Provider Perspectives on Sleep Apnea from Appalachia: A Mixed Methods Study
Abstract: Background
1. Introduction
2. Materials and Methods
2.1. Qualitative Methods
2.2. Quantitative Methods
2.3. Statistical Analysis
2.3.1. Qualitative Analysis: Focus Groups
2.3.2. Quantitative Analysis
3. Results
3.1. Questionnaire Results
3.2. Focus Group Themes
3.2.1. Theme 1: Barriers to OSA Care Delivery
“And lack of transportation. Most of the patients I see, they want to go close to here and there’s only one facility here [sleep specialist] and sometimes scheduling is a nightmare just because you cannot get ahold of anybody there.”
“[T]here’s nothing here locally; they have to go Charleston or a lot of the other what have you and a lot of these people do not have cars or can’t pay four zillion dollars, if they can’t afford for somebody to transport them, then that’s the problem.”
“The constraints that I’ve seen though, nobody wants to do an overnight sleep study and some of the insurances don’t want to pay for the home sleep studies, they only want them to go to a site and nobody wants to do that…”
“I don’t know if it’s related to the [DME] company versus a patient, but they [the patient] will usually come to you first and say, ‘Oh, I couldn’t get that last thing to work or whatever’. So, I don’t know if it’s because on that end they’re [the DME company] hard to get in contact with or they [the patient] dropped the ball.
“[T]here’s certainly some patients who don’t do well with CPAP and they probably don’t tell anybody and just don’t get treatment.”
“They [patients] don’t tell you if it’s actually not working I think.”
“The patients are not very successful with trying to contact the companies once they’ve dropped the equipment…. It’ll be stuck on us to try to get back in contact with the third [party] company.”
“Everybody in my practice complains of fatigue. And almost everybody complains of fatigue and fatigue is such a broad diagnosis. A lot of them you’ll ask them, ‘Do you snore’? ‘Well, I don’t know if I do or not’. They’ll giggle and say, ‘I don’t listen to myself sleep’”.
“I have to say in all honesty I think over my career I’ve probably done a lousy job of screening for sleep apnea. And I’ve probably only referred people for testing when they said they were sleepy. And, um, and even then, I think it was low down on my list of things to consider to do a sleep study and to think about sleep apnea.”
“I don’t think I’m screening and I don’t think I’m doing follow up, um, uh, gosh, questions related to it. It’s really not on, on my radar.”
“I, uh, learned a little bit more about sleep apnea in the past several years from continuing education class. But I think there’s a lot I don’t know.”
“If you mean do I have a questionnaire that I ask my patients or have them complete, the answer is no. But if you ask me if I screen the patient, I do. If you’re obese and hypertensive, if you’re obese and complain of not being able to sleep well at night, or that you wake up coughing or choking along with GERD symptoms, I mean, I screen that way.”
“I was going to say I can read it [the results] and understand some. The last one I had, I thought it was kind of difficult to interpret the gist of the wording and stuff on the report.”
“No, I feel more comfortable when I get the results and seeing its positive to send them [patients] somebody that can do that, not that I wouldn’t, if I had the training, feel like I could do it. I’ve just never had the training.”
“I just don’t know like, you know, change in settings, you know, how many… if they’re [patients] still having episodes of apnea, you know, all of the adjustments you have to make on the machines, I really don’t even know where to start.”
“I just refer and let them [specialists] manage it. I mean, if uh… Even in the dental appliances, I would not know where to… who to approach to about this fitting mouthpieces and things that they do, so I just, I just assume the uh, sleep center knows all that.”
“I only ask them [patients] the last time that their equipment was replaced, like their face mask and that type of stuff, but outside of that I would have no clue.”
“14% of people are uninsured and then you heard people comment that some of the insurances don’t cover this specific test, or that specific, so definitely healthcare coverage is also a barrier.”
“People’s ability to get a test. And, and sometimes, um, they can’t afford it. I, I do, um, patient physicals and the, the DOT [Department of Transportation] requires that everybody who uses a CPAP get a, an annual sleep study. And, um, we really run into a problem that a lot of these guys can’t, or ladies, can’t afford the follow-up sleep study or the follow-up visit. I’m not sure why it’s not well covered by insurance.”
“[T]he other thing is I noticed even before I started doing those physicals that some insurers prefer to just do the overnight sleep study without, uh, referral to a specialist, and so then I was left holding the results and was not real happy about that. So, so to me, the barrier, the biggest barrier is cost and coverage.”
