PCOS Physiopathology and Vitamin D Deficiency: Biological Insights and Perspectives for Treatment
Abstract
1. Introduction
The Pathophysiology of PCOS
2. Vitamin D
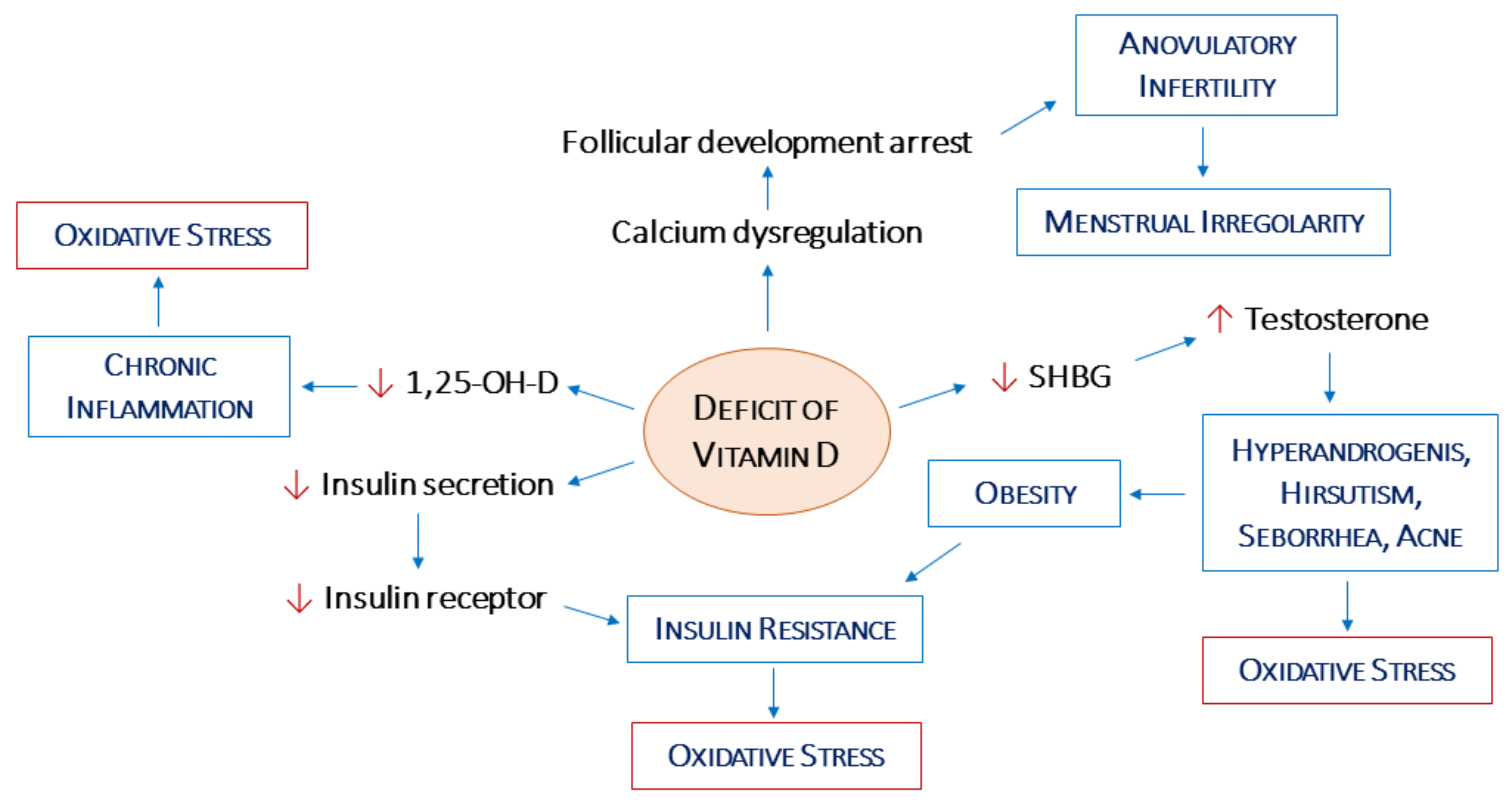
2.1. Vitamin D Deficiency and PCOS Phenotypes
2.2. Vitamin D, Hypothalamic–Pituitary–Gonadal Axis, and Androgen Levels
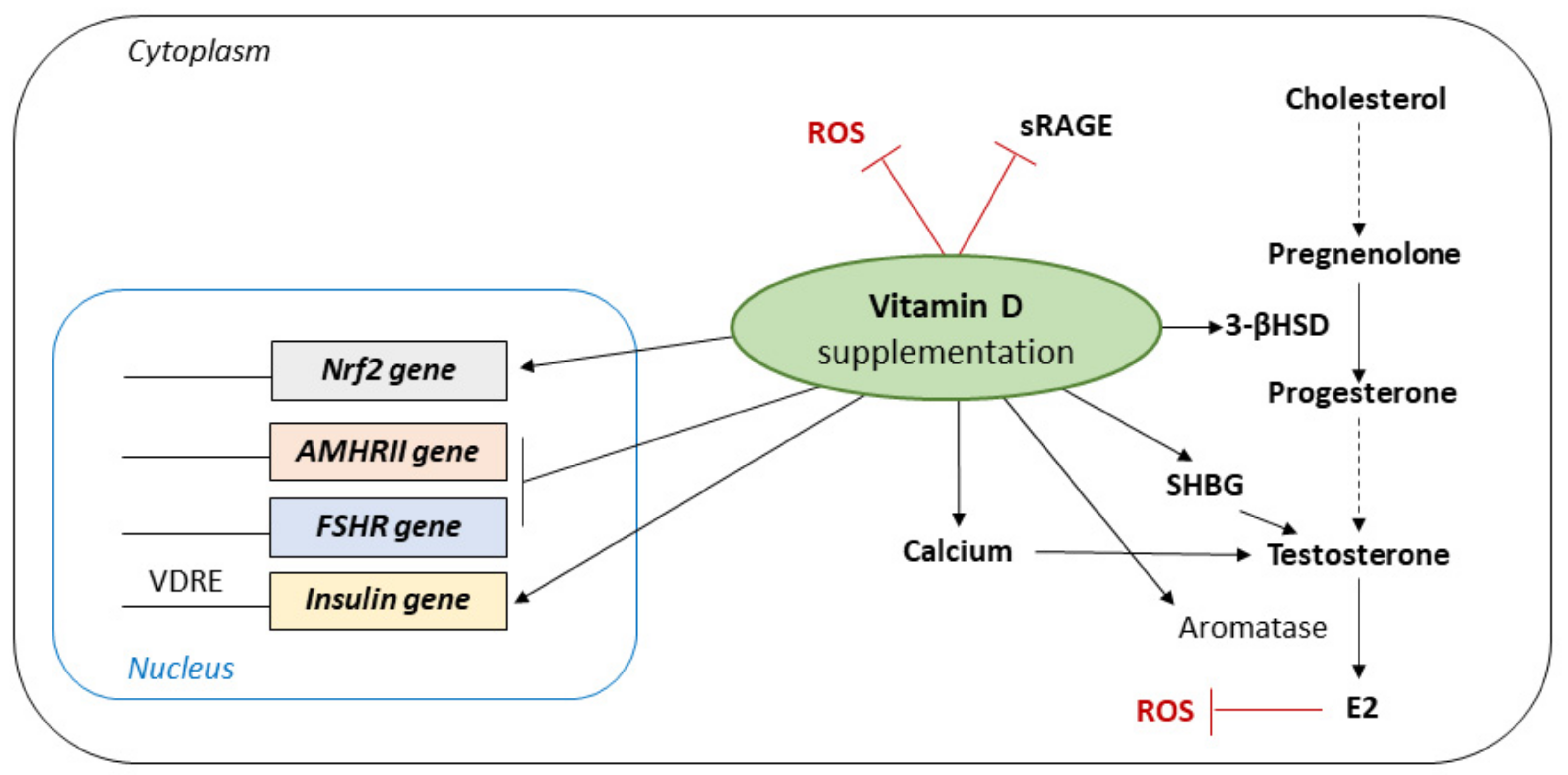
2.3. Vitamin D, Ovarian Physiology, and Oxidative Stress
2.4. Vitamin D, Insulin Resistance, and Obesity
3. Relevance of Supplementation
3.1. Impact of Vitamin D Supplementation on Biomarkers of Oxidative Stress in PCOS
3.2. Vitamin D Supplementation and Fertility Outcomes in PCOS Women
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Azziz, R. Introduction: Determinants of Polycystic Ovary Syndrome. Fertil. Steril. 2016, 106, 4–5. [Google Scholar] [CrossRef] [PubMed]
- Bozdag, G.; Mumusoglu, S.; Zengin, D.; Karabulut, E.; Yildiz, B.O. The Prevalence and Phenotypic Features of Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Hum. Reprod. Oxf. Engl. 2016, 31, 2841–2855. [Google Scholar] [CrossRef] [PubMed]
- De Leo, V.; Musacchio, M.C.; Cappelli, V.; Massaro, M.G.; Morgante, G.; Petraglia, F. Genetic, Hormonal and Metabolic Aspects of PCOS: An Update. Reprod. Biol. Endocrinol. RBE 2016, 14, 38. [Google Scholar] [CrossRef]
- Teede, H.; Deeks, A.; Moran, L. Polycystic Ovary Syndrome: A Complex Condition with Psychological, Reproductive and Metabolic Manifestations That Impacts on Health across the Lifespan. BMC Med. 2010, 8, 41. [Google Scholar] [CrossRef] [PubMed]
- De Groot, P.C.M.; Dekkers, O.M.; Romijn, J.A.; Dieben, S.W.M.; Helmerhorst, F.M. PCOS, Coronary Heart Disease, Stroke and the Influence of Obesity: A Systematic Review and Meta-Analysis. Hum. Reprod. Update 2011, 17, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Sangaraju, S.L.; Yepez, D.; Grandes, X.A.; Talanki Manjunatha, R.; Habib, S. Cardio-Metabolic Disease and Polycystic Ovarian Syndrome (PCOS): A Narrative Review. Cureus 2022, 14, e25076. [Google Scholar] [CrossRef]
- Wehr, E.; Pilz, S.; Schweighofer, N.; Giuliani, A.; Kopera, D.; Pieber, T.R.; Obermayer-Pietsch, B. Association of Hypovitaminosis D with Metabolic Disturbances in Polycystic Ovary Syndrome. Eur. J. Endocrinol. 2009, 161, 575–582. [Google Scholar] [CrossRef]
- Shi, X.-Y.; Huang, A.-P.; Xie, D.-W.; Yu, X.-L. Association of Vitamin D Receptor Gene Variants with Polycystic Ovary Syndrome: A Meta-Analysis. BMC Med. Genet. 2019, 20, 32. [Google Scholar] [CrossRef]
- Armanini, D.; Boscaro, M.; Bordin, L.; Sabbadin, C. Controversies in the Pathogenesis, Diagnosis and Treatment of PCOS: Focus on Insulin Resistance, Inflammation, and Hyperandrogenism. Int. J. Mol. Sci. 2022, 23, 4110. [Google Scholar] [CrossRef]
- Smirnov, V.V.; Beeraka, N.M.; Butko, D.Y.; Nikolenko, V.N.; Bondarev, S.A.; Achkasov, E.E.; Sinelnikov, M.Y.; Sinelnikov, P.R.H. Updates on Molecular Targets and Epigenetic-Based Therapies for PCOS. Reprod. Sci. Thousand Oaks Calif 2022. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Cappelli, V.; Musacchio, M.C.; Bulfoni, A.; Morgante, G.; De Leo, V. Natural Molecules for the Therapy of Hyperandrogenism and Metabolic Disorders in PCOS. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 15–29. [Google Scholar]
- Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group Revised 2003 Consensus on Diagnostic Criteria and Long-Term Health Risks Related to Polycystic Ovary Syndrome (PCOS). Hum. Reprod. Oxf. Engl. 2004, 19, 41–47. [CrossRef] [PubMed]
