Quality of Life in Older Patients after a Heart Failure Hospitalization: Results from the SENECOR Study
Abstract
1. Introduction
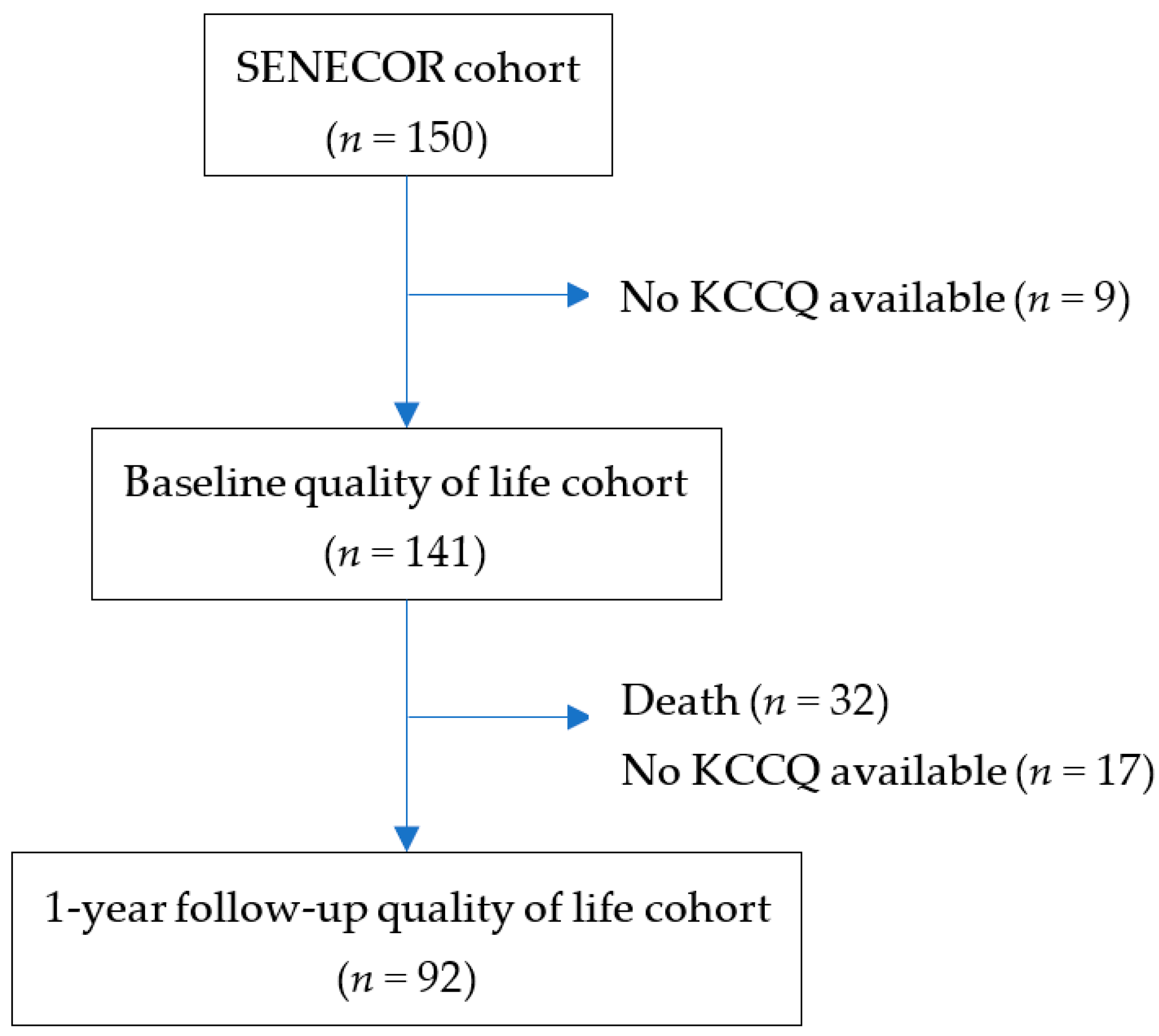
2. Materials and Methods
2.1. Study Design
2.2. Quality-of-Life Assessment
2.3. Study Outcome
2.4. Statistical Analysis
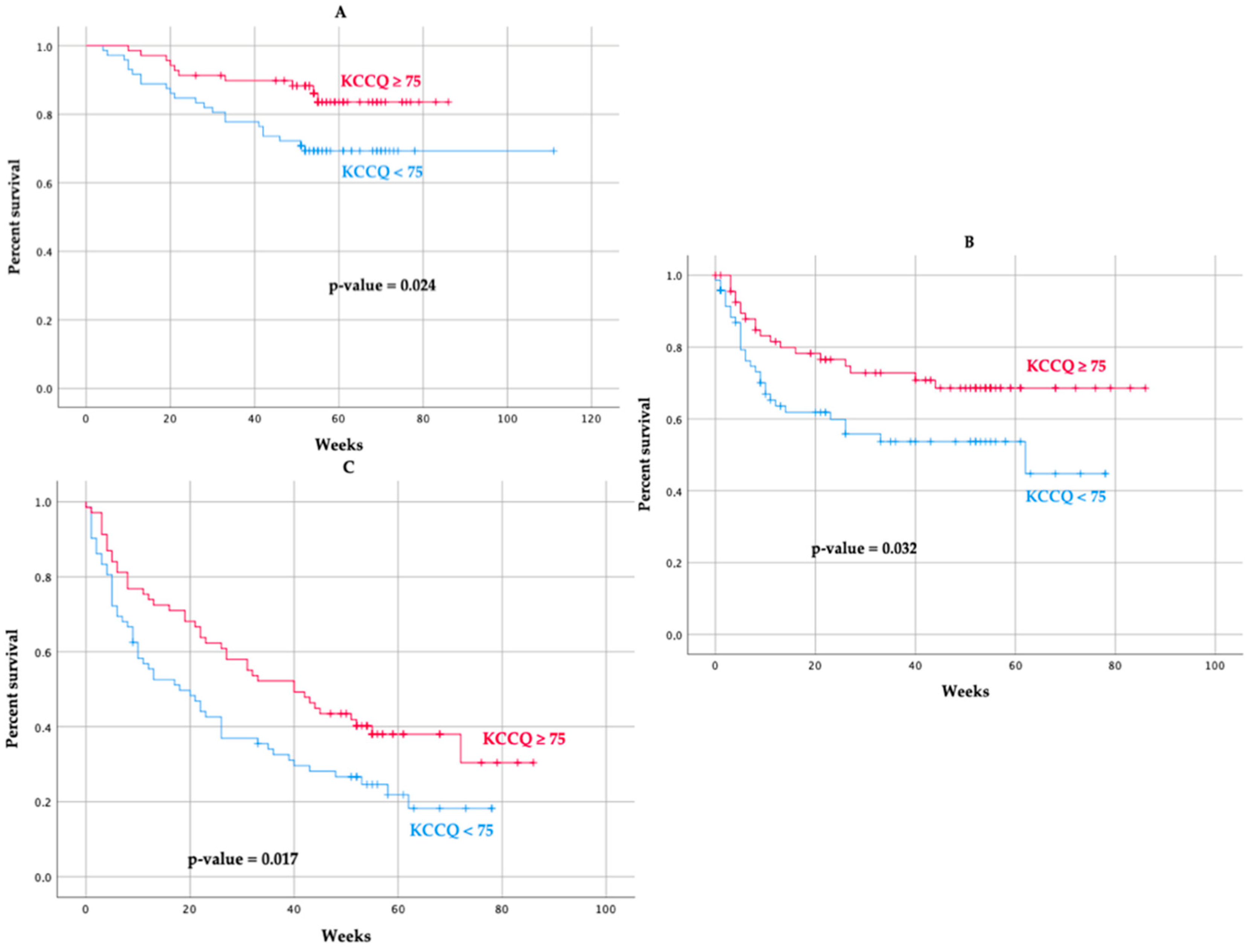
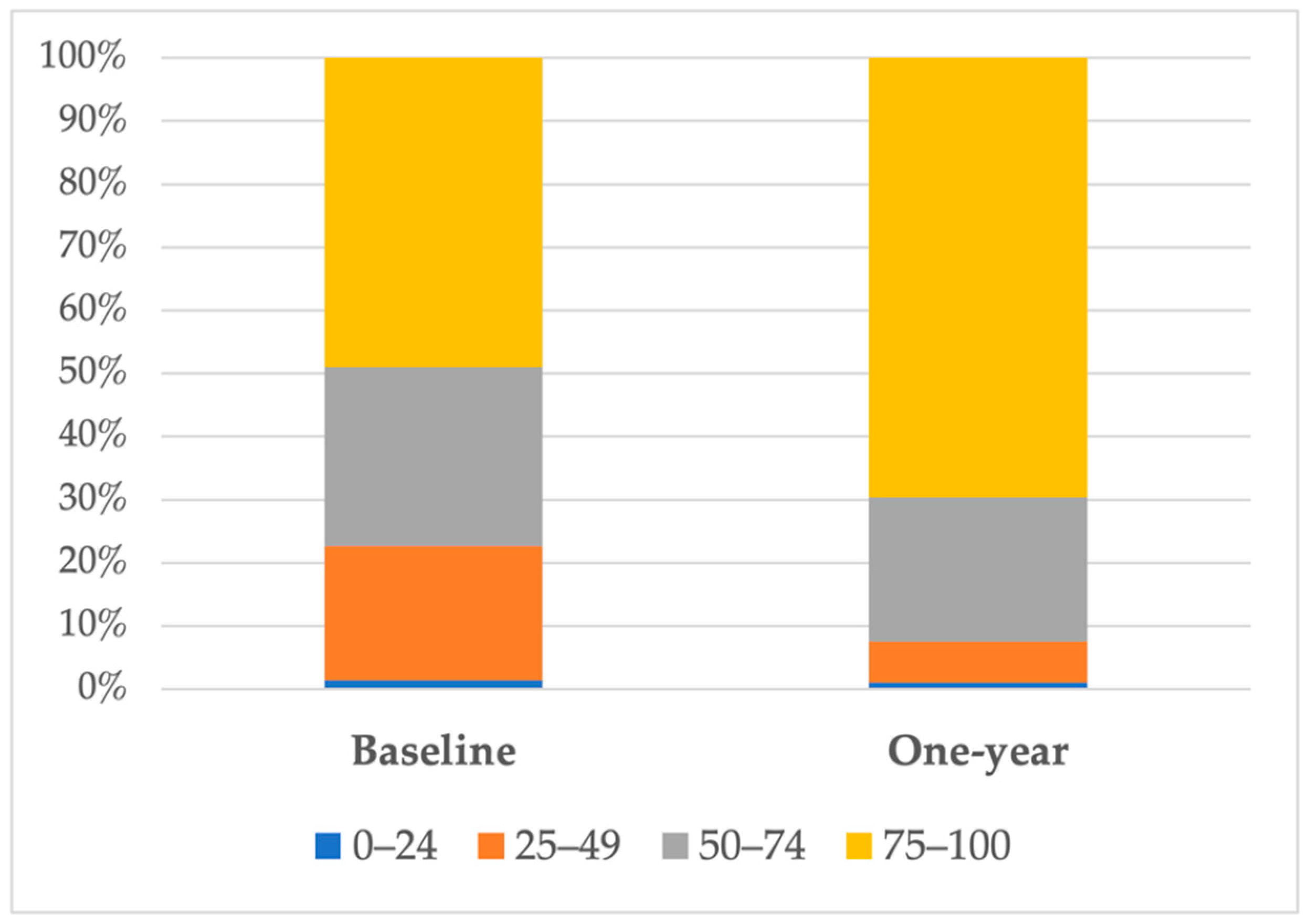
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Farré, N.; Vela, E.; Clèries, M.; Bustins, M.; Cainzos-Achirica, M.; Enjuanes, C.; Moliner, P.; Ruiz, S.; Verdú-Rotellar, J.M.; Comín-Colet, J. Medical Resource Use and Expenditure in Patients with Chronic Heart Failure: A Population-Based Analysis of 88 195 Patients. Eur. J. Heart Fail. 2016, 18, 1132–1140. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Anand, I.S.; Florea, V.G.; Fisher, L. Surrogate End Points in Heart Failure. J. Am. Coll. Cardiol. 2002, 39, 1414–1421. [Google Scholar] [CrossRef][Green Version]
- McMurray, J. Heart Failure: We Need More Trials in Typical Patients. Eur. Heart J. 2000, 21, 699–700. [Google Scholar] [CrossRef]
- Cohn, J.; Cleland, J.G.F.; Lubsen, J.; Borer, J.S.; Steg, P.G.; Perelman, M.; Zannad, F. Unconventional End Points in Cardiovascular Clinical Trials: Should We Be Moving Away from Morbidity and Mortality? J. Card. Fail. 2009, 15, 199–205. [Google Scholar] [CrossRef]
- Al-Kaade, S.; Hauptman, P.J. Health-Related Quality of Life Measurement in Heart Failure: Challenges for the New Millennium. J. Card. Fail. 2001, 7, 194–201. [Google Scholar] [CrossRef]
- Sullivan, M.D.; Levy, W.C.; Russo, J.E.; Crane, B.; Spertus, J.A. Summary Health Status Measures in Advanced Heart Failure: Relationship to Clinical Variables and Outcome. J. Card. Fail. 2007, 13, 560–568. [Google Scholar] [CrossRef]
- Heidenreich, P.A.; Spertus, J.A.; Jones, P.G.; Weintraub, W.S.; Rumsfeld, J.S.; Rathore, S.S.; Peterson, E.D.; Masoudi, F.A.; Krumholz, H.M.; Havranek, E.P.; et al. Health Status Identifies Heart Failure Outpatients at Risk for Hospitalization or Death. J. Am. Coll. Cardiol. 2006, 47, 752–756. [Google Scholar] [CrossRef]
