1. Introduction
Fetal head station (FHS) represents the level of the fetal head in the maternal birth canal evaluated by digital vaginal evaluation. According to the American College of Obstetricians and Gynecologists, the pelvic canal of laboring women is divided into 11 levels, also called stations (from −5 to 5), each of them equivalent in centimeters. At station 0, the lowest part of the fetal presentation is at the level of the maternal ischial spines, and this clinical determination is also called fetal head engagement [
1]. Higher or lower head stations are expressed in centimeters above (negative) or below (positive) the reference plane. The head engagement can also be evaluated by an abdominal examination. When two-fifths of the fetal head is palpable, the lowest part of the fetal presentation has reached the plane of the maternal ischial spines, corresponding to the descent of the biparietal plane of the fetal head to a level below the pelvic inlet [
1,
2].
Digital vaginal examination (DVE) represents the standard evaluation of fetal head station and position in term pregnancy [
3]. Every midwife, resident, or specialist should have proper training and expertise in abdominal and vaginal clinical examination [
4,
5,
6]. Still, the clinical evaluation of fetal head situation appears less accurate than ultrasound determinations [
7,
8,
9] and has low reproducibility [
10,
11]. The presence of caput succedaneum, a significant molding, or a persistent posterior occipital position [
12,
13,
14] can lead to difficult interpretations [
15], but such clinical situations do not occur before the onset of labor. On the other hand, the accuracy of fetal head station assessment before labor is limited because the presenting part is more difficult to palpate through a closed cervix [
1].
It is essential to properly assess FHS to accurately evaluate labor progress. In addition, in nulliparous women at term, before labor onset, a high FHS or non-engagement of the fetal head at term is considered a risk factor for CS [
16,
17,
18,
19]. The ability to predict the chance of a normal vaginal or operative delivery before the onset of labor would be of great usefulness in daily clinical practice to prevent fetomaternal labor complications while avoiding an increased rate of Cesarean sections, and so far the literature has not proven that it is possible to achieve this [
20] However, it is worth continuously trying to predict labor outcome before its onset. Recently, an interesting study by Youssef et al. communicated the impact of dynamic changes of fetal head station on labor outcome [
21].
From these premises, in the present study, we aimed to investigate the situation of the fetal head in the primiparous term and whether the clinical evaluation of FHS has a predictive role in estimating the delivery mode before the onset of labor. Therefore, we designed a longitudinal study with weekly determinations starting from 37 GW with several purposes: first, to determine if the evaluation at early term (37 weeks) is predictive for labor outcome; second, to determine a potential descent trend of the fetal head at term; and third, to evaluate the role of the clinical assessments performed within the week before delivery (WBD).
2. Method
We present the prospectively collected data in the Prenatal Diagnostic Unit of the University Emergency County Hospital of Craiova, regional tertiary maternity. We included consecutive low-risk unselected primiparous women admitted for routine 3rd trimester scan, with a gestation age of more than 37 gestational weeks (GW), based on the first trimester dating scan. We excluded cases with indications for elective Cesarean delivery, and high obstetrical risk, e.g., non-cephalic presentation, multiple pregnancies, preeclampsia, diabetes, fetal growth restriction and macrosomia, teenage and elderly primiparous, and prior Cesarean delivery. We did not exclude the cases with induced labor, regardless of the induction outcome. Each patient was adequately informed regarding the study protocol and had to sign an informed consent form to participate. The protocol included weekly digital vaginal examinations of all enrolled patients until delivery. According to each examination, a clinical fetal head station was noted in the database. The clinical examinations were performed by experienced obstetricians (four senior physicians, with more than 5 years of practice). The experience of the physicians was considered as a valuable tool to ensure the objectivity of FHS examinations. There were no cases which reported examination difficulties. Finally, after we documented all the results in the database, we performed a statistical analysis to investigate the predictive value of clinical fetal head station determination on the delivery mode estimation in primiparous women before the onset of labor. The following parameters were considered: FHS at 37GW, the longitudinal variation of FHS during the weekly evaluations, and the situation of the fetal head in the WBD. The Cesarean delivery cases with other than prolonged or arrested labor indication (fetal distress without prolonged labor, placental abruption, etc.) were also excluded from the final analysis.
