Abstract
Background: Hip fracture in the elderly means that between a quarter and a half of patients do not regain the levels of independence and walking ability that they previously had, according to the literature, after the fracture. Material and methods: Retrospective study of 537 patients aged ≥65 years who survived at the sixth month after fracturing their hip, of which the age, sex, type of fracture, surgical risk, independence (BI), walking ability, cognitive level (PS), comorbidities, indicated drugs, complications, surgical delay, hospital stay, and surgical technique are known. Using Pearson’s χ2 test, all the variables were contrasted with respect to the limitation or not, at the sixth month of the recovery of both independence and pre-admission walking ability. Multivariate analysis provides the necessary adjustment to the previous contrast. Results: We have found that age and PS ≥ 5 at admission limit recovery from both dependency and walking ability. Surgical risk, independence (BI) upon admission, anemia, and constipation during the hospital stay limit the recovery of the BI. Worsening of walking ability during the hospital stay and the type of extra-articular fracture, which was surgically treated by osteosynthesis, limit the recovery of walking ability. Conclusions: The factors previously exposed, and perhaps the fact that patients with hip fractures are not routinely referred to rehabilitation, explain the high proportion of patients who do not recover their previous independency (36%) or walking ability (45%) to the fact of fracturing.
1. Introduction
Hip fracture is the second most common fragility fracture after wrist fracture [1]. Between 28% and 35% of people aged ≥65 years have at least one fall at the same height per year that can potentially end in a fracture, and this incidence increases with age. It is called “multi-fall syndrome”, which affects 30–50% of the institutionalized elderly population [2]. The incidence of hip fracture in Spain was 2.1% each year between 1997 and 2010, a year in which it was 325 cases in men and 766 in women for every 105 inhabitants, and it affects more significantly those aged 85 years or older [3].
The most pessimistic information about the percentage of elderly people who recover their previous function after suffering a hip fracture is 23% [4], but the most optimistic estimate that it can reach more than half, in which case the functional deficit baseline, 25-hydroxy-vitamin D deficiency and complication with “delirium” [5,6] are the most limiting factors for mobility recovery.
Among the instruments used to standardize the measurement of the physical health of the elderly related to the activities of daily living (ADL), the Barthel Index (BI) [7] in its Spanish version [8] has been chosen as it is widely used in geriatrics.
In previous studies, there are multiple scales used to assess mobility and gait. The Tinetti scale [9] is one of them, the “Cumulated Ambulation Score” (CAS), described by Foss N.B., et al. in 2006 [10] and used by Danish authors [11]. Other scales are gait-specific, such as the aforementioned FIM scale [12], which has a module that assesses gait function. The “Functional Ambulation Classification” (FAC) was also initially described more than three decades ago for the evaluation of walking ability in stroke patients [13,14], but it has been used in elderly patients with hip fractures, too, is used in this studio [15,16], and has the advantage of its simplicity in clinical application. It is the one that we will apply in a summarized way, as it is exposed in material and methods.
Much research studies the recovery of patients in the context of rehabilitation programs. However, the results are not conclusive and more research is required [17]. However, there are not so many who study the factors that may limit the recovery of these patients.
A greater fear of falling after a hip fracture is related to the female sex, polypharmacy, poor physical functioning and daily activities, and depressive symptoms one year after the fracture occurred [18]. Frölich et al., in a prospective cohort study, found that those who were the frailest patients were the ones who failed to return to their independent living, but they consider that the majority of the community-dwelling patients returned to independent living only with a minor increase in care needs; they also consider that standing within 24 h from hip fracture surgery was vital in maximizing short-term functional recovery [19]. One systematic review proposed the hand grip strength and frailty as emerging significant predictors of poor functional outcomes and mortality in the literature, in addition to other predictors grouped in medical factors (comorbidity, anesthesia, sarcopenia), surgical factors (delay in intervention, type of fracture), socio-economic factors (age, sex, ethnicity) and system factors including lower case-volume centers [20]. Age, male sex, trochanteric fracture, preoperative delay, postoperative drainage use, serum albumin, and ADL at discharge and internal fixation are related to functional recovery [21,22]. Some of these factors can also influence mortality after hip fracture as advanced age, male sex, living in a rural area, diabetes, tumor, preoperative delay, and postoperative drainage use [22].
This research aims to study which factors exist in our population of patients aged ≥65 years, which limit, and to what degree, the recovery of the situation of independence (BI), as well as their ability to walk prior to suffering a hip fracture.
The hypothesis of this study is based on the fact that the factors that denote poor basal functioning, as well as the presence of health problems and other complications, will be factors that may influence the recovery of the baseline situation.
2. Materials and Methods
2.1. Study Design—Participants
In a retrospective longitudinal study, all patients were treated at the University Hospital of Burgos (HUBU). Inclusion criteria: Patients aged 65 years or older who, by a low energy mechanism, suffered a hip fracture in the biennium 14 March 2019–14 March 2021. All patients admitted to the HUBU with these characteristics were included in the study, followed after discharge from the outpatient clinics of the Orthopedic Surgery and Traumatology Service of the same hospital through face-to-face and non-face-to-face consultations through interviews with the patients, their families, and/or responsible caregivers. Exclusion criteria: Patients with peri-prosthetic fractures, peri-synthesis fractures, and pathological fractures, that is, on bones affected by primary tumor or metastasis, were excluded from the study; likewise, patients who were referred to other hospitals without completing the treatment or follow-up period for any cause, except death. Data collection was carried out on all patients who were admitted to the emergency room for hip fractures and underwent surgery by the Orthopedic Surgery and Traumatology Service.