- Comín-Colet, J.; Garin, O.; Lupón, J.; Manito, N.; Crespo-Leiro, M.G.; Gómez-Bueno, M.; Ferrer, M.; Artigas, R.; Zapata, A.; Elosua, R.; et al. Validation of the Spanish Version of the Kansas City Cardiomyopathy Questionnaire. Rev. Esp. Cardiol. 2011, 64, 51–58. [Google Scholar] [CrossRef]
- Kosiborod, M.N.; Jhund, P.S.; Docherty, K.F.; Diez, M.; Petrie, M.C.; Verma, S.; Nicolau, J.C.; Merkely, B.; Kitakaze, M.; DeMets, D.L.; et al. Effects of Dapagliflozin on Symptoms, Function, and Quality of Life in Patients With Heart Failure and Reduced Ejection Fraction: Results From the DAPA-HF Trial. Circulation 2020, 141, 90–99. [Google Scholar] [CrossRef]
- Kosiborod, M.; Soto, G.E.; Jones, P.G.; Krumholz, H.M.; Weintraub, W.S.; Deedwania, P.; Spertus, J.A. Identifying Heart Failure Patients at High Risk for Near-Term Cardiovascular Events with Serial Health Status Assessments. Circulation 2007, 115, 1975–1981. [Google Scholar] [CrossRef]
- Luo, N.; Teng, T.-H.K.; Tay, W.T.; Anand, I.S.; Kraus, W.E.; Liew, H.B.; Ling, L.H.; O’Connor, C.M.; Piña, I.L.; Richards, A.M.; et al. Multinational and Multiethnic Variations in Health-Related Quality of Life in Patients with Chronic Heart Failure. Am. Heart J. 2017, 191, 75–81. [Google Scholar] [CrossRef]
- Ambrosy, A.P.; Hernandez, A.F.; Armstrong, P.W.; Butler, J.; Dunning, A.; Ezekowitz, J.A.; Felker, G.M.; Greene, S.J.; Kaul, P.; McMurray, J.J.; et al. The Clinical Course of Health Status and Association with Outcomes in Patients Hospitalized for Heart Failure: Insights from ASCEND-HF. Eur. J. Heart Fail. 2016, 18, 306–313. [Google Scholar] [CrossRef]
- Dunlay, S.M.; Gheorghiade, M.; Reid, K.J.; Allen, L.A.; Chan, P.S.; Hauptman, P.J.; Zannad, F.; Maggioni, A.P.; Swedberg, K.; Konstam, M.A.; et al. Critical Elements of Clinical Follow-up after Hospital Discharge for Heart Failure: Insights from the EVEREST Trial. Eur. J. Heart Fail. 2010, 12, 367–374. [Google Scholar] [CrossRef]
- Ekman, I.; Chassany, O.; Komajda, M.; Böhm, M.; Borer, J.S.; Ford, I.; Tavazzi, L.; Swedberg, K. Heart Rate Reduction with Ivabradine and Health Related Quality of Life in Patients with Chronic Heart Failure: Results from the SHIFT Study. Eur. Heart J. 2011, 32, 2395–2404. [Google Scholar] [CrossRef]
