Blood Culture-Negative Infective Endocarditis by Mycoplasma hominis: Case Report and Literature Review
Abstract
:1. Introduction
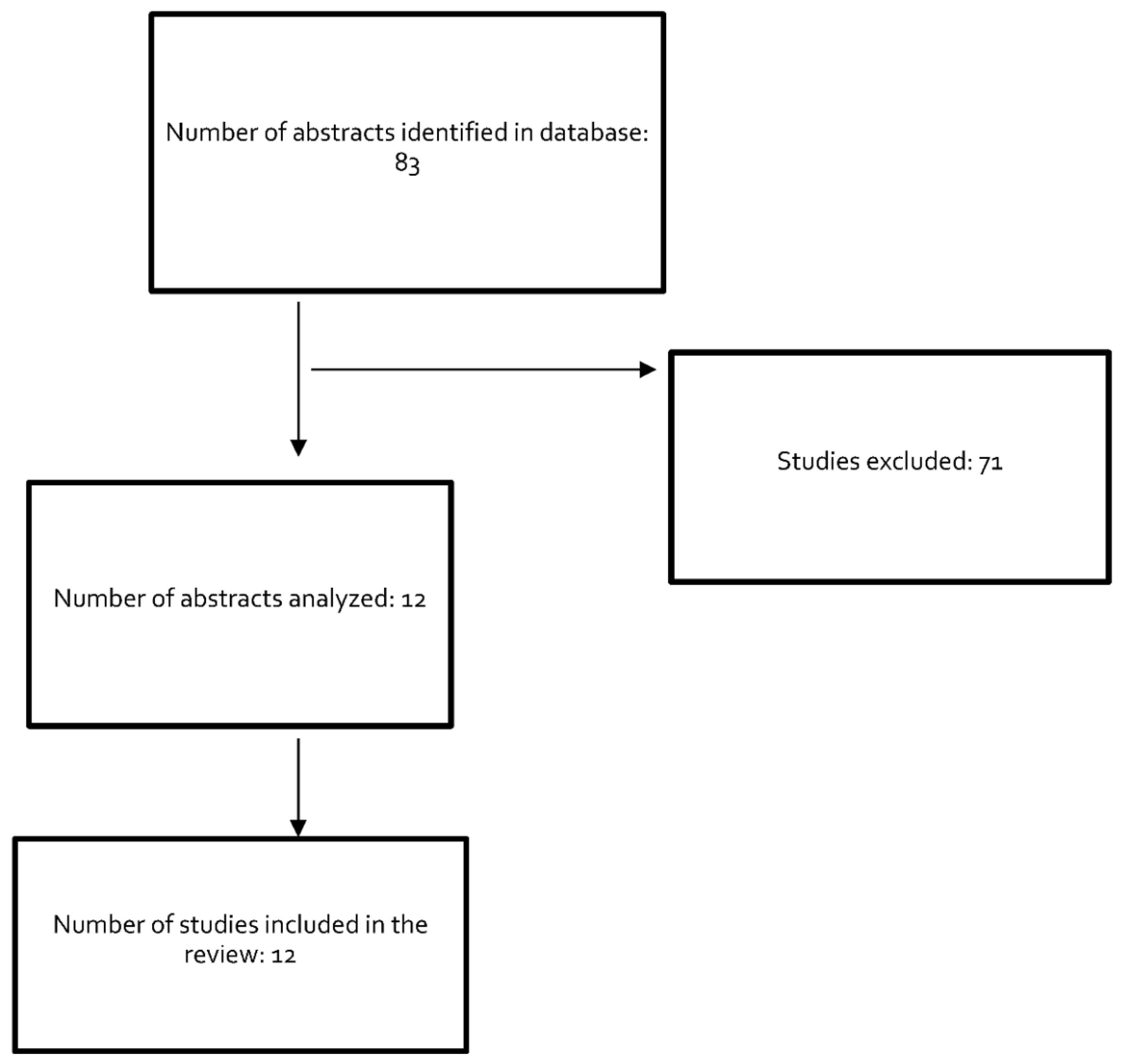
2. Materials and Methods
3. Case Report
4. Discussion
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Ahmed, J.; Rawre, J.; Dhawan, N.; Khanna, N.; Dhawan, B. Mycoplasma hominis: An under recognized pathogen. Indian J. Med. Microbiol. 2021, 39, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Gonzalo de Liria, C.R.; Méndez Hernández, M. Infecciones causadas por Mycoplasma pneumoniae. An. Pediatr. Contin. 2013, 11, 23–29. [Google Scholar] [CrossRef]
- Gómez Rufo, D.; García Sánchez, E.; García Sánchez, J.E.; García Moro, M. Implicaciones clínicas de las especies del género Mycoplasma [Clinical implications of the genus Mycoplasma]. Rev. Esp. Quimioter. 2021, 34, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Farhadifar, F.; Khodabandehloo, M.; Ramazanzadeh, R.; Rouhi, S.; Ahmadi, A.; Ghaderi, E. Survey on association between Mycoplasma hominis endocervical infection and spontaneous abortion using Polymerase Chain Reaction. Int. J. Reprod. Biomed. 2016, 14, 181–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor-Robinson, D. Mollicutes in vaginal microbiology: Mycoplasma hominis, Ureaplasma urealyticum, Ureaplasma parvum and Mycoplasma genitalium. Res. Microbiol. 2017, 168, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Xiang, L.; Lu, B. Infection due to Mycoplasma hominis after left hip replacement: Case report and literature review. BMC Infect. Dis. 2019, 19, 50. [Google Scholar] [CrossRef] [PubMed]
- Hata, A.; Honda, Y.; Asada, K.; Sasaki, Y.; Kenri, T.; Hata, D. Mycoplasma hominis meningitis in a neonate: Case report and review. J. Infect. 2008, 57, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Sáez, A.; Monteagudo, I.; Miñambres, E.; Ots, E.; Rodríguez-Borregán, J.C.; García, C. Pneumonia due to Mycoplasma hominis in a healthy adult. Scand. J. Infect. Dis. 2003, 35, 282–284. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, H.; Shimizu, H.; Katayama, K.; Tadera, K.; Nomura, T.; Omori, K.; Shigemoto, N.; Takasaki, T.; Ohge, H.; Takahashi, S. Postoperative mediastinitis after cardiac surgery caused by Mycoplasma hominis: A case report. Surg. Case Rep. 2021, 7, 248. [Google Scholar] [CrossRef] [PubMed]
- Küchle, C.; Abele-Horn, M.; Menninger, M.; Held, E.; Heesemann, J. Mycoplasma hominis. A rare causative agent of acute pyelonephritis. Dtsch. Med. Wochenschr. 1997, 122, 542–544. [Google Scholar] [CrossRef]
