Network Analysis of DSM Symptoms of Substance Use Disorders and Frequently Co-Occurring Mental Disorders in Patients with Substance Use Disorder Who Seek Treatment
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Instruments
2.3.1. Substance Use Disorders (SUD)
2.3.2. Attention Deficit Hyperactivity Disorder (ADHD)
2.3.3. Other Mental Disorders
2.4. Procedure
2.5. Data Analysis
2.5.1. Network Analyses
2.5.2. Comparison of Symptom Networks by Gender
3. Results
3.1. Demographic and Clinical Characteristics
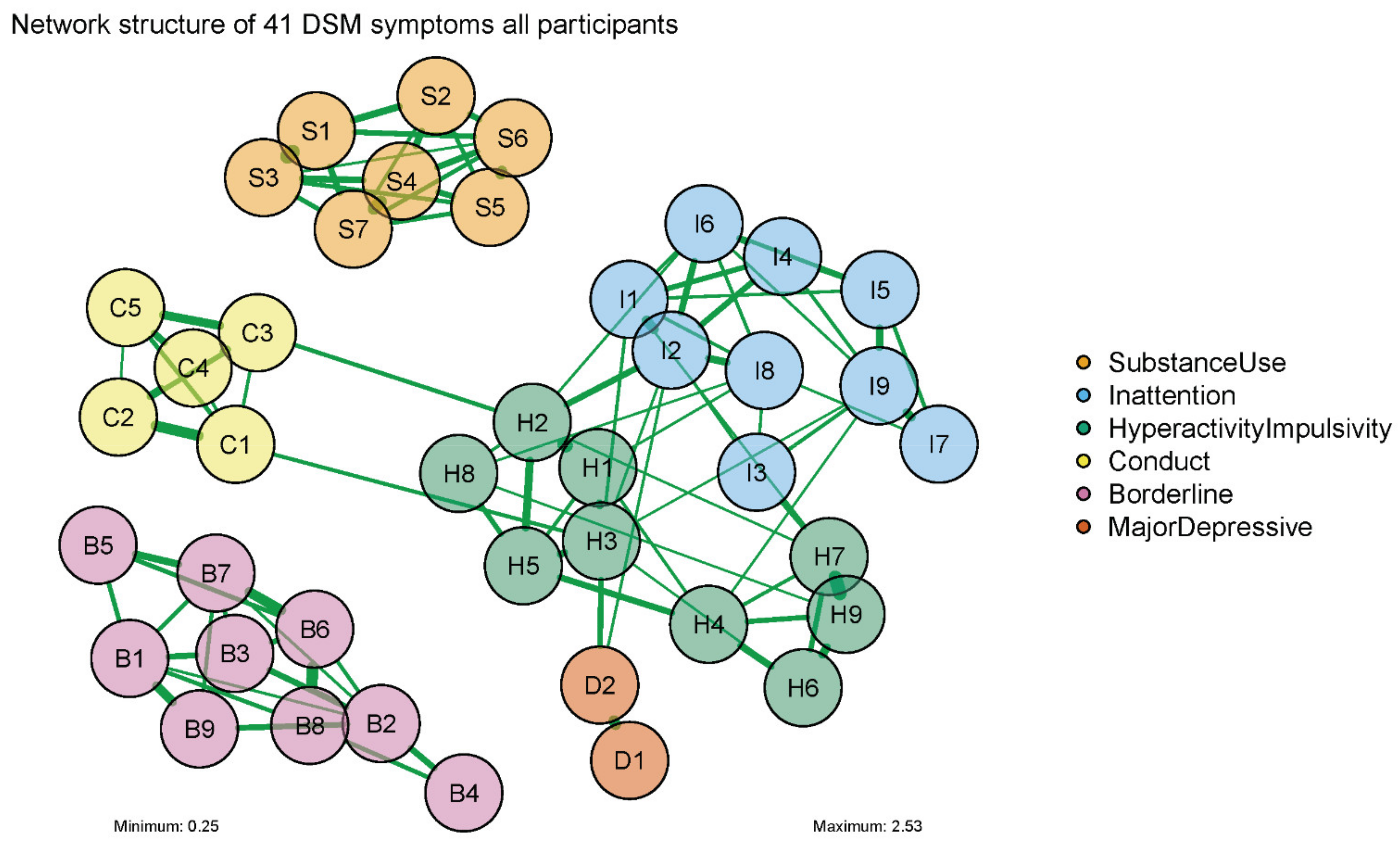
3.2. Estimation of Symptom Networks
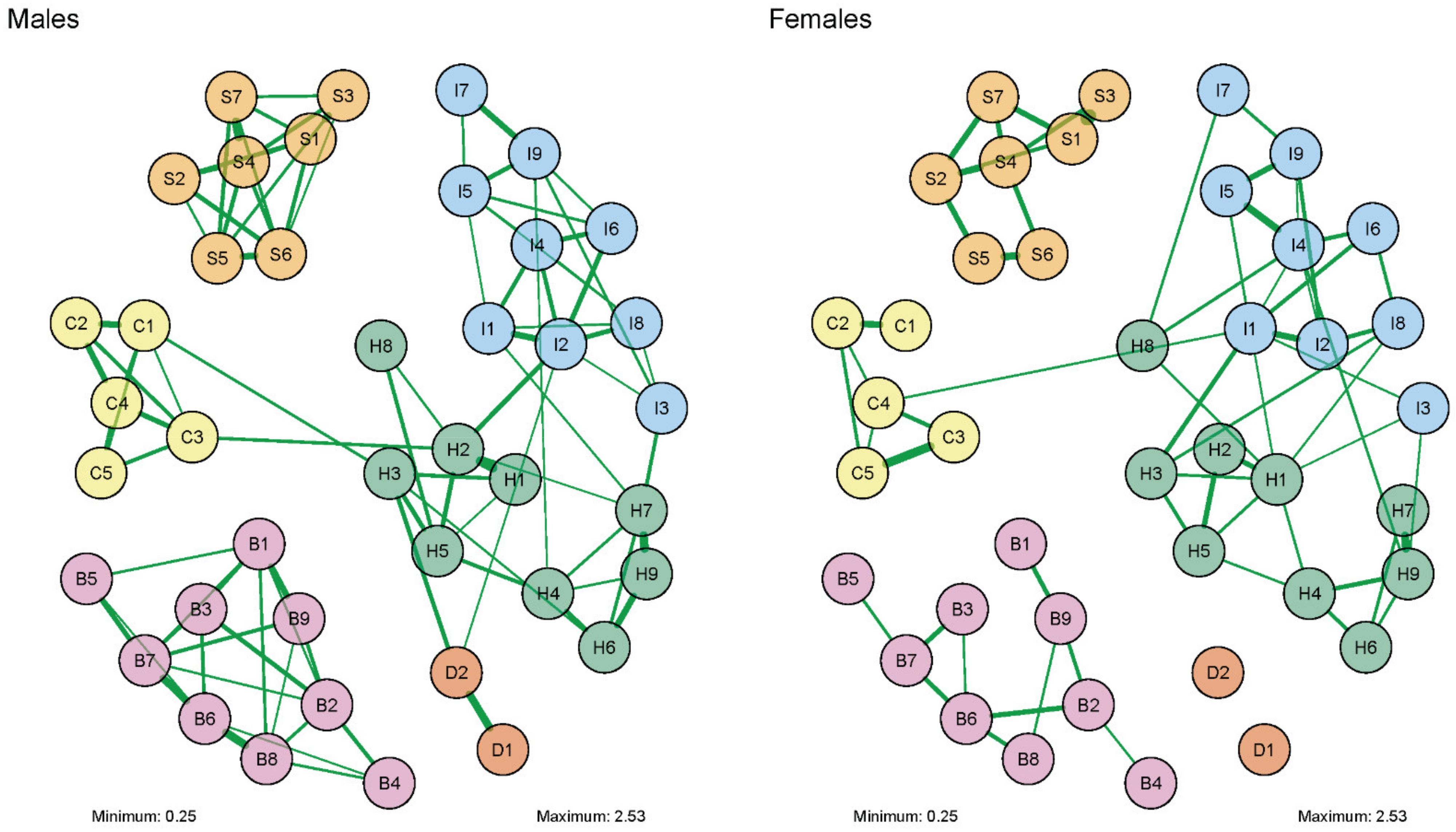
3.3. Comparison of Networks of DSM Symptoms by Gender
4. Discussion
4.1. Limitations
4.2. Clinical Implications and Future Research Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Institute on Drug Abuse. Common Comorbidities with Substance Use Disorders Research Report Part 1: The Connection between Substance Use Disorders and Mental Illness; National Institute on Drug Abuse: Bethesda, MD, USA, 2021.
