Implant Survival and Failure
2.3. Statistical Analysis
3. Results
4. Discussion
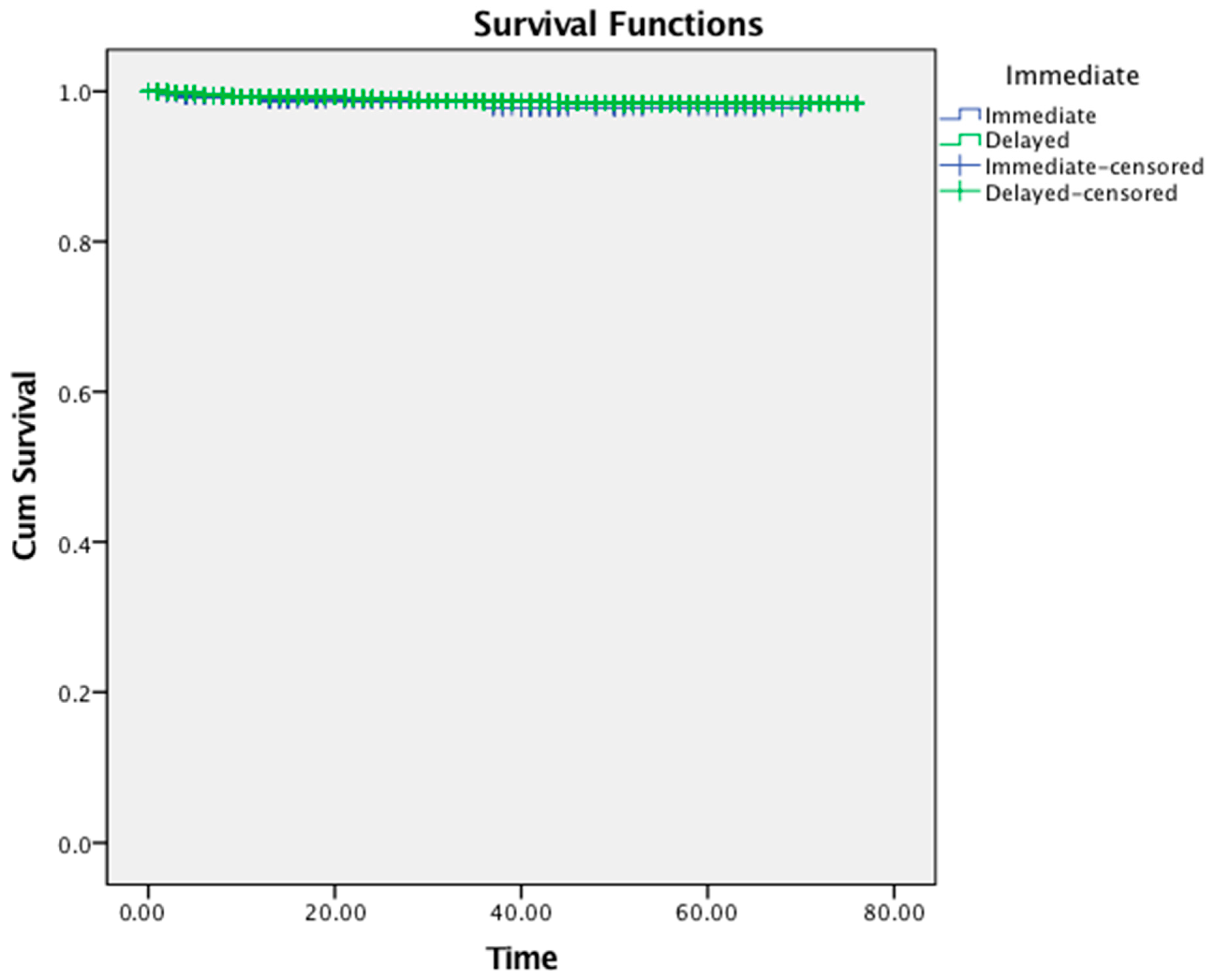
- The overall survival rate of implants placed immediately following tooth extraction was 98.5%, while implants inserted in completely healed extraction sockets showed a survival rate of 98.9%. Nevertheless, imbalances in the baseline characteristics such as tobacco use, arch, region and depression due to study design may have partially influenced the reported finding;
- The implant treatment protocol (immediate versus delayed) was not associated with a higher risk of implant failure (p = 0.48);
- Male patients (p = 0.03) and individuals with osteoporosis (p = 0.001) were more likely to experience dental implant failure than females and non-osteoporotic patients, respectively;
- Implants failed predominantly within the first 13 months of their placement with no differences between the treatment groups.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jung, R.E.; Zembic, A.; Pjetursson, B.E.; Zwahlen, M.; Thoma, D.S. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin. Oral Implants Res. 2012, 23, 2–21. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Thoma, D.; Jung, R.; Zwahlen, M.; Zembic, A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin. Oral Implants Res. 2012, 23, 22–38. [Google Scholar] [CrossRef] [PubMed]
- Van der Weijden, F.; Dell-Acqua, F.; Slot, D.E. Alveolar bone dimensional changes of post-extraction sockets in humans: A systematic review. J. Clin. Periodontol. 2009, 36, 1048–1058. [Google Scholar] [CrossRef] [PubMed]
- Iasella, J.M.; Greenwell, H.; Miller, R.L.; Hill, M.; Drisko, C.; Bohra, A.A.; Scheetz, J.P. Ridge preservation with freeze dried bone allograft and a collagen membrane compared to extraction alone for implant site development: A clinical and histology study in 271 humans. J. Periodontol. 2003, 74, 990–999. [Google Scholar] [CrossRef] [PubMed]
- Lim, G.; Lin, G.H.; Monje, A.; Chan, H.L.; Wang, H.L. Wound healing complications following guided bone regeneration for ridge augmentation: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Implants 2018, 33, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, R.; Puleio, F.; Rizzo, D.; Alibrandi, A.; Lo Giudice, G.; Centofanti, A.; Fiorillo, L.; Di Mauro, D.; Nicita, F. Comparative Investigation of Cutting Devices on Bone Blocks: An SEM Morphological Analysis. Appl. Sci. 2019, 9, 351. [Google Scholar] [CrossRef] [Green Version]
- Abrahamsson, I.; Berglundh, T.; Linder, E.; Lang, N.P.; Lindhe, J. Early bone formation adjacent to rough and turned endosseous implant surfaces. An experimental study in the dog. Clin. Oral Implants Res. 2004, 15, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Lai, H.C.; Zhuang, L.F.; Zhang, Z.Y.; Wieland, M.; Liu, X. Bone apposition around two different sandblasted, large-grit and acid-etched implant surfaces at sites with coronal circumferential defects: An experimental study in dogs. Clin. Oral. Implants Res. 2009, 20, 247–253. [Google Scholar] [CrossRef]