2.2. Sample Size
The sample size was estimated following the procedure for finite populations, using the formula . The known population reported by the National Institute of Statistics (INE) (https://www.ine.es/jaxiT3/Tabla.htm?t=2852, accessed on 25 May 2022) and a similar study [23] was taken into account, establishing a proportion of hip fractures in the population of 0.389% (p = 0.000398, and its complementary q = 0.99602) and assuming a sampling error of 1% (δ2 = 0.01). Based on this, it was concluded that the sample should be made up of 152 patients with hip fractures under care by the HUBU.
2.3. Main Outcomes—Instruments
The head of the Traumatology Section of the Orthopedic Surgery and Traumatology (OST) Service was responsible for collecting the data from each participant’s electronic medical record for further analysis. In order to study variables that may influence cognitive impairment, sociodemographic data such as age (dichotomized in <85 and ≥85 years) and sex (woman/man) and clinical data such as the type of fracture (intracapsular/extracapsular), the type of treatment (surgical/conservative), the surgical technique (arthroplasty/synthesis), complications during admission such as “delirium” or constipation, the surgical risk assessed according to the American Society of Anesthesiologists Physical Status Classification (ASA) [24], prescription of different drugs before admission and after hospital discharge, and concomitant pathologies at the time of admission. The main variable refers to ambulation capacity according to the functional ambulation classification (FAC) [10,11] (categorized their levels 4–5 as “good”, 3–4 as “regular”, and 0–1 as “bad” walking ability).
There are multiple ways to standardize the measurement of the physical health of the elderly: the activities of daily living (ADL) index (“Activities of Daily Living” or “ADL”) [7] and the instrumental activities of daily living (IADL) [8]. In specific questions of mobility, the functional independence measure (FIM) [9] is available, which is fundamentally validated for patients with neurological diseases, and its application is complex. The Barthel Index (BI) [10] in its Spanish version [11] has been chosen because it is the most widely used tool in the functional assessment of elderly patients suffering from hip fracture [12,13,14,15,16]. The categorization of the BI has been performed in four: “1” (BI = 100): fully independent, “2” (100 < BI ≥ 90): slightly dependent, “3” (90 < BI ≥ 60): moderately dependent and “4” (BI < 60): severely or totally dependent. “BI Recovery” is the difference between the BI (variable with four categories 1 to 4) at the income and at the sixth month, so that, if the value is negative, it is understood that they did not recover. “Walking ability recovery” is the category difference in “walking ability” at admission and at the sixth month so that “they do not recover” if said difference is a negative value. The cognitive impairment was assessed using Pfeiffer Scale (PS) [25]. It is a questionnaire that collects the number of errors of the evaluated patient when ten simple questions are posed and establishes four categories of the definition of cognitive impairment depending on the dependence of people in the intellectual area: 0–2 errors is the absence of deterioration or autonomy in the intellectual area, 3–4 errors is slight impairment and help of other people in intellectually complex matters, 5–7 errors is moderate deterioration and require help on a regular basis but not always, and 8–10 errors denote severe deterioration and continuous supervision. In the present study, cognitive impairment according to PS is expressed as a dichotomous variable: absence of cognitive impairment or mild impairment (PS ≤ 4 errors) and moderate or severe cognitive impairment (PS ≥ 5 errors). Data on FAC, BI, PS, and institutionalization prior to admission, at discharge, and at 6 months if the patient survives is collected. All clinical or sociodemographic information is obtained in the emergency department, on the hospitalization floor, or in face-to-face or telematic consultations after hospital discharge.
2.4. Statistical Analysis
To characterize the sample, the mean and standard deviation (SD) were used in the case of continuous variables and absolute frequencies and percentages if the variables were categorical. Both categorical variables from more than two categories and continuous variables were dichotomized based on previous studies and tended to obtain groups as homogeneous as possible. Bivariate analyses were performed to study the relationship between clinical features at “BI Recovery” and “Walking ability recovery”, 6 months using the Pearson independence test (χ2), as well as the likelihood ratio. In the analyses with significant results, the ratio of advantages or “odds” (OR) with its limits (lower/upper) was also obtained. In addition, in order to quantify the magnitude of relationships of bivariate analysis and identify possible predictive factors of main variables at 6 months, depending on the different clinical characteristics, an analysis was performed using binary logistic regression, where dichotomous dependent variables are “BI Recovery” and “Walking ability recovery”. All the significant variables obtained in the previous bivariate analysis were included as independent in the referred multivariate study, and the OR = eβi∗(±Δi) with its limits (lower/upper) was also obtained too.
Statistical analysis was performed with SPSS software version 25 (IBM-Inc., Chicago, IL, USA). For the analysis of statistical significance, a p-value < 0.05 was established.
3. Results
3.1. Recovery of the Initial Situation
The study sample consisted of 665 people, 128 of whom died during the 6 months after hip fracture. The age of the participants was between 65 and 102 years, with a mean of 86.2 years, 76.7% women (n = 510) and 23.3% men (n = 155) (Figure 1). In the group of surviving patients in the series, 36.1% did not regain independence at the sixth month, nor did 44% regain walking ability prior to the fracture.
Figure 1.
Participants flow.
3.2. Influence on Lack of Recovery by 6th Month of the Category of the BI Prior to Admission
3.2.1. Regarding the Previous Situation or Admission
In the bivariate analysis carried out between the BI recovery variable (yes/no) with the variables studied that take into account the situation before the patient was admitted (Table 1), an association was found with age ≥ 85 years, type of extracapsular fracture, also comorbidities such as chronic renal failure and high blood pressure, likewise the use of antihypertensive drugs, all of which are risk factors for non-recovery. There is also a relationship with independence (BI at admission ≥ 60, BI at admission ≥ 90), better cognitive status (PS at admission ≤ 4), and better gait (FAC category ≤ 2). No association was found with age, sex, or institutionalization prior to admission.

