Acute Poisoning Readmissions to an Emergency Department of a Tertiary Hospital: Evaluation through an Active Toxicovigilance Program
Abstract
1. Introduction
- Estimate the number of readmissions 1 year after an index episode of admission for APC, both detected by the HULP toxicovigilance program during its first five years of operation, as well as their possible predisposing factors.
- Analyze the temporal behavior of ERs as a result of APC in this ED during the period of the study and its predictive capacity.
- Predict possible ERs through various risk variables, thus obtaining a risk profile for readmission of the patient with APC.
2. Methods and Materials
3. Results
3.1. Frequency of Readmissions, Patient Characteristics and Profile of the Patient with ER
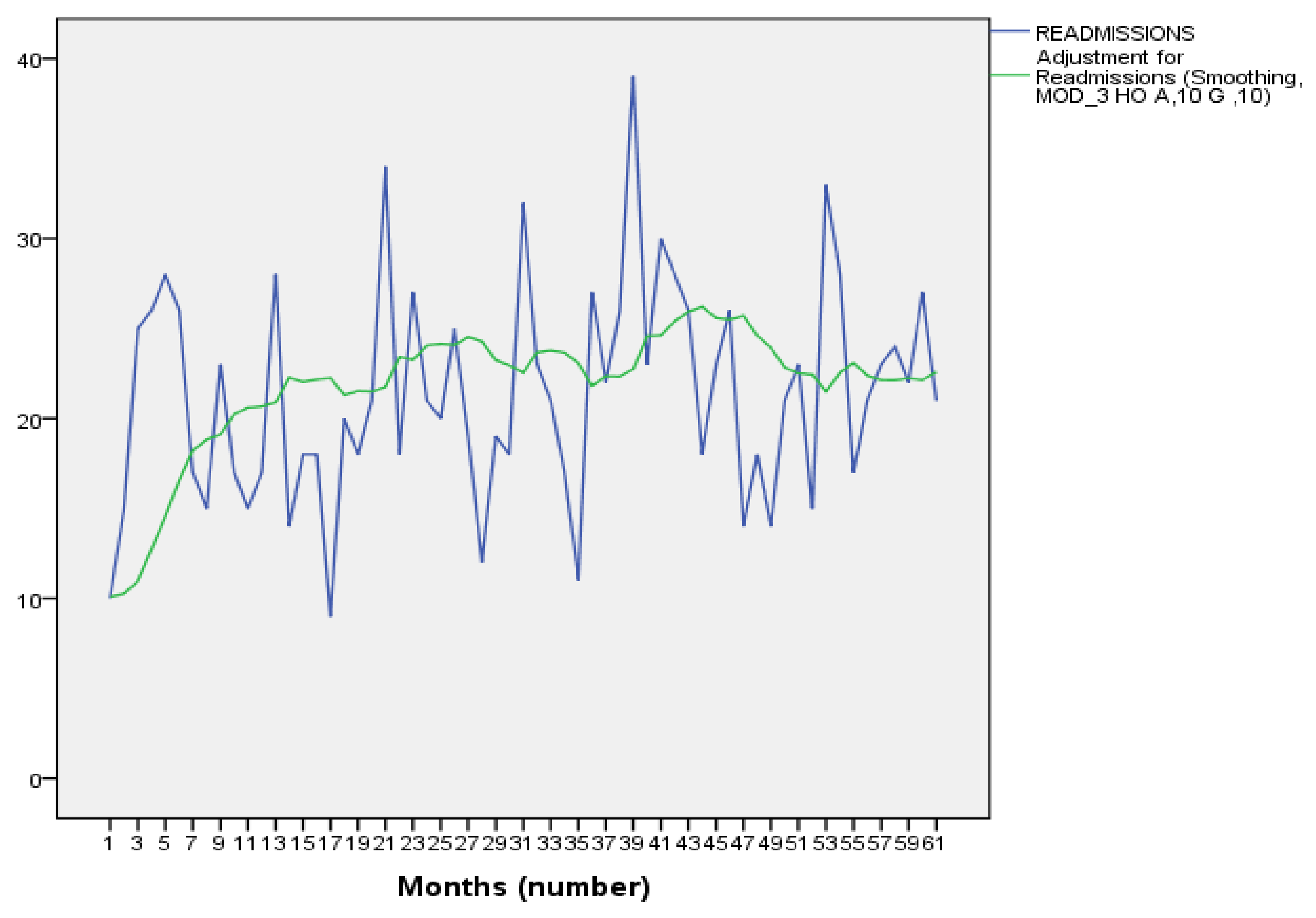
- The time series produced (Figure 1) showed that the number of ERs per month ranged from 9 to 38 in total. The obtained periodogram showed the absence of clear seasonality, which led to application of a Holt linear smoothing model, which predicted the behavior of the number of ERs for April 2016–April 2018. When analyzing the trend, the model that best fitted was the cubic model, with an R2 of 0.877 and with a high significance of the values (p < 0.001), which indicates that the ER will present a progressive rise and subsequent decline, remaining stable in the medium term. The fitting equation is: Z(t) = 10.050 + 1.086t − 0.026t2, and it is shown in Figure 1.