- Lewis, E.F.; Johnson, P.A.; Johnson, W.; Collins, C.; Griffin, L.; Stevenson, L.W. Preferences for Quality of Life or Survival Expressed by Patients with Heart Failure. J. Heart Lung Transplant. 2001, 20, 1016–1024. [Google Scholar] [CrossRef]
- Herrero-Torrus, M.; Badosa, N.; Roqueta, C.; Ruiz-Bustillo, S.; Solé-González, E.; Belarte-Tornero, L.C.; Valdivielso-Moré, S.; Vázquez, O.; Farré, N. Randomized Controlled Trial Comparing a Multidisciplinary Intervention by a Geriatrician and a Cardiologist to Usual Care after a Heart Failure Hospitalization in Older Patients: The SENECOR Study. J. Clin. Med. 2022, 11, 1932. [Google Scholar] [CrossRef]
- Rockwood, K. A Global Clinical Measure of Fitness and Frailty in Elderly People. Can. Med. Assoc. J. 2005, 173, 489–495. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Pfeiffer, E. A Short Portable Mental Status Questionnaire for the Assessment of Organic Brain Deficit in Elderly Patients. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef]
- Spertus, J.A.; Jones, P.G. Development and Validation of a Short Version of the Kansas City Cardiomyopathy Questionnaire. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 469–476. [Google Scholar] [CrossRef]
- Garcia-Caselles, P.; Miralles, R.; Arellano, M.; Torres, R.M.; Aguilera, A.; Pi-Figueras, M.; Cervera, A.M. Validation of A Modified Version of the Gijon’s Social-Familial Evaluation Scale (Sfes): The “Barcelona Sfes Version”, for Patients with Cognitive Impairment. Arch. Gerontol. Geriatr. 2004, 38, 201–206. [Google Scholar] [CrossRef]
- Martí, D.; Miralles, R.; Llorach, I.; García Palleiro, P.; Esperanza, A.; Guillem, J.; Cervera, A.M. Depressive Mood Disorders in an Inpatient Convalescence Unit: Experience and Validation of a 15-Items Spanish Version of the Yesavage Geriatric Depression Scale. Rev. Esp. Geriatr. Gerontol. 2000, 35, 7–14. [Google Scholar]
- Rubenstein, L.Z.; Harker, J.O.; Salva, A.; Guigoz, Y.; Vellas, B. Screening for Undernutrition in Geriatric Practice: Developing the Short-Form Mini-Nutritional Assessment (MNA-SF). J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef]