Table 1.
Bivariate analysis recovery of the BI (yes/no); significant factors prior to or at admission.
Binary logistic regression (Table 2) (Nagerkelke’s R2 = 0.289) finds (in bold) age in completed years, surgical risk (ASA), independence (highest BI: 0–100), and cognitive impairment (number of errors in the EP) as risk factors for non-recovery of BI.

Table 2.
Binary logistic regression of recovery of the BI (yes/no); situation prior to admission.
3.2.2. Regarding the Effect That the Fracture and Admission Exert
We obtained the bivariate analysis (Table 3), and the following risk factors were found: the use of synthesis as a surgical technique, hospital stay ≥ 11 days, BI at discharge < 90, deterioration of at least one category in the BI between hospital admission and discharge, impairment of at least one category in the ability to walk, better cognitive status at discharge (PE ≤ 4), cognitive impairment in at least one category in the PS, “de novo” institutionalization at hospital discharge it associates greater risk than staying at home, and the following events: hemoglobinemia ≤ 8.5 mg/dL, being transfused with ≥3 packed red blood cells, delirium, and constipation. The variable’s type of treatment and surgical delay were not significant in this bivariate analysis.

Table 3.
Bivariate analysis recovery of the BI (yes/no); significant variables—effect of the fracture and outcome.
The multivariate analysis (Table 4) has estimated significant variables with adjustment for not regaining independence: older age, higher BI (0–100) at hospital discharge, but above all, deterioration of BI during admission, in addition to hemoglobinemia ≤ 8.5 mg/dL, and constipation.

Table 4.
Binary logistic regression of recovery of the BI (yes/no); situation during admission.
3.3. Influence on Lack of Recovery by 6th Month of the Category of the Walking Ability Prior to Admission
3.3.1. Regarding the Previous Situation or Admission
Using Pearson’s χ2 tests and likelihood ratio (χRV 2) with the dependent variable recovering (yes/no) walking ability (Table 5), risk factors have been found for non-recovery at the sixth month, age ≥ 85 years, extracapsular type of fracture, ASA III or IV surgical risk, BI < 90 prior to admission, moderate or severe cognitive impairment (PS ≥ 5), institutionalization prior to admission, comorbidities at admission: chronic anemia, heart failure, having the patient prescribed anticoagulants and proton-pump inhibitors before the fracture. The poor ability to walk before admission has been significant as a protective factor for non-recovery at six months; this effect does not change and gains greater associative strength in the multivariate adjustment. There is no association with sex or with BI at admission < 60 points.

Table 5.
Bivariate analysis recovery of the FAC (yes/no); variables significantly associated; situation prior to admission.
The binary logistic regression (Table 6) has obtained the only significant results (R2 = 0.500) for not recovering walking ability, thanks to the adjustment, in addition to older age, the extracapsular type of fracture, surgical risk, number of errors in PS, and use of proton-pump inhibitor, on or prior to admission. IB (0–100) independence and, above all, worse ambulation (FAC) prior to admission have been protective factors for the lack of recovery of gait; these two effects are found in the bivariate analysis.

Table 6.
Binary logistic regression of recovery of the FAC (yes/no); situation prior to admission.
3.3.2. Regarding the Effect That the Fracture and Admission Exert
In the bivariate analysis with variables during admission and at the end of it (Table 7), we have found that the following are risk factors for non-recovery of gait: surgical technique by synthesis, start of standing, and gait beyond the third postoperative day, BI < 90 at discharge, BI < 60 at discharge, poor walking ability at hospital discharge, impairment during admission of at least one category in ambulatory ability, cognitive impairment according to PS ≥ 5, loss during admission of at least one category according to the same PS, and new institution at discharge.

Table 7.
Bivariate analysis recovery of the FAC (yes/no); variables significantly associated; effect of the fracture and outcome.
We have also found various complications that occurred during admission as risk factors: hemoglobinemia ≤ 8.5 mg/dL, being transfused and if performed with three or more packed red blood cells, delirium, constipation, impaired kidney function during admission, urinary tract infection (UTI), acute urine retention (AUR), need to a new prescription of vitamin D at discharge.
There are four variables: deep venous thrombosis (DVT), acute ischemic stroke (AIS) during admission, liquid thickeners, and new neuroleptics prescription at hospital discharge, which are risk factors in the analysis, but the result must be interpreted with reservation, because in the 2 × 2 table, at least one box has expected values less than 5, and therefore, despite their significance, we will not include them in the multivariate analysis.
Neither the type of treatment nor the hospital stay, nor the surgical delay influence the non-recovery of walking capacity.
Institutionalization as a residential destination (new and not new) at discharge is a protector factor in the non-recovery of walking, contrary to new institutionalization, so patients with an institutional destination at discharge have significantly greater possibilities to maintain their previous level of capacity for ambulation.
The multivariate analysis (Table 8), with binary logistic regression (R2 = 0.275), only confirms as true factors associated with not recovering the ability to walk the loss of at least one category of ability to walk during admission and synthesis as a technique surgery used.

Table 8.
Binary logistic regression of recovery of the FAC (yes/no); situation during admission.
Functional loss during admission (see Table 9 and Table 10, as well as Figure 2) after hip fracture in the elderly in our series is basically related to cognitive impairment before said admission, but in a different direction. There is a direct relationship or risk factor regarding the deterioration of the ability to walk. On the other hand, there is an indirect relationship so that patients with greater cognitive impairment at admission experience less loss of independence during admission.

Table 9.
Profile of patient losing independence in at least one BI category during admission according to binary logistic regression.

Table 10.
Profile of patient losing independence in at least one FAC category (≥2 levels) during admission according to binary logistic regression.