- 2.
- The application of the CHAID algorithm allowed us to observe the conclusions of the displayed tree (available as Supplementary Materials), which are:
- The variable “history of addiction” is the best predictor for ER.
- The highest probability of ER (22.8%) is found among those with a history of alcoholism or opiate addiction, a psychiatric history (26.7%), or those that take drugs of abuse as the type of drug involved (29.9%).
- The lowest probability of ER (6.1%) is among those with no addiction or psychiatric history (3.1%). If these patients have a psychiatric history or are unaware of it, the probability of ER rises to 7.7%.
- We emphasize that patients who present multiple addictions as a background have an ER probability of 17.2%, while those who present an association of medications and drugs of abuse as intoxicants involved have a 23.1% probability of ER.
3.2. Predisposing Factors for LRs (Total) and ERs
3.3. Bayesian Analysis Results
4. Discussion
5. Conclusions
- The profile of APC with readmission is a woman between 30 and 50 years of age who barely needs admission to units other than the ED. The most commonly used toxic substances are alcohol, benzodiazepines and cocaine.
- The results of the study allow us to identify predictors for different numbers of readmissions in the year after the index APC as well as for ERs; the detailed analysis of readmissions is thus revealed as a critical indicator of health outcomes in poisoned patients.
- The SAT-HULP thus makes it possible to assess, in depth, the evolution of APC in their environment. Active toxicovigilance programs are important tools for in-depth analysis of the evolution of APC, the consumption of resources, and for evaluation and improvement of the quality of the services involved in the care of intoxicated patients.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alonso Martínez, J.L.; Llorente Díez, B.; Echegaray Agara, M.; Urbieta Echezarreta, M.A.; González Arencibia, C. Reingreso hospitalario en Medicina Interna. An. Med. Interna 2001, 18, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Puente, A.; García-Alegría, J.; Gómez-Aracena, J.; Hidalgo-Rojas, L.; Lorenzo-Nogueiras, L.; Fernández-Crehuet-Navajas, J. Análisis de las causas de los reingresos en un hospital de agudos y su evitabilidad potencial. Med. Clin. 2002, 118, 500–505. [Google Scholar] [CrossRef]
- Yam, C.H.K.; Wong, E.L.Y.; Chan, F.W.K.; Wong, F.Y.Y.; Leung, M.C.M.; Yeoh, E.K. Measuring and preventing potentially avoidable hospital readmissions: A review of the literatura. Hong Kong Med. J. 2010, 16, 383–389. [Google Scholar] [PubMed]
- Anand, P.; Kranker, K.; Chen, A.Y. Estimating the hospital costs of inpatient harms. Health Serv. Res. 2019, 54, 86–96. [Google Scholar] [CrossRef]
- Blanc, A.L.; Fumeaux, T.; Stirneman, J.; Bonnabry, P.; Schaad, N. Hospital readmissions: Current problems and perspectives. Rev. Médicale Suisse 2017, 13, 117–120. [Google Scholar] [CrossRef]
- Lindquist, L.A.; Baker, D.W. Understanding preventable hospital readmissions: Masqueraders, markers, and true causal factors. J. Hosp. Med. 2011, 6, 51–53. [Google Scholar] [CrossRef]