- National Institute on Drug Abuse. Common Comorbidities with Substance Use Disorders Research Report: Part 2: Co-Occurring Substance Use Disorder and Physical Comorbidities; National Institute on Drug Abuse: Bethesda, MD, USA, 2021.
- Kelly, T.M.; Daley, D.C. Integrated treatment of substance use and psychiatric disorders. Soc. Work Public Health 2013, 28, 388–406. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.; Peselow, E. Co-occurring psychotic and addictive disorders: Neurobiology and diagnosis. Clin. Neuropharmacol. 2012, 35, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Conway, K.P.; Compton, W.; Stinson, F.S.; Grant, B.F. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J. Clin. Psychiatry 2006, 67, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Magidson, J.F.; Liu, S.-M.; Lejuez, C.W.; Blanco, C. Comparison of the course of substance use disorders among individuals with and without generalized anxiety disorder in a nationally representative sample. J. Psychiatr. Res. 2012, 46, 659–666. [Google Scholar] [CrossRef]
- Compton, W.M.; Thomas, Y.F.; Stinson, F.S.; Grant, B.F. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Arch. Gen. Psychiatry 2007, 64, 566–576. [Google Scholar] [CrossRef]
- Lai, H.M.; Cleary, M.; Sitharthan, T.; Hunt, G.E. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug Alcohol Depend. 2015, 154, 1–13. [Google Scholar] [CrossRef]
- Van Emmerik-van Oortmerssen, K.; van de Glind, G.; van den Brink, W.; Smit, F.; Crunelle, C.L.; Swets, M.; Schoevers, R.A. Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: A meta-analysis and meta-regression analysis. Drug Alcohol Depend. 2012, 122, 11–19. [Google Scholar] [CrossRef]
- Pennay, A.; Cameron, J.; Reichert, T.; Strickland, H.; Lee, N.K.; Hall, K.; Lubman, D.I. A systematic review of interventions for co-occurring substance use disorder and borderline personality disorder. J. Subst. Abuse Treat. 2011, 41, 363–373. [Google Scholar] [CrossRef]
- Morojele, N.K.; Saban, A.; Seedat, S. Clinical presentations and diagnostic issues in dual diagnosis disorders. Curr. Opin. Psychiatry 2012, 25, 181–186. [Google Scholar] [CrossRef]
- Mueser, K.T.; Gingerich, S. Treatment of co-occurring psychotic and substance use disorders. Soc. Work Public Health 2013, 28, 424–439. [Google Scholar] [CrossRef]
- Torrens, M.; Rossi, P.C.; Martinez-Riera, R.; Martinez-Sanvisens, D.; Bulbena, A. Psychiatric co-morbidity and substance use disorders: Treatment in parallel systems or in one integrated system? Subst. Use Misuse 2012, 47, 1005–1014. [Google Scholar] [CrossRef] [PubMed]
- DeMarce, J.M.; Lash, S.J.; Stephens, R.S.; Grambow, S.C.; Burden, J.L. Promoting continuing care adherence among substance abusers with co-occurring psychiatric disorders following residential treatment. Addict. Behav. 2008, 33, 1104–1112. [Google Scholar] [CrossRef] [PubMed]
- Pedraz, M.; Araos, P.; García-Marchena, N.; Serrano, A.; Romero-Sanchiz, P.; Suárez, J.; Castilla-Ortega, E.; Mayoral-Cleries, F.; Ruiz, J.J.; Pastor, A.; et al. Sex differences in psychiatric comorbidity and plasma biomarkers for cocaine addiction in abstinent cocaine-addicted subjects in outpatient settings. Front. Psychiatry 2015, 6, 17. [Google Scholar] [CrossRef] [PubMed]
- National Institute on Drug Abuse. Substance Use in Women Research Report: Other Sex and Gender Issues for Women Related to Substance Use; National Institute on Drug Abuse: Bethesda, MD, USA, 2021.