- Chen, S.T.; Buser, D. Clinical and esthetic outcomes of implants placed in postextractionsites. Int. J. Oral Maxillofac. Implants 2009, 24, 186–217. [Google Scholar]
- Perel, S.M.; Triplett, R.G. Immediate fixture placement: A treatment planning alternative. Int. J. Oral Maxillofac. Implants 1990, 5, 337–345. [Google Scholar]
- Lazzara, R.J. Immediate implant placementinto extraction sites: Surgical and restorativeadvantages. Int. J. Periodontics Restor. Dent. 1989, 9, 332–343. [Google Scholar]
- Lemes, H.; Sartori, I.A.; Cardoso, L.C.; Ponzoni, D. Behaviour of the buccal crestal bone levelsafter immediate placement of implants subjected to immediate loading. Int. J. Oral Maxillofac. Surg. 2015, 44, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Werbitt, M.J.; Goldberg, P.V. The immediate implant: Bone preservation and bone regeneration. Int. J. Periodontics Restor. Dent. 1992, 12, 206–217. [Google Scholar]
- Schropp, L.; Isidor, F. Timing of implant placement relative to tooth extraction. J. Oral Rehabil. 2008, 35, 33–43. [Google Scholar] [CrossRef]
- Grandi, T.; Guazzi, P.; Samarani, R.; Grandi, G. Immediate provisionalisation of single post-extractive implants versus implants placed in healed sites in the anterior maxilla: 1-year results from a multicentre controlled cohort study. Eur. J. Oral Implantol. 2013, 6, 285–295. [Google Scholar]
- Atieh, M.A.; Alsabeeha, N.H.; Duncan, W.J.; de Silva, R.K.; Cullinan, M.P.; Schwass, D.; Payne, A.G. Immediate single implant restorations in mandibular molar extraction sockets: A controlled clinical trial. Clin. Oral Implants Res. 2013, 24, 484–496. [Google Scholar] [CrossRef]
- Ardekian, L.; Dodson, T.B. Complications associated with the placement of dental implants. Oral. Maxillofac. Surg. Clin. N. Am. 2003, 15, 243–249. [Google Scholar] [CrossRef]
- Esposito, M.; Grusovin, M.G.; Polyzos, I.P.; Felice, P.; Worthington, H.V. Timing of implant placement after tooth extraction: Immediate, immediate-delayed or delayed implants? A Cochrane systematic review. Eur. J. Oral Implantol. 2010, 3, 189–205. [Google Scholar]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Factors influencing early dental implant failures. J. Dent. Res. 2016, 95, 995–1002. [Google Scholar] [CrossRef]
- Manor, Y.; Oubaid, S.; Mardinger, O.; Chaushu, G.; Nissan, J. Characteristics of early versus late implant failure: A retrospective study. J. Oral Maxillofac. Surg. 2009, 67, 2649–2652. [Google Scholar] [CrossRef]