- Caballero, A.; Carrillo, P.; Suárez, I.; Ibañez, M.; Acevedo, J.; Bautista, O. Características y factores pronósticos de reingresos hospitalarios en pacientes afiliados a la Organización Sanitas Internacional durante el año 2008. Rev. Med. Sanitas 2011, 14, 12–26. [Google Scholar]
- Larkin, C.; Di Blasi, Z.; Arensman, E. Risk factors for repetition of self-harm: A systematic review of prospective hospital-based studies. PLoS ONE 2014, 9, e84282. [Google Scholar] [CrossRef]
- Gummin, D.D.; Mowry, J.B.; Spyker, D.A.; Brooks, D.E.; Beuhler, M.C.; Rivers, L.J.; Hashem, H.A.; Ryan, M.L. 2018 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 36th Annual Report. Clin. Toxicol. 2019, 57, 1220–1413. [Google Scholar] [CrossRef]
- Observatorio Europeo de las Drogas y las Toxicomanias. Informe Europeo Sobre Drogas. Tendencias y Novedades 2018; Oficina de Publicaciones de la Unión Europea: Luxembourg, 2019; pp. 45–65. [Google Scholar]
- Kristinsson, J.; Palsson, R.; Gudjonsdottir, G.; Blondal, M.; Gudmundsson, S.; Snook, C. Acute poisonings in Iceland: A prospective nationwide study. Clin. Toxicol. 2008, 46, 126–132. [Google Scholar] [CrossRef]
- Majori, S.; Ricci, G.; Capretta, F.; Loss, R.; Baldovin, T.; Cigolini, D.; Tardivo, S.; Zannoni, M. The impact of acute intoxications in a toxicological unit care in north east Italy. J. Prev. Med. Hyg. 2012, 53, 8–13. [Google Scholar]
- Kaya, E.; Yilmaz, A.; Saritas, A.; Colakoglu, S.; Baltaci, D.; Kandis, H.; Kara, I.H. Acute intoxication cases admitted to the emergency department of a university hospital. Word J. Emerg. Med. 2015, 6, 54–59. [Google Scholar] [CrossRef][Green Version]
- Muñoz, R.; Borobia, A.; Qunitana, M.; Ramírez, E.; Frías, J.; Carcas, A. Desarrollo y validación de un programa de toxicovigilancia con detección automatizada de casos en un hospital terciario (SAT-HULP). Emergencias 2013, 25, 423–429. [Google Scholar]
- Satar, S.; Seydaoglu, G. Analysis of acute adult poisoning in a 6 year period and factors affecting the hospital stay. Adv. Ther. 2005, 22, 137–147. [Google Scholar] [CrossRef]
- Muñoz, R.; Borobia, A.; Qunitana, M.; Martínez, A.; Ramírez, E.; Muñoz, M.; Frías, J.; Carcas, A. Outcomes and Costs of Poisoned Patients Admitted Tertiary Hospital: Evaluation through a Toxicovigilance Program. PLoS ONE 2016, 11, e0152876. [Google Scholar] [CrossRef]
- Prescott, K.; Stratton, R.; Freyer, A.; Hall, I.; Le Jeune, I. Detailed analysis of self-poisoning episodes presenting to a large regional teaching hospital in the UK. Br. J. Clin. Pharmacol. 2009, 68, 260–268. [Google Scholar] [CrossRef]
- Descamps, A.K.; Vandijck, D.M.; Buylaert, W.A.; Mostin, M.A.; Paepe, P. Characteristics and costs in adults with acute poisoning admitted to the emergency department of a university hospital in Belgium. PLoS ONE 2019, 14, e0223479. [Google Scholar] [CrossRef]
- Haberkern, M.; Exadaktylos, A.K.; Marty, H. Alcohol intoxication at a university hospital acute medicine unit with special consideration of young adults: An 8-year observational study from Switzerland. Emerg. Med. J. 2010, 27, 199–202. [Google Scholar] [CrossRef]