“And then they [dental professional] want some ridiculous amount for the, the [oral] appliance. People don’t have the money.”
“And, and, and besides those that pay for it, it’s a question of does the specialist accept that kind of insurance?…. Because if the reimbursement is low, and I think that’s an issue with our person in XXX.”
3.2.2. Theme 2: Facilitators to OSA Care Delivery
“They [specialist and DME] pretty much take care of all that stuff. As long as they do all that, then I’m pretty comfortable with that. But if they don’t, which I’ve never seen them not, we titrate the machines and do all that. And then they will follow them only if they have an underlying COPD or something like that, I think pulmonary gets involved. But other than that, once they’re diagnosed and their machines are titrated and all that good stuff, they [patients] just stay with us.”
“I’ve never had any patient that closed the door on that discussion with me in my practice. They’re usually very open. They feel so bad, and they want to figure out why, whether they believe that or not is the question, but they’re open to the possibilities [of getting assessed for OSA].”
“A lot of them [patients] are these big burly gentlemen that are very manly, and they don’t want to say that, ‘Yeah. Well, maybe something’s not right. I’m not tired’. But yet they can’t lift five pounds, because they are so tired. So, you have this, no disrespect, but this ‘man mentality’ to some of these guys.”
“I mean, it’s my responsibility, but since you’re conducting this study, I would be interested in more education on it [OSA and CPAP]”.
“I probably would consider learning how to manage it [OSA] more myself and prescribe CPAP. Um, I’m sort of hesitant to say that ‘cause I, you know, you, you worry about getting overwhelmed with things. My worry with that would be the clinical time to do it”.
3.3. EMR Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Adult Obesity Prevalence Maps for All 50 States, the District of Columbia, and US Territories. Available online: https://www.cdc.gov/obesity/data/prevalence-maps.html (accessed on 10 January 2022).
- Centers for Disease Control and Prevention. Heart Disease Mortality by State. Available online: https://www.cdc.gov/nchs/pressroom/sosmap/heart_disease_mortality/heartdisease.htm (accessed on 10 January 2022).
- Centers for Disease Control and Prevention. COPD Prevalence by State in the United States. Available online: https://www.cdc.gov/copd/data.html (accessed on 10 January 2022).
- Rural Health Information Hub. Provides Wide Range of Data on Health Disparities, Health Workforce, Demographics, and More. Explore How Metropolitan and Nonmetro Counties Compare, Nationwide and by State. Available online: https://www.ruralhealthinfo.org/data-explorer (accessed on 11 January 2022).