The trial was approved by the University of Medicine and Pharmacy of Craiova Committee of Ethics and Academic and Scientific Deontology (No.: 18/26.02.2016).
3. Statistical Analysis
Descriptive statistics were produced for all study variables (maternal age, height, weight, parity, gestational age, mode and type of delivery, and fetal head station). The data were checked for normality and equal variance using the Kolmogorov–Smirnov test together with the Shapiro–Wilk test. All the continuous variables are presented as the mean and SD or median, if appropriate. The categorical data are presented as frequency and percentage. The results between groups (vaginal delivery and Cesarean delivery) were compared using the Student’s t-test or Mann–Whitney test where applicable with a statistical significance level set at p < 0.05. The statistical analysis was performed using IBM SPSS Statistics for Windows, V.22.0. (IBM Corp.).
4. Results
4.1. Group Characteristics
A total of 276 Caucasian primiparous women from five counties assigned to the University Emergency County Hospital of Craiova were included in the final analysis. Sixteen patients were excluded because they did not comply with the protocol, or the birth information could not be retrieved (5.48% lost to follow-up rate). A total of 74% (N = 204) of the primiparous women were at their first pregnancy.
Figure 1 presents the flow chart summarizing the study group. Maternal and labor characteristics are detailed in
Table 1.
4.2. The Fetal Head Situation at Term
The boxplot representation of the clinical FHS at 37 to 41 GW is presented in
Figure 2. The data show no significant differences between vaginal and Cesarean delivery cases in terms of fetal head station determined at each week at term (
p > 0.05).
The median determinations of clinical FHS at 37 to 41 GW were similar between the two groups: −2.5 vs. −3 at 37 GW, −3 vs. −3 at 38GW, −2 vs. −2 at 39 GW, and −2 vs. −2.5 at 40 GW. A more important difference was noted at 41 GW: station -1 for vaginal deliveries compared with station −3 for Cesarean deliveries.
In the following, we present a detailed analysis of each week at term, underlying the characteristics and differences between the two groups: vaginal and Cesarean section delivery (
Figure 3 and
Figure 4).
At 37 weeks of gestation, almost one-third (30.6%, n = 41) of the primiparous women who eventually delivered vaginally were diagnosed with a fetal head station of -3, and almost half (48.5%, n = 65) presented with a clinical fetal head station of −2 and −1. In the CS group, 70% (n = 28) presented a higher than −3 FHS (
Figure 3 and
Figure 4).
At 38 GW, we noted similar percentages of patients in the two groups for all stations, with minor differences of a maximum of 6% (
Figure 3 and
Figure 4).
At 39 GW, we noted higher rates of CS at high FHS: −5 (10.3% vs. 0.8%), −4 (27.6% vs. 14%), and −2 (31% vs. 27.1%), but surprisingly also at more favorable (lower) clinical head stations: 0 (3.4 % vs. 1.6%) and +1 (6.9% vs. 1.6%). Meanwhile, in the group of vaginal births, we noted higher rates at stations −3 (25.6 vs. 3.4%) and −1 (29.5 vs. 17.2%). The distribution does not respect a certain trend.
A similar variable distribution, where the level of the head station was not correlated with a certain type of delivery, was also noted at 40 weeks of gestation (
Figure 3 and
Figure 4).
At 41 weeks of gestation, 58.3% (n = 14) of primiparous women who delivered vaginally presented a clinical head station at −1 (vs. 33.3%, n = 1 of the CS), while 66.7% (n = 2) of the primiparous women who delivered by Cesarean section presented a high (−3) pelvic head station, vs. 20.8% (n = 5) of the VDs group (
Figure 3 and
Figure 4). The differences are visible and important, but they cannot be considered significant because of the low number of pregnancies evaluated.
