Risk Factors Associated with Mortality in Severe Chest Trauma Patients Admitted to the ICU
Abstract
:1. Introduction
2. Materials and Methods
2.1. Definitions
- -
- Severe chest trauma was defined as an Abbreviated Injury Scale (AIS) value of ≥3 in the thoracic area. The control group included patients without chest trauma and those with thoracic AIS ≤ 2 [8].
- -
- Hemodynamic condition was considered as follows [9]:
- Stable, systolic blood pressure > 90 mmHg during initial trauma care.
- Unstable, responding to volume replacement—systolic blood pressure < 90 mmHg requiring volume replacement for normalization.
- Shock, systolic blood pressure < 90 mmHg requiring volume replacement, blood products, and vasoactive support for normalization.
- Refractory shock, hypotension refractory to volume replacement, blood products, or vasoactive support and activation of the massive bleeding protocol.
- -
- Rhabdomyolysis, laboratory test determination of creatine kinase > 5000 U/L [10].
- -
- Acute kidney injury (AKI) was evaluated by using the Risk, Injury, Failure, Loss of kidney function and End-stage kidney disease (RIFLE) definition [10].
- -
- Trauma-associated coagulopathy, prolongation of the prothrombin and activated partial thromboplastin over 1.5 times the control values, fibrinogen < 150 mg/dL, or thrombocytopenia (<100,000/µL) in the first 24 h [9].
- -
- Multiorgan failure was defined, using the Sequential-related Organ Failure Assessment (SOFA), as the alteration of two or more organs with a score of ≥3 [9].
- -
- Massive hemorrhage was defined as the need for more than 10 packed red blood cell concentrates in the initial 24 h.
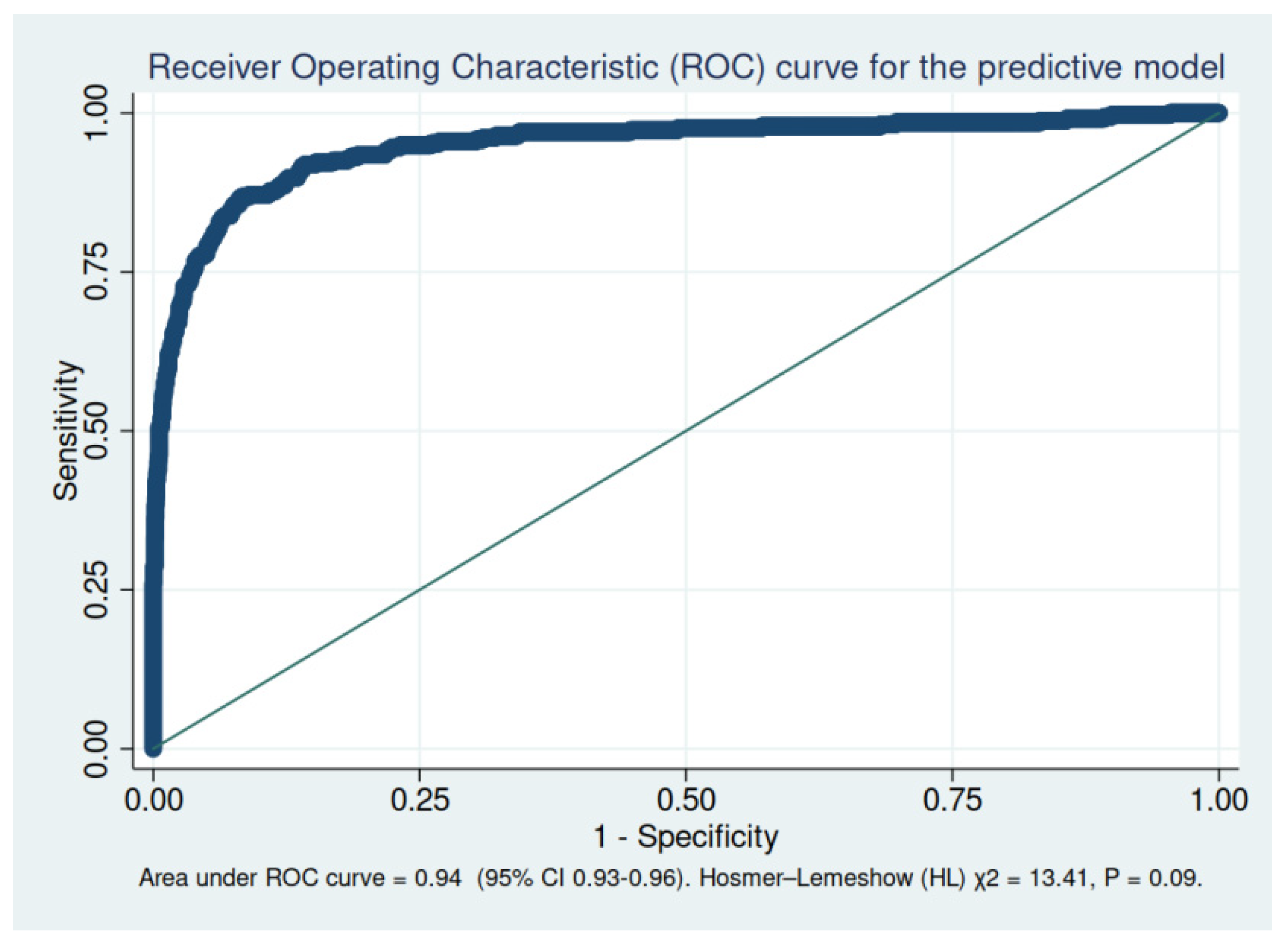
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Krug, E.G.; Sharma, G.K.; Lozano, R. The global burden of injuries. Am. J. Public Health 2000, 90, 523–526. [Google Scholar]
- Chico-Fernández, M.; Llompart-Pou, J.; Guerrero-López, F.; Sánchez-Casado, M.; García-Sáez, I.; Mayor-García, M.; Egea-Guerrero, J.; Fernández-Ortega, J.; Bueno-González, A.; González-Robledo, J.; et al. Epidemiology of severe trauma in Spain. Registry of trauma in the ICU (RETRAUCI). Pilot phase. Med. Intensiv. 2016, 40, 327–347. [Google Scholar] [CrossRef]