- Joseph, S.M.; Novak, E.; Arnold, S.V.; Jones, P.G.; Khattak, H.; Platts, A.E.; Dávila-Román, V.G.; Mann, D.L.; Spertus, J.A. Comparable Performance of the Kansas City Cardiomyopathy Questionnaire in Patients With Heart Failure With Preserved and Reduced Ejection Fraction. Circ. Heart Fail. 2013, 6, 1139–1146. [Google Scholar] [CrossRef]
- Green, C.P.; Porter, C.B.; Bresnahan, D.R.; Spertus, J.A. Development and Evaluation of the Kansas City Cardiomyopathy Questionnaire: A New Health Status Measure for Heart Failure. J. Am. Coll. Cardiol. 2000, 35, 1245–1255. [Google Scholar] [CrossRef]
- Spertus, J.; Peterson, E.; Conard, M.W.; Heidenreich, P.A.; Krumholz, H.M.; Jones, P.; McCullough, P.A.; Pina, I.; Tooley, J.; Weintraub, W.S.; et al. Monitoring Clinical Changes in Patients with Heart Failure: A Comparison of Methods. Am. Heart J. 2005, 150, 707–715. [Google Scholar] [CrossRef]
- Hauptman, P.J.; Masoudi, F.A.; Weintraub, W.S.; Pina, I.; Jones, P.G.; Spertus, J.A. Variability in the Clinical Status of Patients with Advanced Heart Failure. J. Card. Fail. 2004, 10, 397–402. [Google Scholar] [CrossRef]
- Spertus, J.A.; Jones, P.G.; Sandhu, A.T.; Arnold, S.V. Interpreting the Kansas City Cardiomyopathy Questionnaire in Clinical Trials and Clinical Care. J. Am. Coll. Cardiol. 2020, 76, 2379–2390. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Pokharel, Y.; Khariton, Y.; Tang, Y.; Nassif, M.E.; Chan, P.S.; Arnold, S.V.; Jones, P.G.; Spertus, J.A. Association of Serial Kansas City Cardiomyopathy Questionnaire Assessments with Death and Hospitalization in Patients With Heart Failure With Preserved and Reduced Ejection Fraction. JAMA Cardiol. 2017, 2, 1315. [Google Scholar] [CrossRef]
- Ravera, A.; Santema, B.T.; Sama, I.E.; Meyer, S.; Lombardi, C.M.; Carubelli, V.; Ferreira, J.P.; Lang, C.C.; Dickstein, K.; Anker, S.D.; et al. Quality of Life in Men and Women with Heart Failure: Association with Outcome, and Comparison between the Kansas City Cardiomyopathy Questionnaire and the EuroQol 5 Dimensions Questionnaire. Eur. J. Heart Fail. 2021, 23, 567–577. [Google Scholar] [CrossRef]
- Severino, P.; D’Amato, A.; Prosperi, S.; Dei Cas, A.; Mattioli, A.V.; Cevese, A.; Novo, G.; Prat, M.; Pedrinelli, R.; Raddino, R.; et al. Do the Current Guidelines for Heart Failure Diagnosis and Treatment Fit with Clinical Complexity? J. Clin. Med. 2022, 11, 857. [Google Scholar] [CrossRef]