4.3. Week before Delivery
The design of our study enabled us to observe the distribution of the FHS measurements during the WBD in both groups—vaginal and Cesarean deliveries. The clinical evaluations were performed weekly; therefore, the last measurements before labor onset were assigned to “week before delivery” determinations.
The analysis of these determinations showed for both groups similar minimum (−5), maximum (+1), and median (−2) values for the clinical established FHS (
Figure 5).
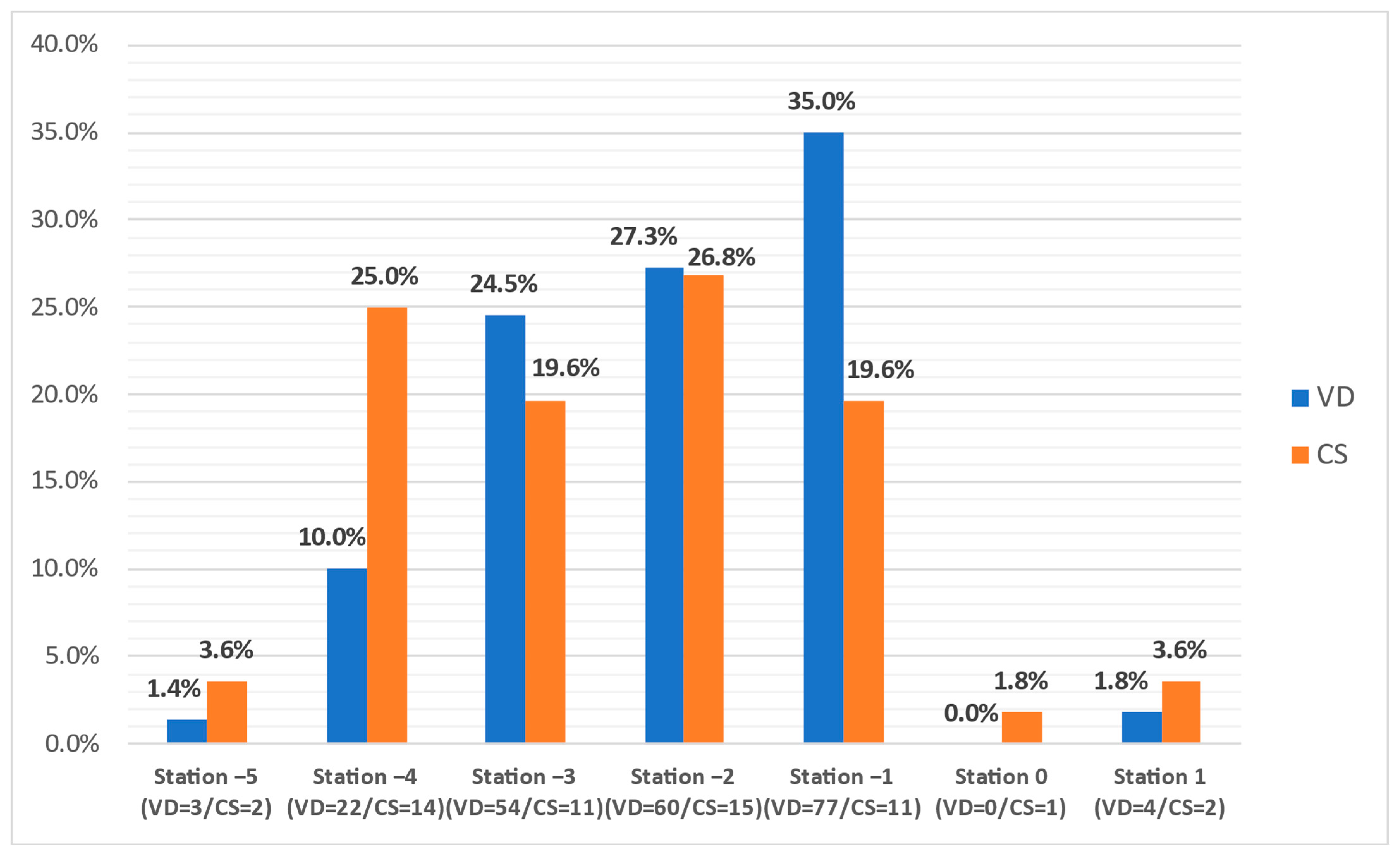
In the group of primiparous women who delivered by Cesarean section, one fifth presented with a clinical fetal head station at −3 (19.6%, n = 11) and −1 (19.6%, n = 11), and one-quarter of cases were noted at the −4 (25%, n = 14) and –2 (26.8%, n = 15) stations (
Figure 6). Most of the women that delivered vaginally were found with similar head stations, but with increasing rates toward more advanced stations: from 10% (n = 22) at station −4 to 35% (n = 77) at station −1. The low number of pregnancies that reached stations 0 and +1 do not allow intergroup comparison. Unlike the weekly evaluations, there were significant differences between the WBD evaluations of the two groups (
p < 0.05).
4.4. Longitudinal Evaluation of Fetal Head Station Depending on the Labor Outcome
Given the study’s longitudinal design, consisting of weekly evaluations at term, we aimed to investigate the evolution of the FHS in the two groups (vaginal and Cesarean delivery) during the term weeks. Therefore, we analyzed the incidence of each FHS throughout the weekly evaluation at term, from 37 to 41 GW in vaginal and Cesarean delivery cases (
Figure 7 and
Figure 8). In both groups, we noted low rates of the extremes, namely stations 0, +1, and −5. In the VD group, the predominant FHS registered were −1, −2, and −3, while the −4 station presented visibly lower rates. Station −4 was better represented in the CS group, in line with the stations mentioned above.
In VD cases (
Figure 7), we noted the predominance of stations −3, −2, and −1 with low extremes (stations −5, −4, 0, +1) and a generally similar trend for all weeks. In the CS group (