- Korsgaard, H.O.; Torgersen, S.; Wentzel-Larsen, T.; Ulberg, R. Substance abuse and personality disorder comorbidity in adolescent outpatients: Are girls more severely ill than boys? Child Adolesc. Psychiatry Ment. Health 2016, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Van Emmerik-van Oortmerssen, K.; van de Glind, G.; Koeter, M.W.; Allsop, S.; Auriacombe, M.; Barta, C.; Bu, E.T.; Burren, Y.; Carpentier, P.J.; Carruthers, S.; et al. Psychiatric comorbidity in treatment-seeking substance use disorder patients with and without attention deficit hyperactivity disorder: Results of the IASP study. Addiction 2014, 109, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Ottosen, C.; Petersen, L.; Larsen, J.T.; Dalsgaard, S. Gender Differences in Associations between Attention-Deficit/Hyperactivity Disorder and Substance Use Disorder. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 227–234.e4. [Google Scholar] [CrossRef][Green Version]
- Grilo, C.M.; Martino, S.; Walker, M.L.; Becker, D.F.; Edell, W.S.; McGlashan, T.H. Psychiatric comorbidity differences in male and female adult psychiatric inpatients with substance use disorders. Compr. Psychiatry 1997, 38, 155–159. [Google Scholar] [CrossRef]
- Borsboom, D.; Cramer, A.O. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef]
- Forrest, L.N.; Sarfan, L.D.; Ortiz, S.N.; Brown, T.A.; Smith, A.R. Bridging eating disorder symptoms and trait anxiety in patients with eating disorders: A network approach. Int. J. Eat. Disord. 2019, 52, 701–711. [Google Scholar] [CrossRef]
- Borsboom, D. A network theory of mental disorders. World Psychiatry 2017, 16, 5–13. [Google Scholar] [CrossRef]
- Cramer, A.O.; Waldorp, L.J.; van der Maas, H.L.; Borsboom, D. Comorbidity: A network perspective. Behav. Brain Sci. 2010, 33, 137–150, discussion 150–193. [Google Scholar] [CrossRef] [PubMed]
- Van de Glind, G.; Konstenius, M.; Koeter, M.W.; van Emmerik-van Oortmerssen, K.; Carpentier, P.J.; Kaye, S.; Degenhardt, L.; Skutle, A.; Franck, J.; Bu, E.T.; et al. Variability in the prevalence of adult ADHD in treatment seeking substance use disorder patients: Results from an international multi-center study exploring DSM-IV and DSM-5 criteria. Drug Alcohol Depend. 2014, 134, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Van de Glind, G.; Van Emmerik-van Oortmerssen, K.; Carpentier, P.J.; Levin, F.R.; Koeter, M.W.; Barta, C.; Kaye, S.; Skutle, A.; Franck, J.; Konstenius, M.; et al. The International ADHD in Substance Use Disorders Prevalence (IASP) study: Background, methods and study population. Int. J. Methods Psychiatr. Res. 2013, 22, 232–244. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Garcia, N.C.; Gonzalez, R.A.; Ramos-Quiroga, J.A.; van den Brink, W.; Luderer, M.; Blankers, M.; Grau-Lopez, L.; Levin, F.R.; Kaye, S.; Demetrovics, Z.; et al. Attention Deficit Hyperactivity Disorder Increases Nicotine Addiction Severity in Adults Seeking Treatment for Substance Use Disorders: The Role of Personality Disorders. Eur. Addict. Res. 2020, 26, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59 (Suppl. 20), 22–33, quiz 34–57. [Google Scholar] [PubMed]
- Epstein, J.; Johnson, D.E.; Conners, C.K. Conners’ Adult ADHD Diagnostic Interview for DSM-IV (CAADID); Multi-Health Systems: North Tonawanda, NY, USA, 2001. [Google Scholar]
- Epstein, J.; Kollins, S. Psychometric properties of an adult ADHD diagnostic interview. J. Atten. Disord. 2006, 9, 504–514. [Google Scholar] [CrossRef] [PubMed]