- Esposito, M.; Hirsch, J.M.; Lekholm, U.; Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants. (I) Success criteria and epidemiology. Eur. J. Oral Sci. 1998, 106, 527–551. [Google Scholar] [CrossRef]
- Derks, J.; Hakansson, J.; Wennstrom, J.L.; Tomasi, C.; Larsson, M.; Berglundh, T. Effectiveness of implant therapy analyzed in a Swedish population: Early and late implant loss. J. Dent. Res. 2015, 94, 44s–51s. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United States Census Bureau. 2010-ACS 5-Year Estimates. 2014. Available online: https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2014/5-year.html (accessed on 21 June 2022).
- Felice, P.; Zucchelli, G.; Cannizzaro, G.; Barausse, C.; Diazzi, M.; Trullenque-Eriksson, A.; Esposito, M. Immediate, immediate-delayed (6 weeks) and delayed (4 months) post-extractive single implants: 4-month post-loading data from a randomised controlled trial. Eur. J. Oral Implantol. 2016, 9, 233–247. [Google Scholar] [PubMed]
- Tonetti, M.S.; Cortellini, P.; Graziani, F.; Cairo, F.; Lang, N.P.; Abundo, R.; Conforti, G.P.; Marquardt, S.; Rasperini, G.; Silvestri, M.; et al. Immediate versus delayed implant placement after anterior single tooth extraction: The timing randomized controlled clinical trial. J. Clin. Periodontol. 2017, 44, 215–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grunder, U.; Polizzi, G.; Goené, R.; Hatano, N.; Henry, P.; Jackson, W.J.; Kawamura, K.; Köhler, S.; Renouard, F.; Rosenberg, R.; et al. A 3-year prospective multicenter follow-up report on the immediate and delayed-immediate placement of implants. Int. J. Oral Maxillofac. Implants 1999, 14, 210–216. [Google Scholar]
- Palattella, P.; Torsello, F.; Cordaro, L. Two-year prospective clinical comparison of immediate replacement vs. immediate restoration of single tooth in the esthetic zone. Clin. Oral Implants Res. 2008, 19, 1148–1153. [Google Scholar] [CrossRef] [PubMed]
- Peñarrocha-Oltra, D.; Demarchi, C.L.; Maestre-Ferrín, L.; Peñarrocha-Diago, M.; Peñarrocha-Diago, M. Comparison of immediate and delayed implants in the maxillary molar region: A retrospective study of 123 implants. Int. J. Oral Maxillofac. Implants 2012, 27, 604–610. [Google Scholar]
- Zafiropoulos, G.G.; Deli, G.; Bartee, B.K.; Hoffmann, O. Single-tooth implant placement and loading in fresh and regenerated extraction sockets. Five-year results: A case series using two different implant designs. J. Periodontol. 2010, 81, 604–615. [Google Scholar] [CrossRef]
- Mello, C.C.; Lemos, C.A.A.; Verri, F.R.; Dos Santos, D.M.; Goiato, M.C.; Pellizzer, E.P. Immediate implant placement into fresh extraction sockets versus delayed implants into healed sockets: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 1162–1177. [Google Scholar] [CrossRef] [Green Version]