Figure 8), we noted station −4 (red line) at higher rates during weeks 39 and 40, and a generally stationary trend at term.
4.5. The Importance of Maternal Clinical Characteristics at Term
We were interested in seeing whether there are significant differences between the two delivery modes regarding the following features: mother’s age, weight, height, and BMI. We have applied the
t-test for independent variables. The results are shown in
Table 2.
From
Table 2, we can see that indeed there are significant differences (
p-value < 0.05) between the two groups in terms of age, weight, and BMI.
Next, we were interested in performing a multiple logistic regression in which the predictive variables considered were the stage of fetal head, age, weight, height, and BMI. The obtained regression equation was:
We also performed an overall goodness of fit through ANOVA. The obtained results in terms of sums of square (SS), degrees of freedom (df), mean squares (MS), F-value, and
p-level are shown in
Table 3.
From
Table 3, we can see that indeed these parameters can be considered when predicting the delivery mode (
p-level < 0.05).
5. Discussion
Using the clinical evaluation of the FHS in primiparous women at term before the labor onset, we expected to find a slow downward progression of the fetal head towards station 0, where fetal head engagement occurs, especially in the group of vaginal deliveries. However, our data showed no significant differences between vaginal and Cesarean delivery cases in terms of the FHS determined at each week at term and a stationary situation of the head descent, with a median station of −3 to −2. The only consistent difference was noted at 41 GW: a −1 median station for the VD group compared to −3 for the CS group, but not a statistically significant difference due to the small number of pregnancies reaching this gestational age. These findings suggest that VD is not associated with a better accommodation or engagement of the fetal head in the maternal pelvis at term.