- Clark, N.M.; Podolski, A.J.; Brooks, E.D.; Chizen, D.R.; Pierson, R.A.; Lehotay, D.C.; Lujan, M.E. Prevalence of Polycystic Ovary Syndrome Phenotypes Using Updated Criteria for Polycystic Ovarian Morphology. Reprod. Sci. 2014, 21, 1034–1043. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Hu, M.; Jia, W.; Liu, G.; Zhang, J.; Wang, B.; Li, J.; Cui, P.; Li, X.; Lager, S.; et al. Hyperandrogenism and Insulin Resistance Modulate Gravid Uterine and Placental Ferroptosis in PCOS-like Rats. J. Endocrinol. 2020, 246, 247–263. [Google Scholar] [CrossRef]
- Rosenfield, R.L.; Ehrmann, D.A. The Pathogenesis of Polycystic Ovary Syndrome (PCOS): The Hypothesis of PCOS as Functional Ovarian Hyperandrogenism Revisited. Endocr. Rev. 2016, 37, 467–520. [Google Scholar] [CrossRef]
- Drummond, A.E. The Role of Steroids in Follicular Growth. Reprod. Biol. Endocrinol. 2006, 4, 16. [Google Scholar] [CrossRef] [PubMed]
- Dupont, J.; Scaramuzzi, R.J. Insulin Signalling and Glucose Transport in the Ovary and Ovarian Function during the Ovarian Cycle. Biochem. J. 2016, 473, 1483. [Google Scholar] [CrossRef] [PubMed]
- DeLuca, H.F. The Metabolism and Functions of Vitamin D. Adv. Exp. Med. Biol. 1986, 196, 361–375. [Google Scholar] [CrossRef] [PubMed]
- Bikle, D.D. Vitamin D: Newer Concepts of Its Metabolism and Function at the Basic and Clinical Level. J. Endocr. Soc. 2020, 4, bvz038. [Google Scholar] [CrossRef]
- Grzesiak, M. Vitamin D3 Action within the Ovary-an Updated Review. Physiol. Res. 2020, 69, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Kinuta, K.; Tanaka, H.; Moriwake, T.; Aya, K.; Kato, S.; Seino, Y. Vitamin D Is an Important Factor in Estrogen Biosynthesis of Both Female and Male Gonads. Endocrinology 2000, 141, 1317–1324. [Google Scholar] [CrossRef]
- Mahmoudi, T. Genetic Variation in the Vitamin D Receptor and Polycystic Ovary Syndrome Risk. Fertil. Steril. 2009, 92, 1381–1383. [Google Scholar] [CrossRef] [PubMed]
- Vulcan, T.; Filip, G.A.; Lenghel, L.M.; Suciu, T.; Ilut, P.; Procopciuc, L.M. Polymorphisms of Vitamin D Receptor and the Effect on Metabolic AndEndocrine Abnormalities in Polycystic Ovary Syndrome: A Review. Horm. Metab. Res. 2021, 53, 645–653. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Lin, Z.; Robb, S.W.; Ezeamama, A.E. Serum Vitamin D Levels and Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Nutrients 2015, 7, 4555–4577. [Google Scholar] [CrossRef] [PubMed]
- Davis, E.M.; Peck, J.D.; Hansen, K.R.; Neas, B.R.; Craig, L.B. Associations between Vitamin D Levels and Polycystic Ovary Syndrome Phenotypes. Minerva Endocrinol. 2019, 44, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Maktabi, M.; Chamani, M.; Asemi, Z. The Effects of Vitamin D Supplementation on Metabolic Status of Patients with Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial. Horm. Metab. Res. 2017, 49, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Kuiri-Hänninen, T.; Sankilampi, U.; Dunkel, L. Activation of the Hypothalamic-Pituitary-Gonadal Axis in Infancy: Minipuberty. Horm. Res. Paediatr. 2014, 82, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Kılınç, S.; Atay, E.; Ceran, Ö.; Atay, Z. Evaluation of Vitamin D Status and Its Correlation with Gonadal Function in Children at Mini-Puberty. Clin. Endocrinol. (Oxf.) 2019, 90, 122–128. [Google Scholar] [CrossRef]