- Hovda, K.; Bjornaas, M.; Skog, K.; Opdahl, A.; Drottning, P.; Ekeberg, O.; Jacobsen, D. Acute poisonings treated in hospitals in Oslo: A one-year prospective study (I): Pattern of poisoning. Clin. Toxicol. 2008, 46, 35–41. [Google Scholar] [CrossRef][Green Version]
- Vallersnes, O.M.; Jacobsen, D.; Ekeberg, O.; Brekke, M. Mortality, morbidity and follow-up after acute poisoning by substances of abuse: A prospective observational cohort study. Scand. J. Public Health 2018, 47, 452–461. [Google Scholar] [CrossRef]
- Heyerdahl, F.; Bjornaas, M.A.; Dahl, R.; Hovda, K.E.; Nore, A.K.; Ekeberg, O.; Jacobsen, D. Repetition of acute poisoning in Oslo: 1-Year prospective study. Br. J. Psychiatry 2009, 194, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Vallersnes, O.M.; Jacobsen, D.; Ekeberg, Ø.; Brekke, M. Factors associated with rapidly repeated acute poisoning by substances of abuse: A prospective observational cohort study. BMC Res. Notes 2018, 11, 724. [Google Scholar] [CrossRef] [PubMed]
- Vallersnes, O.M.; Jacobsen, D.; Ekeberg, Ø.; Brekke, M. Mortality and repeated poisoning after self-discharge during treatment for acute poisoning by substances of abuse: A prospective observational cohort study. BMC Emerg. Med. 2019, 19, 5. [Google Scholar] [CrossRef] [PubMed]
- Rafnsson, S.B.; Oliver, J.J.; Elton, R.A.; Bateman, D.N. Poisons admissions in Edinburgh 1981–2001: Agent trends and predictors of hospital readmissions. Hum. Exp. Toxicol. 2007, 26, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.C.; Benavides, A. El enfoque bayesiano. Otra manera de inferir. Gac. Sanit. 2001, 15, 341–346. [Google Scholar] [CrossRef]
- Carlin, B.P.; Louis, T.A. Bayes an Empirical Bayes Methods for Data Analysis, 2ª ed.; Chapman & Hall/CRC: New York, NY, USA, 2000. [Google Scholar]
- Perea-Milla, E.; Ayçaguer, L.C.S.; Cerdà, J.C.M.; Saiz, F.G.; Rivas-Ruiz, F.; Danet, A.; Vallecillo, M.R.; Oviedo-Joekes, E. Efficacy of prescribed injectable diacetylmorphine in the Andalusian trial. Bayesian analysis of responders and non-responders according to a multi domain outcomes index. Trials 2009, 10, 70. [Google Scholar] [CrossRef] [PubMed]
- García, M.C.; Arias, A.; Rodríguez, C.; Morcillo, A.; Aguirre-Jaime, A. Análisis de series temporales aplicado a intoxicaciones atendidas en urgencias hospitalarias. Emergencias 2011, 23, 193–199. [Google Scholar]
- Berwick, D.M.; Nolan, T.W.; Whittington, J. The Triple Aim: Care, health, and cost. Health Aff. 2008, 27, 759–769. [Google Scholar] [CrossRef]
- Kansagara, D.; Englander, H.; Salanitro, A.; Kagen, D.; Theobald, C.; Freeman, M.; Kripalani, S. Risk prediction models for hospital readmission. JAMA 2011, 306, 1688–1698. [Google Scholar] [CrossRef]
- Health Services Management Centre (HSMC). Evidence for Transforming Community Services. Review: Services for Long Term Conditions; University of Birmingham: Birmingham, UK, 2009. [Google Scholar]
- Krajewski, A.; Friedman, L. Hospital outcomes and economic costs from poisoning cases in Illinois. Clin. Toxicol. 2015, 53, 433–445. [Google Scholar] [CrossRef]
- McMahon, A.; Brohan, J.; Donnelly, M.; Fritzpatrick, G. Characteristics of patients admitted to the intensive care unit following self-poisoning and their impact on resource utilisation. Ir. J. Med. Sci. 2014, 183, 391–395. [Google Scholar] [CrossRef] [PubMed]