- First, M.B.; Gibbon, M.; Spitzer, R.L.; Williams, J.B.W.; Benjamin, L.S. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II); American Psychiatric Press: Washington, DC, USA, 1997. [Google Scholar]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef]
- Ambrosini, P.J. Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS). J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 49–58. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Lecrubier, Y.; Harnett Sheehan, K.; Janavs, J.; Weiller, E.; Keskiner, A.; Schinka, J.; Knapp, E.; Sheehan, M.F.; Dunbar, G.C. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur. Psychiatry 1997, 12, 232–241. [Google Scholar] [CrossRef]
- Van Borkulo, C.; Borsboom, D.; Epskamp, S.; Blanken, T.F.; Boschloo, L.; Schoevers, R.A.; Waldorp, L.J. A new method for constructing networks from binary data. Sci. Rep. 2014, 4, 5918. [Google Scholar] [CrossRef]
- Van Borkulo, C.; Epskamp, S.; Robitzsch, A. IsingFit: Fitting Ising Models Using the eLasso Method. 2016. Available online: https://cran.r-project.org/web/packages/IsingFit/index.html (accessed on 12 April 2021).
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef] [PubMed]
- Van Borkulo, C.; van Bork, R.; Boschloo, L.; Kossakowski, J.J.; Tio, P.; Schoevers, R.A.; Borsboom, D.; Waldorp, L.J. Comparing network structures on three aspects: A permutation test. Psychol. Methods 2022, in press. [CrossRef] [PubMed]
- Van Borkulo, C.; Boschloo, L.; Borsboom, D.; Penninx, B.W.J.H.; Waldorp, L.J.; Schoevers, R.A. Association of symptom network structure with the course of longitudinal depression. JAMA Psychiatry 2015, 72, 1219–1226. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Epskamp, S.; Cramer, A.O.J.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. Qgraph: Network visualizations of relationships in psychometric data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef]
- Boschloo, L.; van Borkulo, C.D.; Rhemtulla, M.; Keyes, K.M.; Borsboom, D.; Schoevers, R.A. The Network Structure of Symptoms of the Diagnostic and Statistical Manual of Mental Disorders. PLoS ONE 2015, 10, e0137621. [Google Scholar] [CrossRef] [PubMed]
- Molina, B.S.G.; Pelham, W.E., Jr. Attention-deficit/hyperactivity disorder and risk of substance use disorder: Developmental considerations, potential pathways, and opportunities for research. Annu. Rev. Clin. Psychol. 2014, 10, 607–639. [Google Scholar] [CrossRef] [PubMed]
- Casey, B.J.; Jones, R.M. Neurobiology of the adolescent brain and behavior: Implications for substance use disorders. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 1189–1201. [Google Scholar] [CrossRef]
- Wilens, T.E.; Decker, M.W. Neuronal nicotinic receptor agonists for the treatment of attention-deficit/hyperactivity disorder: Focus on cognition. Biochem. Pharmacol. 2007, 74, 1212–1223. [Google Scholar] [CrossRef]
- Zulauf, C.A.; Sprich, S.E.; Safren, S.A.; Wilens, T.E. The complicated relationship between attention deficit/hyperactivity disorder and substance use disorders. Curr. Psychiatry Rep. 2014, 16, 436. [Google Scholar] [CrossRef]
- Rhemtulla, M.; Fried, E.I.; Aggen, S.H.; Tuerlinckx, F.; Kendler, K.S.; Borsboom, D. Network analysis of substance abuse and dependence symptoms. Drug Alcohol Depend. 2016, 161, 230–237. [Google Scholar] [CrossRef]