- Chang, E.M.; Kim, Y.S.; Won, H.J.; Yoon, T.K.; Lee, W.S. Association between Sex Steroids, Ovarian Reserve, and Vitamin D Levels in Healthy Nonobese Women. J. Clin. Endocrinol. Metab. 2014, 99, 2526–2532. [Google Scholar] [CrossRef] [PubMed]
- Hahn, S.; Haselhorst, U.; Tan, S.; Quadbeck, B.; Schmidt, M.; Roesler, S.; Kimmig, R.; Mann, K.; Janssen, O.E. Low Serum 25-Hydroxyvitamin D Concentrations Are Associated with Insulin Resistance and Obesity in Women with Polycystic Ovary Syndrome. Exp. Clin. Endocrinol. Diabetes 2006, 114, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Lundqvist, J. Vitamin D as a Regulator of Steroidogenic Enzymes. F1000Research 2014, 3, 155. [Google Scholar] [CrossRef][Green Version]
- Pal, L.; Berry, A.; Coraluzzi, L.; Kustan, E.; Danton, C.; Shaw, J.; Taylor, H. Therapeutic Implications of Vitamin D and Calcium in Overweight Women with Polycystic Ovary Syndrome. Gynecol. Endocrinol. 2012, 28, 965–968. [Google Scholar] [CrossRef]
- Irani, M.; Merhi, Z. Role of Vitamin D in Ovarian Physiology and Its Implication in Reproduction: A Systematic Review. Fertil. Steril. 2014, 102, 460–468.e3. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, L.; Gagliardi, A.; Landi, C.; Focarelli, R.; De Leo, V.; Luddi, A.; Bini, L.; Piomboni, P. Protein Pathways Working in Human Follicular Fluid: The Future for Tailored IVF? Expert Rev. Mol. Med. 2016, 18, e9. [Google Scholar] [CrossRef] [PubMed]
- Bakhshalizadeh, S.; Amidi, F.; Alleyassin, A.; Soleimani, M.; Shirazi, R.; Shabani Nashtaei, M. Modulation of Steroidogenesis by Vitamin D3 in Granulosa Cells of the Mouse Model of Polycystic Ovarian Syndrome. Syst. Biol. Reprod. Med. 2017, 63, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Yao, X.; Zhang, G.; Guo, Y.; Ei-Samahy, M.; Wang, S.; Wan, Y.; Han, L.; Liu, Z.; Wang, F.; Zhang, Y. Vitamin D Receptor Expression and Potential Role of Vitamin D on Cell Proliferation and Steroidogenesis in Goat Ovarian Granulosa Cells. Theriogenology 2017, 102, 162–173. [Google Scholar] [CrossRef]
- Echchgadda, I.; Song, C.S.; Roy, A.K.; Chatterjee, B. Dehydroepiandrosterone Sulfotransferase Is a Target for Transcriptional Induction by the Vitamin D Receptor. Mol. Pharmacol. 2004, 65, 720–729. [Google Scholar] [CrossRef]
- Baka, S.; Malamitsi-Puchner, A. Novel Follicular Fluid Factors Influencing Oocyte Developmental Potential in IVF: A Review. Reprod. Biomed. Online 2006, 12, 500–506. [Google Scholar] [CrossRef]
- Masjedi, F.; Keshtgar, S.; Zal, F.; Talaei-Khozani, T.; Sameti, S.; Fallahi, S.; Kazeroni, M. Effects of Vitamin D on Steroidogenesis, Reactive Oxygen Species Production, and Enzymatic Antioxidant Defense in Human Granulosa Cells of Normal and Polycystic Ovaries. J. Steroid Biochem. Mol. Biol. 2020, 197, 105521. [Google Scholar] [CrossRef]
- Merhi, Z.; Doswell, A.; Krebs, K.; Cipolla, M. Vitamin D Alters Genes Involved in Follicular Development and Steroidogenesis in Human Cumulus Granulosa Cells. J. Clin. Endocrinol. Metab. 2014, 99, E1137–E1145. [Google Scholar] [CrossRef] [PubMed]