A policy of early-term evaluation of primipara to estimate labor outcome does not appear helpful. There are some differences regarding the head situation at 37 GW: almost half of the patients that eventually delivered vaginally presented with a clinical FHS of −2 and −1, while in the CS group, 70% presented a higher than −3 clinical FHS. However, the statistical analysis yields no significant differences. Moreover, at 38GW, similar rates of patients in the two groups were found for all stations.
In addition, at 39 and 40 GW, we noted a variable distribution that does not respect a specific trend in more advanced term pregnancies, and FHS was not correlated with a specific type of delivery.
At 41 GW, as mentioned above concerning the median station, the differences were more visible: more than half of the primiparous women who delivered vaginally presented a clinical FHS −1 vs. one-third of the CS women. In contrast, two-thirds of the primiparous women that delivered by Cesarean section presented a high (−3) pelvic head station, vs. one-fifth of the VD cases. Apparently, at 41 GW, there is a substantial discrepancy between the groups, and the fetal head is better accommodated with the maternal pelvis in pregnancies finalized with vaginal delivery. Still, the low number of evaluated pregnancies does not allow us to safely consider this difference statisticaly significant. Nevertheless, if further studies confirm our findings, a policy to predict labor outcome in late-term or prolonged pregnancy could be implemented based on FHS determination.
The determinations performed during the week before delivery showed for both groups a similar minimum (−5), maximum (+1), and median (−2) fetal head station. However, unlike the weekly evaluations, there were significant differences between the two vaginal and Cesarean delivery groups. Among the CS group, one-fifth presented with −3 and −1 FHS, and −4 and –2 stations were noted in one-quarter of cases. Most of the women that delivered vaginally were found with similar FHS (−4 to −2), but a different distribution with increasing and higher rates at more advanced stations: from 10% at station −4 to 35% at station −1.
To our best knowledge, the literature lacks studies on the delivery outcome based on the dynamic evaluation of the fetal head situation at term before the onset of labor. Therefore, we consider this research a good starting point for future larger studies. There is proof regarding the role of fetal head descent at the beginning of labor as a predictor for labor outcome [
22]. In addition, in women undergoing labor induction at term, digital examination accurately predicted vaginal delivery within 24 h, while fetal fibronectin and ultrasound measurements failed to predict the outcome of induced labor [
23] accurately. Our findings do not confirm the role of head engagement determination in standard term evaluations before labor onset [
22,
23,
24,
25]. In an attempt to predict the delivery mode by digital examination in early labor, several studies [
22,
24,
25] found a considerably lower prediction rate for the Cesarean section delivery than in the study of Levy et al. [
16], which used imagistic means to estimate fetal head situation before labor. The future will most likely provide objective ultrasound techniques that include fetal head position and descent evaluations at term, along with maternal history and clinical characteristics, to provide better predictions for labor outcomes. However, some institutions may have limited access to ultrasound or may not possess well-trained sonographers, such as in low income countries. In these circumstances, the clinical FHS determination might be essential to determine the delivery mode.
However, other clinical characteristics should not be neglected, as maternal weight, height, and gestational BMI are independent factors that are associated with an increased chance of caesarean section, and this has been demonstrated in numerous studies [
25,
26,
27,
28,
29]. Although we investigated a low-risk group, we found significant differences between the vaginal and Cesarean groups in terms of age, weight, and BMI, and demonstrated that these parameters should be considered when predicting the delivery mode. Furthermore, we provided a multiple logistic regression equation for clinical practice that considers the predictive clinical variables at term: the fetal head situation, age, weight, height, and BMI. However, the fine tuning of this prediction should be achieved by increasing the studied population and number of centers involved.
6. Strengths and Limitations of This Study
6.1. Strengths
Our observational prospective cohort study of unselected low-risk primigravidae is the first study to assess, in a dynamic way, the clinical head station at term, previously proposed for labor outcome predictions. Our research serves as a beneficial framework where more data could be added for more accurate predictions.
