Effects of HIV Infection in Plasma Free Fatty Acid Profiles among People with Non-Alcoholic Fatty Liver Disease
Abstract
:1. Introduction
2. Materials and Methods
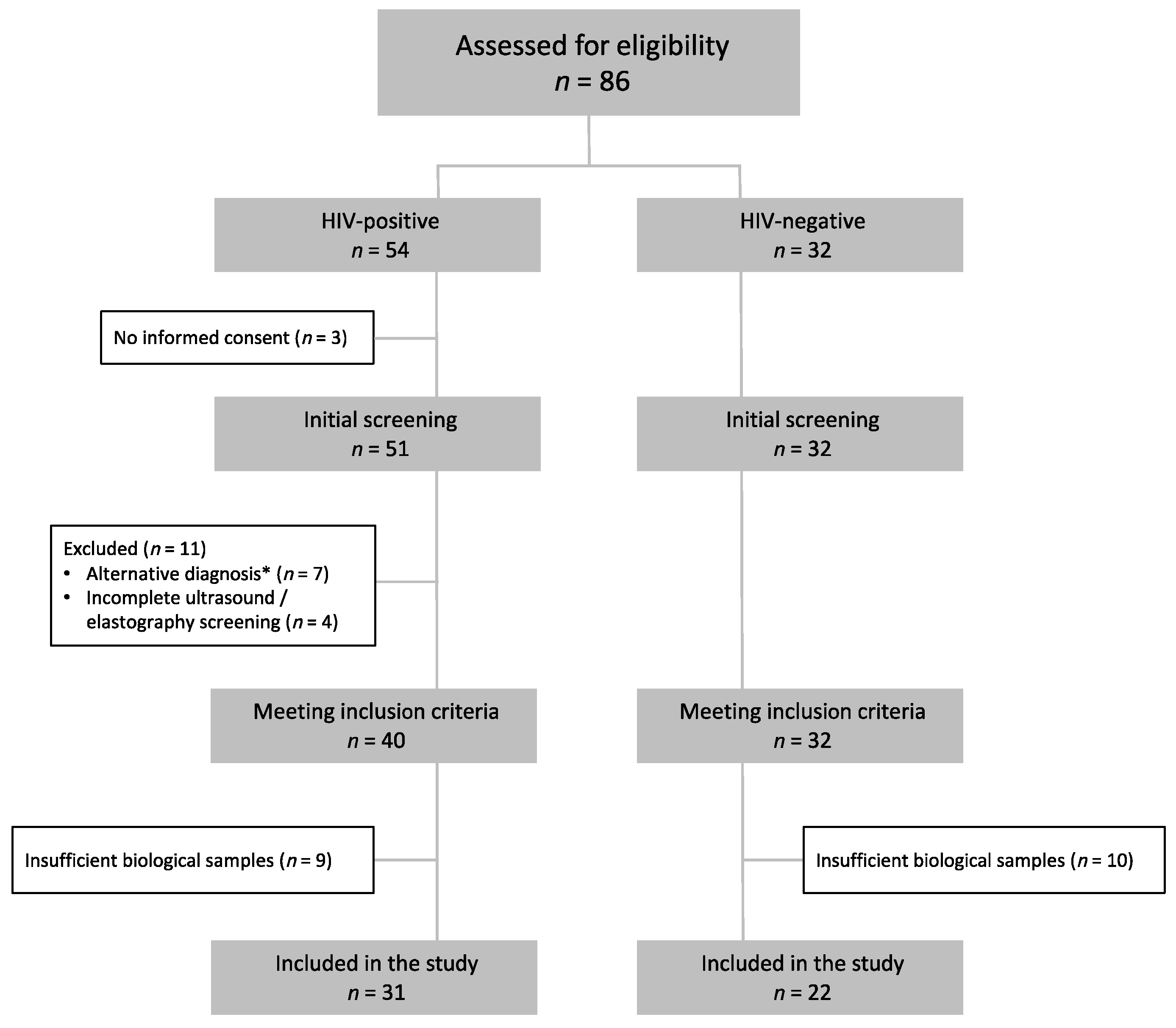
2.1. Study Design and Population
2.2. Determination of Fatty Acid Methyl Esters in Plasma and Serum
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zelber-Sagi, S.; Wong, V.W.-S.; Dufour, J.-F.; Schattenberg, J.M.; et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020, 73, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Cervo, A.; Milic, J.; Mazzola, G.; Schepis, F.; Petta, S.; Krahn, T.; Lebouche, B.; Deschenes, M.; Cascio, A.; Guaraldi, G.; et al. Prevalence, Predictors, and Severity of Lean Nonalcoholic Fatty Liver Disease in Patients Living with Human Immunodeficiency Virus. Clin. Infect. Dis. 2020, 71, E694–E701. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, A.; Price, J.C. HIV-Associated NAFLD: Disease Burden and Management. Curr. Hepatol. Rep. 2019, 18, 482–491. [Google Scholar] [CrossRef]
- Juárez-Hernández, E.; Chávez-Tapia, N.C.; Uribe, M.; Barbero-Becerra, V.J. Role of bioactive fatty acids in nonalcoholic fatty liver disease. Nutr. J. 2016, 15, 72. [Google Scholar] [CrossRef] [Green Version]
- Ferramosca, A.; Zara, V. Modulation of hepatic steatosis by dietary fatty acids. World J. Gastroenterol. 2014, 20, 1746. [Google Scholar] [CrossRef]
- Fritsche, K.L. The science of fatty acids and inflammation. Adv. Nutr. 2015, 6, 293S–301S. [Google Scholar] [CrossRef]
- Bowman, E.R.; Kulkarni, M.; Gabriel, J.; Cichon, M.J.; Riedl, K.; Belury, M.A.; Lake, J.E.; Richardson, B.; Cameron, C.; Cameron, M.; et al. Altered Lipidome Composition Is Related to Markers of Monocyte and Immune Activation in Antiretroviral Therapy Treated Human Immunodeficiency Virus (HIV) Infection and in Uninfected Persons. Front. Immunol. 2019, 10, 785. [Google Scholar] [CrossRef] [Green Version]
- Funderburg, N.T.; Mehta, N.N. Lipid Abnormalities and Inflammation in HIV Inflection. Curr. HIV/AIDS Rep. 2016, 13, 218–225. [Google Scholar] [CrossRef] [Green Version]
- Dirajlal-Fargo, S.; Sattar, A.; Yu, J.; Albar, Z.; Chaves, F.C.; Riedl, K.; Kityo, C.; Bowman, E.; Mccomsey, G.A.; Funderburg, N. Lipidome association with vascular disease and inflammation in HIV+ Ugandan children. AIDS 2021, 35, 15–23. [Google Scholar] [CrossRef]