- Usluogullari, B.; Duvan, C.; Usluogullari, C. Use of Aromatase Inhibitors in Practice of Gynecology. J. Ovarian Res. 2015, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, A.V.; Swami, S.; Peng, L.; Wang, J.; Moreno, J.; Feldman, D. Tissue-Selective Regulation of Aromatase Expression by Calcitriol: Implications for Breast Cancer Therapy. Endocrinology 2010, 151, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Merhi, Z. Crosstalk between Advanced Glycation End Products and Vitamin D: A Compelling Paradigm for the Treatment of Ovarian Dysfunction in PCOS. Mol. Cell. Endocrinol. 2019, 479, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Merhi, Z.; Buyuk, E.; Cipolla, M.J. Advanced Glycation End Products Alter Steroidogenic Gene Expression by Granulosa Cells: An Effect Partially Reversible by Vitamin D. MHR Basic Sci. Reprod. Med. 2018, 24, 318–326. [Google Scholar] [CrossRef]
- Wimalawansa, S.J. Vitamin D Deficiency: Effects on Oxidative Stress, Epigenetics, Gene Regulation, and Aging. Biology 2019, 8, 30. [Google Scholar] [CrossRef]
- Mohammadi, M. Oxidative Stress and Polycystic Ovary Syndrome: A Brief Review. Int. J. Prev. Med. 2019, 10, 86. [Google Scholar] [CrossRef] [PubMed]
- Morgante, G.; Massaro, M.G.; Scolaro, V.; Cappelli, V.; Luddi, A.; Troìa, L.; De Leo, V. Metformin Doses and Body Mass Index: Clinical Outcomes in Insulin Resistant Polycystic Ovary Syndrome Women. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 8136–8142. [Google Scholar] [CrossRef] [PubMed]
- De Leo, V.; Musacchio, M.C.; Morgante, G.; La Marca, A.; Petraglia, F. Polycystic Ovary Syndrome and Type 2 Diabetes Mellitus. Minerva Ginecol. 2004, 56, 53–62. [Google Scholar]
- Lerchbaum, E.; Obermayer-Pietsch, B. Vitamin D and Fertility: A Systematic Review. Eur. J. Endocrinol. 2012, 166, 765–778. [Google Scholar] [CrossRef]
- Pittas, A.G.; Lau, J.; Hu, F.B.; Dawson-Hughes, B. The Role of Vitamin D and Calcium in Type 2 Diabetes. A Systematic Review and Meta-Analysis. J. Clin. Endocrinol. Metab. 2007, 92, 2017–2029. [Google Scholar] [CrossRef]
- Milner, R.D.; Hales, C.N. The Role of Calcium and Magnesium in Insulin Secretion from Rabbit Pancreas Studied in Vitro. Diabetologia 1967, 3, 47–49. [Google Scholar] [CrossRef] [PubMed]
- Lerchbaum, E.; Rabe, T. Vitamin D and Female Fertility. Curr. Opin. Obstet. Gynecol. 2014, 26, 145–150. [Google Scholar] [CrossRef]
- Maestro, B.; Molero, S.; Bajo, S.; Dávila, N.; Calle, C. Transcriptional Activation of the Human Insulin Receptor Gene by 1,25-Dihydroxyvitamin D(3). Cell Biochem. Funct. 2002, 20, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Rajakumar, K.; de las Heras, J.; Chen, T.C.; Lee, S.; Holick, M.F.; Arslanian, S.A. Vitamin D Status, Adiposity, and Lipids in Black American and Caucasian Children. J. Clin. Endocrinol. Metab. 2011, 96, 1560–1567. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, R.M.S.; Novaes, J.F.; Azeredo, L.M.; Azeredo, L.M.; Cândido, A.P.C.; Leite, I.C.G. Association of Vitamin D Insufficiency with Adiposity and Metabolic Disorders in Brazilian Adolescents. Public Health Nutr. 2014, 17, 787–794. [Google Scholar] [CrossRef] [PubMed]
- Guasch, A.; Bulló, M.; Rabassa, A.; Bonada, A.; Del Castillo, D.; Sabench, F.; Salas-Salvadó, J. Plasma Vitamin D and Parathormone Are Associated with Obesity and Atherogenic Dyslipidemia: A Cross-Sectional Study. Cardiovasc. Diabetol. 2012, 11, 149. [Google Scholar] [CrossRef]
- Ganie, M.A.; Marwaha, R.K.; Nisar, S.; Farooqi, K.J.; Jan, R.A.; Wani, S.A.; Gojwari, T.; Shah, Z.A. Impact of Hypovitaminosis D on Clinical, Hormonal and Insulin Sensitivity Parameters in Normal Body Mass Index Polycystic Ovary Syndrome Women. J. Obstet. Gynaecol. J. Inst. Obstet. Gynaecol. 2016, 36, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, J.A.; Ashraf, A. Role of Vitamin d in Insulin Secretion and Insulin Sensitivity for Glucose Homeostasis. Int. J. Endocrinol. 2010, 2010, 351385. [Google Scholar] [CrossRef]