- Eastridge, B.J.; Mabry, R.L.; Seguin, P.; Cantrell, J.; Tops, T.; Uribe, P.; Mallett, O.; Zubko, T.; Oetjen-Gerdes, L.; Rasmussen, T.E. Death on the battlefield (2001–2011): Implications for the future of combat casualty care. J. Trauma Acute Care Surg. 2012, 73 (Suppl. S5), 431–437. [Google Scholar] [CrossRef]
- Llompart-Pou, J.A.; Chico-Fernández, M. Traumatic critical hemorrhage. Future challenges. Med. Intensiva 2021. [Google Scholar] [CrossRef]
- O’Connor, J.V.; Adamski, J. The diagnosis and treatment of non-cardiac thoracic trauma. J. R. Army Med. Corps 2010, 156, 5–14. [Google Scholar] [CrossRef]
- Horst, K.; Andruszkow, H.; Weber, C.D.; Pishnamaz, M.; Herren, C.; Zhi, Q.; Knobe, M.; Lefering, R.; Hildebrand, F.; Pape, H.-C. Thoracic trauma now and then: A 10 year experience from 16,773 severely injured patients. PLoS ONE 2017, 12, e0186712. [Google Scholar] [CrossRef]
- Chrysou, K.; Halat, G.; Hoksch, B.; Schmid, R.A.; Kocher, G.J. Lessons from a large trauma center: Impact of blunt chest trauma in polytrauma patients-still a relevant problem? Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 42. [Google Scholar] [CrossRef]
- Grubmüller, M.; Kerschbaum, M.; Diepold, E.; Angerpointner, K.; Nerlich, M.; Ernstbergeret, A. Severe thoracic trauma—still an independent predictor for death in multiple injured patients? Scand J. Trauma Resusc Emerg. Med. 2018, 26, 6. [Google Scholar] [CrossRef] [Green Version]
- Barea-Mendoza, J.A.; Chico-Fernández, M.; Molina-Díaz, I.; Moreno-Muñoz, G.; Toboso-Casado, J.M.; Viña-Soria, L.; Matachana-Martínez, M.; Freire-Aragón, M.D.; Pérez-Bárcena, J.; Llompart-Pou, J.A. Neurointensive Care and Trauma Working Group of the Spanish Society of Intensive Care Medicine (SEMICYUC). Risk Factors Associated with Early and Late Posttraumatic Multiorgan Failure: An Analysis From RETRAUCI. Shock 2021, 55, 326–331. [Google Scholar] [CrossRef]
- Chico-Fernández, M.; Barea-Mendoza, J.A.; Ormazabal-Zabala, T.; Moreno-Muñoz, G.; Pastor-Marcos, D.; Bueno-González, A.; Iglesias-Santiago, A.; Ballesteros-Sanz, M.Á; Pérez-Bárcena, J.; Llompart-Pou, J.A. Associated risk factors and outcomes of acute kidney injury in severe trauma: Results from the Spanish trauma ICU registry (RETRAUCI). Anaesth. Crit. Care Pain Med. 2020, 39, 503–506. [Google Scholar] [CrossRef]