- Cohen, J.I.; Sloss, L.J.; Kundsin, R.; Golightly, L. Prosthetic valve endocarditis caused by Mycoplasma hominis. Am. J. Med. 1989, 86, 819–821. [Google Scholar] [CrossRef]
- Krausse, R.; Schubert, S. In-vitro activities of tetracyclines, macrolides, fluoroquinolones and clindamycin against Mycoplasma hominis and Ureaplasma ssp. isolated in Germany over 20 years. Clin. Microbiol. Infect. 2010, 16, 1649–1655. [Google Scholar] [CrossRef] [PubMed]
- DiSesa, V.J.; Sloss, L.J.; Cohn, L.H. Heart transplantation for intractable prosthetic valve endocarditis. J. Heart Transplant. 1990, 9, 142–143. [Google Scholar] [PubMed]
- Blasco, M.; Torres, L.; Marco, M.L.; Moles, B.; Villuendas, M.C.; García Moya, J.B. Prosthetic valve endocarditis caused by Mycoplasma hominis. Eur. J. Clin. Microbiol. Infect. Dis. 2000, 19, 638–640. [Google Scholar] [CrossRef]
- Fenollar, F.; Gauduchon, V.; Casalta, J.P.; Lepidi, H.; Vandenesch, F.; Raoult, D. Mycoplasma endocarditis: Two case reports and a review. Clin. Infect. Dis. 2004, 38, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, S.R.; Littlehorn, C.; Nyquist, A.C. Mycoplasma hominis endocarditis in a child with a complex congenital heart defect. Pediatr. Infect. Dis. J. 2006, 25, 851–852. [Google Scholar] [CrossRef]
- Hidalgo-Tenorio, C.; Pasquau, J.; López-Checa, S.; López-Ruz, M.A. Endocarditis por Mycoplasma hominis [Endocarditis due to Mycoplasma hominis]. Enferm. Infecc. Microbiol. Clin. 2006, 24, 470–471. [Google Scholar] [CrossRef]
- Jamil, H.A.; Sandoe, J.A.T.; Gascoyne-Binzi, D.; Chalker, V.J.; Simms, A.D.; Munsch, C.M.; Baig, M.W. Late-onset prosthetic valve endocarditis caused by Mycoplasma hominis, diagnosed using broad-range bacterial PCR. J. Med. Microbiol. 2012, 61, 300–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hussain, S.T.; Gordon, S.M.; Tan, C.D.; Smedira, N.G. Mycoplasma hominis prosthetic valve endocarditis: The value of molecular sequencing in cardiac surgery. J. Thorac. Cardiovasc. Surg. 2013, 146, 7–9. [Google Scholar] [CrossRef] [Green Version]
- Gagneux-Brunon, A.; Grattard, F.; Morel, J.; Suy, F.; Fuzellier, J.-F.; Verhoeven, P.; Cazorla, C.; Guglielminotti, C.; Fresard, A.; Lucht, F.; et al. Mycoplasma hominis, a Rare but True Cause of Infective Endocarditis. J. Clin. Microbiol. 2015, 53, 3068–3071. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romeu Prieto, J.M.; Lizcano Lizcano, A.M.; López de Toro Martín Consuegra, I.; Largo Pau, J.; López Almodóvar, L.F.; García Camacho, E. Culture-negative Endocarditis: Mycoplasma hominis Infection. Rev. Esp. Cardiol. (Engl. Ed.) 2015, 68, 1037–1038. [Google Scholar] [CrossRef] [PubMed]