- Naranjo, M.; Willes, L.; Prillaman, B.A.; Quan, S.F.; Sharma, S. Undiagnosed OSA May Significantly Affect Outcomes in Adults Admitted for COPD in an Inner-City Hospital. Chest 2020, 158, 1198–1207. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Mather, P.J.; Efird, J.T.; Kahn, D.; Shiue, K.Y.; Cheema, M.; Malloy, R.; Quan, S.F. Obstructive Sleep Apnea in Obese Hospitalized Patients: A Single Center Experience. J. Clin. Sleep Med. 2015, 11, 717–723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahar, E.; Whitney, C.W.; Redline, S.; Lee, E.T.; Newman, A.B.; Nieto, F.J.; O’Connor, G.T.; Boland, L.L.; Schwartz, J.E.; Samet, J.M. Sleep-Disordered Breathing and Cardiovascular Disease: Cross-Sectional Results of the Sleep Heart Health Study. Am. J. Respir. Crit. Care Med. 2001, 163, 19–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, S.; Mather, P.; Gupta, A.; Reeves, G.; Rubin, S.; Bonita, R.; Chowdhury, A.; Malloy, R.; Willes, L.; Whellan, D. Effect of Early Intervention with Positive Airway Pressure Therapy for Sleep Disordered Breathing on Six-Month Readmission Rates in Hospitalized Patients with Heart Failure. Am. J. Cardiol. 2016, 117, 940–945. [Google Scholar] [CrossRef] [PubMed]
- Channick, J.E.; Jackson, N.J.; Zeidler, M.R.; Buhr, R.G. Effects of Obstructive Sleep Apnea and Obesity on Thirty-Day Readmissions in Patients with Chronic Obstructive Pulmonary Disease: A Cross-Sectional Mediation Analysis. Ann. Am. Thorac. Soc. 2021, 19, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Peppard, P.E.; Young, T.; Barnet, J.H.; Palta, M.; Hagen, E.W.; Hla, K.M. Increased Prevalence of Sleep-Disordered Breathing in Adults. Am. J. Epidemiol. 2013, 177, 1006–1014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.L.; et al. Estimation of the Global Prevalence and Burden of Obstructive Sleep Apnoea: A Literature-Based Analysis. Lancet Respir Med. 2019, 7, 687–698. [Google Scholar] [CrossRef] [Green Version]
- Epstein, L.J.; Kristo, D.; Strollo, P.J., Jr.; Friedman, N.; Malhotra, A.; Patil, S.P. Clinical Guideline for The Evaluation, Management and Long-Term Care of Obstructive Sleep Apnea in Adults. J. Clin. Sleep Med. 2009, 5, 263–276. [Google Scholar] [CrossRef] [Green Version]
- Stansbury, R.; Abdelfattah, M.; Chan, J.; Mittal, A.; Alqahtani, F.; Sharma, S. Hospital Screening for Obstructive Sleep Apnea in Patients Admitted to A Rural, Tertiary Care Academic Hospital with Heart Failure. Hosp Pract. 2020, 48, 266–271. [Google Scholar] [CrossRef]
- Dunietz, G.L.; Yu, Y.; Levine, R.S.; Conceicao, A.S.; Burke, J.F.; Chervin, R.D.; Braley, T.J. Obstructive Sleep Apnea in Older Adults: Geographic Disparities in PAP Treatment and Adherence. J. Clin. Sleep Med. 2021, 17, 421–427. [Google Scholar] [CrossRef]
- Stansbury, R.; Strollo, P.; Pauly, N.; Sharma, I.; Schaaf, M.; Aaron, A.; Feinberg, J. Under-Recognition of Sleep-Disordered Breathing and Other Common Health Conditions in The West Virginia Medicaid Population: A Driver of Poor Health Outcomes. J. Clin. Sleep Med. 2021, 18, 817–824. [Google Scholar] [CrossRef]
- Health Resources and Services Administration Eligibility Requirements for Federally Qualified Health Centers. Available online: https://www.hrsa.gov/opa/eligibility-and-registration/health-centers/fqhc/index.html (accessed on 28 January 2022).