- Stonehouse, W.; Kruger, A.; Smuts, C.M.; Du Loots, T.; Wentzel-Viljoen, E.; Vorster, H.H. Plasma polyunsaturated fatty acids and liver enzymes in HIV-infected subjects: The Prospective Urban and Rural Epidemiology (PURE) Study. Am. J. Clin. Nutr. 2010, 91, 729–735. [Google Scholar] [CrossRef] [Green Version]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef] [PubMed]
- Castro-Gómez, P.; Fontecha, J.; Rodríguez-Alcalá, L.M. A high-performance direct transmethylation method for total fatty acids assessment in biological and foodstuff samples. Talanta 2014, 128, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Assies, J.; Pouwer, F.; Lok, A.; Mocking, R.; Bockting, C.L.; Visser, I.; Abeling, N.G.G.M.; Duran, M.; Schene, A.H. Plasma and erythrocyte fatty acid patterns in patients with recurrent depression: A matched case-control study. PLoS ONE 2010, 5, e10635. [Google Scholar] [CrossRef] [PubMed]
- Althouse, A.D. Adjust for Multiple Comparisons? It’s Not That Simple. Ann. Thorac. Surg. 2016, 101, 1644–1645. [Google Scholar] [CrossRef] [Green Version]
- Feng, R.; Luo, C.; Li, C.; Du, S.; Okekunle, A.P.; Li, Y. Free fatty acids profile among lean, overweight and obese non-alcoholic fatty liver disease patients: A case—Control study. Lipids Health Dis. 2017, 16, 165. [Google Scholar] [CrossRef] [Green Version]
- Tavares De Almeida, I.; Cortez-Pinto, H.; Fidalgo, G.; Rodrigues, D.; Camilo, M.E. Plasma total and free fatty acids composition in human non-alcoholic steatohepatitis. Clin. Nutr. 2002, 21, 219–223. [Google Scholar] [CrossRef]
- Benedicto, A.M.; Fuster-Martínez, I.; Tosca, J.; Esplugues, J.V.; Blas-García, A.; Apostolova, N. NNRTI and Liver Damage: Evidence of Their Association and the Mechanisms Involved. Cells 2021, 10, 1687. [Google Scholar] [CrossRef]
- Martí-Rodrigo, A.; Alegre, F.; Moragrega, Á.B.; Garcia-Garcia, F.; Martí-Rodrigo, P.; Fernández-Iglesias, A.; Gracia-Sancho, J.; Apostolova, N.; Esplugues, J.V.; Blas-García, A. Rilpivirine Attenuates Liver Fibrosis through Selective STAT1-Mediated Apoptosis in Hepatic Stellate Cells. Gut 2020, 69, 920–932. [Google Scholar] [CrossRef]
- Ohno, Y.; Suto, S.; Yamanaka, M.; Mizutani, Y.; Mitsutake, S.; Igarashi, Y. ELOVL1 production of C24 acyl-CoAs is linked to C24 sphingolipid synthesis. Proc. Natl. Acad. Sci. USA 2010, 107, 18439–18444. [Google Scholar] [CrossRef] [Green Version]