- Benchimol, E.I.; Smeeth, L.; Guttmann, A.; Harron, K.; Moher, D.; Petersen, I.; Sørensen, H.T.; von Elm, E.; Langan, S.M.; RECORD Working Committee. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PloS Med. 2015, 12, e1001885. [Google Scholar] [CrossRef]
- Bayer, J.; Lefering, R.; Reinhardt, S.; Kühle, J.; Zwingmann, J.; Südkamp, N.P.; Hammer, T.; TraumaRegister DGU. Thoracic trauma severity contributes to differences in intensive care therapy and mortality of severely injured patients: Analysis based on the TraumaRegister DGU®. World J. Emerg. Surg. 2017, 12, 43. [Google Scholar] [CrossRef]
- Dai, D.; Yuan, Q.; Sun, Y.; Yuan, F.; Su, Z.; Dinget, J.; Tian, H. Impact of thoracic injury on traumatic brain injury outcome. PLoS ONE 2013, 8, e74204. [Google Scholar]
- Schieren, M.; Wappler, F.; Wafaisade, A.; Lefering, R.; Sakka, S.G.; Kaufmann, J.; Heiroth, H.-J.; Defosse, J.; Böhmer, A.B. Impact of blunt chest trauma on outcome after traumatic brain injury- a matched-pair analysis of the TraumaRegister DGU®. Scand J. Trauma Resusc. Emerg. Med. 2020, 28, 21. [Google Scholar] [CrossRef] [PubMed]
- Bouzat, P.; Raux, M.; David, J.S.; Tazarourte, K.; Galinski, M.; Desmettre, T.; Garrigue, D.; Ducros, L.; Michelet, P.; Expert’s group; et al. Chest trauma: First 48hours management. Anaesth. Crit. Care Pain Med. 2017, 36, 135–145. [Google Scholar] [CrossRef]
- Freixinet Gilart, J.; Hernández Rodríguez, H.; Martínez Vallina, P.; Moreno Balsalobre, R.; Rodríguez Suárez, P.; SEPAR. Guidelines for the diagnosis and treatment of thoracic traumatism. Arch. Bronconeumol. 2011, 47, 41–49. [Google Scholar] [CrossRef]
- Swol, J.; Brodie, D.; Napolitano, L.; Park, P.K.; Thiagarajan, R.; Barbaro, R.P.; Lorusso, R.; McMullan, D.; Cavarocchi, N.; Hssain, A.A.; et al. Indications and outcomes of extracorporeal life support in trauma patients. J. Trauma Acute Care Surg. 2018, 84, 831–837. [Google Scholar] [CrossRef]