- Rutten, R.J.T.; Broekman, T.G.; Schippers, G.M.; Schellekens, A.F.A. Symptom networks in patients with substance use disorders. Drug Alcohol Depend. 2021, 229 Pt B, 109080. [Google Scholar] [CrossRef]
- DeVito, E.E.; Weinberger, A.H.; Pang, R.D.; Petersen, N.; Fagle, T.; Allen, A.M. Impulsivity across substance use categories: Consideration of sex/gender. Curr. Behav. Neurosci. Rep. 2020, 7, 109–127. [Google Scholar] [CrossRef] [PubMed]
- Drapalski, A.; Bennett, M.; Bellack, A. Gender differences in substance use, consequences, motivation to change, and treatment seeking in people with serious mental illness. Subst. Use Misuse 2011, 46, 808–818. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.; Nixon, S.J. Characterizing gender differences in treatment seekers. Alcohol. Clin. Exp. Res. 2014, 38, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.W.; Banducci, A.N.; Guller, L.; Macatee, R.J.; Lavelle, A.; Daughters, S.B.; Lejuez, C.W. An examination of psychiatric comorbidities as a function of gender and substance type within an inpatient substance use treatment program. Drug Alcohol Depend. 2011, 118, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Hunt, G.E.; Malhi, G.S.; Cleary, M.; Lai, H.M.X.; Sitharthan, T. Prevalence of comorbid bipolar and substance use disorders in clinical settings, 1990–2015: Systematic review and meta-analysis. J. Affect. Disord. 2016, 206, 331–349. [Google Scholar] [CrossRef] [PubMed]
- Lux, V.; Kendler, K.S. Deconstructing major depression: A validation study of the DSM-IV symptomatic criteria. Psychol. Med. 2010, 40, 1679–1690. [Google Scholar] [CrossRef]
- National Institute on Drug Abuse. Substance Use in Women Research Report: Sex and Gender Differences in Substance Use; National Institute on Drug Abuse: Bethesda, MD, USA, 2021.
- Degenhardt, L.; Bharat, C.; Glantz, M.D.; Sampson, N.A.; Scott, K.; Lim, C.C.W.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Alonso, J.; Andrade, L.H.; et al. The epidemiology of drug use disorders cross-nationally: Findings from the WHO’s World Mental Health Surveys. Int. J. Drug Policy 2019, 71, 103–112. [Google Scholar] [CrossRef]
- Center for Behavioral Health Statistics and Quality. Results from the 2016 National Survey on Drug Use and Health: Detailed Tables; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2017.
- Kennedy, A.P.; Epstein, D.H.; Phillips, K.A.; Preston, K.L. Sex differences in cocaine/heroin users: Drug-use triggers and craving in daily life. Drug Alcohol Depend. 2013, 132, 29–37. [Google Scholar] [CrossRef]
- Fox, H.C.; Morgan, P.T.; Sinha, R. Sex differences in guanfacine effects on drug craving and stress arousal in cocaine-dependent individuals. Neuropsychopharmacology 2014, 39, 1527–1537. [Google Scholar] [CrossRef]
- Hitschfeld, M.J.; Schneekloth, T.D.; Ebbert, J.O.; Hall-Flavin, D.K.; Karpyak, V.M.; Abulseoud, O.A.; Patten, C.A.; Geske, J.R.; Frye, M.A. Female smokers have the highest alcohol craving in a residential alcoholism treatment cohort. Drug Alcohol Depend. 2015, 150, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Becker, J.B.; McClellan, M.; Reed, B.G. Sociocultural context for sex differences in addiction. Addict. Biol. 2016, 21, 1052–1059. [Google Scholar] [CrossRef] [PubMed]
- Bobzean, S.A.; DeNobrega, A.K.; Perrotti, L.I. Sex differences in the neurobiology of drug addiction. Exp. Neurol. 2014, 259, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Kippin, T.E.; Fuchs, R.A.; Mehta, R.H.; Case, J.M.; Parker, M.P.; Bimonte-Nelson, H.A.; See, R.E. Potentiation of cocaine-primed reinstatement of drug seeking in female rats during estrus. Psychopharmacology 2005, 182, 245–252. [Google Scholar] [CrossRef]