- Matsuzaka, T.; Atsumi, A.; Matsumori, R.; Nie, T.; Shinozaki, H.; Suzuki-Kemuriyama, N.; Kuba, M.; Nakagawa, Y.; Ishii, K.; Shimada, M.; et al. Elovl6 promotes nonalcoholic steatohepatitis. Hepatology 2012, 56, 2199–2208. [Google Scholar] [CrossRef]
- Chen, L.; Wu, N.; Kennedy, L.; Francis, H.; Ceci, L.; Zhou, T.; Samala, N.; Kyritsi, K.; Wu, C.; Sybenga, A.; et al. Inhibition of Secretin/Secretin Receptor Axis Ameliorates NAFLD Phenotypes. Hepatology 2021, 74, 1845–1863. [Google Scholar] [CrossRef] [PubMed]
- Shimano, H. Novel qualitative aspects of tissue fatty acids related to metabolic regulation: Lessons from Elovl6 knockout. Prog. Lipid Res. 2012, 51, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.K.; Shon, J.C.; Seo, H.S.; Liu, K.; Lee, J.W.; Ahn, S.K.; Hong, S.P. Decrease of ceramides with long-chain fatty acids in psoriasis: Possible inhibitory effect of interferon gamma on chain elongation. Exp. Dermatol. 2021, 31, 122–132. [Google Scholar] [CrossRef] [PubMed]


| HIV Positive (n = 31) | HIV Negative (n = 22) | p-Value | |
|---|---|---|---|
| Age, median (IQR) | 56 (46, 61) | 60 (58, 71) | 0.005 |
| Sex, n (%) | |||
| Male | 27 (87) | 9 (40) | 0.001 |
| Female | 4 (13) | 13 (59) | |
| NAFLD severity | |||
| NAFLD-LFS, median (IQR) | −0.05 (−1.13, 3.57) | 1.78 (0.29, 2.62) | 0.293 |
| Controlled attenuation parameter (CAP), median (IQR) | 275 (234, 288) | 313 (273, 357) | 0.053 |
| Body mass index, median (IQR) | 27 (25, 28) | 33 (31, 36) | <0.001 |
| Hypertension, n (%) | 10 (32) | 13 (59) | 0.091 |
| Diabetes mellitus, n (%) | 4 (13) | 10 (45) | 0.006 |
| Metabolic syndrome, n (%) | 6 (19) | 17 (77) | <0.001 |
| Ischemic heart disease, n (%) | 0 (0) | 2 (9) | 0.158 |
| Stroke, n (%) | 0 (0) | 1 (5) | 0.415 |
| Tobacco use, n (%) | 5 (16) | 2 (9) | 0.885 |
| Illicit drug use, n (%) | 2 (6) | 0 (0) | 0.112 |
| Lipid-lowering agents, n (%) | |||
| Statins | 13 (42) | 11 (50) | 0.871 |
| Ezetimibe | 2 (6) | 2 (9) | 0.590 |
| Fibrates | 3 (10) | 1 (5) | 0.633 |
| Diet (food group, servings per week), median (IQR) | |||
| Legumes | 2 (1, 3) | 2 (1, 2) | 0.249 |
| Cereals | 7 (7, 7) | 7 (4, 7) | 0.860 |
| Vegetables | 5 (4, 7) | 6 (4, 8) | 0.386 |
| White fish | 1 (0, 2) | 1 (1, 3) | 0.221 |
| Blue fish | 1 (1, 3) | 1 (1, 2) | 0.986 |
| Red meat (beef) | 2 (1, 3) | 1 (1, 2) | 0.116 |
| Pork | 1 (1, 2) | 2 (1, 2) | 1.000 |
| Poultry | 3 (2, 4) | 3 (2, 5) | 0.811 |