- Cosyn, J.; De Lat, L.; Seyssens, L.; Doornewaard, R.; Deschepper, E.; Vervaeke, S. The effectiveness of immediate implant placement for single tooth replacement compared to delayed implant placement: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46, 224–241. [Google Scholar] [CrossRef] [Green Version]
- Thanissorn, C.; Guo, J.; Jing Ying Chan, D.; Koyi, B.; Kujan, O.; Khzam, N.; Miranda, L.A. Success Rates and Complications Associated with Single Immediate Implants: A Systematic Review. Dent. J. 2022, 10, 31. [Google Scholar] [CrossRef]
- Ibrahim, A.; Chrcanovic, B.R. Dental Implants Inserted in Fresh Extraction Sockets versus Healed Sites: A Systematic Review and Meta-Analysis. Materials 2021, 14, 7903. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.; Ye, S.; Liu, F.; He, F. A retrospective study of 30,959 implants: Risk factors associated with early and late implant loss. J. Clin. Periodontol. 2018, 45, 733–743. [Google Scholar] [CrossRef]
- Wagenberg, B.; Froum, S.J. A retrospective study of 1925 consecutively placed immediate implants from 1988 to 2004. Int. J. Oral Maxillofac. Implants 2006, 21, 71–80. [Google Scholar] [PubMed]
- Grisar, K.; Sinha, D.; Schoenaers, J.; Dormaar, T.; Politis, C. Retrospective Analysis of Dental Implants Placed Between 2012 and 2014, Indications, Risk Factors, and Early Survival. Int. J. Oral Maxillofac. Implants 2017, 32, 649–654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olmedo-Gaya, M.V.; Manzano-Moreno, F.J.; Cañaveral-Cavero, E.; de Dios Luna-del Castillo, J.; Vallecillo-Capilla, M. Risk factors associated with early implant failure: A 5-year retrospective clinical study. J. Prosthet. Dent. 2016, 115, 150–155. [Google Scholar] [CrossRef]
- Anitua, E.; Orive, G.; Aguirre, J.J.; Ardanza, B.; Andía, I. 5-year clinical experience with BTI dental implants: Risk factors for implant failure. J. Clin. Periodontol. 2008, 35, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Young, L.; Grant, R.; Brown, T.; Lamont, T. Does a history of periodontal disease affect implant survival? Evid. Based. Dent. 2021, 22, 24–25. [Google Scholar] [CrossRef]
- Noda, K.; Arakawa, H.; Kimura-Ono, A.; Yamazaki, S.; Hara, E.S.; Sonoyama, W.; Maekawa, K.; Okura, K.; Shintani, A.; Matsuka, Y.; et al. A longitudinal retrospective study of the analysis of the risk factors of implant failure by the application of generalized estimating equations. J. Prosthodont. Res. 2015, 59, 178–184. [Google Scholar] [CrossRef]
- Hwang, D.; Wang, H.L. Medical contraindications to implant therapy: Part II: Relative contraindications. Implant Dent. 2007, 16, 13–23. [Google Scholar] [CrossRef]
- Bornstein, M.M.; Cionca, N.; Mombelli, A. Systemic conditions and treatments as risks for implant therapy. Int. J. Oral Maxillofac. Implants 2009, 24, 12–27. [Google Scholar] [PubMed]