- Bekelman, D.B.; Plomondon, M.E.; Carey, E.P.; Sullivan, M.D.; Nelson, K.M.; Hattler, B.; McBryde, C.F.; Lehmann, K.G.; Gianola, K.; Heidenreich, P.A.; et al. Primary Results of the Patient-Centered Disease Management (PCDM) for Heart Failure Study. JAMA Intern. Med. 2015, 175, 725. [Google Scholar] [CrossRef]
- Lewis, E.F. Are Hospitalizations for Heart Failure the Great Equalizer? JACC Heart Fail. 2015, 3, 539–541. [Google Scholar] [CrossRef]
| KCCQ < 75 (n = 72) | KCCQ 75–100 (n = 69) | p-Value | |
|---|---|---|---|
| Age (years) | 81.7 ± 4.8 | 82.3 ± 4.7 | 0.43 |
| Female | 37 (51.4) | 34 (49.3) | 0.80 |
| Hypertension | 63 (90) | 62 (89.9) | 0.98 |
| Diabetes mellitus | 31 (44.3) | 28 (41.2) | 0.71 |
| Dyslipidemia | 47 (66.2) | 41 (59.4) | 0.41 |
| Stroke/TIA | 9 (13.4) | 10 (15.4) | 0.75 |
| Chronic kidney disease | 54 (75) | 44 (63.8) | 0.15 |
| Anemia | 42 (58.3) | 39 (56.5) | 0.83 |
| Peripheral vascular disease | 9 (12.7) | 14 (20.6) | 0.21 |
| Chronic lung disease | 28 (38.9) | 18 (26.1) | 0.11 |
| Cancer | 16 (22.5) | 19 (27.9) | 0.43 |
| Myocardial infarction | 18 (25) | 11 (15.9) | 0.18 |
| Coronary percutaneous intervention | 14 (19.4) | 10 (14.5) | 0.43 |
| TAVI or Mitraclip | 1 (1.4) | 2 (2.9) | 0.48 |
| Cardiac surgery: | |||
| CABG | 2 (2.8) | 3 (4.3) | |
| Valve replacement | 4 (5.6) | 6 (8.7) | 0.60 |
| CABG and valve replacement | 3 (4.2) | 2 (2.8) | |
| Atrial fibrillation or flutter | 54 (75) | 43 (62.3) | 0.10 |
| Moderate-to-severe valve disease | 22 (31.4) | 22 (32.8) | 0.86 |
| Device therapy: | |||
| Pacemaker | 12 (16.7) | 10 (14.5) | 0.52 |
| CRT or ICD | 1 (1.4) | 4 (5.7) | |
| Previous history of HF | 43 (59.7) | 38 (55.1) | 0.58 |
| Duration of HF *: | |||
| <3 months | 12 (27.9) | 3 (7.9) | |
| 3–6 months | 1 (2.3) | 3 (7.9) | |
| 6–12 months | 4 (9.3) | 5 (13.2) | 0.18 |
| 1–5 years | 17 (39.5) | 15 (39.5) | |
| >5 years | 9 (20.9) | 11 (28.9) | |
| HF hospitalization the previous year * | 19 (45.2) | 12 (32.4) | 0.25 |
| HF categories: | |||
| HFpEF (LVEF ≥ 50%) | 48 (66.7) | 46 (66.7) | |
| HFmrEF (LVEF 40–49%) | 9 (12.5) | 6 (8.7) | 0.70 |
| HFrEF (LVEF < 40%) | 15 (20.8) | 17 (24.6) | |