| Suicide (n = 474) | Abusive (n = 476) | Accidental (n = 18) | Grand Total (n = 968) | |
|---|---|---|---|---|
| Sex (n (%) women) | 300 (60.6) | 187 (37.7) | 8 (1.6) | 495 (51.1) |
| Age (mean (SD)) | 39.6 (14.7) | 41.3 (15.3) | 69.1 (23.3) | 41.0 (17.8) |
| History of addiction (n (%) YES) | 291 (43.7) | 373 (43.0) | 2 (0.3) | 666 (68.8) |
| Psychiatric history (n (%) YES) | 448 (58.6) | 313 (40.9) | 3 (0.4) | 764 (78.9) |
| Type of intoxicant (n (%)) | ||||
| Medication | 378 (91.0) | 22 (5.3) | 15 (3.6) | 415 (42.9) |
| Drug of abuse | 92 (16.8) | 454 (82.9) | 1 (0.2) | 547 (56.5) |
| Domestic product | 4 (80.0) | - | 1 (20.0) | 5 (0.5) |
| Industrial product | - | - | - | - |
| Other (includes food poisoning) | - | - | 1 (100.0) | 1 (0.1) |
| Symptoms on admission (n (%) YES) | 359 (43.1) | 466 (56.0) | 7 (0.8) | 832 (85.9) |
| Analytical determination (n (%) YES) | 146 (62.4) | 72 (30.8) | 16 (6.8) | 234 (24.1) |
| Digestive decontamination (n (%) YES) | 204 (94.4) | 11 (5.1) | 1 (0.5) | 216 (22.3) |
| Use of antidote (n (%) YES) | 100 (81.3) | 16 (13.0) | 7 (5.7) | 123 (12.7) |
| Patient destination (n (%)) | ||||
| Discharge from ED | 342 (43.1) | 434 (54.7) | 17 (2.1) | 793 (81.9) |
| Admission to ICU | 10 (90.9) | 1 (9.1) | - | 11 (1.1) |
| Admission to the Medicine Department | 5 (38.5) | 8 (61.5) | - | 13 (1.3) |
| Death | - | - | - | - |
| Transfer | 46 (83.6) | 8 (14.5) | 1 (1.8) | 55 (5.7) |
| Voluntary Discharge | 10 (32.5) | 21 (67.7) | - | 31 (3.2) |
| Admission to the Psychiatric Unit | 28 (90.3) | 3 (9.7) | - | 31 (3.2) |
| OR | CI 95% | p Value | |
|---|---|---|---|
| At least 1 Re-admission per year (n = 516) | |||
| Psychiatric History | |||
| Unknown * | 1.64 | 1.05–2.56 | 0.030 |
| Yes | 3.30 | 2.53–4.30 | <0.001 |
| No (Ref) | |||
| Addiction Background | |||
| Multiple addiction | 1.93 | 1.18–3.16 | 0.009 |
| Alcohol | 1.60 | 1.04–2.46 | 0.031 |
| Tobacco (Ref) | |||
| Type of Intoxication | |||
| Accidental | 0.50 | 0.26–0.96 | 0.036 |
| Abusive/Recreational (Ref) | |||
| Type of Intoxicant | |||
| Drugs of Abuse | 8.88 | 1.17–67.25 | 0.035 |
| Other (Ref) | |||
| 2 readmissions per year (n = 185) | |||
| Psychiatric History | |||
| Unknown | 3.77 | 1.81–7.83 | <0.001 |
| Yes | 7.13 | 4.19–12.13 | <0.001 |
| No (Ref) | |||
| Addiction Background | |||
| No | 0.32 | 0.17–0.62 | 0.001 |
| Alcohol | 1.96 | 1.03–3.72 | 0.040 |
| Tobacco (Ref) | |||
| Intoxicant-Drugs of Abuse Combination | |||
| No | 4.90 | 1.72–13.95 | 0.003 |
| Yes (Ref) | |||
| 3 or more readmissions per year | |||
| Sex | |||
| Female | 1.38 | 1.03–1.84 | 0.031 |
| Male (Ref) | |||
| Psychiatric History | |||
| Unknown | 5.66 | 2.94–10.87 | <0.001 |
| Yes | 10.88 | 6.49–18.21 | <0.001 |
| No (Ref) | |||
| Addiction History | |||
| Multiple addiction | 2.68 | 1.14–6.30 | 0.023 |
| Alcohol | 4.59 | 2.15–9.81 | <0.001 |
| Tobacco (Ref) | |||
| Combination of Intoxicants-Drugs of Abuse | |||
| No | 4.90 | 1.72–13.95 | 0.003 |
| Yes (Ref) | |||
| 3 or more readmissions per year (n = 267) | |||
| Sex | |||
| Female | 1.38 | 1.03–1.84 | 0.031 |
| Male (Ref) | |||
| Psychiatric History | |||
| Unknown | 0.33 | 2.94–10.87 | 0.000 |