- Block, M.S.; Christensen, B.J.; Mercante, D.E.; Chapple, A.G. What Factors Are Associated with Implant Failure? J. Oral Maxillofac. Surg. 2021, 79, 91–97. [Google Scholar] [CrossRef]
- Alsaadi, G.; Quirynen, M.; Komárek, A.; van Steenberghe, D. Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection. J. Clin. Periodontol. 2007, 34, 610–617. [Google Scholar] [CrossRef] [PubMed]
- Giro, G.; Chambrone, L.; Goldstein, A.; Rodrigues, J.A.; Zenóbio, E.; Feres, M.; Figueiredo, L.C.; Cassoni, A.; Shibli, J.A. Impact of osteoporosis in dental implants: A systematic review. World J. Orthop. 2015, 6, 311–315. [Google Scholar] [CrossRef] [PubMed]
- De Medeiros, F.C.F.L.; Kudo, G.A.H.; Leme, B.G.; Saraiva, P.P.; Verri, F.R.; Honório, H.M.; Pellizzer, E.P.; Santiago Junior, J.F. Dental implants in patients with osteoporosis: A systematic review with meta-analysis. Int. J. Oral Maxillofac. Surg. 2018, 47, 480–491. [Google Scholar] [CrossRef]
- Aghaloo, T.; Pi-Anfruns, J.; Moshaverinia, A.; Sim, D.; Grogan, T.; Hadaya, D. The Effects of Systemic Diseases and Medications on Implant Osseointegration: A Systematic Review. Int. J. Oral Maxillofac. Implants 2019, 34, s35–s49. [Google Scholar] [CrossRef] [PubMed]
- Diz, P.; Scully, C.; Sanz, M. Dental implants in the medically compromised patient. J. Dent. 2013, 41, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.B.; Revuru, V.S.; Lohse, C.M. Association of Systemic Conditions with Dental Implant Failures in 6384 Patients during a 31-Year Follow-up Period. Int. J. Oral Maxillofac. Implants 2017, 32, 1153–1161. [Google Scholar] [CrossRef]
- Chuang, S.K.; Wei, L.J.; Douglass, C.W.; Dodson, T.B. Risk factors for dental implant failure: A strategy for the analysis of clustered failure-time observations. J. Dent. Res. 2002, 81, 572–577. [Google Scholar] [CrossRef]
- Sánchez-Pérez, A.; Moya-Villaescusa, M.J.; Caffesse, R.G. Tobacco as a risk factor for survival of dental implants. J. Periodontol. 2007, 78, 351–359. [Google Scholar] [CrossRef]
- Kang, D.Y.; Kim, M.; Lee, S.J.; Cho, I.W.; Shin, H.S.; Caballé-Serrano, J.; Park, J.-C. Early implant failure: A retrospective analysis of contributing factors. J. Periodontal. Implant Sci. 2019, 49, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, A.P.; Lourenço, J.D.; Junqueira, J.J.M.; Larissa Emidio de França, S.; Martins, J.S.; Oliveira Junior, M.C.; Begalli, I.; Velosa, A.P.P.; Olivo, C.R.; Bastos, T.B.; et al. The deleterious effects of smoking in bone mineralization and fibrillar matrix composition. Life Sci. 2020, 241, 117132. [Google Scholar] [CrossRef] [PubMed]