| Ecocardiographic parameters: | |||
| LVEF (%) | 52.1 ± 13.6 | 52.7 ± 15.2 | 0.79 |
| Left ventricular mass index (g/m2), n = 134 | 120.2 ± 30.7 | 134.2 ± 36.7 | 0.018 |
| TAPSE (mm), n = 126 | 17.5 ± 4.3 | 17.3 ± 3.6 | 0.72 |
| Right ventricle (mm), n = 88 | 28.9 ± 6.7 | 29.7 ± 7.3 | 0.56 |
| Heart failure etiology | |||
| Ischaemic | 10 (14.1) | 12 (17.4) | |
| Hypertensive | 11 (15.5) | 12 (17.4) | |
| Dilated cardiomyopathy | 4 (5.6) | 6 (8.7) | 0.16 |
| Valve heart disease | 21 (29.6) | 17 (24.6) | |
| Other/unknown | 25 (35.2) | 22 (31.9) | |
| Medications at discharge: | |||
| ACEI/ARB-II/ARNI | 35 (49.3) | 39 (57.4) | 0.34 |
| MRA | 9 (12.7) | 12 (17.6) | 0.41 |
| Betablockers | 52 (73.2) | 49 (72.1) | 0.87 |
| Diuretics | 68 (95.8) | 67 (98.5) | 0.62 |
| Anticoagulation | 53 (74.6) | 46 (67.6) | 0.36 |
| Antiplatelet therapy | 12 (16.9) | 14 (20.6) | 0.58 |
| Oral antidiabetic drugs | 24 (34.3) | 20 (29.4) | 0.54 |
| Insulin | 14 (19.7) | 10 (14.7) | 0.43 |
| Proton-pump inhibitors | 48 (67.6) | 46 (67.6) | 1.00 |
| Statin | 50 (70.4) | 37 (54.4) | 0.051 |
| Calcium channel antagonists | 25 (36.2) | 17 (25.0) | 0.15 |
| Nitrates | 16 (22.5) | 10 (14.7) | 0.24 |
| Hydralazine | 10 (14.1) | 7 (10.3) | 0.50 |
| Amiodarone | 16 (22.9) | 8 (11.8) | 0.09 |
| Digoxin | 3 (4.3) | 1 (1.5) | 0.62 |
| Vitamin D supplements | 25 (35.2) | 20 (29.4) | 0.47 |
| Oral iron supplements | 19 (26.8) | 19 (27.9) | 0.88 |
| Benzodiazepines | 16 (22.5) | 14 (20.6) | 0.78 |
| Antidepressant drugs | 20 (28.2) | 16 (23.5) | 0.53 |
| Bronchodilators | 27 (38.0) | 20 (29.4) | 0.28 |
| KCCQ < 75 (n = 72) | KCCQ 75–100 (n = 69) | p-Value | |
|---|---|---|---|
| NT-proBNP at discharge, pg/mL | 1977.5 (950.5–3917.0) | 2774.5 (1767.0–6191.5) | 0.018 |
| High-sensitivity T troponin (Hs-TnT) at discharge, ng/L | 37.5 (26.6–65.1) | 43.7 (30.5–70.2) | 0.26 |
| eGFR (mL/min) at discharge | 46.4 ± 19.9 | 47.3 ± 20.4 | 0.81 |
| Frailty (Clinical Frailty Scale) ≥ 4 | 44 (61.1) | 27 (40.3) | 0.014 |
| Clinical Frailty Scale | 4.2 ± 1.4 | 3.7 ± 1.1 | 0.02 |
| Barthel index | 81.8 ± 19.7 | 90.4 ± 12.3 | 0.002 |
| Basic activities of daily living (Barthel index): | |||
| Independent (100) | 17 (23.6) | 25 (36.2) | |