- United States Census Bureau West Virginia Data Page. Available online: https://www.census.gov/quickfacts/WV (accessed on 15 June 2022).
- Schotland, H.M.; Jeffe, D.B. Development of the Obstructive Sleep Apnea Knowledge and Attitudes (OSAKA) Questionnaire. Sleep Med. 2003, 4, 443–450. [Google Scholar] [CrossRef]
- Chai-Coetzer, C.L.; Antic, N.A.; Rowland, L.S.; Reed, R.L.; Esterman, A.; Catcheside, P.G.; Eckermann, S.; Vowles, N.; Williams, H.; Dunn, S.; et al. Primary Care Vs Specialist Sleep Center Management of Obstructive Sleep Apnea and Daytime Sleepiness and Quality of Life: A Randomized Trial. JAMA 2013, 309, 997–1004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pendharkar, S.R.; Dechant, A.; Bischak, D.P.; Tsai, W.H.; Stevenson, A.M.; Hanly, P.J. An Observational Study of the Effectiveness of Alternative Care Providers in the Management of Obstructive Sleep Apnea. J. Sleep Res. 2016, 25, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Tarraubella, N.; Sánchez-de-la-Torre, M.; Nadal, N.; De Batlle, J.; Benítez, I.; Cortijo, A.; Urgelés, M.C.; Sanchez, V.; Lorente, I.; Lavega, M.M.; et al. Management of Obstructive Sleep Apnoea in A Primary Care Vs Sleep Unit Setting: A Randomised Controlled Trial. Thorax 2018, 73, 1152–1160. [Google Scholar] [CrossRef] [PubMed]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef]
- Grote, L.; McNicholas, W.T.; Hedner, J. ESADA Collaborators. Sleep Apnoea Management in Europe During The COVID-19 Pandemic: Data from The European Sleep Apnoea Database (ESADA). Eur. Respir. J. 2020, 55, 2001323. [Google Scholar] [CrossRef]
- Spagnuolo, C.M.; McIsaac, M.; Dosman, J.; Karunanayake, C.; Pahwa, P.; Pickett, W. Distance to Specialist Medical Care and Diagnosis of Obstructive Sleep Apnea in Rural Saskatchewan. Can. Respir. J. 2019, 2019, 1683124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allen, A.J.; Amram, O.; Tavakoli, H.; Almeida, F.R.; Hamoda, M.; Ayas, N.T. Relationship Between Travel Time from Home to A Regional Sleep Apnea Clinic in British Columbia, Canada, And the Severity of Obstructive Sleep. Ann. Am. Thorac. Soc. 2016, 13, 719–723. [Google Scholar] [CrossRef]
- Billings, M.E. Regional Differences in PAP Care: More Questions Than Answers. J. Clin. Sleep Med. 2021, 17, 363–364. [Google Scholar] [CrossRef]
- Bruyneel, M. Telemedicine in the Diagnosis and Treatment of Sleep Apnoea. Eur. Respir. Rev. 2019, 28, 151. [Google Scholar] [CrossRef] [Green Version]
- Singh, J.; Badr, M.S.; Diebert, W.; Epstein, L.; Hwang, D.; Karres, V.; Khosla, S.; Mims, K.N.; Shamim-Uzzaman, A.; Kirsch, D.; et al. American Academy of Sleep Medicine (AASM) Position Paper for the Use of Telemedicine for the Diagnosis and Treatment of Sleep Disorders. J. Clin. Sleep Med. 2015, 11, 1187–1198. [Google Scholar] [CrossRef] [PubMed]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for Healthcare: Capabilities, Features, Barriers, and Applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef] [PubMed]