- Ejaz, S.; Lim, C.W. Toxicological overview of cigarette smoking on angiogenesis. Environ. Toxicol. Pharmacol. 2005, 20, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Mustapha, A.D.; Salame, Z.; Chrcanovic, B.R. Smoking and Dental Implants: A Systematic Review and Meta-Analysis. Medicina 2021, 58, 39. [Google Scholar] [CrossRef]
- Carr, A.B.; Choi, Y.G.; Eckert, S.E.; Desjardins, R.P. Retrospective cohort study of the clinical performance of 1-stage dental implants. Int. J. Oral Maxillofac. Implants 2003, 18, 399–405. [Google Scholar]
- Olson, J.W.; Dent, C.D.; Morris, H.F.; Ochi, S. Long-term assessment (5 to 71 months) of endosseous dental implants placed in the augmented maxillary sinus. Ann. Periodontol. 2000, 5, 152–156. [Google Scholar] [CrossRef]
- Zinser, M.J.; Randelzhofer, P.; Kuiper, L.; Zöller, J.E.; De Lange, G.L. The predictors of implant failure after maxillary sinus floor augmentation and reconstruction: A retrospective study of 1045 consecutive implants. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 571–582. [Google Scholar] [CrossRef]
- Beretta, M.; Cicciù, M.; Poli, P.P.; Rancitelli, D.; Bassi, G.; Grossi, G.B.; Maiorana, C. A Retrospective Evaluation of 192 Implants Placed in Augmented Bone: Long-Term Follow-Up Study. J. Oral Implantol. 2015, 41, 669–674. [Google Scholar] [CrossRef] [Green Version]
- Hong, J.Y.; Shin, E.Y.; Herr, Y.; Chung, J.H.; Lim, H.C.; Shin, S.I. Implant survival and risk factor analysis in regenerated bone: Results from a 5-year retrospective study. J. Periodontal. Implant Sci. 2020, 50, 379–391. [Google Scholar] [CrossRef]
- Quirynen, M.; Gijbels, F.; Jacobs, R. An infected jawbone site compromising successful osseointegration. Periodontology 2000, 33, 129–144. [Google Scholar] [CrossRef] [PubMed]
- Rosenquist, B.; Grenthe, B. Immediate placement of implants into extraction sockets: Implant survival. Int. J. Oral Maxillofac. Implants 1996, 11, 205–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chrcanovic, B.R.; Martins, M.D.; Wennerberg, A. Immediate placement of implants into infected sites: A systematic review. Clin. Implant Dent. Relat. Res. 2015, 17, e1–e16. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Capparé, P.; Crespi, G.; Lo Giudice, G.; Gastaldi, G.; Gherlone, E. Immediate Implant Placement in Sockets with Asymptomatic Apical Periodontitis. Clin. Implant Dent. Relat. Res. 2017, 19, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.T.; Chuang, S.K.; Stoupel, J. Survival analysis and other clinical outcomes of immediate implant placement in sites with periapical lesions: Systematic review. Int. J. Oral Maxillofac. Implant 2015, 30, 268–278. [Google Scholar] [CrossRef] [Green Version]
- Tran, D.T.; Gay, I.C.; Diaz-Rodriguez, J.; Parthasarathy, K.; Weltman, R.; Friedman, L. Survival of Dental Implants Placed in Grafted and Nongrafted Bone: A Retrospective Study in a University Setting. Int. J. Oral Maxillofac. Implant 2016, 31, 310–317. [Google Scholar] [CrossRef]