| Minimally dependent (61–99) | 45 (62.5) | 41 (59.4) | 0.07 |
| Partially to totally dependent (0–60) | 10 (13.9) | 3 (4.3) | |
| Instrumental activities of daily living (Lawton index) | 4.6 ± 2.3 | 5.3 ± 1.9 | 0.054 |
| Pfeiffer Short Portable Mental Status Questionnaire (SPMSQ) | 1 (1–3) | 1 (0–2) | 0.08 |
| NYHA functional class | 2.5 ± 0.6 | 2 ± 0.4 | <0.001 |
| Intervention geriatrician and cardiologist | 31 (43.1) | 40 (58) | 0.08 |
| KCCQ-12 at baseline | 53 ± 15.9 | 88.3 ± 7.8 | <0.001 |
| KCCQ < 75 (n = 72) | KCCQ 75–100 (n = 69) | p-Value | |
|---|---|---|---|
| All-cause mortality | 22 (30.6) | 10 (14.5) | 0.014 |
| All-cause hospitalization | 55 (76.4) | 43 (62.3) | 0.017 |
| HF hospitalization | 30 (41.7) | 19 (27.5) | 0.051 |
| No KCCQ Improvement (n = 15) | KCCQ Improvement (n = 29) | p-Value | |
|---|---|---|---|
| Age (years) | 80.0 ± 4.4 | 81.9 ± 5.08 | 0.23 |
| Female | 11 (73.3) | 12 (41.4) | 0.04 |
| Hypertension | 14 (93.3) | 25 (89.3) | 1.00 |
| Diabetes mellitus | 8 (53.3) | 14 (50) | 0.84 |
| Dyslipidemia | 11 (73.3) | 19 (65.5) | 0.74 |
| Stroke/TIA | 2 (13.3) | 4 (14.8) | 1.00 |
| Chronic kidney disease | 11 (73.3) | 22 (75.9) | 1.00 |
| Anemia | 9 (60) | 14 (48.3) | 0.46 |
| Peripheral vascular disease | 2 (14.3) | 4 (13.8) | 1.00 |
| Chronic lung disease | 6 (40) | 9 (31) | 0.55 |
| Cancer | 2 (13.3) | 10 (34.5) | 0.17 |
| Myocardial infarction | 2 (13.3) | 4 (13.8) | 1.00 |
| Coronary percutaneous intervention | 2 (13.3) | 7 (24.1) | 0.69 |
| TAVI or Mitraclip | 1 (7.1) | 0 (0) | 0.33 |
| Cardiac surgery: | 2 (13.3) | 4 (13.8) | 0.69 |
| Atrial fibrillation or flutter | 10 (66.7) | 23 (79.3) | 0.47 |
| Moderate to severe valve disease | 4 (28.6) | 8 (27.6) | 1.00 |
| Device therapy: | |||
| Pacemaker | 12 (16.7) | 10 (14.5) | 0.52 |
| CRT or ICD | 1 (1.4) | 4 (5.7) | |
| Previous history of HF | 7 (46.7) | 18 (62.1) | 0.33 |
| HF hospitalization the previous year * | 2 (28.6) | 5 (29.4) | 1.00 |
| LVEF (%) | 62.3 ± 3.9 | 49.3 ± 13.2 | <0.001 |
| No KCCQ Improvement (n = 15) | KCCQ Improvement (n = 29) | p-Value | |
|---|---|---|---|
| NT-proBNP at discharge, pg/mL | 1162 (606.6–3579.0) | 1799.5 (801.9–3562.5) | 0.44 |