6.2. Limitations
The concept of normalcy is population-based and our study enrolled only Caucasian women, a fact that may affect generalizability.
The study’s dataset is unbalanced, given the discrepancy between the rates and numbers of vaginal and Cesarean births. This fact is due to the unselected/consecutive enrollment of the pregnant primiparous women. Finally, more accurate data may be retrieved from ultrasound evaluations at term, because the intra-observer and inter-observer clinical variability of head station evaluations is significant, independently of the presence of caput succedaneum, significant molding, or head position.
7. Conclusions
In conclusion, we noticed that the clinical evaluation of fetal head station in primiparous women before the onset of labor has a limited potential to provide additional information regarding the prediction of the delivery mode. There is a potential benefit for the determinations performed within the week before delivery, which would require weekly assessments of the head station at term, a policy that is unlikely to be implemented. Another potential benefit was the labor outcome estimation in late-term or prolonged pregnancy. We require confirmation of these data in larger studies before counseling primiparous women at term before the labor onset based on the clinical fetal engagement data. New research should consider ultrasound determinations of the fetal head situation regarding the head station, occiput position, and maternal characteristics.
Author Contributions
Conceptualization, methodology, D.G.I., R.C.D. and M.-L.C.; formal analysis, M.-L.C.; investigation, data curation, writing—original draft preparation, L.M.D., R.C.D., R.D.N.; writing—review and editing, M.-L.C. and D.G.I.; validation, visualization, supervision, project administration, D.G.I. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a grant from the University of Medicine and Pharmacy Craiova, project number 26/531/3, “Prediction of the delivery mode using clinical and ultrasound evaluation at term” (CLINECO). The Article Processing Charges were funded by the University of Medicine and Pharmacy of Craiova, Romania.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of University of Medicine and Pharmacy of Craiova (18/26.02.2016).”
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cunningham, F.; Leveno, K.J.; Bloom, S.L.; Spong, C.Y.; Dashe, J.S.; Hoffman, B.L.; Casey, B.M.; Sheffield, J.S. Chapter 22 Normal Labor Williams Obstetrics, 24th ed.; McGraw Hill: New York, NY, USA, 2014; pp. 899, 924. [Google Scholar]
- Norwitz, E.R.; Robinson, J.N.; Repke, J.T. Labor and delivery. In Obstetrics: Normal and Problem Pregnancies, 4th ed.; Gabbe, S.G., Niebyl, J.R., Simpson, J.L., Eds.; Churchill Livingstone: New York, NY, USA, 2001; pp. 353–394. [Google Scholar]
- Downe, S.; Gyte, G.M.; Dahlen, H.G.; Singata, M. Routine vaginal examinations for assessing progress of labour to improve outcomes for women and babies at term. Cochrane Database Syst. Rev. 2013, 15, CD010088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friedman, E.A. Labor in multiparas; a graphicostatistical analysis. Obstet. Gynecol. 1956, 8, 691–703. [Google Scholar] [CrossRef]