| Yes | 0.26 | 6.49–18.21 | 0.000 |
| No (Ref) | |||
| Addiction History | |||
| Multiple addiction | 2.68 | 1.14–6.30 | 0.023 |
| Tobacco (Ref) | |||
| Intoxicant-Drugs of Abuse Combination | |||
| No | 9.01 | 2.76–29.38 | 0.000 |
| Yes (Ref) |
| HR | CI 95% | p Value | |
|---|---|---|---|
| Type of Intoxicant Drugs of Abuse | 9.81 | 1.29–74.74 | 0.028 |
| Type of Suicidal Intoxication | 1.42 | 1.02–1.96 | 0.035 |
| AH Alcohol * PH Unknown Interaction | 4.24 | 1.85–9.75 | 0.001 |
| AH Opioid * PH Unknown Interaction | 10.05 | 1.39–72.61 | 0.022 |
| AH Multiple addiction * PH Present Interaction | 2.72 | 1.87–3.96 | <0.001 |
| AH Absent * PH Present Interaction | 2.37 | 1.76–3.19 | <0.001 |
| AH Alcohol * PH Present Interaction | 5.72 | 4.27–7.68 | <0.001 |
| AH Opioid * PH Present Interaction | 7.89 | 3.65–17.08 | <0.001 |
| AH Cocaine * PH Present Interaction | 4.89 | 2.87–8.34 | <0.001 |
| AH Cannabis * PH Present Interaction | 4.64 | 2.33–9.23 | <0.001 |
| Odds Ratio Estimation | ||||
|---|---|---|---|---|
| Data: A priori probability interval (95%) | 1st Case | 2nd Case | ||
| OR | 1.170 | 2.060 | ||
| Lower Limit | 0.780 | 1.070 | ||
| Upper Limit | 1.760 | 3.970 | ||
| Data: Empirical confidence interval (95%) | ||||
| OR | 8.880 | 3.300 | ||
| Lower Limit | 1.170 | 2.415 | ||
| Upper Limit | 67.250 | 3.949 | ||
| Probability (OR > X) for selected points | ||||
| Point | 1.10 | 9.00 | 2.00 | 3.50 |
| Probability | 0.755 | 0.000 | 1.000 | 0.159 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muñoz Romo, R.; Borobia Pérez, A.M.; Mayayo Alvira, R.; Urroz, M.; Rodríguez Mariblanca, A.; Guijarro Eguinoa, F.J.; Diaz García, L.; Cobo Mora, J.; Rivera, A.; Torres, R.; et al. Acute Poisoning Readmissions to an Emergency Department of a Tertiary Hospital: Evaluation through an Active Toxicovigilance Program. J. Clin. Med. 2022, 11, 4508. https://doi.org/10.3390/jcm11154508
Muñoz Romo R, Borobia Pérez AM, Mayayo Alvira R, Urroz M, Rodríguez Mariblanca A, Guijarro Eguinoa FJ, Diaz García L, Cobo Mora J, Rivera A, Torres R, et al. Acute Poisoning Readmissions to an Emergency Department of a Tertiary Hospital: Evaluation through an Active Toxicovigilance Program. Journal of Clinical Medicine. 2022; 11(15):4508. https://doi.org/10.3390/jcm11154508
Chicago/Turabian StyleMuñoz Romo, Raúl, Alberto M. Borobia Pérez, Rosa Mayayo Alvira, Mikel Urroz, Amelia Rodríguez Mariblanca, Francisco J. Guijarro Eguinoa, Lucia Diaz García, Julio Cobo Mora, Angelica Rivera, Rosario Torres, and et al. 2022. "Acute Poisoning Readmissions to an Emergency Department of a Tertiary Hospital: Evaluation through an Active Toxicovigilance Program" Journal of Clinical Medicine 11, no. 15: 4508. https://doi.org/10.3390/jcm11154508
APA StyleMuñoz Romo, R., Borobia Pérez, A. M., Mayayo Alvira, R., Urroz, M., Rodríguez Mariblanca, A., Guijarro Eguinoa, F. J., Diaz García, L., Cobo Mora, J., Rivera, A., Torres, R., & Carcas Sansuán, A. J. (2022). Acute Poisoning Readmissions to an Emergency Department of a Tertiary Hospital: Evaluation through an Active Toxicovigilance Program. Journal of Clinical Medicine, 11(15), 4508. https://doi.org/10.3390/jcm11154508