- Kasotakis, G.; Hasenboehler, E.A.; Streib, E.W.; Patel, N.; Patel, M.B.; Alarcon, L.; Bosarge, P.L.; Love, J.; Haut, E.R.; Como, J.J. Operative fixation of rib fractures after blunt trauma: A practice management guideline from the Eastern Association for the Surgery of Trauma. J. Trauma Acute Care Surg. 2017, 82, 618–626. [Google Scholar] [CrossRef]
- Huber, S.; Biberthaler, P.; Delhey, P.; Trentzsch, H.; Winter, H.; van Griensven, M.; Rolf Lefering, S.H.; Trauma Register DGU. Predictors of poor outcomes after significant chest trauma in multiply injured patients: A retrospective analysis from the German Trauma Registry (Trauma Register DGU®). Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 52. [Google Scholar] [CrossRef] [Green Version]
- Söderlund, T.; Ikonen, A.; Pyhältö, T.; Handolin, L. Factors associated with in-hospital outcomes in 594 consecutive patients suffering from severe blunt chest trauma. Scand. J. Surg. 2015, 104, 115–1120. [Google Scholar] [CrossRef]
- Battle, C.E.; Hutchings, H.; Evans, P.A. Risk factors that predict mortality in patients with blunt chest wall trauma: A systematic review and meta-analysis. Injury 2012, 43, 8–17. [Google Scholar] [CrossRef]
- Moore, L.; Clark, D.E. The value of trauma registries. Injury 2008, 39, 686–695. [Google Scholar] [CrossRef] [PubMed]
- Lecky, F.; Woodford, M.; Edwards, A.; Bouamra, O.; Coats, T. Trauma scoring systems and databases. Br. J. Anaesth. 2014, 113, 286–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, E.E.; Moore, H.B.; Kornblith, L.Z.; Neal, M.D.; Hoffman, M.; Mutch, N.J.; Schöchl, H.; Hunt, B.J.; Sauaia, A. Trauma-induced coagulopathy. Nat. Rev. Dis. Primers 2021, 7, 30. [Google Scholar] [CrossRef] [PubMed]
| Severe Chest Trauma n = 3821 | Control Group n = 5969 | p-Value | |
|---|---|---|---|
| Age | 49.72 (18.28) | 49.97 (19.79) | 0.668 |
| Sex | 79.53% | 76.47% | <0.01 |
| Penetrating | 5.26% | 6.50% | 0.012 |
| ISS | 25.60 (12.39) | 16.12 (9.47) | <0.001 |
| ISS ≥16 | 80.53% | 53.68% | <0.01 |
| NISS | 31.27 (13.75) | 22.02 (14.00) | <0.001 |
| Mechanism | <0.01 | ||
| Ground-level fall | 11.70% | 30.41% | |
| RTA-car | 21.49% | 13.49% | |
| Precipitation | 18.42% | 11.83% | |
| RTA-motorcycle | 20.70% | 12.95% | |
| RTA-run over | 8.40% | 8.56% | |
| Other | 19.29% | 23.67% | |
| Prehospital mobile ICU | 74.33% | 70.95% | <0.01 |