- Messina, M.P.; Piccioni, M.G.; Petrella, C.; Vitali, M.; Greco, A.; Ralli, M.; Ceccanti, M.; Ferraguti, G.; Neri, I.; Ricchi, A.; et al. Advanced midwifery practice: Intrapartum ultrasonography to assess fetal head station and comparison with vaginal digital examination. Minerva Obstet. Gynecol. 2021, 73, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Roosevelt, L.; Diebel, M.; Zielinski, R.E. Achieving competency in vaginal examinations: The challenge of balancing student learning needs with best practice in maternity care. Midwifery 2018, 61, 39–41. [Google Scholar] [CrossRef]
- Drăgușin, R.C.; Șorop-Florea, M.; Pătru, C.L.; Zorilă, L.G.; Sirbu, M.; Cernea, N.; Tudorache, S.; Iliescu, D.G. Ultrasound Longitudinal Evaluation of Fetal Head Engagement before the Onset of Labor. A Clinical Protocol and Pilot Study. In Proceedings of the Conference Proceedings, 5th Congress of the Romanian Society of Ultrasound in Obstetrics and Gynecology, Targu Mures, Romania, 20–22 April 2017. [Google Scholar]
- Popowski, T.; Porcher, R.; Fort, J.; Javoise, S.; Rozenberg, P. Influence of ultrasound determination of fetal head position on mode of delivery: A pragmatic randomized trial. Ultrasound Obstet. Gynecol. 2015, 46, 520–525. [Google Scholar] [CrossRef]
- Gillor, M.; Vaisbuch, E.; Zaks, S.; Barak, O.; Hagay, Z.; Levy, R. Transperineal sonographic assessment of angle of progression as a predictor of successful vaginal delivery following induction of labor. Ultrasound Obstet. Gynecol. 2017, 49, 240–245. [Google Scholar] [CrossRef]
- Sherer, D.M.; Onyeije, C.I.; Bernstein, P.S.; Kovacs, P.; Manning, F.A. Utilization of real-time ultrasound on labor and delivery in an active academic teaching hospital. Am. J. Perinatol. 1999, 16, 303–307. [Google Scholar] [CrossRef]
- Armbrust, R.; Henrich, W.; Hinkson, L.; Grieser, C.; Siedentopf, J.P. Correlation of intrapartum translabial ultrasound parameters with computed tomographic 3D reconstruction of the female pelvis. J. Perinat. Med. 2016, 44, 567–571. [Google Scholar] [CrossRef]
- Iliescu DG, Dragusin RC, Cernea D, Patru CL, Florea M, Tudorache S, Intrapartum ultrasound-an integrated approach for best prognosis. Med. Ultrason. 2017, 19, 932.
- Iliescu, D.G.; Drăguşin, R.C.; Şorop-Florea, M.; Novac, M.; Căpitănescu, R.G.; Tudorache, Ş. Intrapartum ultrasound-Potential benefit in late occiput rotation from posterior to anterior position. Obstet. Ginecol. 2016, 64, 183–186. [Google Scholar]
- Ludvigsen, E.; Skjeldestad, F.E. Station of the fetal head at complete cervical dilation impacts duration of second stage of labor. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2019, 31, 100100. [Google Scholar] [CrossRef] [PubMed]
- Dupuis, O.; Silveira, R.; Zetner, A.; Dittmar, A.; Gaucherand, P.; Cucherat, M.; Redarce, T.; Rudigoz, R.-C. Birth simulator: Reliability of transvaginal assessment of fetal head station as defined by the American College of Obstetricians and Gynecologists classification. Am. J. Obstet. Gynecol. 2005, 192, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Levy, R.; Zaks, S.; Ben-Arie, A.; Perlman, S.; Hagay, Z.; Vaisbuch, E. Can the “angle of progression” as measured in pregnant women before the onset of labor predict mode of delivery? Ultrasound Obstet. Gynecol. 2012, 40, 332–337. [Google Scholar] [CrossRef] [PubMed]
- Kilpatrick, S.; Garrison, E. Chapter 12. Normal Labor and Delivery. In Obstetrics: Normal and Problem Pregnancies, 7th ed.; Gabbe, S., Niebyl, J., Simpson, J., Landon, M., Galan, H., Jauniaux, E., Driscoll, D., Berghella, V., Grobman, W., Eds.; Churchill Livingstone: New York, NY, USA, 2017; p. 253. [Google Scholar]