| Dairy products | 13 (7, 14) | 14 (11, 14) | 0.056 |
| Fats (oil, butter) | 7 (7, 7) | 7 (5, 7) | 0.809 |
| Alcohol | 1 (3, 7) | 0 (0, 0) | 0.003 |
| Coffee or tea | 7 (7, 7) | 7 (7, 7) | 0.937 |
| Soft drinks | 2 (0, 3) | 0 (0, 2) | 0.136 |
| Liver enzymes, median (IQR) | |||
| GGT (U/L) | 63 (47, 106) | 60 (37, 125) | 0.787 |
| ALT (U/L) | 35 (30, 49) | 48 (33, 63) | 0.299 |
| AST (U/L) | 28 (24, 39) | 34 (27, 43) | 0.338 |
| Total bilirubin (mg/dL) | 0.7 (0.6. 0.9) | 0.7 (0.5, 0.9) | 0.709 |
| Lipid profile, median (IQR) | |||
| Total cholesterol (mg/dL) | 202 (178, 215) | 194 (156, 223) | 0.658 |
| LDL (mg/dL) | 116 (92, 144) | 104 (79, 147) | 0.714 |
| HDL (mg/dL) | 44 (35, 54) | 47 (41, 48) | 0.510 |
| Triglycerides (mg/dL) | 168 (108, 224) | 118 (84, 148) | 0.059 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Sanz, J.; Calvo, M.V.; Serrano-Villar, S.; Montes, M.L.; Martín-Mateos, R.; Burgos-Santamaría, D.; Díaz-Álvarez, J.; Talavera-Rodríguez, A.; Rosas, M.; Moreno, S.; et al. Effects of HIV Infection in Plasma Free Fatty Acid Profiles among People with Non-Alcoholic Fatty Liver Disease. J. Clin. Med. 2022, 11, 3842. https://doi.org/10.3390/jcm11133842
Martínez-Sanz J, Calvo MV, Serrano-Villar S, Montes ML, Martín-Mateos R, Burgos-Santamaría D, Díaz-Álvarez J, Talavera-Rodríguez A, Rosas M, Moreno S, et al. Effects of HIV Infection in Plasma Free Fatty Acid Profiles among People with Non-Alcoholic Fatty Liver Disease. Journal of Clinical Medicine. 2022; 11(13):3842. https://doi.org/10.3390/jcm11133842
Chicago/Turabian StyleMartínez-Sanz, Javier, María Visitación Calvo, Sergio Serrano-Villar, María Luisa Montes, Rosa Martín-Mateos, Diego Burgos-Santamaría, Jorge Díaz-Álvarez, Alba Talavera-Rodríguez, Marta Rosas, Santiago Moreno, and et al. 2022. "Effects of HIV Infection in Plasma Free Fatty Acid Profiles among People with Non-Alcoholic Fatty Liver Disease" Journal of Clinical Medicine 11, no. 13: 3842. https://doi.org/10.3390/jcm11133842
APA StyleMartínez-Sanz, J., Calvo, M. V., Serrano-Villar, S., Montes, M. L., Martín-Mateos, R., Burgos-Santamaría, D., Díaz-Álvarez, J., Talavera-Rodríguez, A., Rosas, M., Moreno, S., Fontecha, J., & Sánchez-Conde, M. (2022). Effects of HIV Infection in Plasma Free Fatty Acid Profiles among People with Non-Alcoholic Fatty Liver Disease. Journal of Clinical Medicine, 11(13), 3842. https://doi.org/10.3390/jcm11133842