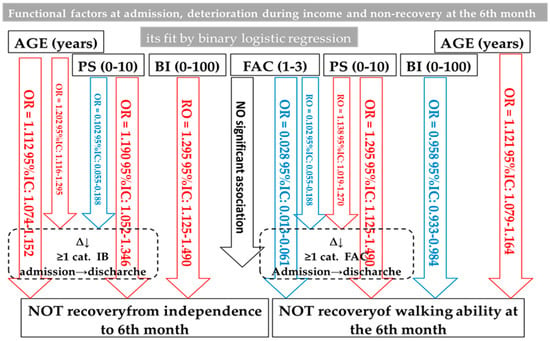
Figure 2.
Summary of the interaction between functional factors in the elderly with hip fracture in our patients.
Below (Figure 2), the relationships between functional variables are exposed so that in blue, we have those that prevent and in red, those that are risk factors for non-functional recovery in the sixth month.
4. Discussion
Age is the factor that, in almost any publication, is associated with the limitation in the recovery of the previous function after a hip fracture in the elderly and in any period of time: 2 and 6 months [26]; 4 months [27], 6 months [28,29], 8 months [30], 1 year [31,32], 6 y 18 months [33], or not specifying a certain time, but when a more or less specific rehabilitation program ends [34,35,36,37,38,39,40,41,42]. In general, men have the worst evolution, according to much of the literature consulted [36,37,43]. According to Sylliaas et al. [44], women have a worse evolution, although there are also authors who, coincidentally with our work, do not appreciate differences [32,45]. In our study, as in the literature consulted, age, both in bivariate and multivariate analysis, is a risk factor for the non-recovery of independence and, also, for the non-recovery of ambulatory capacity.
In our investigation, the average stay is not associated with a lack of functional recovery. Martin-Martin et al. [40] associate it with worse mobility and Orive et al. [33] with BI impairment. The surgical delay in this work does not condition the functional evolution either, but there are studies in which surgical delay ≥ 48 h limits mobility [28] or the recovery of independence [33].
The pathology associated with the patient who is admitted to be treated for a hip fracture has different importance. The frailty of the elderly can be defined by the number of severe or terminal chronic diseases that the patient has [46], obtaining an index that is adjusted for age and baseline functional status. Kua J. et al. [47] have highlighted that the previously known geriatric scale [48] called Reported Edmonton Frail Scale, has a high prognostic value in all hospital admissions for acute processes in the elderly, and specifically a significant impairment (OR = 6.19, p = 0.01) of basic activities of daily living (ADL) [49,50] in the sixth month after hip fracture.
The number of concurrent comorbidities has been described as a factor of poor functional prognosis at four months [41] that we have not found. In fact, in our multivariate adjustment, no comorbidity influences the recovery of function at six months. Parkinson’s disease has a proven relationship with ambulatory capacity in patients with hip fractures [51]. In addition, it has been described that hypertension and diabetes are comorbidities associated with a greater limitation of functional recovery [36,41]. In addition, it has been described that hypertension and diabetes are comorbidities associated with greater limitation of functional recovery [52,53]. The greater surgical risk of our patients limits the recovery of [43] independence in terms of the BI value, not as well as the recovery of the march in our research, as other authors refer [30,33].
Several authors [51,54] associate the need for help to walk or not being able to walk alone outside the residential setting before admission with not regaining independence (IADL) [55] a year after the fracture. McGilton et al. [56] consider that poor global functional status, gait, and cognitive status at admission are limiting to recovery. Lower BI and more errors in the PS impair both the global functional status and the ability to walk Mariconda M. et al. [57] at one year. In our series, cognitive impairment prior to admission limits the recovery of both independence and gait in the sixth month after the hip fracture. The most independent patients, according to the BI before the fracture in this series, are the ones with the most limited global functional recovery (BI) in the sixth month. This phenomenon and with the same index is described in the literature [33] with prospective research at 6 and 18 months. However, in our patients, functional deterioration during admission is directly related to said previous cognitive deterioration only in the case of walking. Patients with a worse baseline cognitive situation acquire a lesser loss of their independence between admission and discharge. Similarly, patients with worse gait have at admission (higher value of the FAC variable), as occurs with dependency, with less functional reserve at admission, less loss generated by the fracture, and they maintain levels at the sixth month not as different from the previous ones. Therefore, the high value of the FAC variable prevents the non-recovery of the gait function. The essential factor so that these functions, independence and ability to walk, are not recovered is their qualitative loss during admission, especially in the case of loss of dependency (OR = 25.43, 95% CI: 12.61–51.28). Our work coincides with Dubljanin-Raspopović E. et al. [27] in that cognitive impairment is a pre-eminent factor in global functional (BI) and gait non-recovery.
Our patients from a nursing home before fracture have, after adjusting variables, a recovery of BI and gait not significantly different from those who lived at home, coinciding with Ariza-Vega P. et al. [31]. Other works instead [32,42] consider that institutionalization prior to admission limits gait recovery.
The extra-articular fracture type has, in general, a worse functional prognosis in the literature [32,40,45,52], just as we have clearly found in our multivariate analysis regarding the non-recovery of gait function. The worse prognosis in the evolution of BI can, at least in part, be explained by age since our patients with extra-articular fractures have a higher mean age, as in almost all the literature [16,53]. Di Monaco [58] does not find differences in prognosis between the types of fracture. A meta-analysis [59] showed that the use of total arthroplasty in patients with displaced intracapsular fractures gives better functional results than osteosynthesis, and total hip arthroplasty, according to prospective studies, is preferable in this type of fracture both due to its functional outcome as having fewer complications [60,61,62]. The synthesis, in our research, by the bivariate analysis, is followed by less recovery of both dependency (BI) and walking capacity at six months. This effect, in the multivariate analysis, is annulled in terms of non-recovery of BI; and persists as a risk factor in the non-recovery of walking. The mean age of our survivors does not differ significantly between those who underwent synthesis or arthroplasty. The only complications that we have been able to relate to the functional prognosis after multivariate adjustment have been anemia, coinciding with Foss N.B. et al. [10], and constipation; however, for other authors [63], they are ulcers by pressure and “delirium”.