- Cunningham, F.G.; Leveno, K.J.; Bloom, S.L.; Dashe, J.S.; Hoffman, B.L.; Casey, B.M.; Spong, C.Y. (Eds.) CHAPTER 2 Maternal Anatomy, p.68; CHAPTER 21 Physiology of Labor, p.414, CHAPTER 22 Normal Labor, p.427. In Williams Obstetrics, 25th ed.; McGraw Hill: New York, NY, USA, 2018; pp. 68, 414, 427. [Google Scholar]
- Marshall, J.E.; Raynor, M.D. (Eds.) Myles Textbook for Midwives, 16th ed.; Chapter 9. Changes and Adaptation in Pregnancy; 10. Antenatal Carep; 17. Physiology and Care during the Transition and Second Stages Phases of Labor; Churchill Livingstone Elsevier: Edinburgh, UK, 2014; pp. 148, 193, 373. [Google Scholar]
- Iliescu, D. Re: Can angle of progression in pregnant women before onset of labor predict mode of delivery? R. Levy, S. Zaks, A. Ben-Arie, S. Perlman, Z. Hagay and E. Vaisbuch. Ultrasound Obstet Gynecol 2012; 40: 332-337. Ultrasound Obstet. Gynecol. 2012, 40, 255–256. [Google Scholar] [CrossRef]
- Youssef, A.; Dodaro, M.G.; Montaguti, E.; Consolini, S.; Ciarlariello, S.; Farina, A.; Bellussi, F.; Rizzo, N.; Pilu, G. Dynamic changes of fetal head descent at term before the onset of labor correlate with labor outcome and can be improved by ultrasound visual feedback. J. Matern.-Fetal Neonatal Med. 2021, 34, 1847–1854. [Google Scholar] [CrossRef]
- Roshanfekr, D.; Blakemore, K.J.; Lee, J.; Hueppchen, N.A.; Witter, F.R. Station at onset of active labor in nulliparous patients and risk of caesarean delivery. Obstet. Gynecol. 1999, 93, 329–331. [Google Scholar]
- Reis, F.M.; Gervasi, M.T.; Florio, P.; Bracalente, G.; Fadalti, M.; Severi, F.M.; Petraglia, F. Prediction of successful induction of labor at term: Role of clinical history, digital examination, ultrasound assessment of the cervix, and fetal fibronectin assay. Am. J. Obstet. Gynecol. 2003, 189, 1361–1367. [Google Scholar] [CrossRef]
- Debby, A.; Rotmensch, S.; Girtler, O.; Sadan, O.; Golan, A.; Glezerman, M. Clinical significance of the floating fetal head in nulliparous women in labor. J. Reprod. Med. 2003, 48, 37–40. [Google Scholar]
- Shin, K.S.; Brubaker, K.L.; Ackerson, L.M. Risk of cesarean delivery in nulliparous women at greater than 41 weeks’ gestational age with an unengaged vertex. Am. J. Obstet. Gynecol. 2004, 190, 129–134. [Google Scholar] [CrossRef]
- Xiong, C.; Zhou, A.; Cao, Z.; Zhang, Y.; Qiu, L.; Yao, C.; Wang, Y.; Zhang, B. Association of pre-pregnancy body mass index, gestational weight gain with cesarean section in term deliveries of China. Sci. Rep. 2016, 6, 37168. [Google Scholar] [CrossRef] [Green Version]
- Huang, L.; Zhang, J.; Sun, H.; Dong, H.; Li, R.; Cai, C.; Gao, Y.; Wu, C.; Lan, X.; Zeng, G. Association of gestational weight gain with cesarean section: A prospective birth cohort study in Southwest China. BMC Pregnancy Childbirth 2021, 21, 57. [Google Scholar] [CrossRef] [PubMed]
- Mogren, I.; Lindqvist, M.; Petersson, K.; Nilses, C.; Small, R.; Granåsen, G.; Edvardsson, K. Maternal height and risk of caesarean section in singleton births in Sweden-A population-based study using data from the Swedish Pregnancy Register 2011 to 2016. PLoS ONE 2018, 13, e0198124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marbaniang, S.P.; Lhungdim, H.; Chaurasia, H. Effect of maternal height on the risk of caesarean section in singleton births: Evidence from a large-scale survey in India. BMJ Open 2022, 12, e054285. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).