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implant 1986, 1, 11–25. [Google Scholar]
| Characteristics | Total | Immediate Implant | Delayed Implant | p-Value * |
|---|---|---|---|---|
| n = 4519—100% | n = 265—5.9% | n = 4254—94.1% | ||
| Age | 60.27 ± 13.11 (Range: 18–93) | 59.89 ± 14.10 | 60.30 ± 13.05 | 0.62 |
| Gender n (%) | 0.31 | |||
| Males | 2293 (50.7) | 126 (47.5) | 2167 (50.9) | |
| Females | 2226 (49.3) | 139 (52.5) | 2087 (49.1) | |
| Tobacco use n (%) | <0.001 | |||
| Yes | 581 (12.9) | 16 (6.0) | 565 (13.3) | |
| No | 3938 (87.1) | 249 (94.0) | 3689 (86.7) | |
| Socioeconomic status | 0.87 | |||
| n (%) | ||||
| Low | 800 (17.7) | 48 (18.1) | 752 (17.7) | |
| High | 3719 (82.3) | 217 (81.9) | 3502 (82.3) | |
| Insurance status n (%) | 0.27 | |||
| Yes | 2849 (63.0) | 176 (66.4) | 2673 (62.8) | |
| No | 1670 (37.0) | 89 (33.6) | 1581 (37.2) | |
| Arch n (%) | <0.001 | |||
| Maxilla | 2333 (51.6) | 173 (65.3) | 2160 (50.8) | |
| Mandible | 2186 (48.4) | 92 (34.7) | 2094 (49.2) | |
| Region n (%) | <0.001 | |||
| Anterior (incisors, canines) | 1285 (28.4) | 132 (49.8) | 1153 (27.1) | |
| Posterior (premolars, molars) | 3234 (71.6) | 133 (50.2) | 3101 (72.9) | |
| Treatment outcome | 0.54 | |||
| n (%) | ||||
| Survived | 4468 (98.9) | 261 (98.5) | 4207 (98.9) | |
| Failed | 51 (1.1) | 4 (1.5) | 47 (1.1) | |
| Hypertension n (%) | 0.36 | |||
| Yes | 1246 (27.6) | 66 (24.9) | 1180 (27.7) | |
| No | 3273 (72.4) | 199 (75.1) | 3074 (72.3) | |
| History of heart attack n (%) | 0.38 | |||
| Yes | 151 (3.3) | 6 (2.3) | 145 (3.4) | |
| No | 4368 (96.7) | 259 (97.7) | 4109 (96.6) | |
| High cholesterol | 0.56 | |||
| n (%) | ||||
| Yes | 1166 (25.8) | 64 (24.2) | 1102 (25.9) | |
| No | 3353 (74.2) | 201 (75.8) | 3152 (74.1) | |
| Asthma | 0.52 | |||
| Yes | 288 (6.4) | 14 (5.3) | 274 (6.4) | |
| No | 4231 (93.6) | 251 (94.7) | 3980 (93.6) | |
| Diabetes n (%) | 0.14 | |||
| Yes | 386 (8.5) | 16 (6.0) | 370 (8.7) | |
| No | 4133 (91.5) | 249 (94.0) | 3884 (91.3) | |
| Thyroid disorder | 0.38 | |||
| n (%) | ||||
| Yes | 534 (11.8) | 36 (13.6) | 498 (11.7) | |
| No | 3985 (88.2) | 229 (86.4) | 3756 (88.3) | |
| Kidney disease n (%) | 0.35 | |||
| Yes | 85 (1.9) | 7 (2.6) | 78 (1.8) | |
| No | 4434 (98.1) | 258 (97.4) | 4176 (98.2) | |
| Arthritis n (%) | 0.25 | |||
| Yes | 1001 (22.2) | 51 (19.2) | 950 (22.3) | |
| No | 3518 (77.8) | 214 (80.8) | 3304 (77.7) | |
| Artificial joint n (%) | 0.25 | |||
| Yes | 363 (8.0) | 16 (6.0) | 347 (8.2) | |
| No | 4156 (92.0) | 249 (94.0) | 3907 (91.8) | |
| Osteoporosis n (%) | 0.89 | |||
| Yes | 251 (5.6) | 15 (5.7) | 236 (5.5) | |
| No | 4268 (94.4) | 250 (94.3) | 4018 (94.5) | |