It is a relative limitation that the measurement of the evolution at six months is a shorter time than that of some publications, which was already mentioned that they take 12 or 18 months, although there is no lack of medium-term studies: six months like ours, even at two, and four months in some cases. It has been pointed out that most of the recovery of global independence (BI) occurs in the first trimester [51]. The scientific evidence of a retrospective observational study is less than that of a cohort study, fundamentally because it is a mere consultation of registered data, no matter how rigorous the anamnesis and record of it have been. Our hip fractures do not follow any rehabilitation program, which may be related to the high percentages of lack of functional recovery that we have; in agreement with Orive et al. [33] when they state that not referring to rehabilitation increases the possibility of deterioration of the BI prior to six months, more than two times (OR = 2.34, 95% CI: 1.31–4.16) and at 18 months more than three (OR = 3.18, 95% CI: 1.62–6.25) with respect to undergoing rehabilitation treatment.
As strengths, it should be noted that the sample is large enough. Includes all fractures treated by our hospital in relation to its health area. This minimizes potential selection biases that often accompany a retrospective study. Take all possible variables. In addition to performing statistical analysis comparing dichotomous qualitative variables, binary logistic regression, in which we also incorporate quantitative independent variables for adjustment, allows us to eliminate biases such as effect modification or interaction, especially in relation to age. Although retrospective, it is still a longitudinal study, which to a large extent allows its conclusions to be taken as a valid explanation of the knowledge of the factors that truly influence limiting functional recovery in the elderly with hip fractures in our environment.
The results of this research show the factors in our population of patients aged ≥65 years, which limit, and to what extent, the recovery of the situation of independence (IB), as well as their ability to walk before suffering a hip fracture, as established in the objective of the research.
5. Conclusions
The factors associated with both the lower recovery of the BI and the ability to walk are older age and worse cognitive status at admission. Perhaps the lack of referral to rehabilitation of our patients is a very important factor to take into account in the poor recovery from dependency and walking.
Limitations to the recovery of independence are one’s own independence (high BI) on admission and discharge, the loss of it during admission, and the high surgical risk (ASA).
Both dependency (low BI) as well as impaired ambulatory capacity during admission limit recovery of gait.
Patients suffering from extracapsular fractures and surgical treatment by synthesis limit the recovery of walking in the sixth month. Likewise, patients taking proton-pump inhibitors prior to admission have less recovery from walking.
Hemoglobinemia < 8.5 mg/dL, as well as constipation, are the complications that are associated with a worse prognosis of dependence, but not “delirium”.
Sex does not influence, neither have any comorbidity been found, nor the greater number of concomitant comorbid processes with hip fracture related to functional prognosis
Author Contributions
Conceptualization, E.G.M., E.G.G. and A.d.P.M.-R.; methodology, E.G.M., E.G.G. and J.J.G.-B.; software, E.G.M., E.G.G. and M.S.-P.; validation, E.G.M., E.G.G., A.d.P.M.-R. and J.J.G.-B.; formal analysis, E.G.M., E.G.G. and M.S.-P.; investigation, E.G.M. and E.G.G.; resources, E.G.M., E.G.G., A.d.P.M.-R. and J.J.G.-B.; data curation, E.G.M., E.G.G., A.d.P.M.-R. and J.J.G.-B.; writing—original draft preparation, E.G.G. and J.G.-S.; writing—review and editing, E.G.G., M.S.-P. and J.G.-S.; visualization, E.G.M., E.G.G., A.d.P.M.-R., J.J.G.-B., M.S.-P. and J.G.-S.; supervision, J.G.-S. and J.J.G.-B.; project administration, E.G.M., E.G.G. and J.J.G.-B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee for Drug Research of the Health Area of Burgos and Soria (CEIm 2537, approved on 27 April 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest. Official Defense Bulletin certifies that Enrique González Marcos belongs to the Military Corps of Health in the Scale of Officers.