| Prehospital intubation | 22.03% | 22.41% | 0.825 |
| Hemodinamically stable | 56.71% | 70.02% | <0.01 |
| Severe Chest Trauma n = 3821 | Control Group n = 5969 | p-Value | |
|---|---|---|---|
| Head | 30.83% | 55.79% | <0.001 |
| Face | 2.88% | 3.17% | 0.420 |
| Abdomen | 18.35% | 12.00% | <0.001 |
| Extremities | 22.27% | 17.62% | <0.001 |
| External | 0.24% | 1.71% | <0.001 |
| Severe Chest Trauma n = 3821 | Control Group n = 5969 | p-Value | |
|---|---|---|---|
| Head | 3.06 (1.23) | 3.56 (1.15) | <0.001 |
| Face | 1.79 (0.73) | 1.79 (0.73) | 0.896 |
| Abdomen | 2.68 (0.94) | 2.80 (0.90) | <0.001 |
| Extremities | 2.52 (0.90) | 2.61 (0.95) | <0.001 |
| External | 1.25 (1.56) | 2.26 (1.56) | <0.001 |
| Severe Chest Trauma n = 3821 | Control Group n = 5969 | p-Value | |
|---|---|---|---|
| Rhabdomyolysis | 22.46% | 11.33% | <0.001 |
| Trauma-associated coagulopathy | 20.14% | 13.41% | <0.001 |
| Massive hemorrhage | 9.20% | 4.21% | <0.001 |
| Acute kidney injury | 22.53% | 13.88% | <0.001 |
| Intracranial hypertension | 11.44% | 20.37% | <0.001 |
| Respiratory failure (PaO2/FiO2 < 300) | 39.94% | 17.77% | <0.001 |
| Nosocomial infection | 23.34% | 19.97% | <0.001 |
| Multiorgan failure | 14.76% | 7.01% | <0.001 |
| Severe Chest Trauma n = 3821 | Control Group n = 5969 | p-Value | |
|---|---|---|---|
| Angioembolization | 7.4% | 5.83% | 0.004 |
| MV | 45.09% | 50.96% | <0.001 |
| Days of MV (if ≥1 day) | 10.58 (12.50) | 7.46 (11.00) | <0.001 |
| ICU LOS | 9.97 (16.33) | 7.85 (12.48) | <0.001 |
| ICU mortality | 10.43% | 12.95% | <0.001 |
| In-hospital mortality | 11.81% | 15.00% | <0.001 |
| Cause of death | <0.001 | ||
| Exsanguination | 13.56% | 4.09% | |
| Intracranial hypertension | 34.84% | 57.26% | |
| Multiorgan failure | 30.05% | 14.39% | |
| Other | 21.54% | 24.26% |
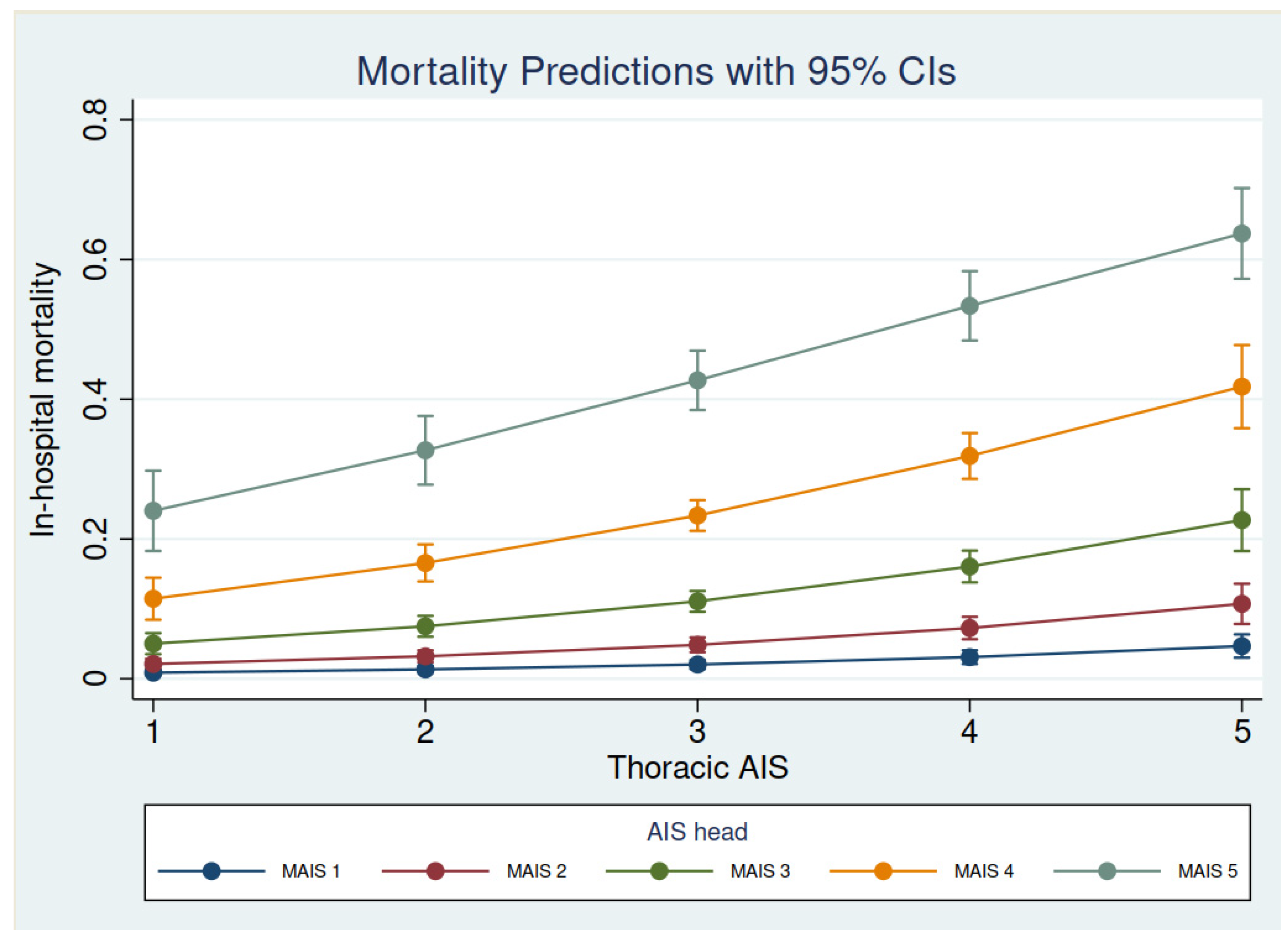
| Variable | OR (95% CI) | p-Value |
|---|---|---|
| Age | 1.03 (1.02–1.04) | <0.001 |
| NISS | 1.02 (1.01–1.04) | <0.001 |
| AIS-head | ||
| AIS-head 2 | 1.92 (1.03–3.58) | 0.039 |
| AIS-head 3 | 1.88 (1.06–3.34) | 0.030 |
| AIS-head 4 | 5.84 (3.29–10.36) | <0.001 |
| AIS-head 5 | 15.92 (8.66–29.26) | <0.001 |
| Hemodynamics | ||
| Unstable volume-response | 1.91 (1.01–3.59) | 0.044 |