| High-sensitivity T troponin (Hs-TnT) at discharge, ng/L | 31.6 (22.9–44.5) | 46.9 (22.4–73.0) | 0.21 |
| eGFR (mL/min) at discharge | 52.9 ± 23.2 | 46.0 ± 22.1 | 0.36 |
| Frailty (Clinical Frailty Scale) ≥ 4 | 12 (80.0) | 16 (55.2) | 0.11 |
| Clinical Frailty Scale | 4.5 ± 1.4 | 3.9 ± 1.1 | 0.14 |
| Barthel index | 76.2 ± 22.0 | 86.1 ± 15.3 | 0.09 |
| Instrumental activities of daily living (Lawton index) | 4.5 ± 2.3 | 4.6 ± 2.0 | 0.82 |
| Pfeiffer Short Portable Mental Status Questionnaire (SPMSQ) | 1 (1–2) | 1 (1–3) | 0.62 |
| NYHA functional class | 2.7 ± 0.7 | 2.2 ± 0.6 | 0.053 |
| Intervention geriatrician and cardiologist | 8 (53.3) | 15 (51.7) | 0.92 |
| KCCQ-12 at baseline | 55.1 ± 15.3 | 52.6 ± 17.5 | 0.64 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luiso, D.; Herrero-Torrus, M.; Badosa, N.; Roqueta, C.; Ruiz-Bustillo, S.; Belarte-Tornero, L.C.; Valdivielso-Moré, S.; Morales, R.O.; Vázquez, O.; Farré, N. Quality of Life in Older Patients after a Heart Failure Hospitalization: Results from the SENECOR Study. J. Clin. Med. 2022, 11, 3035. https://doi.org/10.3390/jcm11113035
Luiso D, Herrero-Torrus M, Badosa N, Roqueta C, Ruiz-Bustillo S, Belarte-Tornero LC, Valdivielso-Moré S, Morales RO, Vázquez O, Farré N. Quality of Life in Older Patients after a Heart Failure Hospitalization: Results from the SENECOR Study. Journal of Clinical Medicine. 2022; 11(11):3035. https://doi.org/10.3390/jcm11113035
Chicago/Turabian StyleLuiso, Daniele, Marta Herrero-Torrus, Neus Badosa, Cristina Roqueta, Sonia Ruiz-Bustillo, Laia C. Belarte-Tornero, Sandra Valdivielso-Moré, Ronald O. Morales, Olga Vázquez, and Núria Farré. 2022. "Quality of Life in Older Patients after a Heart Failure Hospitalization: Results from the SENECOR Study" Journal of Clinical Medicine 11, no. 11: 3035. https://doi.org/10.3390/jcm11113035
APA StyleLuiso, D., Herrero-Torrus, M., Badosa, N., Roqueta, C., Ruiz-Bustillo, S., Belarte-Tornero, L. C., Valdivielso-Moré, S., Morales, R. O., Vázquez, O., & Farré, N. (2022). Quality of Life in Older Patients after a Heart Failure Hospitalization: Results from the SENECOR Study. Journal of Clinical Medicine, 11(11), 3035. https://doi.org/10.3390/jcm11113035