| Depression n (%) | 0.001 | |||
| Yes | 604 (13.4) | 18 (6.8) | 586 (13.8) | |
| No | 3915 (86.6) | 247 (93.2) | 3668 (86.2) | |
| Anxiety n (%) | 0.23 | |||
| Yes | 505 (11.2) | 23 (8.7) | 482 (11.3) | |
| No | 4014 (88.8) | 242 (91.3) | 3772 (88.7) | |
| Cancer n (%) | 0.92 | |||
| Yes | 520 (11.5) | 31 (11.7) | 489 (11.5) | |
| No | 3999 (88.5) | 234 (88.3) | 3765 (88.5) | |
| History of cancer treatment n (%) | 0.41 | |||
| Yes | 362 (8.0) | 17 (6.4) | 345 (8.1) | |
| No | 4157 (92.0) | 248 (93.6) | 3909 (91.9) |
| Variable | Hazzard Ratio | 95% Confidence Interval | p-Value * | |
|---|---|---|---|---|
| Lower | Upper | |||
| Treatment: immediate implant | 1.61 | 0.57 | 4.57 | 0.37 |
| Age (increase by 1 year) | 1.00 | 0.97 | 1.02 | 0.70 |
| Gender: male | 2.06 | 1.08 | 3.92 | 0.03 |
| Tobacco use | 1.76 | 0.88 | 3.54 | 0.11 |
| Socioeconomic status: high | 0.62 | 0.32 | 1.20 | 0.15 |
| Insurance status: insured | 1.19 | 0.68 | 2.08 | 0.55 |
| Arch: mandible | 1.02 | 0.59 | 1.78 | 0.94 |
| Region: posterior | 1.40 | 0.72 | 2.71 | 0.32 |
| Hypertension | 0.99 | 0.49 | 1.97 | 0.97 |
| History of heart attack | 0.00 | 0.00 | - | 0.98 |
| Hypercholesterolemia | 0.89 | 0.44 | 1.81 | 0.75 |
| Asthma | 0.00 | 0.00 | 5.205 × 10293 | 0.97 |
| Diabetes | 0.38 | 0.09 | 1.64 | 0.19 |
| Thyroid disorder | 0.60 | 0.21 | 1.72 | 0.34 |
| Kidney disease | 2.24 | 0.49 | 10.22 | 0.30 |
| Arthritis | 1.35 | 0.67 | 2.72 | 0.40 |
| Artificial joint | 1.36 | 0.50 | 3.71 | 0.55 |
| Osteoporosis | 4.56 | 1.80 | 11.54 | 0.001 |
| Depression | 1.70 | 0.74 | 3.92 | 0.21 |
| Anxiety | 1.22 | 0.47 | 3.16 | 0.69 |
| Cancer | 2.01 | 0.60 | 6.71 | 0.26 |
| History of cancer treatment | 0.31 | 0.06 | 1.56 | 0.15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chatzopoulos, G.S.; Wolff, L.F. Survival Rates and Factors Affecting the Outcome Following Immediate and Delayed Implant Placement: A Retrospective Study. J. Clin. Med. 2022, 11, 4598. https://doi.org/10.3390/jcm11154598
Chatzopoulos GS, Wolff LF. Survival Rates and Factors Affecting the Outcome Following Immediate and Delayed Implant Placement: A Retrospective Study. Journal of Clinical Medicine. 2022; 11(15):4598. https://doi.org/10.3390/jcm11154598
Chicago/Turabian StyleChatzopoulos, Georgios S., and Larry F. Wolff. 2022. "Survival Rates and Factors Affecting the Outcome Following Immediate and Delayed Implant Placement: A Retrospective Study" Journal of Clinical Medicine 11, no. 15: 4598. https://doi.org/10.3390/jcm11154598
APA StyleChatzopoulos, G. S., & Wolff, L. F. (2022). Survival Rates and Factors Affecting the Outcome Following Immediate and Delayed Implant Placement: A Retrospective Study. Journal of Clinical Medicine, 11(15), 4598. https://doi.org/10.3390/jcm11154598