- Kotaskova, I.; Nemec, P.; Vanerkova, M.; Malisova, B.; Tejkalova, R.; Orban, M. First report of Sneathia sanguinegens together with Mycoplasma hominis in postpartum prosthetic valve infective endocarditis: A case report. BMC Infect. Dis. 2017, 17, 563. [Google Scholar] [CrossRef] [PubMed]
- Givone, F.; Peghin, M.; Vendramin, I.; Carletti, S.; Tursi, V.; Pasciuta, R.; Livi, U.; Bassetti, M. Salvage heart transplantation for Mycoplasma hominis prosthetic valve endocarditis: A case report and review of the literature. Transpl. Infect. Dis. 2020, 22, e13249. [Google Scholar] [CrossRef] [PubMed]
- Brouqui, P.; Raoult, D. Endocarditis due to rare and fastidious bacteria. Clin. Microbiol. Rev. 2001, 14, 177–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fournier, P.E.; Thuny, F.; Richet, H.; Lepidi, H.; Casalta, J.P.; Arzouni, J.P.; Maurin, M.; Celard, M.; Mainardi, J.L.; Caus, T.; et al. Comprehensive diagnostic strategy for blood culture-negative endocarditis: A prospective study of 819 new cases. Clin. Infect. Dis. 2010, 51, 131–140. [Google Scholar] [CrossRef] [Green Version]
- Hurrell, H.; Roberts-Thomson, R.; Prendergast, B.D. Non-infective endocarditis. Heart 2020, 106, 1023–1029. [Google Scholar] [CrossRef]
- Marín, M.; Muñoz, P.; Sánchez, M.; Del Rosal, M.; Alcalá, L.; Rodríguez-Créixems, M.; Bouza, E.; on behalf of the Group for the Management of Infective Endocarditis of the Gregorio Marañón Hospital. Molecular diagnosis of infective endocarditis by real- time broad-range polymerase chain reaction (PCR) and sequencing directly from heart valve tissue. Medicine 2007, 86, 195–202. [Google Scholar] [CrossRef]
| Variable | Reference Range in Our Hospital | At Hospital Admission | At Intensive Care Unit Admission | 12 Days after Initiation of Antibiotherapy |
|---|---|---|---|---|
| Hemoglobin (g/dL) | 12.5–17.2 | 11.2 | 10.5 | 10.6 |
| Hematocrit (%) | 37–49 | 35.6 | 29.2 | 32.8 |
| Leukocyte count (μL) | 3600–10,500 | 13,060 | 19,000 | 5840 |
| Absolute neutrophil count (μL) | 1500–7700 | 11,580 | 17,000 | 3030 |
| Absolute lymphocyte count (μL) | 1–1400 | 610 | 1330 | 1770 |
| Absolute monocyte count (μL) | 100–900 | 680 | 510 | 680 |
| Platelet count (μL) | 130,000–370,000 | 326,000 | 265,000 | 364,000 |
| Prothrombin time (%) | 75–130 | 73.1 | 49 | 69 |
| Fibrinogen (mg/dL) | 170–450 | 900 | 773.5 | 335 |
| D-Dimer (mg/L) | 0–0.5 | 3.19 | ||
| Glucose (mg/dL) | 75–115 | 183 | 149 | 87 |
| Urea (mg/dL) | 18–37.7 | 92 | 129 | 42 |
| Creatinine (mg/dL) | 0.67–1.17 | 2.03 | 3.74 | 1.22 |
| Total bilirubin (mg/dL) | 0.3–1.2 | 1.23 | 1.67 | 0.8 |