References
- Kanis, J.A.; McCloskey, E.V.; Johansson, H.; Cooper, C.; Rizzoli, R.; Reginster, J.-Y. European Guidance for the Diagnosis and Management of Osteoporosis in Postmenopausal Women. Osteoporos. Int. 2013, 24, 23–57. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Age-Friendly Cities: A Guide; World Health Organization: Geneva, Switzerland, 2007; ISBN 9241547308. [Google Scholar]
- Azagra, R.; López-Expósito, F.; Martin-Sánchez, J.C.; Aguyé, A.; Moreno, N.; Cooper, C.; Díez-Pérez, A.; Dennison, E.M. Changing Trends in the Epidemiology of Hip Fracture in Spain. Osteoporos. Int. 2014, 25, 1267–1274. [Google Scholar] [CrossRef] [PubMed]
- Ekegren, C.L.; Edwards, E.R.; Page, R.; Hau, R.; De Steiger, R.; Bucknill, A.; Liew, S.; Oppy, A.; Gabbe, B.J. Twelve-Month Mortality and Functional Outcomes in Hip Fracture Patients under 65 Years of Age. Injury 2016, 47, 2182–2188. [Google Scholar] [CrossRef]
- Vochteloo, A.J.H.; Moerman, S.; Tuinebreijer, W.E.; Maier, A.B.; de Vries, M.R.; Bloem, R.M.; Nelissen, R.G.H.H.; Pilot, P. More than Half of Hip Fracture Patients Do Not Regain Mobility in the First Postoperative Year. Geriatr. Gerontol. Int. 2013, 13, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Pioli, G.; Lauretani, F.; Pellicciotti, F.; Pignedoli, P.; Bendini, C.; Davoli, M.L.; Martini, E.; Zagatti, A.; Giordano, A.; Nardelli, A.; et al. Modifiable and Non-Modifiable Risk Factors Affecting Walking Recovery after Hip Fracture. Osteoporos. Int. 2016, 27, 2009–2016. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.I. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Baztán, J.J.; del Molino, J.P.; Alarcón, T.; Cristóbal, E.S.; Izquierdo, G. Índice de Barthel: Instrumento Válido Para La Valoración Functional de Pacientes Con Enfermedad Cerebrovascular. Rev. Esp. Geriatr. Gerontol. 1993, 28, 32–40. [Google Scholar]
- Tinetti, M.E. Performance-Oriented Assessment of Mobility Problems in Elderly Patients. J. Am. Geriatr. Soc. 1986, 34, 119–126. [Google Scholar] [CrossRef]
- Foss, N.B.; Kristensen, M.T.; Kehlet, H. Prediction of Postoperative Morbidity, Mortality and Rehabilitation in Hip Fracture Patients: The Cumulated Ambulation Score. Clin. Rehabil. 2006, 20, 701–708. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Andersen, L.; Bech-Jensen, R.; Moos, M.; Hovmand, B.; Ekdahl, C.; Kehlet, H. High Intertester Reliability of the Cumulated Ambulation Score for the Evaluation of Basic Mobility in Patients with Hip Fracture. Clin. Rehabil. 2009, 23, 1116–1123. [Google Scholar] [CrossRef]
- Ottenbacher, K.J.; Hsu, Y.; Granger, C.V.; Fiedler, R.C. The Reliability of the Functional Independence Measure: A Quantitative Review. Arch. Phys. Med. Rehabil. 1996, 77, 1226–1232. [Google Scholar] [CrossRef]
- Holden, M.K.; Gill, K.M.; Magliozzi, M.R.; Nathan, J.; Piehl-Baker, L. Clinical Gait Assessment in the Neurologically Impaired: Reliability and Meaningfulness. Phys. Ther. 1984, 64, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Holden, M.K.; Gill, K.M.; Magliozzi, M.R. Gait Assessment for Neurologically Impaired Patients: Standards for Outcome Assessment. Phys. Ther. 1986, 66, 1530–1539. [Google Scholar] [CrossRef] [PubMed]
- Moreno, J.A.; Garcia, I.; Serra, J.A.; Nunez, C.; Bellon, J.M.; Alvarez, A. Comparative Study of Two Rehabilitation Models in Hip Fracture. Rehabilitación 2006, 40, 123. [Google Scholar] [CrossRef]
- Takahashi, A.; Naruse, H.; Kitade, I.; Shimada, S.; Tsubokawa, M.; Kokubo, Y.; Matsumine, A. Functional Outcomes after the Treatment of Hip Fracture. PLoS ONE 2020, 15, e0236652. [Google Scholar] [CrossRef]
- Handoll, H.H.G.; Cameron, I.D.; Mak, J.C.S.; Panagoda, C.E.; Finnegan, T.P. Multidisciplinary Rehabilitation for Older People with Hip Fractures. Cochrane Database Syst. Rev. 2021. [Google Scholar] [CrossRef] [PubMed]
- Jaatinen, R.; Luukkaala, T.; Hongisto, M.T.; Kujala, M.A.; Nuotio, M.S. Factors Associated with and 1-Year Outcomes of Fear of Falling in a Geriatric Post-Hip Fracture Assessment. Aging Clin. Exp. Res. 2022, 1–10. [Google Scholar] [CrossRef]
- Frandsen, C.F.; Stilling, M.; Glassou, E.N.; Hansen, T.B. The Majority of Community-Dwelling Hip Fracture Patients Return to Independent Living with Minor Increase in Care Needs: A Prospective Cohort Study. Arch. Orthop. Trauma Surg. 2022, 1–10. [Google Scholar] [CrossRef]
- Xu, B.Y.; Yan, S.; Low, L.L.; Vasanwala, F.F.; Low, S.G. Predictors of Poor Functional Outcomes and Mortality in Patients with Hip Fracture: A Systematic Review. BMC Musculoskelet. Disord. 2019, 20, 568. [Google Scholar] [CrossRef]
- Ju, J.; Zhang, P.; Jiang, B. Risk Factors for Functional Outcomes of the Elderly with Intertrochanteric Fracture: A Retrospective Cohort Study. Orthop. Surg. 2019, 11, 643–652. [Google Scholar] [CrossRef]
- Meng, D.; Bai, X.; Wu, H.; Yao, S.; Ren, P.; Bai, X.; Lu, C.; Song, Z. Patient and Perioperative Factors Influencing the Functional Outcomes and Mortality in Elderly Hip Fractures. J. Investig. Surg. 2021, 34, 262–269. [Google Scholar] [CrossRef] [PubMed]
- INE. Población Por Provincias y Sexo. 2852. Available online: https://www.ine.es/jaxiT3/Tabla.htm?t=2852 (accessed on 13 June 2022).