- Billings, M.E.; Cohen, R.T.; Baldwin, C.M.; Johnson, D.A.; Palen, B.N.; Parthasarathy, S.; Patel, S.R.; Russell, M.; Tapia, I.E.; Williamson, A.A.; et al. Disparities in Sleep Health and Potential Intervention Models: A Focused Review. Chest 2021, 159, 1232–1240. [Google Scholar] [CrossRef] [PubMed]
- Phillips, B. Improving Access to Diagnosis and Treatment of Sleep-Disordered Breathing. Chest 2007, 132, 1418–1420. [Google Scholar] [CrossRef]
- Shamim-Uzzaman, Q.A.; Bae, C.J.; Ehsan, Z.; Setty, A.R.; Devine, M.; Dhankikar, S.; Donskoy, I.; Fields, B.; Hearn, H.; Hwang, D.; et al. The Use of Telemedicine for the Diagnosis and Treatment of Sleep Disorders: An American Academy of Sleep Medicine Update. J. Clin. Sleep Med. 2021, 17, 1103–1107. [Google Scholar] [CrossRef]
- Afifi, R.A.; Parker, E.A.; Dino, G.; Hall, D.M.; Ulin, B. Reimagining Rural: Shifting Paradigms About Health and Well-Being in the Rural United States. Annu. Rev. Public Health 2022, 43, 135–154. [Google Scholar] [CrossRef] [PubMed]
- Chhatre, S.; Chang, Y.H.A.; Gooneratne, N.S.; Kuna, S.; Strollo, P.; Jayadevappa, R. Association Between Adherence to Continuous Positive Airway Pressure Treatment and Cost Among Medicare Enrollees. Sleep 2020, 43, zsz188. [Google Scholar] [CrossRef]
- Benjafield, A.V.; Oldstone, L.M.; Willes, L.A.; Kelly, C.; Nunez, C.M.; Malhotra, A.; On Behalf of the medXcloud Group. Positive Airway Pressure Therapy Adherence with Mask Resupply: A Propensity-Matched Analysis. J. Clin. Med. 2021, 10, 72. [Google Scholar] [CrossRef]
- Weaver, T.E.; Grunstein, R.R. Adherence to Continuous Positive Airway Pressure Therapy: The Challenge to Effective treatment. Proc. Am. Thorac. Soc. 2008, 5, 173–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
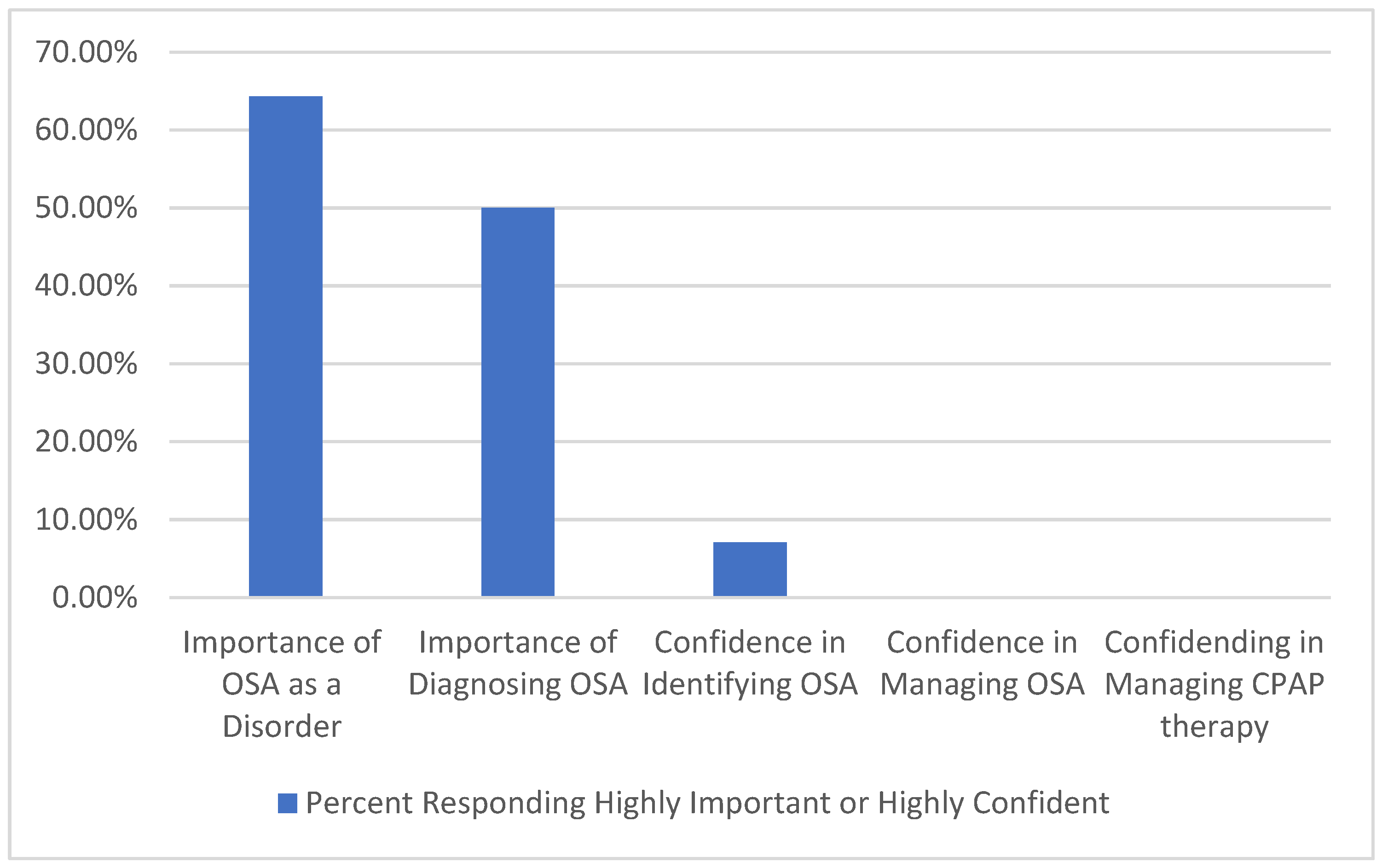
| Provider Knowledge and Beliefs of Sleep Apnea |
|
| Provider Percieved Barriers to Osa Management in Rural Commmunities |
|
| AGE Mean (SD) | |
| Mean | 53.0 years (12.5) [Range 31 years–75 years] |
| Gender, N (Percent) | |
| Male | 3 (21.4%) |
| Female | 11 (78.6%) |
| Race, N (Percent) | |
| Caucasian | 14 (100%) |
| Practice Type, N (Percent) | |
| Advanced Practice Provider | 8 (57.1%) |
| Physician | 6 (42.9%) |
| Practice Tenure, Mean (SD) [Range] | |
| Total Years in Practice | 16.2 (15.0) [less than one month to 43 years] |
| Total Years in Practice at FQHC | 8.7 (13.5) [less than one month to 43 years] |
| Degree N (Percent) | |
| MD | 5 (35.7%) |
| DO | 1 (7.1%) |
| NP | 6 (42.8%) |
| PA | 2 (14.3%) |
| Item Number | Number and Percent Answer Correctly | Item Number | Number and Percent Answer Correctly |
|---|---|---|---|
| Item 1 | 14 (100%) | Item 10 | 13 (92.69%) |
| Item 2 | 10 (71.4%) | Item 11 | 14 (100%) |
| Item 3 | 4 (28.6%) | Item 12 | 14 (100%) |
| Item 4 | 8 (57.1%) | Item 13 | 11 (78.6%) |
| Item 5 | 12 (85.7%) | Item 14 | 14 (100%) |
| Item 6 | 13 (92.6%) | Item 15 | 11 (78.6%) |
| Item 7 | 12 (85.7%) | Item 16 | 12 (85.7%) |
| Item 8 | 4 (28.6%) | Item 17 | 9 (64.3%) |
| Item 9 | 12 (85.6%) | Item 18 | 14 (100%) |
| Theme | Subtheme | Representative Quotes |
|---|---|---|
| Barriers to OSA Care Delivery (N = 94) | OSA Care Access | “And lack of transportation.” |