| Aspartate transaminase (U/L) | 10–50 | 67 | 5425 | 22 |
| Alanine transaminase (U/L) | 1–50 | 95 | 4950 | 62 |
| Gamma-glutamyl transferase (U/L) | 1–55 | 462 | 336 | 33 |
| Alkaline phosphatase (U/L) | 30–120 | 219 | 197 | 84 |
| Lactate dehydrogenase (U/L) | 10–248 | 362 | 5515 | 253 |
| Sodium (mEq/L) | 136–145 | 137 | 141 | 143 |
| Potassium (mEq/L) | 3.50–5.10 | 4.90 | 4.60 | 4.30 |
| Ferritin (ng/mL) | 20–250 | 504.5 | 31 | |
| NT-proBNP (pg/mL) | 10–300 | 1430 | 5450 | 328 |
| C-reactive protein (mg/L) | 0.1–5 | 142.9 | 320 | 2.2 |
| Procalcitonin (ng/mL) | 0.02–0.5 | 9.57 | >100 | |
| High-sensitivity troponin I (pg/mL) | 2.3–19.8 | 18.8 | 88.8 |
| Cases | Reference | Age (Years)- Sex | History of Cardiac Surgery | Time Elapsed from Surgery to Diagnosis | Species Isolated (Method) | Positive Sample | Valve Involvement | Empirical Treatment | Targeted Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Cohen et al. [11] DiSesa et al. [13] | 25-F | Aortic and mitral valve replacement | 3 months | Mycoplasma hominis (culture) | Mitral annulus sample | Mitral and aortic | Vancomycin, gentamycin, and ampicillin | Clindamycin and rifampicin iv. (6 w) Oral doxycycline (4 w) | Rescue with orthotopic heart transplantation. Survives |
| 2 | Blasco et al. [14] | 46-M | Mitral valve replacement | 15 days | Mycoplasma hominis (culture) | Prosthetic valve sample | Dehiscence of the mitral prosthesis | Vancomycin and amikacin | Not reported | Death |
| 3 | Fenollar et al. [15] | 33-M | Mitral valve annuloplasty | 6 months | Mycoplasma hominis (16S rDNA PCR) | Cardiac valve specimen | Dehiscence of mitral plasty | Amoxicillin and gentamycin | Doxycycline (4 w) | Survives |
| 4 | Domínguez et al. [16] | 4-F | Biventricular repair | 22 days | Mycoplasma hominis (culture and 16S rDNA PCR) | Pleural fluid, blood sample, and myocardium sample | Right atrial vegetation and perivalvular abscess | Vancomycin, meropenem, levofloxacin, gentamycin, and fluconazole | Clindamycin and levofloxacin | Death |
| 5 | Hidalgo-Tenorio et al. [17] | 48-M | Aortic valve replacement | 2 months | Mycoplasma hominis (culture) | Valve sample | Dehiscence of aortic plasty and acute regurgitation | Vancomycin, gentamycin, and cefepime | Doxycycline and levofloxacin (8 w) | Survives |
| 6 | Jamil et al. [18] | 40-M | Aortic and mitral valve replacement | 9 years | Mycoplasma hominis (16S rDNA PCR and culture) | Valve sample | Partial mitral prosthesis dehiscence with severe paraprosthetic regurgitation | Vancomycin, ciprofloxacin, and rifampicin | Doxycycline and clindamycin (8 w) | Survives |