- Johansen, A.; Tsang, C.; Boulton, C.; Wakeman, R.; Moppett, I. Understanding Mortality Rates after Hip Fracture Repair Using ASA Physical Status in the National Hip Fracture Database. Anaesthesia 2017, 72, 961–966. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, E. A Short Portable Mental Status Questionnaire for the Assessment of Organic Brain Deficit in Elderly Patients. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Cornwall, R.; Gilbert, M.S.; Koval, K.J.; Strauss, E.; Siu, A.L. Functional Outcomes and Mortality Vary among Different Types of Hip Fractures: A Function of Patient Characteristics. Clin. Orthop. Relat. Res. 2004, 425, 64–71. [Google Scholar] [CrossRef]
- Dubljanin-Raspopović, E.; Marković-Denić, L.; Matanović, D.; Grajić, M.; Krstić, N.; Bumbaširević, M. Is Pre-Fracture Functional Status Better than Cognitive Level in Predicting Short-Term Outcome of Elderly Hip Fracture Patients? Arch. Med. Sci. AMS 2012, 8, 115. [Google Scholar] [CrossRef]
- Maggi, S.; Siviero, P.; Wetle, T.; Besdine, R.W.; Saugo, M.; Crepaldi, G.F. A Multicenter Survey on Profile of Care for Hip Fracture: Predictors of Mortality and Disability. Osteoporos. Int. 2010, 21, 223–231. [Google Scholar] [CrossRef]
- Ganczak, M.; Chrobrowski, K.; Korzeń, M. Predictors of a Change and Correlation in Activities of Daily Living after Hip Fracture in Elderly Patients in a Community Hospital in Poland: A Six-Month Prospective Cohort Study. Int. J. Environ. Res. Public Health 2018, 15, 95. [Google Scholar] [CrossRef]
- Siebens, H.C.; Sharkey, P.; Aronow, H.U.; Horn, S.D.; Munin, M.C.; DeJong, G.; Smout, R.J.; Radnay, C.S. Outcomes and Weight-Bearing Status during Rehabilitation after Arthroplasty for Hip Fractures. PM&R 2012, 4, 548–555. [Google Scholar]
- Ariza-Vega, P.; Jiménez-Moleón, J.J.; Kristensen, M.T. Non-Weight-Bearing Status Compromises the Functional Level up to 1 Yr after Hip Fracture Surgery. Am. J. Phys. Med. Rehabil. 2014, 93, 641–648. [Google Scholar] [CrossRef]
- Pajulammi, H.M.; Pihlajamäki, H.K.; Luukkaala, T.H.; Nuotio, M.S. Pre-and Perioperative Predictors of Changes in Mobility and Living Arrangements after Hip Fracture—A Population-Based Study. Arch. Gerontol. Geriatr. 2015, 61, 182–189. [Google Scholar] [CrossRef]
- Orive, M.; Anton-Ladislao, A.; García-Gutiérrez, S.; Las Hayas, C.; González, N.; Zabala, J.; Quintana, J.M. Prospective Study of Predictive Factors of Changes in Pain and Hip Function after Hip Fracture among the Elderly. Osteoporos. Int. 2016, 27, 527–536. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, D.; Friger, M.; Lieberman, D. Rehabilitation Outcome Following Hip Fracture Surgery in Elderly Diabetics: A Prospective Cohort Study of 224 Patients. Disabil. Rehabil. 2007, 29, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.T.; Kehlet, H. Most Patients Regain Prefracture Basic Mobility after Hip Fracture Surgery in a Fast-Track Programme. Dan. Med. J. 2012, 59, A4447. [Google Scholar]
- Semel, J.; Gray, J.M.; Ahn, H.J.; Nasr, H.; Chen, J.J. Predictors of Outcome Following Hip Fracture Rehabilitation. PM&R 2010, 2, 799–805. [Google Scholar]
- Luk, J.K.H.; Chiu, P.K.C.; Tam, S.; Chu, L.W. Relationship between Admission Albumin Levels and Rehabilitation Outcomes in Older Patients. Arch. Gerontol. Geriatr. 2011, 53, 84–89. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Foss, N.B.; Ekdahl, C.; Kehlet, H. Prefracture Functional Level Evaluated by the New Mobility Score Predicts In-Hospital Outcome after Hip Fracture Surgery. Acta Orthop. 2010, 81, 296–302. [Google Scholar] [CrossRef]
- Tan, A.K.H.; Taiju, R.; Menon, E.B.; Koh, G.C. Postoperated Hip Fracture Rehabilitation Effectiveness and Efficiency in a Community Hospital. Ann. Acad. Med. Singap. 2014, 43, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Martín-Martín, L.M.; Arroyo-Morales, M.; Sánchez-Cruz, J.J.; Valenza-Demet, G.; Valenza, M.C.; Jiménez-Moleón, J.J. Factors Influencing Performance-Oriented Mobility after Hip Fracture. J. Aging Health 2015, 27, 827–842. [Google Scholar] [CrossRef]
- Gialanella, B.; Ferlucci, C.; Monguzzi, V.; Prometti, P. Determinants of Outcome in Hip Fracture: Role of Daily Living Activities. Eur. J. Phys. Rehabil. Med. 2015, 51, 253–260. [Google Scholar]
- Cary Jr, M.P.; Pan, W.; Sloane, R.; Bettger, J.P.; Hoenig, H.; Merwin, E.I.; Anderson, R.A. Self-Care and Mobility Following Postacute Rehabilitation for Older Adults with Hip Fracture: A Multilevel Analysis. Arch. Phys. Med. Rehabil. 2016, 97, 760–771. [Google Scholar] [CrossRef]
- Cohn, M.R.; Cong, G.-T.; Nwachukwu, B.U.; Patt, M.L.; Desai, P.; Zambrana, L.; Lane, J.M. Factors Associated with Early Functional Outcome after Hip Fracture Surgery. Geriatr. Orthop. Surg. Rehabil. 2016, 7, 3–8. [Google Scholar] [CrossRef]