- Li, H.W.R.; Brereton, R.E.; Anderson, R.A.; Wallace, A.M.; Ho, C.K.M. Vitamin D Deficiency Is Common and Associated with Metabolic Risk Factors in Patients with Polycystic Ovary Syndrome. Metabolism. 2011, 60, 1475–1481. [Google Scholar] [CrossRef]
- Ngo, D.T.M.; Chan, W.P.; Rajendran, S.; Heresztyn, T.; Amarasekera, A.; Sverdlov, A.L.; O’Loughlin, P.D.; Morris, H.A.; Chirkov, Y.Y.; Norman, R.J.; et al. Determinants of Insulin Responsiveness in Young Women: Impact of Polycystic Ovarian Syndrome, Nitric Oxide, and Vitamin D. Nitric Oxide Biol. Chem. 2011, 25, 326–330. [Google Scholar] [CrossRef] [PubMed]
- Menichini, D.; Facchinetti, F. Effects of Vitamin D Supplementation in Women with Polycystic Ovary Syndrome: A Review. Gynecol. Endocrinol. 2020, 36, 1–5. [Google Scholar] [CrossRef] [PubMed]
- De Leo, V.; Cappelli, V.; Morgante, G.; Di Sabatino, A. The role of vitamin D in assisted reproduction techniques. Minerva Ginecol. 2018, 70, 268–285. [Google Scholar] [CrossRef]
- Belenchia, A.M.; Tosh, A.K.; Hillman, L.S.; Peterson, C.A. Correcting Vitamin D Insufficiency Improves Insulin Sensitivity in Obese Adolescents: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2013, 97, 774–781. [Google Scholar] [CrossRef] [PubMed]
- Yildizhan, R.; Kurdoglu, M.; Adali, E.; Kolusari, A.; Yildizhan, B.; Sahin, H.G.; Kamaci, M. Serum 25-Hydroxyvitamin D Concentrations in Obese and Non-Obese Women with Polycystic Ovary Syndrome. Arch. Gynecol. Obstet. 2009, 280, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Ott, J.; Wattar, L.; Kurz, C.; Seemann, R.; Huber, J.C.; Mayerhofer, K.; Vytiska-Binstorfer, E. Parameters for Calcium Metabolism in Women with Polycystic Ovary Syndrome Who Undergo Clomiphene Citrate Stimulation: A Prospective Cohort Study. Eur. J. Endocrinol. 2012, 166, 897–902. [Google Scholar] [CrossRef]
- Gallea, M.; Granzotto, M.; Azzolini, S.; Faggian, D.; Mozzanega, B.; Vettor, R.; Mioni, R. Insulin and Body Weight but Not Hyperandrogenism Seem Involved in Seasonal Serum 25-OH-Vitamin D3 Levels in Subjects Affected by PCOS. Gynecol. Endocrinol. 2014, 30, 739–745. [Google Scholar] [CrossRef]
- Maestro, B.; Dávila, N.; Carranza, M.C.; Calle, C. Identification of a Vitamin D Response Element in the Human Insulin Receptor Gene Promoter. J. Steroid Biochem. Mol. Biol. 2003, 84, 223–230. [Google Scholar] [CrossRef]
- Bikle, D. Nonclassic Actions of Vitamin D. J. Clin. Endocrinol. Metab. 2009, 94, 26–34. [Google Scholar] [CrossRef]
- Shoelson, S.E.; Herrero, L.; Naaz, A. Obesity, Inflammation, and Insulin Resistance. Gastroenterology 2007, 132, 2169–2180. [Google Scholar] [CrossRef]
- Akbari, M.; Ostadmohammadi, V.; Lankarani, K.B.; Tabrizi, R.; Kolahdooz, F.; Heydari, S.T.; Kavari, S.H.; Mirhosseini, N.; Mafi, A.; Dastorani, M.; et al. The Effects of Vitamin D Supplementation on Biomarkers of Inflammation and Oxidative Stress Among Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Horm. Metab. Res. Horm. Stoffwechselforschung Horm. Metab. 2018, 50, 271–279. [Google Scholar] [CrossRef]
- Foroozanfard, F.; Jamilian, M.; Bahmani, F.; Talaee, R.; Talaee, N.; Hashemi, T.; Nasri, K.; Asemi, Z.; Esmaillzadeh, A. Calcium plus Vitamin D Supplementation Influences Biomarkers of Inflammation and Oxidative Stress in Overweight and Vitamin D-Deficient Women with Polycystic Ovary Syndrome: A Randomized Double-Blind Placebo-Controlled Clinical Trial. Clin. Endocrinol. (Oxf.) 2015, 83, 888–894. [Google Scholar] [CrossRef] [PubMed]