| Provider Knowledge/Beliefs OSA | “I, uh, learned a little bit more about sleep apnea in the past several years from continuing education class. But I think there’s a lot I don’t know.” | |
| Cost of OSA Care | “I noticed even before I started doing those physicals that some insurers prefer to just do the overnight sleep study without, uh, referral to a specialist, and so then I was left holding the results and was not real happy about that. So, so to me, the barrier, the biggest barrier is cost and coverage.” | |
| Facilitators to OSA care Delivery (N = 33) | Specialty Referral Access | They [specialist and DME] pretty much take care of all that stuff. As long as they do all that, then I’m pretty comfortable with that.” |
| Patient Characteristics | “I’ve never had any patient that closed the door on that discussion [regarding OSA] with me in my practice.” | |
| Community Based Care needs to improve OSA management in targeted rural areas (N = 19) | Community Programming | “A lot of them [patients] are these big burly gentlemen that are very manly, and they don’t want to say that, ‘Yeah. Well, maybe something’s not right. I’m not tired’. But yet they can’t lift five pounds, because they are so tired. So, you have this, no disrespect, but this ‘man mentality’ to some of these guys.” |
| Provider Preferences | “I mean, it’s my responsibility, but since you’re conducting this study, I would be interested in more education on it [OSA and CPAP]”. | |
| Educational Needs | “I probably would consider learning how to manage it [OSA] more myself and prescribe CPAP.” |
| Data Source | OSA Prevalence |
|---|---|
| Expected WV Adult Medicaid OSA Prevalence from National Data Sources [15] | 25% |
| Observed WV Adult Medicaid OSA Prevalence from State Database Analysis [15] | 8.8% |
| FQHC Specific OSA Prevalence from Local EMR Database Analysis | 2.3% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stansbury, R.; Rudisill, T.; Salyer, R.; Kirk, B.; De Fazio, C.; Baus, A.; Aryal, S.; Strollo, P.J.; Sharma, S.; Feinberg, J. Provider Perspectives on Sleep Apnea from Appalachia: A Mixed Methods Study. J. Clin. Med. 2022, 11, 4449. https://doi.org/10.3390/jcm11154449
Stansbury R, Rudisill T, Salyer R, Kirk B, De Fazio C, Baus A, Aryal S, Strollo PJ, Sharma S, Feinberg J. Provider Perspectives on Sleep Apnea from Appalachia: A Mixed Methods Study. Journal of Clinical Medicine. 2022; 11(15):4449. https://doi.org/10.3390/jcm11154449
Chicago/Turabian StyleStansbury, Robert, Toni Rudisill, Rachel Salyer, Brenna Kirk, Caterina De Fazio, Adam Baus, Shubekchha Aryal, Patrick J. Strollo, Sunil Sharma, and Judith Feinberg. 2022. "Provider Perspectives on Sleep Apnea from Appalachia: A Mixed Methods Study" Journal of Clinical Medicine 11, no. 15: 4449. https://doi.org/10.3390/jcm11154449
APA StyleStansbury, R., Rudisill, T., Salyer, R., Kirk, B., De Fazio, C., Baus, A., Aryal, S., Strollo, P. J., Sharma, S., & Feinberg, J. (2022). Provider Perspectives on Sleep Apnea from Appalachia: A Mixed Methods Study. Journal of Clinical Medicine, 11(15), 4449. https://doi.org/10.3390/jcm11154449