| Shock | 4.70 (2.89–7.65) | <0.001 |
| Refractory shock | 73.52 (37.73–143.27) | <0.001 |
| Prehospital intubation | 2.18 (1.55–3.05) | <0.001 |
| Multiorgan failure | 2.82 (1.82–4.38) | <0.001 |
| Acute kidney injury | 1.89 (1.27–2.81) | 0.001 |
| Nosocomial infection | 0.41 (0.26–0.62) | <0.001 |
| Trauma-associated coagulopathy | 0.87 (0.79–0.96) | 0.006 |
| Tracheostomy | 0.08 (0.04–0.15) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barea-Mendoza, J.A.; Chico-Fernández, M.; Quintana-Díaz, M.; Pérez-Bárcena, J.; Serviá-Goixart, L.; Molina-Díaz, I.; Bringas-Bollada, M.; Ruiz-Aguilar, A.L.; Ballesteros-Sanz, M.Á.; Llompart-Pou, J.A.; et al. Risk Factors Associated with Mortality in Severe Chest Trauma Patients Admitted to the ICU. J. Clin. Med. 2022, 11, 266. https://doi.org/10.3390/jcm11010266
Barea-Mendoza JA, Chico-Fernández M, Quintana-Díaz M, Pérez-Bárcena J, Serviá-Goixart L, Molina-Díaz I, Bringas-Bollada M, Ruiz-Aguilar AL, Ballesteros-Sanz MÁ, Llompart-Pou JA, et al. Risk Factors Associated with Mortality in Severe Chest Trauma Patients Admitted to the ICU. Journal of Clinical Medicine. 2022; 11(1):266. https://doi.org/10.3390/jcm11010266
Chicago/Turabian StyleBarea-Mendoza, Jesús Abelardo, Mario Chico-Fernández, Manuel Quintana-Díaz, Jon Pérez-Bárcena, Luís Serviá-Goixart, Ismael Molina-Díaz, María Bringas-Bollada, Antonio Luis Ruiz-Aguilar, María Ángeles Ballesteros-Sanz, Juan Antonio Llompart-Pou, and et al. 2022. "Risk Factors Associated with Mortality in Severe Chest Trauma Patients Admitted to the ICU" Journal of Clinical Medicine 11, no. 1: 266. https://doi.org/10.3390/jcm11010266
APA StyleBarea-Mendoza, J. A., Chico-Fernández, M., Quintana-Díaz, M., Pérez-Bárcena, J., Serviá-Goixart, L., Molina-Díaz, I., Bringas-Bollada, M., Ruiz-Aguilar, A. L., Ballesteros-Sanz, M. Á., Llompart-Pou, J. A., & on behalf of the Neurointensive Care and Trauma Working Group of the Sociedad Española de Medicina Intensiva Crítica y Unidades Coronarias (SEMICYUC). (2022). Risk Factors Associated with Mortality in Severe Chest Trauma Patients Admitted to the ICU. Journal of Clinical Medicine, 11(1), 266. https://doi.org/10.3390/jcm11010266