- Ostadmohammadi, V.; Jamilian, M.; Bahmani, F.; Asemi, Z. Vitamin D and Probiotic Co-Supplementation Affects Mental Health, Hormonal, Inflammatory and Oxidative Stress Parameters in Women with Polycystic Ovary Syndrome. J. Ovarian Res. 2019, 12, 5. [Google Scholar] [CrossRef] [PubMed]
- Sepehrmanesh, Z.; Kolahdooz, F.; Abedi, F.; Mazroii, N.; Assarian, A.; Asemi, Z.; Esmaillzadeh, A. Vitamin D Supplementation Affects the Beck Depression Inventory, Insulin Resistance, and Biomarkers of Oxidative Stress in Patients with Major Depressive Disorder: A Randomized, Controlled Clinical Trial. J. Nutr. 2016, 146, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Rashidi, B.; Haghollahi, F.; Shariat, M.; Zayerii, F. The Effects of Calcium-Vitamin D and Metformin on Polycystic Ovary Syndrome: A Pilot Study. Taiwan. J. Obstet. Gynecol. 2009, 48, 142–147. [Google Scholar] [CrossRef]
- Zec, I.; Tislaric-Medenjak, D.; Megla, Z.B.; Kucak, I. Anti-Müllerian Hormone: A Unique Biochemical Marker of Gonadal Development and Fertility in Humans. Biochem. Medica 2011, 21, 219–230. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhi, X. Roles of Vitamin D in Reproductive Systems and Assisted Reproductive Technology. Endocrinology 2020, 161, bqaa023. [Google Scholar] [CrossRef] [PubMed]
- Fang, F.; Ni, K.; Cai, Y.; Shang, J.; Zhang, X.; Xiong, C. Effect of Vitamin D Supplementation on Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Complement. Ther. Clin. Pract. 2017, 26, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Kollmann, M.; Obermayer-Pietsch, B.; Lerchbaum, E.; Feigl, S.; Hochstätter, R.; Pregartner, G.; Trummer, C.; Klaritsch, P. Vitamin D Concentrations at Term Do Not Differ in Newborns and Their Mothers with and without Polycystic Ovary Syndrome. J. Clin. Med. 2021, 10, 537. [Google Scholar] [CrossRef]
- Dennis, N.A.; Houghton, L.A.; Jones, G.T.; van Rij, A.M.; Morgan, K.; McLennan, I.S. The Level of Serum Anti-Müllerian Hormone Correlates with Vitamin D Status in Men and Women but Not in Boys. J. Clin. Endocrinol. Metab. 2012, 97, 2450–2455. [Google Scholar] [CrossRef] [PubMed]
- Malloy, P.J.; Peng, L.; Wang, J.; Feldman, D. Interaction of the Vitamin D Receptor with a Vitamin D Response Element in the Mullerian-Inhibiting Substance (MIS) Promoter: Regulation of MIS Expression by Calcitriol in Prostate Cancer Cells. Endocrinology 2009, 150, 1580–1587. [Google Scholar] [CrossRef] [PubMed]
- Holzer, I.; Parry, J.P.; Beitl, K.; Pozderovic, B.; Marculescu, R.; Ott, J. Parameters for Calcium Metabolism in Women with Polycystic Ovary Syndrome Who Undergo Stimulation with Letrozole: A Prospective Cohort Study. J. Clin. Med. 2022, 11, 2597. [Google Scholar] [CrossRef] [PubMed]
- Dehghani Firouzabadi, R.; Aflatoonian, A.; Modarresi, S.; Sekhavat, L.; MohammadTaheri, S. Therapeutic Effects of Calcium & Vitamin D Supplementation in Women with PCOS. Complement. Ther. Clin. Pract. 2012, 18, 85–88. [Google Scholar] [CrossRef]
- Conway, G.; Dewailly, D.; Diamanti-Kandarakis, E.; Escobar-Morreale, H.F.; Franks, S.; Gambineri, A.; Kelestimur, F.; Macut, D.; Micic, D.; Pasquali, R.; et al. The Polycystic Ovary Syndrome: A Position Statement from the European Society of Endocrinology. Eur. J. Endocrinol. 2014, 171, P1–P29. [Google Scholar] [CrossRef] [PubMed]