- Sylliaas, H.; Thingstad, P.; Wyller, T.B.; Helbostad, J.; Sletvold, O.; Bergland, A. Prognostic Factors for Self-Rated Function and Perceived Health in Patient Living at Home Three Months after a Hip Fracture. Disabil. Rehabil. 2012, 34, 1225–1231. [Google Scholar] [CrossRef]
- Shakouri, S.K.; Eslamian, F.; Azari, B.K.; Sadeghi-Bazargani, H.; Sadeghpour, A.; Salekzamani, Y. Predictors of Functional Improvement among Patients with Hip Fracture at a Rehabilitation Ward. Pak. J. Biol. Sci. 2009, 12, 1516–1520. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Press, Y.; Grinshpun, Y.; Berzak, A.; Friger, M.; Clarfield, A.M. The Effect of Co-Morbidity on the Rehabilitation Process in Elderly Patients after Hip Fracture. Arch. Gerontol. Geriatr. 2007, 45, 281–294. [Google Scholar] [CrossRef]
- Kua, J.; Ramason, R.; Rajamoney, G.; Chong, M.S. Which Frailty Measure Is a Good Predictor of Early Post-Operative Complications in Elderly Hip Fracture Patients? Arch. Orthop. Trauma Surg. 2016, 136, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Hilmer, S.N.; Perera, V.; Mitchell, S.; Murnion, B.P.; Dent, J.; Bajorek, B.; Matthews, S.; Rolfson, D.B. The Assessment of Frailty in Older People in Acute Care. Australas. J. Ageing 2009, 28, 182–188. [Google Scholar] [CrossRef]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of Illness in the Aged: The Index of ADL: A Standardized Measure of Biological and Psychosocial Function. JAMA 1963, 185, 914–919. [Google Scholar] [CrossRef]
- Nouri, F.M.; Lincoln, N.B. An Extended Activities of Daily Living Scale for Stroke Patients. Clin. Rehabil. 1987, 1, 301–305. [Google Scholar] [CrossRef]
- Lin, P.-C.; Chang, S.-Y. Functional Recovery among Elderly People One Year after Hip Fracture Surgery. J. Nurs. Res. JNR 2004, 12, 72–82. [Google Scholar] [CrossRef]
- Thingstad, P.; Egerton, T.; Ihlen, E.F.; Taraldsen, K.; Moe-Nilssen, R.; Helbostad, J.L. Identification of Gait Domains and Key Gait Variables Following Hip Fracture. BMC Geriatr. 2015, 15, 150. [Google Scholar] [CrossRef] [PubMed]
- Hagino, H.; Furukawa, K.; Fujiwara, S.; Okano, T.; Katagiri, H.; Yamamoto, K.; Teshima, R. Recent Trends in the Incidence and Lifetime Risk of Hip Fracture in Tottori, Japan. Osteoporos. Int. 2009, 20, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Ingemarsson, A.H.; Frandin, K.; Mellstrom, D.; Moller, M. Walking Ability and Activity Level after Hip Fracture in the Elderly–a Follow-Up. J. Rehabil. Med. 2003, 35, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- McGilton, K.S.; Chu, C.H.; Naglie, G.; van Wyk, P.M.; Stewart, S.; Davis, A.M. Factors Influencing Outcomes of Older Adults after Undergoing Rehabilitation for Hip Fracture. J. Am. Geriatr. Soc. 2016, 64, 1601–1609. [Google Scholar] [CrossRef]
- Mariconda, M.; Costa, G.G.; Cerbasi, S.; Recano, P.; Orabona, G.; Gambacorta, M.; Misasi, M. Factors Predicting Mobility and the Change in Activities of Daily Living after Hip Fracture: A 1-Year Prospective Cohort Study. J. Orthop. Trauma 2016, 30, 71–77. [Google Scholar] [CrossRef]
- Di Monaco, M.; Castiglioni, C.; De Toma, E.; Gardin, L.; Giordano, S.; Tappero, R. Handgrip Strength Is an Independent Predictor of Functional Outcome in Hip-Fracture Women: A Prospective Study with 6-Month Follow-Up. Medicine 2015, 94, e542. [Google Scholar] [CrossRef] [PubMed]
- Rogmark, C.; Johnell, O. Primary Arthroplasty Is Better than Internal Fixation of Displaced Femoral Neck Fractures: A Meta-Analysis of 14 Randomized Studies with 2289 Patients. Acta Orthop. 2006, 77, 359–367. [Google Scholar] [CrossRef]
- Tidermark, J.; Ponzer, S.; Svensson, O.; Söderqvist, A.; Törnkvist, H. Internal Fixation Compared with Total Hip Replacement for Displaced Femoral Neck Fractures in the Elderly: A Randomised, Controlled Trial. J. Bone Jt. Surg. Br. 2003, 85, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Blomfeldt, R.; Törnkvist, H.; Ponzer, S.; Söderqvist, A.; Tidermark, J. Displaced Femoral Neck Fracture: Comparison of Primary Total Hip Replacement with Secondary Replacement after Failed Internal Fixation: A 2-Year Follow-up of 84 Patients. Acta Orthop. 2006, 77, 638–643. [Google Scholar] [CrossRef]
- Blomfeldt, R.; Törnkvist, H.; Eriksson, K.; Söderqvist, A.; Ponzer, S.; Tidermark, J. A Randomised Controlled Trial Comparing Bipolar Hemiarthroplasty with Total Hip Replacement for Displaced Intracapsular Fractures of the Femoral Neck in Elderly Patients. J. Bone Jt. Surg. Br. 2007, 89, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Uriz-Otano, F.; Uriz-Otano, J.I.; Malafarina, V. Factors Associated with Short-Term Functional Recovery in Elderly People with a Hip Fracture. Influence of Cognitive Impairment. J. Am. Med. Dir. Assoc. 2015, 16, 215–220. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).