- Lewis, B.; Hoffman, L.A.; Nixon, S.J. Sex differences in drug use among polysubstance users. Drug Alcohol Depend. 2014, 145, 127–133. [Google Scholar] [CrossRef]
- Fonseca, F.; Robles-Martínez, M.; Tirado-Muñoz, J.; Alías-Ferri, M.; Mestre-Pintó, J.-I.; Coratu, A.M.; Torrens, M. A Gender Perspective of Addictive Disorders. Curr. Addict. Rep. 2021, 8, 89–99. [Google Scholar] [CrossRef]
- American Educational Research Association; American Psychological Association; National Council on Measurement in Education. Standards for Educational and Psychological Testing; American Educational Research Association: Washington, DC, USA, 2014. [Google Scholar]
- Naglieri, J.A.; Goldstein, S. Assessment of Executive Function using Rating Scales: Psychometric Considerations. In Handbook of Executive Functions; Goldstein, S., Naglieri, J., Eds.; Springer: New York, NY, USA, 2014; pp. 159–170. [Google Scholar]
- Jones, P.J.; Ma, R.; McNally, R.J. Bridge Centrality: A Network Approach to Understanding Comorbidity. Multivar. Behav. Res. 2021, 56, 353–367. [Google Scholar] [CrossRef]
| Node | Disorder and Symptom Descriptions |
|---|---|
| Substance Use Disorder | |
| S1 | tolerance |
| S2 | abstinence or withdrawal |
| S3 | used more or longer than intended |
| S4 | tried to cut down or quit |
| S5 | spent time using or acquiring substance |
| S6 | reduced time on social or other activities for substance use |
| S7 | keep using despite health or psychological problems |
| Inattention | |
| I1 | fails to give close attention/make careless mistakes |
| I2 | difficulty sustaining attention |
| I3 | does not seem to listen when spoken to directly |
| I4 | Difficult to follow through on instructions/fails to finish projects |
| I5 | difficulty organizing tasks or activities |
| I6 | avoid, dislike, reluctant to tasks that require sustained mental effort |
| I7 | often loses things necessary for tasks or activities |
| I8 | often easily distracted by extraneous stimuli |
| I9 | often forgetful in daily activities |
| Hyperactivity/Impulsivity | |
| H1 | fidgets a lot when seated |
| H2 | often trouble remaining seated |
| H3 | often experience feelings of restlessness |
| H4 | difficulty being as quiet as others |
| H5 | always on the go |
| H6 | often talks too much |
| H7 | often answer questions before completed |
| H8 | often have trouble waiting for your turn |
| H9 | often interrupts others |
| Conduct Disorder | |
| C1 | skipped school or stayed out < age 15 |
| C2 | Lie cheat steal < age 15 |
| C3 | Fights, threatened, intimidated others < age 15 |
| C4 | destroyed others property or set fires < age 15 |
| C5 | maltreatment animals or cruelty to people < age 15 |
| Borderline Personality Disorder | |
| B1 | you got upset at the thought of someone leaving you |
| B2 | ups and downs in relationships with people you care about |
| B3 | feeling of who you are and which direction you are going has suddenly changed |
| B4 | often done things impulsively |
| B5 | tried to injure yourself or threatened to do so |
| B6 | many sudden mood swings |
| B7 | you often feel empty inside |
| B8 | often angry outbursts or so angry that you lose control |
| B9 | when under great stress, feeling suspicious or alienated towards people |