- Wild, R.A.; Rizzo, M.; Clifton, S.; Carmina, E. Lipid Levels in Polycystic Ovary Syndrome: Systematic Review and Meta-Analysis. Fertil. Steril. 2011, 95, 1073–1079.e11. [Google Scholar] [CrossRef] [PubMed]
- Bacha, D.S.; Rahme, M.; Al-Shaar, L.; Baddoura, R.; Halaby, G.; Singh, R.J.; Mahfoud, Z.R.; Habib, R.; Arabi, A.; El-Hajj Fuleihan, G. Vitamin D3 Dose Requirement That Raises 25-Hydroxyvitamin D to Desirable Level in Overweight and Obese Elderly. J. Clin. Endocrinol. Metab. 2021, 106, e3644–e3654. [Google Scholar] [CrossRef] [PubMed]
| Issue | References | Main Outcomes |
|---|---|---|
| Vitamin D deficienc and PCOS phenotypes | [7,20,24] | VD low levels may worsen PCOS symptoms; an inverse correlation has been reported between serum VD level and metabolic and hormonal disturbances in different PCOS phenotypes. |
| [25,26] | A higher prevalence of VD deficiency in PCOS cases with androgen excess may be demonstrated. In the B-PCOS phenotype, VD supplementation significantly decreased fasting plasma glucose, insulin, HOMA-IR index, and increased quantitative insulin sensitivity. | |
| Vitamin D, PG axis, and androgen levels | [29] | VD may improve female fertility by modulating androgenic activity. |
| [28] | Association between 25-OH-D levels and gonadal hormones at mini-puberty. | |
| [30,31] | VD is able to affect the expression and activities of some of the enzymes involved in the production of sex hormones. | |
| [32] | Effect of VD supplementation on regulating testosterone unbalance. | |
| Vitamin D, ovarian physiology, and oxidative stress | [46] | Oxidative stress markers are increased in PCOS patients. |
| [45] | Low levels of VD are correlated to decreased Nrf2 transcription and increased risks from oxidative stress-related tissue damage. | |
| [33,34] | VD shows a possible physiologic role in ovarian follicular development and luteinization, and VD supplement can contribute to these processes. | |
| [35,36] | In human luteinized granulosa cells, VD decreases the expression of both the AMH receptor and FSH receptor. | |
| [37,39] | VD stimulates ovarian steroidogenesis by inducing the expression of DHEAS and aromatase. | |
| [40,39] | VD increases the 3β-HSD RNA levels in vitro, possibly reflecting a state of granulosa cell luteinization. | |
| [29,41,42] | VD may change the expression of the aromatase, the enzyme catalyzing the biosynthesis of estrogen, which is an androgen precursor. | |
| Vitamin D, insulin resistance, and obesity | [61,62,63] | VD deficiency is a contributing factor to IR, obesity, and metabolic syndrome, all of which are commonly associated with ovulatory dysfunction: a VD supplement implies a better and healthier ovarian physiology. |
| [64] | Association between concentration of VD and obesity has been strongly demonstrated both in adults and in adolescents: adipose tissue decreases circulating 25OH-D by trapping it. | |
| [65] | Association of increased HOMA-IR, BMI, triglycerides, and total testosterone, with decreased 25OH-D concentrations in the obese PCOS patients. | |
| [66] | Weight and hyperinsulinemia had a significant influence on these values: VD levels were lower in obese PCOS women, and VD serum levels were comparable between normoinsulinemic PCOS women and controls. | |