| 7 | Hussain et al. [19] | 57-M | Aortic valve replacement and mitral valve decalcification | 1 year | Mycoplasma hominis (16S rDNA PCR) | Valve sample | Aortic regurgitation | Vancomycin and ceftriaxone | Doxycycline iv and oral moxifloxacin (duration ND) | Survives |
| 8 | Gagneux-Brunon et al. [20] | 74-M | Aortic and mitral valve replacement | 6 months | Mycoplasma hominis (16S rDNA PCR and culture) | Cardiac valve sample | Dehiscence of aortic prosthesis | Vancomycin, Linezolid, and Daptomycin (after suspending linezolid). | Moxifloxacin (2 days). Clindamycin and doxycycline (9 w) | Survives |
| 9 | Romeu Prieto et al. [21] | 54-M | Aortic valve replacement | 7 months | Mycoplasma hominis (16S rDNA PCR) | Valve sample | Massive aortic regurgitation | Daptomycin, ceftriaxone, and gentamicin. | Doxycycline and levofloxacin (8 w) | Survives |
| 10 | Kotaskova et al. [22] | ND-F | Tricuspid valve replacement | 1 year | Mycoplasma hominis (16S rDNA PCR) and Sneatha sanguinegens | Valve sample | Massive tricuspid regurgitation | Amoxicillin/clavulanic acid, ampicillin and gentamicin | Not reported | Loss to follow up. Death |
| 11 | Givone et al. [23] | 28-M | Aortic valve and root replacement | 13 months | Mycoplasma hominis (16S rDNA PCR) | Aortic tissue specimen | Para-aortic pseudoaneurysm and severe aortic insufficiency | Daptomycin, ampicillin, and anidulafungin | Moxifloxacin (8 w) | Survives. Heart transplant |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bustos-Merlo, A.; Rosales-Castillo, A.; Cobo, F.; Hidalgo-Tenorio, C. Blood Culture-Negative Infective Endocarditis by Mycoplasma hominis: Case Report and Literature Review. J. Clin. Med. 2022, 11, 3841. https://doi.org/10.3390/jcm11133841
Bustos-Merlo A, Rosales-Castillo A, Cobo F, Hidalgo-Tenorio C. Blood Culture-Negative Infective Endocarditis by Mycoplasma hominis: Case Report and Literature Review. Journal of Clinical Medicine. 2022; 11(13):3841. https://doi.org/10.3390/jcm11133841
Chicago/Turabian StyleBustos-Merlo, Antonio, Antonio Rosales-Castillo, Fernando Cobo, and Carmen Hidalgo-Tenorio. 2022. "Blood Culture-Negative Infective Endocarditis by Mycoplasma hominis: Case Report and Literature Review" Journal of Clinical Medicine 11, no. 13: 3841. https://doi.org/10.3390/jcm11133841
APA StyleBustos-Merlo, A., Rosales-Castillo, A., Cobo, F., & Hidalgo-Tenorio, C. (2022). Blood Culture-Negative Infective Endocarditis by Mycoplasma hominis: Case Report and Literature Review. Journal of Clinical Medicine, 11(13), 3841. https://doi.org/10.3390/jcm11133841