| Major Depression | |
| D1 | depressed mood (current) |
| D2 | depressed mood (lifetime) |
| Males | Females | Total Sample a | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| 597 (77.33) | 175 (22.67) | 772 (100) | |
| Age Mean (SD) | 37.99 (11.23) | 36.86 (10.98) | 37.74 (11.17) |
| Ethnicity ** | |||
| Caucasian | 351 (64.17) | 108 (72.97) | 459 (66.04) |
| Hispanic | 175 (31.99) | 29 (19.59) | 204 (29.35) |
| Other | 21 (3.84) | 11 (7.43) | 32 (4.60) |
| Marital status | |||
| Single/Divorced | 458 (78.16) | 123 (71.93) | 581 (76.75) |
| Housing | |||
| Homeless/In shelter | 105 (18.45) | 32 (19.16) | 137 (18.61) |
| Alone | 185 (32.51) | 61 (36.53) | 246 (33.42) |
| With Partner/Friends/Parents | 279 (49.03) | 74 (44.31) | 353 (47.96) |
| Employment * | |||
| Employed | 192 (33.10) | 39 (23.35) | 231 (30.92) |
| Unemployed | 299 (51.55) | 94 (56.29) | 393 (52.61) |
| Sick leave/Disability | 89 (15.34 | 34 (20.36) | 123 (16.47) |
| Main substance used * | |||
| Alcohol | 220 (37.23) | 61 (35.26) | 281 (36.78) |
| Amphetamines | 35 (5.92) | 17 (9.83) | 52 (6.81) |
| Cannabis | 123 (20.81) | 20 (11.56) | 143 (18.72) |
| Cocaine | 72 (12.18) | 17 (9.83) | 89 (11.65) |
| Heroin | 90 (15.23) | 31 (17.92) | 121 (15.84) |
| Prescription opioids | 20 (3.38) | 12 (6.94) | 32 (4.19) |
| Methadone | 12 (2.03) | 6 (3.47) | 18 (2.36) |
| Other | 19 (3.21) | 9 (5.20) | 28 (3.66) |
| Psychiatric comorbidity | |||
| Adult ADHD * | 85 (14.60) | 15 (8.72) | 100 (13.26) |
| Conduct disorder (<age16) | 159 (46.09) | 52 (48.15) | 211 (46.58) |
| ASP | 122 (35.67) | 48 (45.28) | 170 (37.95) |
| BPD *** | 131 (21.94) | 62(35.43) | 193 (25.00) |
| MDD | 152 (48.56) | 56 (56.57) | 208 (50.49) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Toro, E.; Wolf, C.J.H.; González, R.A.; van den Brink, W.; Schellekens, A.; Vélez-Pastrana, M.C.; on behalf of the AFP Working Collaborative Group. Network Analysis of DSM Symptoms of Substance Use Disorders and Frequently Co-Occurring Mental Disorders in Patients with Substance Use Disorder Who Seek Treatment. J. Clin. Med. 2022, 11, 2883. https://doi.org/10.3390/jcm11102883
López-Toro E, Wolf CJH, González RA, van den Brink W, Schellekens A, Vélez-Pastrana MC, on behalf of the AFP Working Collaborative Group. Network Analysis of DSM Symptoms of Substance Use Disorders and Frequently Co-Occurring Mental Disorders in Patients with Substance Use Disorder Who Seek Treatment. Journal of Clinical Medicine. 2022; 11(10):2883. https://doi.org/10.3390/jcm11102883
Chicago/Turabian StyleLópez-Toro, Edith, Casper J. H. Wolf, Rafael A. González, Wim van den Brink, Arnt Schellekens, María C. Vélez-Pastrana, and on behalf of the AFP Working Collaborative Group. 2022. "Network Analysis of DSM Symptoms of Substance Use Disorders and Frequently Co-Occurring Mental Disorders in Patients with Substance Use Disorder Who Seek Treatment" Journal of Clinical Medicine 11, no. 10: 2883. https://doi.org/10.3390/jcm11102883
APA StyleLópez-Toro, E., Wolf, C. J. H., González, R. A., van den Brink, W., Schellekens, A., Vélez-Pastrana, M. C., & on behalf of the AFP Working Collaborative Group. (2022). Network Analysis of DSM Symptoms of Substance Use Disorders and Frequently Co-Occurring Mental Disorders in Patients with Substance Use Disorder Who Seek Treatment. Journal of Clinical Medicine, 11(10), 2883. https://doi.org/10.3390/jcm11102883