| [53,67] | VD may improve insulin activity by stimulating VDR gene expression. VDR is present in the promoter of the human insulin gene and 1,25OH-D3 is able to induce the transcription of the human insulin gene. | |
| [51] | VD may affect insulin-responsiveness through calcium, since insulin secretion is a calcium-dependent process. | |
| [68,69] | VD shows an immunomodulatory effect: low levels of VD may induce an inflammatory response, which is associated with insulin resistance. | |
| Vitamin D supplementation and oxidative stress in PCOS | [70] | Significant improvement in high-sensitivity C-reactive protein, MDA, and total antioxidant capacity in women with PCOS receiving VD supplementation, while no effects were reported for NO and GSH levels. |
| [71] | The combined calcium plus VD supplements had greater decreases in plasma MDA concentrations, and significant increases in plasma total antioxidant capacity and GSH levels compared with calcium alone, VD alone, and placebo groups. | |
| [72] | Co-administration of VD and probiotic to women with PCOS significantly improved the serum levels of high-sensitivity C-reactive protein, plasma total antioxidant capacity, GSH, and MDA. | |
| [73] | Beneficial effects from VD supplementation were not observed. | |
| Vitamin D and fertility outcomes in PCOS women | [74,76] | VD is related to menstrual irregularity, altered follicular development, ovulatory dysfunction, metabolic alterations, and decreased pregnancy rate. |
| [82] | Significant improvement in regulating menstrual abnormalities and follicle maturation in women receiving calcium and VD supplementation. | |
| [77] | The combined supplementation with metformin plus VD improves the regularity of the menstrual cycles. | |
| [33,79] | Relationship between VD and AMH: its expression and serum levels are altered by environmental factors, such as VD deficiency and obesity. In the serum, 25OH-D is positively correlated with AMH, and appropriate VD supplementation in VD-depleted women can suppress the seasonal changes that occur in serum AMH. In VD-deficient women with PCOS, VD supplementation lowers the abnormally elevated serum AMH levels, possibly indicating a mechanism by which VD improves folliculogenesis. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morgante, G.; Darino, I.; Spanò, A.; Luisi, S.; Luddi, A.; Piomboni, P.; Governini, L.; De Leo, V. PCOS Physiopathology and Vitamin D Deficiency: Biological Insights and Perspectives for Treatment. J. Clin. Med. 2022, 11, 4509. https://doi.org/10.3390/jcm11154509
Morgante G, Darino I, Spanò A, Luisi S, Luddi A, Piomboni P, Governini L, De Leo V. PCOS Physiopathology and Vitamin D Deficiency: Biological Insights and Perspectives for Treatment. Journal of Clinical Medicine. 2022; 11(15):4509. https://doi.org/10.3390/jcm11154509
Chicago/Turabian StyleMorgante, Giuseppe, Ilenia Darino, Amelia Spanò, Stefano Luisi, Alice Luddi, Paola Piomboni, Laura Governini, and Vincenzo De Leo. 2022. "PCOS Physiopathology and Vitamin D Deficiency: Biological Insights and Perspectives for Treatment" Journal of Clinical Medicine 11, no. 15: 4509. https://doi.org/10.3390/jcm11154509
APA StyleMorgante, G., Darino, I., Spanò, A., Luisi, S., Luddi, A., Piomboni, P., Governini, L., & De Leo, V. (2022). PCOS Physiopathology and Vitamin D Deficiency: Biological Insights and Perspectives for Treatment. Journal of Clinical Medicine, 11(15), 4509. https://doi.org/10.3390/jcm11154509








